Abstracts
OBJECTIVE: To examine the reliability of the SF-36 general health questionnaire when used to evaluate the health status of critically ill patients before admission to intensive care and to measure their health-related quality of life prior to admission and its relation to severity of illness and length of stay in the intensive care unit. METHODS: Prospective cohort study conducted in the intensive care unit of a public teaching hospital. Over three months, communicative and oriented patients were interviewed within the first 72 hours of intensive care unit admission; 91 individuals participated. The APACHE II score was used to assess severity of illness, and the SF-36 questionnaire was used to measure health-related quality of life. RESULTS: The reliability of SF-36 was verified in all dimensions using Cronbach's alpha coefficient. In six dimensions of eight domains the value exceeded 0.70. The average SF-36 scores of the health-related quality of life dimensions for the patients before admission to intensive care unit were 57.8 for physical functioning, 32.4 for role-physical, 53.0 for bodily pain, 63.2 for general health, 50.6 for vitality, 56.2 for social functioning, 54.6 for role-emotional and 60.3 for mental health. The correlations between severity of illness and length of stay and the health-related quality of life scores were very low, ranging from -0.152 to 0.175 and -0.158 to 0.152, respectively, which were not statistically significant. CONCLUSION: In the sample studied, the SF-36 demonstrated good reliability when used to measure health-related quality of life in critically ill patients before admission to the intensive care unit. The worst score was role-physical and the best was general health. Health-related quality of life of patients before admission was not correlated with severity of illness or length of stay in the intensive care unit.
Quality of life; Intensive care units; Outcomes and process assessment (Health Care)
OBJETIVO: Avaliar a confiabilidade do SF-36 para pacientes graves no período anterior à admissão em unidade de terapia intensiva e mensurar a qualidade de vida relacionada à saúde prévia e sua relação com a gravidade da doença e o tempo de permanência em unidade de terapia intensiva. MÉTODOS: Estudo de coorte prospectivo realizado em unidades de terapia intensiva de um hospital escola público. Foram entrevistados 91 pacientes comunicativos e orientados nas primeiras 72 horas de admissão nas unidades de terapia intensiva durante 3 meses. O escore APACHE II foi utilizado para avaliar a gravidade da doença e o questionário SF-36 para avaliar a qualidade de vida relacionada à saúde. RESULTADOS: A confiabilidade do SF-36 foi avaliada em todas as dimensões por meio do coeficiente alfa de Cronbach. Em seis, de oito dimensões, o valor excedeu 0,70. As médias dos escores do SF-36 para pacientes críticos referentes ao período anterior à admissão em unidades de terapia intensiva foram: 57,8 para capacidade funcional; 32,4 para aspectos físicos; 53,0 para dor; 63,2 para estado geral de saúde; 50,6 para vitalidade; 56,2 para aspectos sociais; 54,6 para aspectos emocionais e 60,3 para saúde mental. As correlações entre gravidade da doença, tempo de permanência e escores da qualidade de vida relacionada à saúde foram muito baixas, variando de -0,152 a 0,175 e -0,158 a 0,152, respectivamente. CONCLUSÃO : O SF-36 demonstrou boa confiabilidade quando utilizado para medir qualidade de vida relacionada à saúde em pacientes críticos antes da admissão em unidade de terapia intensiva. O domínio com maior comprometimento prévio foi aspectos físicos e o melhor foi o estado geral de saúde. A qualidade de vida relacionada à saúde prévia dos pacientes não se correlacionou com a gravidade da doença e o tempo de permanência em unidade de terapia intensiva.
Qualidade de vida; Unidades de terapia intensiva; Avaliação de resultados (Cuidados de Saúde)
ORIGINAL ARTICLE
Quality of life before admission to the intensive care unit
Nathalia Perazzo TereranI; Suely Sueko Viski ZaneiII; Iveth Yamaguchi WhitakerII
IHospital Universitário, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP), Brazil
IIEscola Paulista de Enfermagem, Universidade Federal de São Paulo - UNIFESP - São Paulo (SP), Brazil
Corresponding author
ABSTRACT
OBJECTIVE: To examine the reliability of the SF-36 general health questionnaire when used to evaluate the health status of critically ill patients before admission to intensive care and to measure their health-related quality of life prior to admission and its relation to severity of illness and length of stay in the intensive care unit.
METHODS: Prospective cohort study conducted in the intensive care unit of a public teaching hospital. Over three months, communicative and oriented patients were interviewed within the first 72 hours of intensive care unit admission; 91 individuals participated. The APACHE II score was used to assess severity of illness, and the SF-36 questionnaire was used to measure health-related quality of life.
RESULTS: The reliability of SF-36 was verified in all dimensions using Cronbach's alpha coefficient. In six dimensions of eight domains the value exceeded 0.70. The average SF-36 scores of the health-related quality of life dimensions for the patients before admission to intensive care unit were 57.8 for physical functioning, 32.4 for role-physical, 53.0 for bodily pain, 63.2 for general health, 50.6 for vitality, 56.2 for social functioning, 54.6 for role-emotional and 60.3 for mental health. The correlations between severity of illness and length of stay and the health-related quality of life scores were very low, ranging from -0.152 to 0.175 and -0.158 to 0.152, respectively, which were not statistically significant.
CONCLUSION: In the sample studied, the SF-36 demonstrated good reliability when used to measure health-related quality of life in critically ill patients before admission to the intensive care unit. The worst score was role-physical and the best was general health. Health-related quality of life of patients before admission was not correlated with severity of illness or length of stay in the intensive care unit.
Keywords: Quality of life; Intensive care units; Outcomes and process assessment (Health Care)
INTRODUCTION
The conduct of intensive care medicine is often complex and requires the expenditure of substantial technological and financial resources. Generally, the more severe the patient's illness is, the greater the financial cost and length of stay in the intensive care unit (ICU) are, and the greater the requirement for equipment used for diagnosis and treatment. Despite these endeavors the outcome is not always the one hoped for, which explains why cost-effectiveness studies are being undertaken.(1-3) In this context, different aspects of outcome need to be evaluated, such as ethical and economic considerations along with quality of life (QOL).
Studies examining QOL are important because they can help professionals make decisions, identify and define priorities related to the patient's problems, compare diseases and evaluate the effectiveness of treatments. For patients and their families, the information gained from QOL studies helps them to choose the most appropriate treatment.(4,5)
The concept of QOL is multidimensional and quite broad, consisting of several aspects of life. When the term is used in reference to health care the expression adopted is health-related quality of life (HRQOL), which refers to the level of wellbeing and satisfaction in an individual's life and how, from the patient's perspective, it is affected by disease, accidents and treatments.(6)
Most studies analyze the patient's condition after discharge from the ICU;(7-11) few have evaluated HRQOL before admission. Studies that evaluate the QOL or HRQOL of the patient before admission can yield information that will improve healthcare providers' understanding of the profile of their patient population, assist decision making about specific actions and guide health organizations' policymaking.(4,12)
Studies on QOL or HRQOL in critically ill patients in Brazil are still scarce, and there has not been any research regarding previous QOL/HRQOL with intensive care outcomes (severity, length of stay, discharge or death in the ICU and hospital).
The aims of this study were to evaluate the reliability of the Short Form Health Survey (SF-36) questionnaire for general health and well-being when applied to critically ill patients and to measure their pre-admission HRQOL and its relation to the severity of illness and length of stay in the ICU.
METHODS
Approval for this prospective study was obtained from the Research Ethics Committee at the Universidade Federal de São Paulo (UNIFESP), São Paulo (SP), Brazil (CEP nº 0828/04). Data were obtained from adult medical and surgical patients in the four ICUs of São Paulo Hospital: a respiratory ICU (six beds); an anesthesiology ICU (16 beds); a cardiology ICU (eight beds) and a general ICU (seven beds).
The inclusion criteria were alert and orientated patients 18 years of age or older, who resided in the ICU for more than 24 hours with the ability to communicate and provided written informed consent to participate. Patients were excluded if they were intubated or underwent a tracheotomy, unconscious or sedated, unable to understand Portuguese or declined to participate in the study.
One of the researchers interviewed all patients who complied with the inclusion criteria within the first 72 hours of admission. No attempt was made to influence or bias the patient's responses to the questionnaire.
Demographic and clinical data were collected on all eligible patients. This included: age; gender; length of ICU stay; origin; admission diagnoses; severity of illness by Acute Physiology, Age and Chronic Health Evaluation II (APACHE II) score and whether the patient was discharged from the ICU or died.
The validated Portuguese translation of the original SF-36 was used to measure HRQOL.(13) This instrument contains 36 questions that evaluate eight multi-item domains or dimensions, all related to health: physical functioning; role-physical; bodily pain; social functioning; general health; vitality; role-emotional and mental health. Answers to the 36 items were transformed and weighted according to earlier recommendations, and subsequent scoring was performed according to predefined guidelines. Scores for each domain range from zero (worst possible health state) to 100 (best possible health state). The dimensions can be classified in two sub-groups: physical health and mental health.(14)
Given that general health status differs over time (the recall period), the original version of the SF-36 questionnaire used four weeks as the optimum recall period for QOL measurement.(14) To concur with this, we asked the participants to recall their experiences and feelings in the previous four weeks when answering the questions, which was considered adequate to reflect the basal state of health and HRQOL before ICU admission.
Descriptive statistics and frequencies were calculated when indicated. Cronbach's alpha coefficient was calculated to evaluate the internal reliability of the component questions of each of the eight dimensions in this sample. A Cronbach's alpha coefficient >0.7 was considered to demonstrate acceptable reliability.(15) Spearman's correlation coefficient was calculated to examine the relationship between the severity of illness and ICU length of stay. All statistical analyses were performed using Statistical Package for the Social Sciences (SPSS) software (SPSS) version 13 (Chicago, Illinois, USA), with p<0.05 regarded as statistically significant.
RESULTS
From August to November 2004, 373 patients were admitted to the ICUs. Of these, 91 patients met the inclusion criteria. Forty-four (48.3%) were patients on the coronary unit, 26 (28.6%) on the anesthesiology ICU, 8 (8.8%) on the general ICU and 13 (14.3%) in the respiratory ICU.
The mean age of patients of the sample was 55.8 years (standard deviation, SD±16). Fifty patients (54.9%) were male. Thirty-nine (42.9%) were admitted from the emergency room. The majority of patients (59.3%) were medical. Most patients had more than one chronic disease, most commonly arterial hypertension and diabetes mellitus.
The causes of admission to the ICU were cardiovascular dysfunction (47.2%) and elective surgery (38.5%). The mean ICU length of stay was 4.3 days (SD±6.6). The mean APACHE II score was 10.2 (SD±4.2). Only three patients (3.3%) died in the ICU. The demographic and clinical characteristics are shown in table 1.
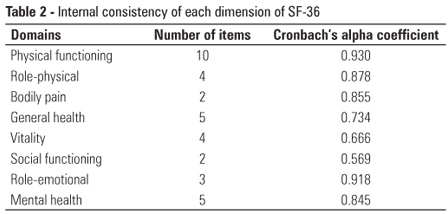
The reliability of the SF-36 was verified in all dimensions through the internal consistency test (Cronbach's alpha coefficient). In six dimensions the value exceeded 0.70. Only the "vitality" and "social functioning" dimensions did not exceed this level, with Cronbach's alpha corresponding to 0.666 and 0.569, respectively (Table 2).
To compare means between all variables in this study and the SF-36 dimensions, the average scores of the dimensions were calculated, taking into account the total number of participants. The SF-36 scores for the medical and surgical patients were evaluated separately and compared with reference to each of the dimensions. Using the t test for non-related samples, the results did not allow us to draw any conclusions about potential differences in HRQOL between medical and surgical patients (Table 3).
The mean APACHE score was 10.2 (SD±4.2). The mean ICU stay was 4.3 days (SD±6.6). The correlation between the severity of illness and the scores of HRQOL dimensions ranged from -0.152 to 0.175, and the correlation between ICU length of stay and the scores of HRQOL dimensions ranged from -0.158 to -0.152, which were not statistically significant (p>0.05).
Regarding conditions when leaving the ICU, 88 (96.7%) of the patients were discharged to wards and three (3.0%) died while staying in the ICU. As the number of deaths was low, we did not explore a potential relationship between HRQOL domains and discharge conditions because of the strong possibility of inaccurate results.
DISCUSSION
The main goals of this study were to evaluate the pre-admission HRQOL of medical or surgical patients in the ICU, and verify whether there was an association between HRQOL and the other variables often used to evaluate intensive care outcomes, such as the severity of illness and length of ICU stay.
In relation to the reliability of SF-36, the values obtained through the internal consistency test (Cronbach's alpha) confirmed that the instrument is satisfactory when applied to critically ill patients. In six dimensions, the coefficient exceeded 0.70, and the average for all dimensions was 0.799.
The patients participating in our study had an average APACHE II score of 10.2 (SD±4.2), which is lower than the average of between 18 and 22 that was reported in other studies.(11,16) The patients in this study had a relatively low severity index, most likely due to better clinical conditions. This could also explain the low mortality (3.3%) found in our study, and because the patients were conscious and able to communicate, they were most likely less ill and a positive clinical outcome was more likely.
The length of stay in ICUs varies considerably, depending on how ill the patients are. In Brazil, despite the large variability, the average is approximately 6 days,(17) and in this sample, it was 4.3 days (SD±6.6), possibly because the participants were not severely ill.
The average HRQOL scores in this study are similar to the average reported by patients with chronic obstructive pulmonary disease or systemic arterial hypertension, except for the "general state of health" and "vitality". These were higher in our cohort, and similar to the average of normal American individuals.(15)
One study has analyzed the QOL of 199 medical (68.0%) and surgical (32.0%) patients with a mean APACHE II score of 12.5 (SD±0.41).(18) When compared with our results, it is evident that our participants reported lower mean scores in the "role-physical", "pain", "role-emotional", "mental health" and "social functioning" dimensions. In "physical functioning", the means were similar, but were higher in "vitality" and "general health".
The SF-36 has been used to assess patients admitted to the ICU predominantly for cardiovascular and pulmonary disorders in order to compare the pre-ICU status in the short (1 month after ICU stay) and long term (9 months after ICU stay). The domain scores pre-ICU were: physical functioning 43.5 (SD±31.0), role-physical 32.0 (SD±43.8), bodily pain 47.6 (SD±36.5), general health 49.6 (SD±20.1), vitality 42.1 (SD±24.3), social functioning 72.1 (SD±29.1), role-emotional 60.3 (SD±46.8) and mental health 58.4 (SD±24.5).(19) These data are very similar to ours. These results suggest that the HRQOL before intensive care is generally poor in the physical health dimensions (physical functioning, role physical, bodily pain, general health and vitality), although in this study the dimensions included in mental health were also lower (scores<60.3).
Another retrospective assessment of quality of life before ICU hospitalization using the SF-36 revealed that patients with acute lung injury reported HRQOL scores that were consistently lower than population norms ("general health" and "vitality" were 56.4, and "role-emotional" was 75.6). In our study, the mean scores in the domains general health were 63.2, vitality 50.6 and role-emotional 54.6.(20)
QOL before ICU admission has also been assessed by means of a specific questionnaire for critically ill patients, as applied to 187 patients. Only 28% of patients had a normal QOL, 38% had mild deterioration, 21% had moderate deterioration, 10% had major deterioration and 3% had severe limitation of QOL. The authors found that pre-admission QOL correlates with age and severity of illness, and those who died while staying in the ICU or hospital showed worse QOL scores before being admitted to the ICU. In addition, they comment that pre-admission QOL assessment is important and should be incorporated in clinical practice.(21)
In contrast, our findings do not show these outcomes. However, there are limitations to our study, including the small sample size (91 participants) and participants with low APACHE scores that contributed to shorter hospital stays and lower mortality. Generalizing these findings to all ICU admissions may be misleading because our results were limited to a single institution.
Despite these limitations the most important aspect of our study was the inclusion of only conscious and communicative patients. This criterion was used based on the premise adopted by experts in the subject, who emphasize the importance of questions being answered by the patients themselves, considering that QOL/HRQOL assessment entails many subjective concepts.(22) Thus, the possibility of a member of the family or the next of kin answering questions on the patient's behalf if the patient were unable to communicate was not considered. This decision excluded the vast majority of patients and selected those who most likely had less severe illnesses.
This study raised several issues that should be considered in studies examining the HRQOL of critically ill patients or other individuals unable to express themselves verbally or in writing. How can the mainly subjective aspects of HRQOL be measured in a patient who cannot communicate? Would the use of substitutes (proxy responses) be a reliable and valid alternative? If so, could the results be interpreted in the same way? Would they be equivalent, valid and reliable?
Many authors of studies that have examined levels of agreement between patients and their proxies have discussed the role of the substitute or replacement when the patient is unable to respond. The concerns expressed are consistent and justified, as using a substitute in place of the patient breaks the fundamental principle of the concept of QOL, namely the perception of the individual aspects of your own life, and naturally, the individual himself is the only one who can know these. However, most also agree that studies that have excluded people who for some reason were unable to communicate result in erroneous conclusions.(23-25) Additionally, there are studies that have reported variable levels of agreement between patient and proxy estimates of baseline QOL in ICU survivors.(26,27) In general, proxies underestimated the patient's quality of life, although the differences were small.(23,27)
In any QOL/HRQOL study involving critically patients in ICUs, the likelihood of excluding a large proportion of patients who are unable to communicate is an unavoidable fact. This should not diminish the importance of QOL before ICU admission as an issue for physicians, nurses and other healthcare professionals involved in the patient's treatment. Being mindful of the expected QOL at discharge can assist in determining the appropriateness and value of additional interventions or further treatment.(21,20,27) Thus, alternative means should be explored to assist in this endeavor. It is important to assure the reliability and validity of the instruments used in the study of critically ill patients or their proxies (usually relatives), as well as strategies that assure reliable outcomes. Larger studies should be conducted that take these considerations into account.
CONCLUSION
The SF-36 questionnaire was found to be internally consistent and reliable in six dimensions for critically ill patients. The average scores of the HRQOL dimensions prior to admission varied from 32.4 (role-physical) to 63.2 (general health). These results suggest that the HRQOL of patients in our study sample before ICU admission is relatively low in all dimensions because 100 is the maximum. However, the pre-admission HRQOL of patients was weakly correlated with the severity of illness and length of stay in the ICU. These findings can be explained by limitations in our study's sample size and design; however, the reliability data suggest that the SF-36 is a powerful tool to evaluate the HRQOL of ICU patients.
REFERENCES
- 1. Ridley S, Biggam M, Stone P. A cost-utility analysis of intensive therapy. II: Quality of life in survivors. Anaesthesia. 1994;49(3):192-6.
- 2. Chelluri L, Grenvick A, Silverman M. Intensive care for critical ill elderly: mortality, costs, and quality of life. Review of the literature. Arch Intern Med. 1995;155(10):1013-22.
- 3. Nyman DJ, Sprung CL. End-of-life decision making in the intensive care unit. Intensive Care Med. 2000;26(10):1414-20.
- 4. Higginson IJ, Carr AJ. Measuring quality of life: Using quality of life measures in the clinical setting. BMJ. 2001;322(7297):1297-300.
- 5. Guyatt GH, Feeny DH, Patrick DL. Measuring health-related quality of life. Ann Intern Med. 1993;118(8):622-9.
- 6. Fitzpatrick R, Davey C, Buxton MJ, Jones DR. Evaluating patient-based outcome measures for use in clinical trials. Health Technol Assess. 1998;2(14):i-iv, 1-74. Available in: http://www.ncchta.org/fullmono/mon214.pdf
- 7. Soran A, Chelluri L, Lee KK, Tisherman SA. Outcome and quality of life of patients with acute pancreatitis requiring intensive care. J Surg Res. 2000;91(1):89-94.
- 8. Schelling G, Stoll C, Vogelmeier C, Hummel T, Behr J, Kapfhammer HP, et al. Pulmonary function and health-related quality of life in a sample of long-term survivors of the acute respiratory distress syndrome. Intensive Care Med. 2000;26(9):1304-11.
- 9. Herrige MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS; Canadian Critical Care Trials Group. One-year in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683-93.
- 10. Chelluri L, Im KA, Belle SH, Schulz R, Rotondi AJ, Donahoe MP, et al. Long-term mortality and quality of life after prolonged mechanical ventilation. Crit Care Med. 2004;32(1):61-9.
- 11. Wehler M, Geise A, Hadzionerovic D, Aljukic E, Reulbach U, Hahn EG, et al. Health-related quality of life of patients with multiple organ dysfunction: individual changes and comparison with normative population. Crit Care Med. 2003;31(4):1094-101.
- 12. Rivera Fernández R, Sánchez-Cruz JJ, Abizanda-Campos R, Vázquez-Mata G. Quality of life before intensive care unit admission and its influence on resource utilization and mortality rate. Crit Care Med. 2001;29(9):1701-9.
- 13. Ciconelli RM, Ferraz MB, Santos W, Meinão I, Quaresma MR. Tradução para a língua portuguesa e validação do questionário genérico de avaliação de qualidade de vida SF-36 (Brasil SF-36). Rev Bras Reumatol. 1999;39(3):143-50.
- 14. Ware JE Jr, Kosinski M, Bayliss MS, McHorney CA, Rogers WH, Raczek A. Comparison of methods for the scoring and statistical analysis of SF-36 health profile and summary measures: summary of results from the Medical Outcomes Study. Med Care. 1995;33(4 Suppl):AS264-79.
- 15. Lohr KN, Aaronson NK, Alonso J, Burnam MA, Patrick DL, Perrin EB, et al. Evaluating quality-of-life and health status instruments: development of scientific review criteria. Clin Ther. 1996;18(5):979-92.
- 16. Schelling G, Stoll C, Haller M, Briegel J, Manert W, Hummel T, et al. Health-related quality of life and posttraumatic stress disorder in survivors of the acute respiratory distress syndrome. Crit Care Med. 1998;26(4):651-9.
-
17Associação de Medicina Intensiva Brasileira - AMIB. 2º Censo Brasileiro de UTIs, 2002/2003. São Paulo: AMIB; 2002-2003.
- 18. Welsh CH, Thompson K, Long-Krug S. Evaluation of patient-perceived health status using the Medical Outcomes Survey Short-Form 36 in an intensive care unit population. Crit Care Med. 1999;27(8):1466-71.
- 19. Graf J, Koch M, Dujardin R, Kersten A, Janssens U. Health-related quality of life before, 1 month after, and 9 months after intensive care in medical cardiovascular and pulmonary patients. Crit Care Med. 2003;31(8):2163-9.
- 20. Gifford JM, Husain N, Dinglas VD, Colantuoni E, Needham DM. Baseline quality of life before intensive care: a comparison of patient versus proxy responses. Crit Care Med. 2010;38(3):855-60.
- 21. Abelha FJ, Santos CC, Barros H. Quality of life before surgical ICU admission. BMC Surg. 2007;7:23.
- 22. Pickard AS, Knight SJ. Proxy evaluation of health-related quality of life: a conceptual framework for understanding multiple proxy perspectives. Med Care. 2005;43(5):493-9.
- 23. Hofhuis J, Hautvast JL, Schrijvers AJ, Bakker J. Quality of life on admission to the intensive care: can we query the relatives? Intensive Care Med. 2003;29(6):974-9.
- 24. Weinfurt KP, Trucco SM, Willke RJ, Schulman KA. Measuring agreement between patient and proxy responses to multidimensional health-related quality-of-life measures in clinical trials. An application of psychometric profile analysis. J Clin Epidemiol. 2002;55(6):608-18.
- 25. von Essen L. Proxy ratings of patient quality of life--factors related to patient-proxy agreement. Acta Oncol. 2004;43(3):229-34
- 26. Addington- Hall J, Kalra L. Who should measure quality of life? BMJ. 2001;322(7299):1417-20.
- 27. Oeyen SG, Vandijck DD, Benoit DD, Annemans L, Decruyenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386-400.
Publication Dates
-
Publication in this collection
31 Jan 2013 -
Date of issue
Dec 2012
History
-
Received
18 Apr 2012 -
Accepted
01 Nov 2012