ABSTRACT
Objective:
To establish the prevalence of physical, cognitive and psychiatric disabilities, associated factors and their relationship with the qualities of life of intensive care survivors in Brazil.
Methods:
A prospective multicenter cohort study is currently being conducted at 10 adult medical-surgical intensive care units representative of the 5 Brazilian geopolitical regions. Patients aged ≥ 18 years who are discharged from the participating intensive care units and stay 72 hours or more in the intensive care unit for medical or emergency surgery admissions or 120 hours or more for elective surgery admissions are consecutively included. Patients are followed up for a period of one year by means of structured telephone interviews conducted at 3, 6 and 12 months after discharge from the intensive care unit. The outcomes are functional dependence, cognitive dysfunction, anxiety and depression symptoms, posttraumatic stress symptoms, health-related quality of life, rehospitalization and long-term mortality.
Discussion:
The present study has the potential to contribute to current knowledge of the prevalence and factors associated with postintensive care syndrome among adult intensive care survivors in Brazil. In addition, an association might be established between postintensive care syndrome and health-related quality of life.
Keywords:
Critical care outcomes; Quality of life; Cognitive dysfunction; Anxiety; Depression; Stress disorders, Posttraumatic; Disabled persons
RESUMO
Objetivo:
Avaliar a prevalência de incapacidades físicas, cognitivas e psiquiátricas, fatores associados e sua relação com qualidade de vida em pacientes sobreviventes de internação em unidades de terapia intensiva brasileiras.
Métodos:
Um estudo de coorte prospectivo multicêntrico está sendo conduzido em dez unidades de terapia intensiva adulto clínico-cirúrgicas representativas das cinco regiões geopolíticas do Brasil. Pacientes com idade ≥ 18 anos que receberam alta das unidades de terapia intensiva participantes e permaneceram internados na unidade de terapia intensiva por 72 horas ou mais, nos casos de internação clínica ou cirúrgica de urgência, e por 120 horas ou mais, nos casos de internação cirúrgica eletiva, serão incluídos de forma consecutiva. Estes pacientes serão seguidos por 1 ano, por meio de entrevistas telefônicas estruturadas 3, 6 e 12 meses pós-alta da unidade de terapia intensiva. Dependência funcional, disfunção cognitiva, sintomas de ansiedade e depressão, sintomas de estresse pós-traumático, qualidade de vida relacionada à saúde, re-hospitalizações e mortalidade em longo prazo serão avaliados como desfechos.
Discussão:
O presente estudo tem o potencial de contribuir para o conhecimento a respeito da prevalência e dos fatores associados à síndrome pós-cuidados intensivos na população de pacientes adultos sobreviventes de internação em unidades de terapia intensiva brasileiras. Ademais, a associação entre síndrome pós-cuidados intensivos e qualidade de vida relacionada à saúde poderá ser estabelecida.
Descritores:
Resultados de cuidados críticos; Qualidade de vida; Disfunção Cognitiva; Ansiedade; Depressão; Transtornos de estresse pós-traumáticos; Pessoas com deficiência
INTRODUCTION
Intensive care units (ICUs) have evolved over time to provide the best human, organizational and technological resources to reduce the mortality of critically ill patients,(11 Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39(2):371-9.,22 Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(2):502-9.) and intensive care development thus centers on the goal of reducing mortality-theoretically the most important outcome.(33 Vest MT, Murphy TE, Araujo KL, Pisani MA. Disability in activities of daily living, depression, and quality of life among older medical ICU survivors: a prospective cohort study. Health Qual Life Outcomes. 2011;9:9.,44 Jones C. Recovery post ICU. Intensive Crit Care Nurs. 2014;30(5):239-45.) However, the increased survival of patients poses new challenges. The reduced mortality of critically ill patients has led healthcare professionals to diagnose and treat a “new disease” caused by complications related to the patient's stay in the ICU.(22 Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(2):502-9.)
Merely surviving an acute critical illness may not necessarily imply optimal quality of life after discharge. Post intensive care syndrome (PICS) is characterized by physical, cognitive and psychiatric disorders that have the potential to impair the quality of life of patients and often that of their families.(55 Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS; Canadian Critical Care Trials Group. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683-93.
6 Carson SS, Bach PB, Brzozowski L, Leff A. Outcomes after long-term acute care. An analysis of 133 mechanically ventilated patients. Am J Respir Crit Care Med. 1999;159(5 Pt 1):1568-73.
7 Hofhuis JG, van Stel HF, Schrijvers AJ, Rommes JH, Bakker J, Spronk PE. Conceptual issues specifically related to health-related quality of life in critically ill patients. Crit Care. 2009;13(1):118.
8 Cameron JI, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, Friedrich JO, Mehta S, Lamontagne F, Levasseur M, Ferguson ND, Adhikari NK, Rudkowski JC, Meggison H, Skrobik Y, Flannery J, Bayley M, Batt J, dos Santos C, Abbey SE, Tan A, Lo V, Mathur S, Parotto M, Morris D1, Flockhart L, Fan E, Lee CM, Wilcox ME, Ayas N, Choong K, Fowler R, Scales DC, Sinuff T, Cuthbertson BH, Rose L, Robles P, Burns S, Cypel M, Singer L, Chaparro C, Chow CW, Keshavjee S, Brochard L, Hébert P, Slutsky AS, Marshall JC, Cook D, Herridge MS; RECOVER Program Investigators (Phase 1: towards RECOVER); Canadian Critical Care Trials Group. One-year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374(19):1831-41.-99 Oyen SG, Vandijck DM, Benoit DD, Annemans L, Decruvenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386-400.) Complex interactions between comorbidities, complications of the acute critical illness (e.g., hypotension, hypoxia, hypo- or hyperglycemia and polyneuromyopathy), life support (e.g., sedation, mechanical ventilation and dialysis), organizational aspects of intensive care (e.g., restricted contact with family) and adjustment to the post-ICU period (e.g., changes in body image, disabilities, difficulty in returning to work and poor social support network) might impair the functional physical statuses of patients in the long run as well as contribute to the occurrence of cognitive dysfunction, anxiety, depression and posttraumatic stress disorder (PTSD).(1010 Needham DM, Wozniak AW, Hough CL, Morris PE, Dinglas VD, Jackson JC, Mendez-Tellez PA, Shanholtz C, Ely EW, Colantuoni E, Hopkins RO; National Institutes of Health NHLBI ARDS Network. Risk factors for physical impairment after acute lung injury in a national, multicenter study. Am J Respir Crit Care Med. 2014;189(10):1214-24.
11 Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-94.
12 Myhren H, Ekeberg O, Tøien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010;14(1):R14.
13 Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007;11(1):R28.
14 Rosa RG, Tonietto TF, da Silva DB, Gutierres FA, Ascoli AM, Madeira LC, Rutzen W, Falavigna M, Robinson CC, Salluh JI, Cavalcanti AB, Azevedo LC, Cremonese RV, Haack TR, Eugênio CS, Dornelles A, Bessel M, Teles JMM, Skrobik Y, Teixeira C; ICU Visits Study Group Investigators. Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med. 2017;45(10):1660-7.-1515 Azoulay E, Vincent JL, Angus DC, Arabi YM, Brochard L, Brett SJ, et al. Recovery after critical illness: putting the puzzle together - a consensus of 29. Crit Care. 2017;21(1):296.)
Although the medical literature on PICS is increasing,(1616 Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153(3):167-75.
17 Haas JS, Teixeira C, Cabral CR, Fleig AH, Freitas AP, Treptow EC, et al. Factors influencing physical functional status in intensive care unit survivors two years after discharge. BMC Anesthesiol. 2013;13:11.
18 Dietrich C, Cardoso JR, Vargas F, Sanchez EC, Dutra FH, Moreira C, et al. Functional ability in younger and older elderlies after discharge from the intensive care unit. A prospective cohort. Rev Bras Ter Intensiva. 2017;29(3):293-302.
19 de Azevedo JR, Montenegro WS, Rodrigues DP, de C Souza SC, Araujo VF, de Paula MP, et al. Long-term cognitive outcomes among unselected ventilated and non-ventilated ICU patients. J Intensive Care. 2017;5:18.
20 Bienvenu OJ, Friedman LA, Colantuoni E, Dinglas VD, Sepulveda KA, Mendez-Tellez P, et al. Psychiatric symptoms after acute respiratory distress syndrome: a 5-year longitudinal study. Intensive Care Med. 2018;44(1):38-47.
21 Oliveira HS, Fumis RR. Sex and spouse conditions influence symptoms of anxiety, depression, and posttraumatic stress disorder in both patients admitted to intensive care units and their spouses. Rev Bras Ter Intensiva. 2018;30(1):35-41.
22 Dexheimer Neto FL, Rosa RG, Duso BA, Haas JS, Savi A, Cabral CR, et al. Public versus private healthcare systems following discharge from the ICU: a propensity score-matched comparison of outcomes. Biomed Res Int. 2016;2016:6568531.-2323 Rosa RG, Kochhann R, Berto P, Biason L, Maccari JG, De Leon P, et al. More than the tip of the iceberg: association between disabilities and inability to attend a clinic-based post-ICU follow-up and how it may impact on health inequalities. Intensive Care Med. 2018;44(8):1352-4.) most studies that have been published to date involve specific subpopulations (e.g., patients with sepsis or acute respiratory distress syndrome - ARDS) or assess specific interventions (e.g., mechanical ventilation or dialysis) or isolated complications related to the patient's stay in the ICU (e.g., delirium).(2424 Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190(1):62-9.
25 Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM; Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293-304.
26 Vesz PS, Cremonese RV, Rosa RG, Maccari JG, Teixeira C. Impact of mechanical ventilation on quality of life and functional status after ICU discharge: a cross-sectional study. Rev Assoc Med Bras. 2018;64(1):47-53.-2727 Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367(1):30-9.) In addition, the evaluations are fragmented (e.g., assessment of cognitive disorders among patients with sepsis or of motor disorders in patients with ARDS) and are not necessarily representative of a large portion of the ICU survivor population. To date, no study has performed a broad-scope, long-term evaluation of the physical, cognitive and mental domains of PICS among a general population of ICU survivors.
The main objective of the present study is to investigate the prevalence of physical disabilities and late cognitive and psychological dysfunctions among ICU survivors in Brazil.
The secondary aims of this study are to perform a long-term evaluation of factors associated with functional dependence, cognitive dysfunction, anxiety, depression and PTSD symptoms among ICU survivors in Brazil and to evaluate the factors associated with readmission and long-term mortality as well as the relationship between physical, cognitive and psychiatric disabilities and health-related quality of life.
METHODS
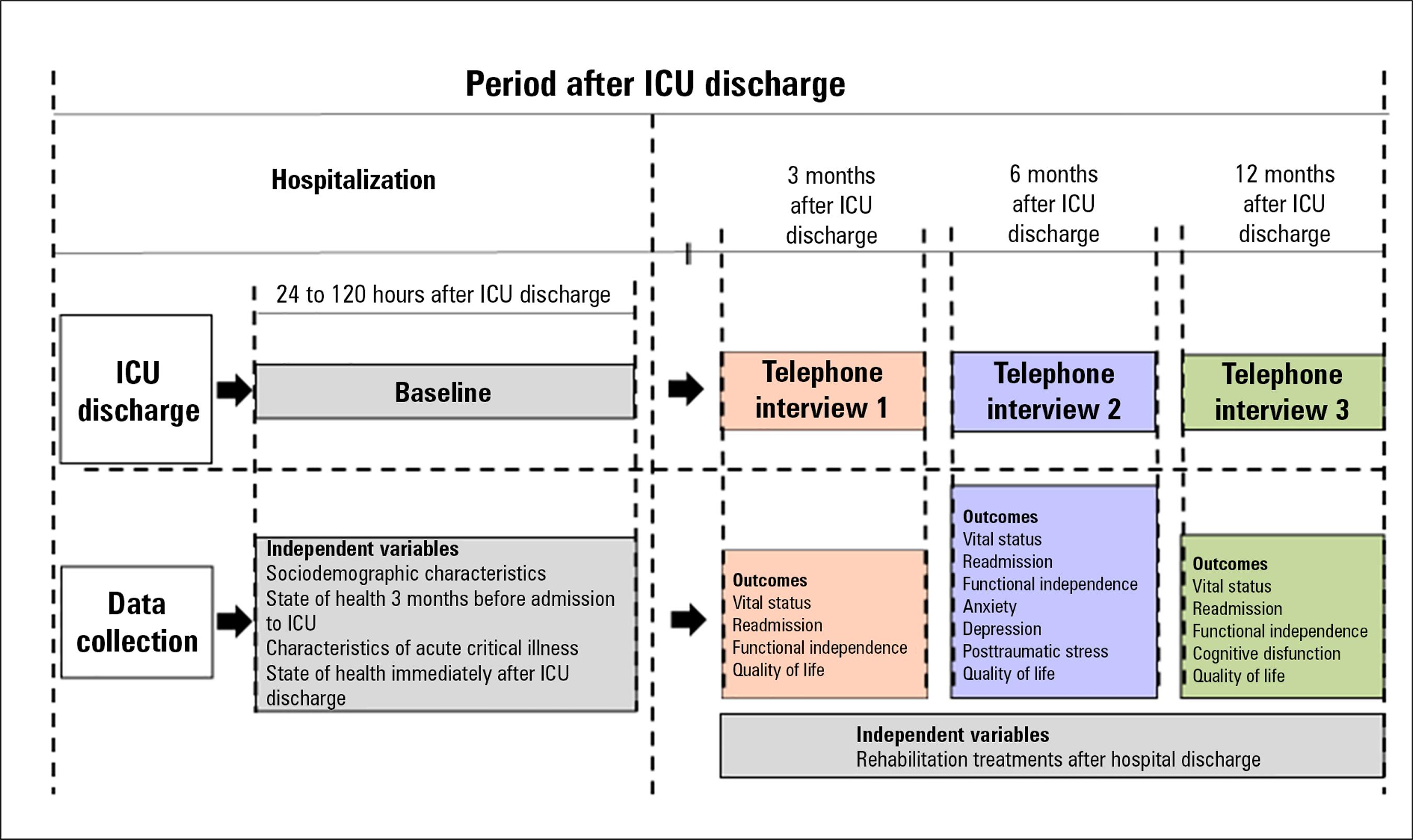
The present study is a prospective multicenter cohort study. Ten medical-surgical ICUs representative of the 5 geopolitical regions of Brazil (Figure 1) have been selected as study sites. Medical-surgical ICUs in public or private hospitals with 10 or more beds in which the staff manifested interest and had availability to implement the study protocol were selected by convenience sampling. For logistical and financial reasons, 6 of the included ICUs are located in Porto Alegre in the Southern region. To increase the representativeness of the sample, we included one interested hospital with characteristics similar to those of each of the other 4 Brazilian regions. ICU survivors are recruited while still at the hospital, 24 to 120 hours after discharge from the ICU. They are followed up for a period of 12 months by means of structured telephone interviews conducted at 3, 6 and 12 months after ICU discharge (Figure 2).
Participant eligibility
Patients aged ≥ 18 years who are discharged from the participating ICUs and stay in the ICU ≥ 72 hours (medical or urgent surgery admissions) or ≥ 120 hours (elective surgery admissions) are consecutively included.
The exclusion criteria are as follows: transfer from another ICU or hospital; direct discharge from the ICU to home or direct transfer from the ICU to another hospital; need for respiratory isolation after ICU discharge; impossibility of assessing the patient during the first 5 days after ICU discharge; no available telephone contact; readmission to the ICU; and refusal or withdrawal of agreement to participate.
Outcomes
Functional dependence
The degree of functional dependence will be measured by means of the Brazilian version of the Barthel index (BI)(2828 Minosso JS, Amendola F, Alvarenga MR, Oliveira MA. Validation of the Barthel Index in elderly patients attended in outpatient clinics, in Brazil. Acta Paul Enferm. 2010;23(2):218-23.) at 3, 6 and 12 months after ICU discharge. The BI measures functional dependence in personal care and mobility. The score ranges from 0 to 100; a higher score indicates less functional dependence.
Cognitive dysfunction
Long-term cognitive dysfunction will be investigated by means of the Brazilian version (validated for telephone administration) of the Montreal Cognitive Assessment (tMoCA)(2929 Pendlebury ST, Welch SJ, Cuthbertson FC, Mariz J, Mehta Z, Rothwell PM. Telephone assessment of cognition after transient ischemic attack and stroke: modified telephone interview of cognitive status and telephone Montreal Cognitive Assessment versus face-to-face Montreal Cognitive Assessment and neuropsychological battery. Stroke. 2013;44(1):227-9.) at 12 months after the patient's discharge from the ICU. tMoCA scores range from 0 to 22; higher scores indicate better cognitive status.
Anxiety and depression symptoms
Anxiety and depression symptoms will be investigated at 6 months after ICU discharge by means of the Brazilian version of the Hospital Anxiety and Depression Scale (HADS).(3030 Botega NJ, Bio MR, Zomignani MA, Garcia Jr C, Pereira WA. Mood disorders among medical in-patients: a validation study of the hospital anxiety and depression scale (HAD). Rev Saúde Pública. 1995;29(5):355-63.) HADS comprises 2 domains, anxiety and depression. The score for each domain ranges from 0 to 21; higher scores indicate greater intensity of anxiety or depression symptoms.
Posttraumatic stress
Posttraumatic stress disorder symptoms will be investigated at 6 months after ICU discharge by means of the Brazilian version of the Impact of Event Scale-6 (IES-6).(3131 Thoresen S, Tambs K, Hussain A, Heir T, Johansen VA, Bisson JI. Brief measure of posttraumatic stress reactions: impact of Event Scale-6. Soc. Psychiatry Psychiatr Epidemiol. 2010;45(3):405-12.) The IES-6 score ranges from 0 to 24; higher scores indicate a greater intensity of PTSD symptoms.
Readmission
The rates of unplanned readmission will be calculated at 3, 6 and 12 months after ICU discharge. The outcomes to be analyzed during the 12-month follow-up period are the cumulative incidence of first unplanned readmission after hospital discharge and the number of readmissions per patient.
Mortality
The vital statuses of patients will be investigated at 3, 6 and 12 months after ICU discharge.
Health-related quality of life
The quality of life of the participants will be investigated by means of the Brazilian version of the Short-Form Health Survey version 2 (SF-12v2).(3232 Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-33.) SF-12v2 analyzes health-related quality of life based on the respondent's perception of health aspects in the previous 4 weeks. It comprises 8 domains: general health, physical functioning, physical role function, bodily pain, vitality, emotional role function, mental health and social functioning. The 8 domains are summarized in 2 dimensions, physical and mental. In each case, the score ranges from 0 to 100, and higher scores indicate better health-related quality of life.
Other outcomes
The following exploratory outcomes will be considered during follow-up: instrumental activities of daily living, assessed based on the Lawton-Brody index(3333 Santos RL, Virtuoso Jr JS. Reliability of the Brazilian version of the scale of instrumental activities of daily living. RBPS. 2008;21(4):290-6.) at 12 months after ICU discharge; functional assessment of oral intake, assessed by means of the Functional Oral Intake Scale (FOIS) at 3, 6 and 12 months after ICU discharge;(3434 Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516-20.) risk of dysphagia, assessed by means of the Eating Assessment Tool-10 (EAT-10)(3535 Gonçalves MI, Remaili CB, Behlau M. Cross-cultural adaptation of the Brazilian version of the Eating Assessment Tool - EAT-10. Codas. 2013;25(6):601-4.) at 3 and 12 months after ICU discharge; level of physical activity, measured using the International Physical Activity Questionnaire (IPAQ)(3636 Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381-95.) at 3, 6 and 12 months after ICU discharge; return to work (for patients employed at the time of admission to ICU) at 3, 6 and 12 months after ICU discharge; and medical expenses and variation in family income at 3 months after ICU discharge.
Figure 2 shows the time points at which data will be collected during the follow-up period. Trained investigators are responsible for enrolling participants and for collecting baseline data at each participating hospital. Telephone follow-up will be performed from a telephone center located at the study coordination center (Hospital Moinhos de Vento). Five sets of independent variables will be analyzed (Table 1) : (1) sociodemographic characteristics; (2) state of health 3 months before admission to the ICU; (3) characteristics of the acute critical illness; (4) state of health immediately after ICU discharge; and (5) rehabilitation treatment received by the patient after hospital discharge. Sociodemographic characteristics, state of health 3 months before admission to the ICU, and characteristics of the acute critical disease will be retrospectively analyzed based on data extracted from medical records and on a structured interview with the participants conducted at 24 to 120 hours after ICU discharge. The patient's state of health immediately after ICU discharge will also be evaluated at that time. Rehabilitation treatments after hospital discharge will be analyzed based on information obtained during the telephone follow-up. All outcomes will be investigated by means of telephone interviews at 3, 6 and 12 months after ICU discharge.
In cases involving patients who lack the cognitive or physical conditions necessary to provide consent, consent to participation is requested from family members. During the in-person interview at baseline and during the telephone interviews, family members are allowed to answer some objective questions when patients do not exhibit adequate physical or cognitive conditions. Family members are not allowed to respond to the instruments that measure subjective outcomes, such as cognition, anxiety or depression symptoms, PTSD, health-related quality of life, level of physical activity and symptoms of dysphagia.
Despite the use of a protocol to ensure the objectivity of the interviews, spontaneous mentions of clinical complaints are expected to occur during the in-person interview at baseline and during the telephone interviews. Because this is an observational study, no intervention will be performed in such cases. In cases involving medical complaints, the investigators are trained to orient the patient or family members to report the complaint to the assistant physician or to the healthcare staff involved in the patient care. In regard to sensitive questions during interviews at the time of recruitment and during interviews, the investigators will reinforce that participants are entitled to choose not to answer questions that make them uncomfortable.
Telephone follow-up
Unlike the baseline assessment performed immediately after ICU discharge, which will be conducted at the participating hospital, telephone follow-up will be performed at a single center. Regardless of the hospital at which the participate receives care, all participants will be followed up by investigators who have been trained in the use of standardized telephone interview methods. To ensure the privacy of the respondents, the telephone interviews will be performed in a secluded room in which only the interviewer is present.
The ICU discharge date serves as a reference for scheduling the telephone interviews. Based on the estimated dates, investigators have a 30-day window period (15 days before and 15 days after the estimated date) to conduct the interviews. Interviews will be rated lost when the participants' telephone lines are disconnected or do not exist or after 10 attempts at different times on several days within the window period. If one interview is lost, contact is nonetheless attempted at the subsequent scheduled interview times.
Procedures to ensure the quality of the data
The following procedures will be performed to ensure the quality of the data:
-
To ensure standardization of the study procedures, the investigators responsible for data collection at each participating center will receive training in loco prior to the beginning of recruitment.
-
The investigators at each participating center will have access to the study coordination center as a means of dispelling doubts and solving potential problems.
-
The data will be entered on printed standardized data collection forms and stored in an electronic data capture system (REDCap, Vanderbilt University, Nashville, TN, USA). To ensure the adequacy of data transcription, routine double-checking will be performed as data are entered into the electronic data capture system.
-
A data cleaning routine will be applied frequently. The investigators at the participating centers will be contacted in cases of inconsistencies or missing data. This information also provides feedback in regard to the need for retraining.
-
Remote monitoring of data quality will be performed at the study coordination center.
-
Telephone interviews will be taped and audited to verify consistency in data collection. The audio files will be anonymously stored in a server that meets the same security norms as those used for data in electronic medical records. Access to the files, which is restricted to the study team, will require user identification and a password.
The sample size was calculated as the number of participants needed to estimate the prevalence of functional dependence, cognitive dysfunction, anxiety, depression and PTSD symptoms. An adequate sample size for all questions to be answered was chosen. The significance level for estimating the prevalence of each outcome described in table 2,(1212 Myhren H, Ekeberg O, Tøien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010;14(1):R14.,1313 Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007;11(1):R28.,1818 Dietrich C, Cardoso JR, Vargas F, Sanchez EC, Dutra FH, Moreira C, et al. Functional ability in younger and older elderlies after discharge from the intensive care unit. A prospective cohort. Rev Bras Ter Intensiva. 2017;29(3):293-302.,1919 de Azevedo JR, Montenegro WS, Rodrigues DP, de C Souza SC, Araujo VF, de Paula MP, et al. Long-term cognitive outcomes among unselected ventilated and non-ventilated ICU patients. J Intensive Care. 2017;5:18.) set using the corresponding absolute precision intervals, is 5%. Considering (1) cumulative mortality rates of 15% at 3 months, 25% at 6 months and 40% at one year after ICU discharge,(11 Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39(2):371-9.) (2) cumulative losses to follow-up of 5% at 3 months, 10% at 6 months and 20% at 12 months, and (3) a potential failure rate of 40% in obtaining responses to telephone follow-up interviews, analysis of 1,212 patients at 3 months, 600 patients at 6 months and 432 patients at 12 months after ICU discharge would require the inclusion of 1,500 participants. The mortality rate at 3 months includes deaths that may occur during the period between transfer from the ICU and hospital discharge. Because this is a multicenter study, we chose to increase the sample size by 10% considering that no estimates of outcome variation exist among the participating centers.
Sample sizes needed to detect the prevalence of disabilities after discharge from an intensive care unit
Statistical analysis
The analyses to be performed in the present study are aimed at providing a broad view of the physical, cognitive and psychiatric disabilities of ICU survivors in Brazil. Continuous variables will be expressed as the mean and standard deviation or median and interquartile range as appropriate. Categorical variables will be described as absolute and relative frequencies. Regression models will be used to analyze the association between independent variables and outcomes; the distribution of the outcomes of interest probabilities will be fitted using generalized linear models. Graphic analysis will be performed to evaluate the distribution of variables and to verify the assumptions of the regression model. The outcomes relative to physical, cognitive and psychiatric disabilities will be expressed as prevalence rates, mean scores and the corresponding standard deviations. The outcomes measured at each time point, including individual and joint prevalence rates, will also be represented by means of Venn diagrams. Scores on the health-related quality of life questionnaire will be expressed as the mean and standard deviation over time. Mortality after ICU discharge will be represented as survival curves. Functional dependence will also be analyzed as the incidence of BI reduction at each follow-up time point compared to that at baseline. Considering that nonsurvivors and participants unable to respond might represent poorer outcomes, we will perform sensitivity analysis, encompassing the best and worst scenarios, taking into consideration both vital status and unability to respond. A 0.05 significance level will be adopted for all comparisons. R version 3.4.4 software (R-project for statistical computing) will be used for statistical analysis.
The present study will comply with Brazilian National Health Council Resolution no. 466/12. The study protocol was approved by the institutional research ethics committee at the coordination center (CAAE 04258312.4.1001.5330) and by the research ethics committees of all participating centers. The consent form includes information on the study aims, data collection and recording methods and ensures confidentiality and anonymity. Participants are granted the right to withdraw from the study at any time. They are also assured that the collected data will be used only for research purposes.
Discussion and current status of the study
Health-related quality of life might be defined as the measure of how an individual's normal or expected physical, emotional and social well-being is influenced by a health problem or its treatment.(3737 Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645-9.) Advances in diagnostic and therapeutic options have resulted in an increased number of patients who survive acute critical illness.(3838 Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014;311(13):1308-16.) Several studies have been performed to analyze short-term mortality within this context. However, research on other relevant aspects, such as prevalence of disabilities after ICU admission, their determinants and their relationship with health-related quality of life, is still insufficient.
After ICU discharge, critically ill patients may develop physical, cognitive and/or psychiatric disorders that lead to prolonged recovery, higher consumption of healthcare resources, and possible impairment of quality of life.(99 Oyen SG, Vandijck DM, Benoit DD, Annemans L, Decruvenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386-400.,3939 Herridge MS, Moss M, Hough CL, Hopkins RO, Rice TW, Bienvenu OJ, et al. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med. 2016;42(5):725-38.,4040 Ruhl AP, Huang M, Colantuoni E, Karmarkar T, Dinglas VD, Hopkins RO, Needham DM; With the National Institutes of Health, NationalHeart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Healthcare utilization and costs in ARDS survivors: a 1-year longitudinal national US multicenter study. Intensive Care Med. 2017;43(7):980-91.) In a systematic review that included 53 studies, ICU survivors consistently reported having a poorer quality of life than healthy controls, even after adjustments were made for age and sex.(99 Oyen SG, Vandijck DM, Benoit DD, Annemans L, Decruvenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386-400.) Despite the plausibility of the association between PICS and impaired health-related quality of life, studies comparing the qualities of life of ICU survivors with and without PICS are scarce.
The strengths of the present study are its prospective multicenter design, its inclusion of a large population of ICU survivors, its use of an a priori definition of objective outcomes, and its use of standardized and validated tools for the diagnosis of disabilities after ICU discharge. The limitations of this study derive from the uncertainty regarding the number of patients effectively needed to determine the prevalence of disabilities after ICU discharge, as high rates of mortality and morbidity following critical illness might contribute to losses to follow-up and the inability of the participants to respond to telephone interviews.(2222 Dexheimer Neto FL, Rosa RG, Duso BA, Haas JS, Savi A, Cabral CR, et al. Public versus private healthcare systems following discharge from the ICU: a propensity score-matched comparison of outcomes. Biomed Res Int. 2016;2016:6568531.) These aspects might further contribute to underestimation of the prevalence of disabilities after ICU discharge. The use of data reported in studies conducted abroad to calculate the sample size might also interfere with the outcome estimates. Those studies were chosen because they applied the same tools and time points for assessment of each outcome; thus, their design is quite similar to ours.
The study protocol and design were finalized in March 2015. All the investigators from all the participating centers received training on the study procedures in loco. We are currently recruiting patients at 10 ICUs representative of the Brazilian geopolitical distribution (Figure 1). As of December 2017, 1,554 patients have been included in the study. We expect that follow-up of all the patients included in the cohort will be completed by December 2018.
CONCLUSION
The present study will contribute to knowledge regarding the prevalence of disabilities, their determinants and their impact on the qualities of life of intensive care unit survivors in Brazil. The results are expected to give rise to new research questions aimed at investigating the causes of such disabilities and identifying preventive and rehabilitation measures for adult intensive care unit survivors.
-
Funding: The present study is being conducted in partnership with the Brazilian Ministry of Health through the Program of Institutional Development of the Brazilian Unified Health System (PROADI-SUS). This support program is considered a goal of the National Health Plan, with emphasis on its relevance and potential contribution to SUS governance according to Administrative Ruling no. 3.362 of 8 December 2017 concerning the following field of action: III-health research of public interest: projects for studies related to health promotion and recovery, prevention of diseases and other health problems.
-
Institution in charge: Hospital Moinhos de Vento is the coordination center for the present study.
ACKNOWLEDGMENTS
We thank the data collection teams at the participating ICUs, the Hospital Moinhos de Vento, and the Ministry of Health for their support. We thank the Coordenação Geral de Atenção Hospitalar e de Urgência (Hospital and Urgent Care General Coordination; CGHOSP) for its support. The present study is endorsed by the Rede Brasileira de Pesquisa em Terapia Intensiva (Brazilian Network in Intensive Care Research; BRICnet).
REFERÊNCIAS
-
1Desai SV, Law TJ, Needham DM. Long-term complications of critical care. Crit Care Med. 2011;39(2):371-9.
-
2Needham DM, Davidson J, Cohen H, Hopkins RO, Weinert C, Wunsch H, et al. Improving long-term outcomes after discharge from intensive care unit: report from a stakeholders' conference. Crit Care Med. 2012;40(2):502-9.
-
3Vest MT, Murphy TE, Araujo KL, Pisani MA. Disability in activities of daily living, depression, and quality of life among older medical ICU survivors: a prospective cohort study. Health Qual Life Outcomes. 2011;9:9.
-
4Jones C. Recovery post ICU. Intensive Crit Care Nurs. 2014;30(5):239-45.
-
5Herridge MS, Cheung AM, Tansey CM, Matte-Martyn A, Diaz-Granados N, Al-Saidi F, Cooper AB, Guest CB, Mazer CD, Mehta S, Stewart TE, Barr A, Cook D, Slutsky AS; Canadian Critical Care Trials Group. One-year outcomes in survivors of the acute respiratory distress syndrome. N Engl J Med. 2003;348(8):683-93.
-
6Carson SS, Bach PB, Brzozowski L, Leff A. Outcomes after long-term acute care. An analysis of 133 mechanically ventilated patients. Am J Respir Crit Care Med. 1999;159(5 Pt 1):1568-73.
-
7Hofhuis JG, van Stel HF, Schrijvers AJ, Rommes JH, Bakker J, Spronk PE. Conceptual issues specifically related to health-related quality of life in critically ill patients. Crit Care. 2009;13(1):118.
-
8Cameron JI, Chu LM, Matte A, Tomlinson G, Chan L, Thomas C, Friedrich JO, Mehta S, Lamontagne F, Levasseur M, Ferguson ND, Adhikari NK, Rudkowski JC, Meggison H, Skrobik Y, Flannery J, Bayley M, Batt J, dos Santos C, Abbey SE, Tan A, Lo V, Mathur S, Parotto M, Morris D1, Flockhart L, Fan E, Lee CM, Wilcox ME, Ayas N, Choong K, Fowler R, Scales DC, Sinuff T, Cuthbertson BH, Rose L, Robles P, Burns S, Cypel M, Singer L, Chaparro C, Chow CW, Keshavjee S, Brochard L, Hébert P, Slutsky AS, Marshall JC, Cook D, Herridge MS; RECOVER Program Investigators (Phase 1: towards RECOVER); Canadian Critical Care Trials Group. One-year outcomes in caregivers of critically ill patients. N Engl J Med. 2016;374(19):1831-41.
-
9Oyen SG, Vandijck DM, Benoit DD, Annemans L, Decruvenaere JM. Quality of life after intensive care: a systematic review of the literature. Crit Care Med. 2010;38(12):2386-400.
-
10Needham DM, Wozniak AW, Hough CL, Morris PE, Dinglas VD, Jackson JC, Mendez-Tellez PA, Shanholtz C, Ely EW, Colantuoni E, Hopkins RO; National Institutes of Health NHLBI ARDS Network. Risk factors for physical impairment after acute lung injury in a national, multicenter study. Am J Respir Crit Care Med. 2014;189(10):1214-24.
-
11Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787-94.
-
12Myhren H, Ekeberg O, Tøien K, Karlsson S, Stokland O. Posttraumatic stress, anxiety and depression symptoms in patients during the first year post intensive care unit discharge. Crit Care. 2010;14(1):R14.
-
13Girard TD, Shintani AK, Jackson JC, Gordon SM, Pun BT, Henderson MS, et al. Risk factors for post-traumatic stress disorder symptoms following critical illness requiring mechanical ventilation: a prospective cohort study. Crit Care. 2007;11(1):R28.
-
14Rosa RG, Tonietto TF, da Silva DB, Gutierres FA, Ascoli AM, Madeira LC, Rutzen W, Falavigna M, Robinson CC, Salluh JI, Cavalcanti AB, Azevedo LC, Cremonese RV, Haack TR, Eugênio CS, Dornelles A, Bessel M, Teles JMM, Skrobik Y, Teixeira C; ICU Visits Study Group Investigators. Effectiveness and safety of an extended ICU visitation model for delirium prevention: a before and after study. Crit Care Med. 2017;45(10):1660-7.
-
15Azoulay E, Vincent JL, Angus DC, Arabi YM, Brochard L, Brett SJ, et al. Recovery after critical illness: putting the puzzle together - a consensus of 29. Crit Care. 2017;21(1):296.
-
16Unroe M, Kahn JM, Carson SS, Govert JA, Martinu T, Sathy SJ, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153(3):167-75.
-
17Haas JS, Teixeira C, Cabral CR, Fleig AH, Freitas AP, Treptow EC, et al. Factors influencing physical functional status in intensive care unit survivors two years after discharge. BMC Anesthesiol. 2013;13:11.
-
18Dietrich C, Cardoso JR, Vargas F, Sanchez EC, Dutra FH, Moreira C, et al. Functional ability in younger and older elderlies after discharge from the intensive care unit. A prospective cohort. Rev Bras Ter Intensiva. 2017;29(3):293-302.
-
19de Azevedo JR, Montenegro WS, Rodrigues DP, de C Souza SC, Araujo VF, de Paula MP, et al. Long-term cognitive outcomes among unselected ventilated and non-ventilated ICU patients. J Intensive Care. 2017;5:18.
-
20Bienvenu OJ, Friedman LA, Colantuoni E, Dinglas VD, Sepulveda KA, Mendez-Tellez P, et al. Psychiatric symptoms after acute respiratory distress syndrome: a 5-year longitudinal study. Intensive Care Med. 2018;44(1):38-47.
-
21Oliveira HS, Fumis RR. Sex and spouse conditions influence symptoms of anxiety, depression, and posttraumatic stress disorder in both patients admitted to intensive care units and their spouses. Rev Bras Ter Intensiva. 2018;30(1):35-41.
-
22Dexheimer Neto FL, Rosa RG, Duso BA, Haas JS, Savi A, Cabral CR, et al. Public versus private healthcare systems following discharge from the ICU: a propensity score-matched comparison of outcomes. Biomed Res Int. 2016;2016:6568531.
-
23Rosa RG, Kochhann R, Berto P, Biason L, Maccari JG, De Leon P, et al. More than the tip of the iceberg: association between disabilities and inability to attend a clinic-based post-ICU follow-up and how it may impact on health inequalities. Intensive Care Med. 2018;44(8):1352-4.
-
24Prescott HC, Langa KM, Liu V, Escobar GJ, Iwashyna TJ. Increased 1-year healthcare use in survivors of severe sepsis. Am J Respir Crit Care Med. 2014;190(1):62-9.
-
25Herridge MS, Tansey CM, Matté A, Tomlinson G, Diaz-Granados N, Cooper A, Guest CB, Mazer CD, Mehta S, Stewart TE, Kudlow P, Cook D, Slutsky AS, Cheung AM; Canadian Critical Care Trials Group. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364(14):1293-304.
-
26Vesz PS, Cremonese RV, Rosa RG, Maccari JG, Teixeira C. Impact of mechanical ventilation on quality of life and functional status after ICU discharge: a cross-sectional study. Rev Assoc Med Bras. 2018;64(1):47-53.
-
27Saczynski JS, Marcantonio ER, Quach L, Fong TG, Gross A, Inouye SK, et al. Cognitive trajectories after postoperative delirium. N Engl J Med. 2012;367(1):30-9.
-
28Minosso JS, Amendola F, Alvarenga MR, Oliveira MA. Validation of the Barthel Index in elderly patients attended in outpatient clinics, in Brazil. Acta Paul Enferm. 2010;23(2):218-23.
-
29Pendlebury ST, Welch SJ, Cuthbertson FC, Mariz J, Mehta Z, Rothwell PM. Telephone assessment of cognition after transient ischemic attack and stroke: modified telephone interview of cognitive status and telephone Montreal Cognitive Assessment versus face-to-face Montreal Cognitive Assessment and neuropsychological battery. Stroke. 2013;44(1):227-9.
-
30Botega NJ, Bio MR, Zomignani MA, Garcia Jr C, Pereira WA. Mood disorders among medical in-patients: a validation study of the hospital anxiety and depression scale (HAD). Rev Saúde Pública. 1995;29(5):355-63.
-
31Thoresen S, Tambs K, Hussain A, Heir T, Johansen VA, Bisson JI. Brief measure of posttraumatic stress reactions: impact of Event Scale-6. Soc. Psychiatry Psychiatr Epidemiol. 2010;45(3):405-12.
-
32Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220-33.
-
33Santos RL, Virtuoso Jr JS. Reliability of the Brazilian version of the scale of instrumental activities of daily living. RBPS. 2008;21(4):290-6.
-
34Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil. 2005;86(8):1516-20.
-
35Gonçalves MI, Remaili CB, Behlau M. Cross-cultural adaptation of the Brazilian version of the Eating Assessment Tool - EAT-10. Codas. 2013;25(6):601-4.
-
36Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. 2003;35(8):1381-95.
-
37Karimi M, Brazier J. Health, health-related quality of life, and quality of life: what is the difference? Pharmacoeconomics. 2016;34(7):645-9.
-
38Kaukonen KM, Bailey M, Suzuki S, Pilcher D, Bellomo R. Mortality related to severe sepsis and septic shock among critically ill patients in Australia and New Zealand, 2000-2012. JAMA. 2014;311(13):1308-16.
-
39Herridge MS, Moss M, Hough CL, Hopkins RO, Rice TW, Bienvenu OJ, et al. Recovery and outcomes after the acute respiratory distress syndrome (ARDS) in patients and their family caregivers. Intensive Care Med. 2016;42(5):725-38.
-
40Ruhl AP, Huang M, Colantuoni E, Karmarkar T, Dinglas VD, Hopkins RO, Needham DM; With the National Institutes of Health, NationalHeart, Lung, and Blood Institute Acute Respiratory Distress Syndrome Network. Healthcare utilization and costs in ARDS survivors: a 1-year longitudinal national US multicenter study. Intensive Care Med. 2017;43(7):980-91.
Edited by
Publication Dates
-
Publication in this collection
10 Jan 2019 -
Date of issue
Oct-Dec 2018
History
-
Received
10 Apr 2018 -
Accepted
30 May 2018