Abstract
Objective:
To identify the effects of sleep education programs reported in the literature on the sleep of infants, children, and adolescents.
Method:
This integrative review surveyed the online database Pubmed®and the EBSCOhost®research platform from October to November 2018 using selected descriptors to answer the following question: what are the effects of sleep education programs on the sleep of infants, children, and adolescents, when applied? Inclusion criteria were: scientific articles with full text available in Portuguese or English of primary empiric quantitative studies published between 2013 and 2018.
Results:
The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) model was applied to articles meeting the inclusion criteria. Ninety-three articles were selected. After reading titles and abstracts and identifying the answer to our study question, the final sample consisted of eight articles.
Conclusion:
The integrative review results show education programs have positive effects on sleep when applied to participants of all age groups. The joint application of programs and other methods for improving sleep in children and adolescents was described as beneficial. The results contribute to Nursing because nurses may have a relevant role in effectively implementing and developing sleep education programs.
Keywords
Infant; Child; Adolescent; Sleep; Education
Resumo
Objetivo:
Identificar na literatura a influência de programas educativos de sono, no sono dos lactentes, crianças e adolescentes.
Métodos:
Estudo de revisão integrativa, através de pesquisa na base de dados bibliográficas online Pubmed® e no agregador de base de dados EBSCOhost®, com os descritores de pesquisa selecionados, no período de outubro a novembro de 2018, para responder à pergunta norteadora: Qual a influência dos programas educativos de sono, no sono dos lactentes, crianças e adolescentes quando aplicados? Os critérios de inclusão foram: artigos científicos, disponíveis em texto integral, nos idiomas português ou inglês, relativos a estudos primários, empíricos, de abordagem quantitativa, publicados entre 2013 e 2018.
Resultados:
Foram seguidos os passos do modelo PRISMA ( Preferred Reporting Items for Systematic Reviews and Meta-Analyses ), atendendo aos critérios de inclusão. Foram selecionados 93 artigos e, após a leitura do título e resumo, bem como a identificação da resposta à pergunta norteadora, a amostra final integra 8 artigos.
Conclusão:
Os resultados da revisão integrativa evidenciam que existe uma influência positiva no sono quando aplicados programas de educação sobre o sono em todas as faixas etárias. Foram descritas vantagens na sua aplicação em articulação com outros métodos, para a melhoria do sono das crianças e adolescentes. A implicação destes resultados para a Enfermagem é que o enfermeiro poderá ter uma atuação relevante na implementação e no desenvolvimento efetivo de programas de educação relativamente a esta problemática.
Descritores
Lactente; Criança; Adolescente; Sono; Educação
Resumen
Objetivo:
Identificar en la literatura la influencia de programas educativos de sueño, en el sueño de lactantes, niños y adolescentes.
Métodos:
Estudio de revisión integradora, mediante investigación en la base de datos bibliográfica electrónica Pubmed® y en el agregador de base de datos EBSCOhost®, con los descriptores de investigación seleccionados, en el período de octubre a noviembre de 2018, para responder a la pregunta orientadora: ¿Cuál es la influencia de los programas educativos de sueño, en el sueño de lactantes, niños y adolescentes cuando estos se aplican? Los criterios de inclusión fueron: artículos científicos, con texto completo disponible, en los idiomas portugués o inglés, relativos a estudios primarios, empíricos, de enfoque cualitativo, publicados entre 2013 y 2018.
Resultados:
Se siguieron los pasos del modelo PRISMA ( Preferred Reporting Items for Systematic Reviews and Meta-Analyses ), considerando los criterios de inclusión. Se seleccionaron 93 artículos y, luego de leer el título y el resumen y de identificar la respuesta a la pregunta orientadora, la muestra final fue formada por 8 artículos.
Conclusión:
Los resultados de la revisión integradora evidencian que existe una influencia positiva en el sueño cuando se aplican programas de educación sobre el sueño en todos los grupos de edad. Se describieron las ventajas de su aplicación junto con otros métodos para mejorar el sueño de niños y adolescentes. El impacto de estos resultados en la enfermería es que el enfermero podrá tener una actuación relevante en la implementación y en el desarrollo efectivo de programas de educación relacionados con esta problemática.
Descriptores
Lactante; Niño; Adolescente; Sueño; Educación
Introduction
Sleep is a determining health factor in children and adolescents; sleep deprivation has been correlated with negative effects in various domains, such as cognitive and academic performance, emotional and behavior regulation, and risk of accidental fall and obesity.(11. Silva FG, Silva CR, Braga LB, Serrão Neto AS. [Hábitos e problemas do sono dos dois anos aos dez anos: estudo populacional]. Acta Pediatr Port. 2013;44(5):196–202.)The number of daily sleep hours identified in Portuguese children is below the recommended number of sleep hours; thus, obtaining new tools is critical to develop exclusive, effective, and targeted interventions to prevent sleep deprivation in children.(22. Crispim JN, Boto LR, Melo IS, Ferreira R. Padrão de sono e factores de risco para privação de sono numa população pediátrica portuguesa. Acta Pediatr Port. 2011;42(3):93–8.)In Portugal, a 2018 study(33. Silva EM, Simões PA, Macedo MC, Duarte JC, Silva DM. Perceção parental sobre hábitos e qualidade do sono das crianças em idade pré-escolar. Rev Enferm Ref. 2018;4(17):63–72.)of sleep habits and quality in preschool children was conducted using self-report questionnaires for parents. This study shows that sleep quality in children is usually good, however, a third of the population studied presents poor sleep. Another 2016 study(44. Pinto TR, Pinto JC, Rebelo-Pinto H, Paiva T. O sono em adolescentes portugueses: proposta de um modelo tridimensional. Anal Psicol. 2016;4(34):339–52.)conducted in a population of adolescents concluded that Portuguese teenagers sleep an average of 7h41m (this duration is below the recommendations for this age group) and showed there are irregularities between weekday sleep and weekend sleep (both in wake times and bedtimes). Study data showed adolescents faced sleep deprivation hindering the execution of daily tasks, and circadian rhythms, which are critical for building healthy sleep, were not followed.
Developing health-promoting care for healthy or sick children by primarily using education for health and maximizing health potential is a field of action nurses specializing in pediatric health can safely and skillfully provide advanced care in, supporting the child and their family's needs.(55. Ordem dos Enfermeiros O. Regulamento de competências específicas do enfermeiro especialista em enfermagem de saúde infantil e pediátrica. Regulamento n.º 422/2018 [Internet]. 2018. Diário da República, 2.ª série, N.º 133, 12 de julho de 2018. [citado 2018 Nov 9]. Disponível em https://www.ordemenfermeiros.pt/media/8733/infantil.pdf.
https://www.ordemenfermeiros.pt/media/87...
)Because specialist nurses have roles that span the various settings experienced by children and their families, they can partner with families to promote the highest possible state of health and contribute to educating them and increasing health literacy.
Sleep is a biological need that affects the child's physical and psychomotor growth and development. It is figured in the Portuguese National Plan for Child and Youth Health (PNSIJ) as an anticipatory care topic in the setting of doctor's visits for youth ranging from 1-month-old infants to 18-year-old adolescents.(66. Direção Geral de Saúde. Programa Nacional de Saúde Infantil e Juvenil [Internet]. Lisboa: Direção Geral de Saúde; 2013 [citado 2018 Nov 9]. Disponível em https://www.dgs.pt/documentos-e-publicacoes/programa-tipo-de-atuacao-em-saude-infantil-e-juvenil.aspx
https://www.dgs.pt/documentos-e-publicac...
)This reveals the importance of addressing childhood sleep considering the principles of child-and-family-centered care.
Many parents report their children have difficulty sleeping.(22. Crispim JN, Boto LR, Melo IS, Ferreira R. Padrão de sono e factores de risco para privação de sono numa população pediátrica portuguesa. Acta Pediatr Port. 2011;42(3):93–8.,77. Maia Í, Pinto F. Hábitos de sono. Nascer e Crescer: Rev Hosp Crianças Maria Pia. 2008;17 (1):9–12.)Sleep issues are a common concern in doctor's visits and are not always taken seriously or considered as a part of infancy. These issues are largely due to a lack of education on the acquisition of sleep habits.(77. Maia Í, Pinto F. Hábitos de sono. Nascer e Crescer: Rev Hosp Crianças Maria Pia. 2008;17 (1):9–12.)Thus, knowing sleep education programs of different countries and their efficacy is critical for inspiring healthcare providers to stimulate the community to implement sleep programs as a means to promote healthy sleep in infants/children and adolescents.
For this reason, the present study aims at answering the following question using the PIO strategy:(88. Cunha PL, Cunha CS, Alves PF. Manual revisão bibliográfica sistemática integrativa: a pesquisa baseada em evidência. Belo Horizonte: Grupo Ãnima Educação; 2014 [citado 2018 Nov 9]. Disponível em https://docplayer.com.br/1122683-Revisao-bibliografica-sistematica-integrativa.html
https://docplayer.com.br/1122683-Revisao...
)what are the effects of sleep education programs on the sleep of infants, children, and adolescents (population, P), when applied? This question considers a population (P) of infants, children, adolescents, and their families; interventions (I) are sleep education programs; and the result (O) is the effects on sleep of children, adolescents, and their families. This study's objective is to identify the effects of sleep education programs reported in the literature on the sleep of infants, children, and adolescents.
Methods
Evidence-based practice is a critical decision-making tool in the care provision setting. It is supported by the best scientific results of primary studies and leads to an analytical and constructive reasoning of one's own practice.(99. Ferrito C. Enfermagem baseada na evidência: estudo piloto sobre necessidades de informação científica para a prática de enfermagem. Percursos. 2007; 3:36–40.)
Literature integrative review is a research technique that gathers and summarizes scientific knowledge available from research on a given theme.(1010. Souza MT, Silva MD, Carvalho R. Integrative review: what it is and how to do. einstein (Sao Paulo). 2010; 8(1):102-6.)Considering the scientific literature on health, this investigation process is essential for actualizing knowledge and putting it into operation in care settings, as well as in investigative settings.
This review was conducted based on the following steps: identifying an issue and structuring an initial question, defining a research and article selection strategy, assessing and analyzing studies, and producing an integrative synthesis. Two independent reviewers analyzed and assessed study quality using the Joana Briggs Institute (JBI) assessment grids based on study type. Studies meeting at least 60% of the JBI assessment grid items were included in the integrative review. In the face of disagreement, investigators met to reach a consensus on the inclusion or exclusion of the study in question.
Pubmed®and the EBSCOhost®research platform (CINAHL Complete , Cochrane Database of Systematic Reviews , MedicLatina, MEDLINE Complete, Nursing & Allied Health Collection: Comprehensive ) were the databases surveyed from October to November 2018. The following English health sciences descriptors (DeCS) were used: Child; Adolescent ; Sleep , and Education. Descriptors were correlated using the boolean operator “ and ” and the programme keyword. The following filters were used to limit our search: full-text articles published between 2013 and 2018 in Portuguese and English.
The established inclusion criteria were: scientific articles published on the aforementioned indexed databases with full text available in Portuguese or English for primary empiric quantitative studies published between 2013 and 2018. Studies meeting the inclusion criteria were chosen to be included in the integrative review based on a reading of titles and abstracts.
Results
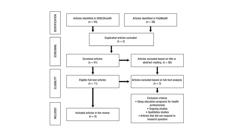
Our database survey with the selected health descriptors and filters identified 93 articles, 55 of which were found in the online research platform EBSCOhost®and 38 were found in Pubmed®. Two duplicated articles were then excluded, resulting in 91 articles. After reading titles, abstracts, and identifying answers to the study question, 80 articles were excluded, resulting in a corpus of 11 articles. Exclusion criteria were studies on the application of sleep education programs for healthcare providers, ongoing studies, qualitative studies, and theoretical articles that did not answer the starting question. We then proceeded to reading the 11 remaining articles in full and applying the inclusion and exclusion criteria to study objective, which allowed for the selection of 8 articles to integrate the review's final sample. Figure 1 shows the selection process steps as per the PRISMA ( Preferred Reporting Items for Systematic Reviews and Meta-Analyses) model/diagram principles(1111. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement. PLoS Med 6(7): e1000097.). It schematically shows the article selection strategy that led to our final sample.
Article selection to obtain the final sample using the PRISMA(1111. Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement. PLoS Med 6(7): e1000097.)flowchart
After selecting the articles, methodological quality was assessed by two independent reviewers. The Joanna Briggs Institute [JBI](1212. Joanna Briggs Institute - JBI [Internet]. Joannabriggs.org. 2017 [citado 2018 Nov 5]. Disponível em: https://joannabriggs.org/ebp/critical_appraisal_tools
https://joannabriggs.org/ebp/critical_ap...
)defines evidence-based care as viable, adequate, and effective care. To assess each study's methodological quality, the JBI(1212. Joanna Briggs Institute - JBI [Internet]. Joannabriggs.org. 2017 [citado 2018 Nov 5]. Disponível em: https://joannabriggs.org/ebp/critical_appraisal_tools
https://joannabriggs.org/ebp/critical_ap...
)standardized critical assessment instrument was applied based on study type. Studies showing at least 60% positive response to JBI items(1212. Joanna Briggs Institute - JBI [Internet]. Joannabriggs.org. 2017 [citado 2018 Nov 5]. Disponível em: https://joannabriggs.org/ebp/critical_appraisal_tools
https://joannabriggs.org/ebp/critical_ap...
)were included, i.e., eight articles remained.
Studies showed the following evidence levels as per the JBI tool(1212. Joanna Briggs Institute - JBI [Internet]. Joannabriggs.org. 2017 [citado 2018 Nov 5]. Disponível em: https://joannabriggs.org/ebp/critical_appraisal_tools
https://joannabriggs.org/ebp/critical_ap...
)were: 7 studies were level 1.c and 1 study was level 2.c. They were quantitative in nature, consisting mostly of pilot studies and randomized controlled trials.
Studies were conducted in six countries: New England (1 study); Canada (2 studies); Hong Kong (1 study); India (1 study), Japan (1 study), New Zealand (1 study), and United States of America (1 study).
All studies included pediatric age groups. Some studies focused on programs for children/adolescents and others on programs for parents of infants, which allowed the authors to acquire a balanced view on the theme.
The data serialization procedure was conducted using a chart created to aid in extracting relevant information from the analyzed studies. This table comprises the following items: article description (title, authors, year, and country); study objective; design and methodology; participants; and results/conclusions obtained by study authors. Results extracted from the studies are shown in Chart 1 .
Discussion
The selected articles show sleep education programs for infants, children, and adolescents may be a valid strategy to raise awareness in the community.
Adolescents began going to bed earlier on weekends, which increased their sleep duration, as evidenced in E1,(1313. Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015 Sep;1(3):197–204.)E2,(1414. Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787–92.)E3,(1515. John B, Bellipady SS, Bhat SU. Sleep Promotion Program for Improving Sleep Behaviors in Adolescents: A randomized controlled pilot study. Scientifica (Cairo). 2016; 2016:8013431.). This may consequently reveal an improvement in academic performance, as seen in studies E1,(1313. Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015 Sep;1(3):197–204.)and E6.(1818. Gruber R, Somerville G, Bergmame L, Fontil L, Paquin S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. 2016; 21:93–100.)
Studies E6(1818. Gruber R, Somerville G, Bergmame L, Fontil L, Paquin S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. 2016; 21:93–100.)and E7(1919. Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a Sleep Education Program for Low-Income Preschool Children and Their Families. Sleep. 2014; 37(6): 1117-25.)show that children's sleep duration increased on weekdays, and bedtimes were also earlier than usual. The adoption of sleep promoting behaviors in adolescents was seen in E5(1717. Tamura N, Tanaka H. Effects of a sleep education program with self-help treatment on sleeping patterns and daytime sleepiness in Japanese adolescents: A cluster randomized trial. Chronobiol Int. 2016;33(8):1073–85.), promoting a reduction in daily sleepiness. Regarding infants, E8(2020. Hall WA, Hutton E, Brant RF, Collet JP, Gregg K, Saunders R, et al. A randomized controlled trial of an intervention for infants' behavioral sleep problems. BMC Pediatr. 2015;15(181):181.)showed that after the application of the sleep education program, infants began awaking less during night sleep.
We highlight that E2,(1414. Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787–92.)E4(1616. Wing YK, Chan NY, Man Yu MW, Lam SP, Zhang J, Li SX, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics. 2015;135(3):e635–43.), and E7(1919. Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a Sleep Education Program for Low-Income Preschool Children and Their Families. Sleep. 2014; 37(6): 1117-25.)show the importance of maintaining the implemented programs to verify effective health gains on the long term. Study results showed that programs for children, their families, and the school setting may be successful in increasing sleep duration in students and improving sleep efficiency; cross-sectionally, one of the measures used in sleep education programs were sleep information sessions (E1;(1313. Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015 Sep;1(3):197–204.)E2;(1414. Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787–92.)E3;(1515. John B, Bellipady SS, Bhat SU. Sleep Promotion Program for Improving Sleep Behaviors in Adolescents: A randomized controlled pilot study. Scientifica (Cairo). 2016; 2016:8013431.)E4;(1616. Wing YK, Chan NY, Man Yu MW, Lam SP, Zhang J, Li SX, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics. 2015;135(3):e635–43.)E5;(1717. Tamura N, Tanaka H. Effects of a sleep education program with self-help treatment on sleeping patterns and daytime sleepiness in Japanese adolescents: A cluster randomized trial. Chronobiol Int. 2016;33(8):1073–85.)E6;(1818. Gruber R, Somerville G, Bergmame L, Fontil L, Paquin S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. 2016; 21:93–100.)E7;(1919. Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a Sleep Education Program for Low-Income Preschool Children and Their Families. Sleep. 2014; 37(6): 1117-25.)and E8).(2020. Hall WA, Hutton E, Brant RF, Collet JP, Gregg K, Saunders R, et al. A randomized controlled trial of an intervention for infants' behavioral sleep problems. BMC Pediatr. 2015;15(181):181.)
In E1,(1313. Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015 Sep;1(3):197–204.)sleep information sessions were conducted with study participants, and parents/caregivers also received information on the theme. Eight sessions were conducted to address the following topics: what is sleep; why is it important to sleep; healthy sleep habits; where and when to sleep; sleep/wakefulness cycles; routines; sleep patterns; sleep health; and the effects of caffeine. The study reports that adolescents tend to sleep less, which in turn causes daytime sleepiness. The study states that adolescents used caffeine and mobile devices near bedtime, which produced a delay in bedtimes. It also highlights that sleep education programs are a way to avoid sleep restriction, which subsequently improves sleep hygiene and adolescents' behavior. The study concurrently demonstrated the value in raising awareness about healthy sleep-related behavior.
In E2,(1414. Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787–92.)as in the previous study, in addition to study participants, parents and caregivers also received sleep information. Five in-class sessions were conducted and an individual sleep diary was kept. Sessions included topics such as: the effects of alcohol and drugs on sleep, depression/anxiety, and sleep. This study highlighted that many students reported poor sleep and showed high prevalence of daytime sleepiness. It showed that with the application of a sleep education program adolescents tended to increase weekend sleep, which influenced their sleep behavior positively.
In E3,(1515. John B, Bellipady SS, Bhat SU. Sleep Promotion Program for Improving Sleep Behaviors in Adolescents: A randomized controlled pilot study. Scientifica (Cairo). 2016; 2016:8013431.)a positive effect in overall sleep quality was shown, i.e., in sleep-onset latency, sleep duration, and daytime sleepiness. Over the course of a 2-week interval, the implemented program produced a positive effect on sleep duration in adolescents. Over the course of a 6-week interval, the program resulted in adolescents decreasing their daytime sleepiness. Additionally, teenagers also increased weekend sleep duration. The program was developed in five sessions that addressed topics such as: definition of sleep, functions of sleep, sleep stages, factors causing sleep deprivation, the impact of sleep problems, sleep complaints, circadian process, natural sleep shift, the relation between sleep and memory, how to establish good sleep hygiene practices, and training and visualization for stress reduction and relaxation. Adolescents were encouraged to practice techniques learned in class before going to bed.
In E4,(1616. Wing YK, Chan NY, Man Yu MW, Lam SP, Zhang J, Li SX, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics. 2015;135(3):e635–43.)in addition to study participants, parents and caregivers also received sleep information. The study program was developed based on a town hall seminar (introduction of the program together with a general understanding of sleep medicine; it also provided tips for better sleep hygiene practices.) and two small class workshops (characterized by interactive small group discussions and case studies). Additionally, a set of structured educational materials was developed covering: the importance of sleep; the consequences of sleep deprivation; factors contributing to insufficient sleep; and good sleep practices. Students were also asked to chart a sleep diary. Study authors highlight the significance of the dissemination of relevant information on the importance of adequate sleep among schools, families, and society. They report the need for further studies with a longer follow-up to evaluate effective changes in sleep behavior. Further studies are also needed to promote motivation among students to change sleep behavior. The study concludes that schools and education authorities should consider incorporating an introductory sleep education component into their regular school curriculum to equip teachers and students with essential sleep knowledge.
In E5,(1717. Tamura N, Tanaka H. Effects of a sleep education program with self-help treatment on sleeping patterns and daytime sleepiness in Japanese adolescents: A cluster randomized trial. Chronobiol Int. 2016;33(8):1073–85.)similarly to E4, authors report the study was unable to examine the maintenance effect due to lack of follow-up data. Furthermore, the complex approach of the study made it difficult to identify which specific aspects of the intervention accounted for the changes observed. Despite these limitations, positive changes in habits benefiting sleep promotion were seen; that is, getting up at a fixed time every morning, avoiding taking a nap at the end of the day, avoiding stimulating beverages after dinner. The study reports using the sleep education program and an adjunctive self-help treatment program was effective not only for increasing sleep knowledge but also for improving sleep-promoting behaviors and sleep patterns/reducing daytime sleepiness.
This was a school-based program, and students were administered a sleep knowledge test before and after the intervention. Students were provided with in-class information on proper sleep health and sleep-promoting behaviors. Following sleep education, students were asked to assess their own sleeping patterns, daytime functioning, and sleep-promoting behaviors. Students were then asked to select and practice one sleep-promoting behavior and monitor their progress using sleep diaries.
E6(1818. Gruber R, Somerville G, Bergmame L, Fontil L, Paquin S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. 2016; 21:93–100.)sought to promote good sleep habits and extend sleep durations among children. Sleep deprivation in children is likely to be caused by lifestyle habits. Additionally, school-age children are more receptive to guidance from adult figures. The study shows that many school-age children obtain insufficient sleep, and that this has an impact on daytime performance. The study further demonstrates that small, cumulative improvements in sleep can have detectable effects on the learning capacity and performance of school-age children, thereby supporting the introduction of sleep curricula into schools.
The program was implemented in schools based on for modules: Sleep Knowledge and Education (which empowered students to make healthier choices); Family and Community Involvement (which encouraged parents and children to discuss sleep in the context of a balanced lifestyle); Sleep Promotion for Staff (which empowered staff); and Sleep-friendly School Environment (which encouraged school principals to assess their school's policies, curricula, workload, and activity schedules in order to identify modifiable factors that could be targeted in order to support student's healthy sleep).
In E7,(1919. Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a Sleep Education Program for Low-Income Preschool Children and Their Families. Sleep. 2014; 37(6): 1117-25.)the sleep education program was designed to be an at school and at home intervention, based on educating preschool children, parents, and teachers. Parents and teachers received instruction on sleep to enable parents to follow the recommended routines at home. Families received a parent instruction guide including bedtime routines and sleep articles. Through lessons taught by the classroom teacher students gained an understanding of healthy sleep habits and how to follow a bedtime routine. Children received a teddy bear to mimic a bedtime routine, a reading book, a blanket, a toothbrush, and a toothpaste in order for them to incorporate these objects into their night sleep routine. A bedtime routine chart, complete with stickers, was given to children to provide incentive to follow the bedtime routine steps at home. This study did not limit its intervention to conducting education sessions on the child's sleep, it also provided materials for implementing a consistent routine.
In E8,(2020. Hall WA, Hutton E, Brant RF, Collet JP, Gregg K, Saunders R, et al. A randomized controlled trial of an intervention for infants' behavioral sleep problems. BMC Pediatr. 2015;15(181):181.)implementing the sleep education program for parents of infants resulted in fewer night wakes and an improvement in parent fatigue and sleep quality. Additionally, it also improved parents' knowledge about sleep, infant feeding at night, and managing of infants' sleep. These positive effects on infant and parent sleep led to an improvement in family dynamic. The study's literature review found that behavioral sleep problems affect 20-30% of infants and often persist in later childhood. This percentage is often related with fragmented sleep and/or short sleep duration in infants. Thus, implementing sleep education programs at an early age may constitute a valuable intervention.
The program consisted of teaching sessions addressing information about infants' patterns; negative sleep associations; unrealistic expectations about sleep; effects of sleep loss on infants and parents; and strategies to reduce night waking. Additionally, participants also received telephone calls for reinforcement of concepts and support.
This study's results support the Portuguese Pediatric Society's 2017 recommendations(2121. Sociedade Portuguesa de Pediatria (SPP). Recomendações SPS-SPP prática da sesta da criança nas creches e infantários, públicos ou privados [Internet]. Lisboa: SPP ;2017 [citado 2018 Nov 17]. Disponível em http://criancaefamilia.spp.pt/media/125327/VERSAO-EDUCADORES-E-PAIS_RECOMENDACOES-SPS-SPP-SESTA-NA-CRIANCA.pdf.
http://criancaefamilia.spp.pt/media/1253...
)on the practice of napping in nurseries or day care facilities to standardize and promote sleep. Results also highlight the need to promote sleep in children together with their families, for which doctor's visits may constitute a privileged setting for action.
Conclusion
Youth sleep is a pressing theme. The fact that our environment and social life may negatively affect sleep has started to be duly appreciated. All of society's demands for parents, children, and adolescents disregard human circadian rhythms and attempt to reprogram Man's circadian rhythms, which significantly affects sleep quantity and quality. We conclude this review has met its objective, namely verifying the effects of applying sleep education programs on the sleep of infants, children, and adolescents by analyzing and describing the included studies. Given the results of the studies, sleep education programs can be considered an effective intervention on the sleep of children and adolescents and can be valued as a sleep health promotion strategy for children. In addition to the possibility afforded by these programs of affecting the community and primary health and care, hospitals may also be considered privileged sites for action if sleep programs are duly adapted and instituted. The authors highlight the need to develop further studies and raise awareness among nurses on the relevance of acquiring sleep knowledge, so that effective interventions may be established covering School Health and nursing visits for monitoring child health (as shown in the sleep programs). In conclusion, sleep must be seen as a health-determining factor in children and adolescents. It is paramount to encourage healthcare providers to develop sleep education programs to prevent potential health issues.
Acknowledgment
We acknowledge the Polytechnic Institute of Viseu for the funding received for this submission.
Referências
-
1Silva FG, Silva CR, Braga LB, Serrão Neto AS. [Hábitos e problemas do sono dos dois anos aos dez anos: estudo populacional]. Acta Pediatr Port. 2013;44(5):196–202.
-
2Crispim JN, Boto LR, Melo IS, Ferreira R. Padrão de sono e factores de risco para privação de sono numa população pediátrica portuguesa. Acta Pediatr Port. 2011;42(3):93–8.
-
3Silva EM, Simões PA, Macedo MC, Duarte JC, Silva DM. Perceção parental sobre hábitos e qualidade do sono das crianças em idade pré-escolar. Rev Enferm Ref. 2018;4(17):63–72.
-
4Pinto TR, Pinto JC, Rebelo-Pinto H, Paiva T. O sono em adolescentes portugueses: proposta de um modelo tridimensional. Anal Psicol. 2016;4(34):339–52.
-
5Ordem dos Enfermeiros O. Regulamento de competências específicas do enfermeiro especialista em enfermagem de saúde infantil e pediátrica. Regulamento n.º 422/2018 [Internet]. 2018. Diário da República, 2.ª série, N.º 133, 12 de julho de 2018. [citado 2018 Nov 9]. Disponível em https://www.ordemenfermeiros.pt/media/8733/infantil.pdf
» https://www.ordemenfermeiros.pt/media/8733/infantil.pdf -
6Direção Geral de Saúde. Programa Nacional de Saúde Infantil e Juvenil [Internet]. Lisboa: Direção Geral de Saúde; 2013 [citado 2018 Nov 9]. Disponível em https://www.dgs.pt/documentos-e-publicacoes/programa-tipo-de-atuacao-em-saude-infantil-e-juvenil.aspx
» https://www.dgs.pt/documentos-e-publicacoes/programa-tipo-de-atuacao-em-saude-infantil-e-juvenil.aspx -
7Maia Í, Pinto F. Hábitos de sono. Nascer e Crescer: Rev Hosp Crianças Maria Pia. 2008;17 (1):9–12.
-
8Cunha PL, Cunha CS, Alves PF. Manual revisão bibliográfica sistemática integrativa: a pesquisa baseada em evidência. Belo Horizonte: Grupo Ãnima Educação; 2014 [citado 2018 Nov 9]. Disponível em https://docplayer.com.br/1122683-Revisao-bibliografica-sistematica-integrativa.html
» https://docplayer.com.br/1122683-Revisao-bibliografica-sistematica-integrativa.html -
9Ferrito C. Enfermagem baseada na evidência: estudo piloto sobre necessidades de informação científica para a prática de enfermagem. Percursos. 2007; 3:36–40.
-
10Souza MT, Silva MD, Carvalho R. Integrative review: what it is and how to do. einstein (Sao Paulo). 2010; 8(1):102-6.
-
11Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group (2009). Preferred Reporting Items for Systematic Reviews and MetaAnalyses: The PRISMA Statement. PLoS Med 6(7): e1000097.
-
12Joanna Briggs Institute - JBI [Internet]. Joannabriggs.org. 2017 [citado 2018 Nov 5]. Disponível em: https://joannabriggs.org/ebp/critical_appraisal_tools
» https://joannabriggs.org/ebp/critical_appraisal_tools -
13Wolfson AR, Harkins E, Johnson M, Marco C. Effects of the Young Adolescent Sleep Smart Program on sleep hygiene practices, sleep health efficacy, and behavioral well-being. Sleep Health. 2015 Sep;1(3):197–204.
-
14Kira G, Maddison R, Hull M, Blunden S, Olds T. Sleep education improves the sleep duration of adolescents: a randomized controlled pilot study. J Clin Sleep Med. 2014;10(7):787–92.
-
15John B, Bellipady SS, Bhat SU. Sleep Promotion Program for Improving Sleep Behaviors in Adolescents: A randomized controlled pilot study. Scientifica (Cairo). 2016; 2016:8013431.
-
16Wing YK, Chan NY, Man Yu MW, Lam SP, Zhang J, Li SX, et al. A school-based sleep education program for adolescents: a cluster randomized trial. Pediatrics. 2015;135(3):e635–43.
-
17Tamura N, Tanaka H. Effects of a sleep education program with self-help treatment on sleeping patterns and daytime sleepiness in Japanese adolescents: A cluster randomized trial. Chronobiol Int. 2016;33(8):1073–85.
-
18Gruber R, Somerville G, Bergmame L, Fontil L, Paquin S. School-based sleep education program improves sleep and academic performance of school-age children. Sleep Med. 2016; 21:93–100.
-
19Wilson KE, Miller AL, Bonuck K, Lumeng JC, Chervin RD. Evaluation of a Sleep Education Program for Low-Income Preschool Children and Their Families. Sleep. 2014; 37(6): 1117-25.
-
20Hall WA, Hutton E, Brant RF, Collet JP, Gregg K, Saunders R, et al. A randomized controlled trial of an intervention for infants' behavioral sleep problems. BMC Pediatr. 2015;15(181):181.
-
21Sociedade Portuguesa de Pediatria (SPP). Recomendações SPS-SPP prática da sesta da criança nas creches e infantários, públicos ou privados [Internet]. Lisboa: SPP ;2017 [citado 2018 Nov 17]. Disponível em http://criancaefamilia.spp.pt/media/125327/VERSAO-EDUCADORES-E-PAIS_RECOMENDACOES-SPS-SPP-SESTA-NA-CRIANCA.pdf
» http://criancaefamilia.spp.pt/media/125327/VERSAO-EDUCADORES-E-PAIS_RECOMENDACOES-SPS-SPP-SESTA-NA-CRIANCA.pdf
Publication Dates
-
Publication in this collection
14 Dec 2020 -
Date of issue
2020
History
-
Received
22 July 2019 -
Accepted
06 Mar 2020