Abstracts
INTRODUCTION: Cerebral palsy is a disorder characterized by an abnormal activity, movement and posture development. The Bobath concept is one of the most used methods for the neuropediatric rehabilitation and is based on the acquisition of sensorimotor skills according to the normal sequence of the psychomotor development. OBJECTIVE: In this study, we explore the relationship between electromyographic signal (EMG) in muscles involved in the cervical control in the frontal, sagittal and transversal planes and facilitation techniques using key points of control, which is part of the Bobath approach. MATERIALS AND METHODS: The methodology was quantitative applied in a case study of one child, seven years old, with Cerebral palsy and West syndrome diagnosis. The surface EMG activity of muscle groups involved in the cervical control (extensors, flexors and lateral flexors) was collected under therapeutic handling using key points of control in ventral decubitus on the wedge and in lateral decubitus along 5 seconds. RESULTS: The EMG signal from extensors and flexors muscles was augmented under therapeutic handling for weight bearing using the hip joint as key point of control in both decubitus. Although the EMG basal signal in the ventral position had been intensified during the weight bearing, the EMG activity was higher when the handling was performed using the lateral position. CONCLUSION: We concluded that the therapeutic handling for weigh bearing using the hip joint as key point of control induced the facilitation of cervical control. The use of the lateral position as well as the repetition of this position in a maintained way, since the correct alignment position is observed, should be able to induce higher facilitation of cervical control than weigh bearing in ventral position on the wedge.
Cerebral palsy; Physical therapy modalities; Electromyography
INTRODUÇÃO: Paralisia cerebral é um distúrbio caracterizado por alterações no desenvolvimento da atividade, do movimento e da postura. O Conceito Neuroevolutivo Bobath é um método utilizado na reabilitação neuropediátrica, fundamentando-se na facilitação da aquisição de habilidades sensório-motoras de acordo com a sequência de desenvolvimento neuropsicomotor normal. OBJETIVO: Verificar atividade eletromiográfica de músculos envolvidos no controle cervical nos planos frontal, sagital e transverso, mediante manuseio em pontos-chave de controle, objetivando transferência de peso e estabilização corporal. MATERIAIS E MÉTODOS: Trata-se de uma avaliação quantitativa em um estudo de caso, no qual uma paciente de sete anos de idade, com diagnóstico clínico de paralisia cerebral e síndrome de West, foi submetida à análise eletromiográfica da musculatura envolvida no controle cervical, mediante manuseio em pontos-chave de controle. O registo ocorreu durante o manuseio utilizando postura de decúbito ventral sobre cunha e postura de decúbito lateral sobre o solo. RESULTADOS: O sinal eletromiográfico dos extensores e flexores na região cervical intensificou-se mediante manuseio para transferência de peso em ponto-chave de quadril em ambas as posturas. Embora o sinal de base tenha sido ampliado durante a transferência de peso para o quadril, o registro eletromiográfico nos segmentos musculares avaliados foi superior no decúbito lateral. CONCLUSÕES: Verificou-se que a transferência de peso para o quadril induziu facilitação do controle cervical e que o decúbito lateral de forma repetida e sustentada, mediante correto manuseio, alinhamento e transferência de peso, facilitou de forma mais pronunciada a atividade muscular na região cervical e de tronco superior do que o manuseio em decúbito ventral sobre a cunha.
Paralisia cerebral; Modalidades de fisioterapia; Eletromiografia
ORIGINAL ARTICLES
Electromyographic activity of trunk muscles during therapy using the Bobath Concept
Aline de Souza PagnussatI; Anelise de Saldanha SimonII; Camila Grazziotin dos SantosIII; Morgana PostalIV; Sonia ManaceroV; Renata Raab RamosVI
IPhysiotherapist, PhD in Neuroscience from the Federal University of Rio Grande do Sul (UFRGS), professor of Physiotherapy, Federal University of Health Sciences of Porto Alegre (UFCSPA), Porto Alegre, RS -Brazil, e-mails: alinesp@ufcspa.edu.br, alinespagnussat@gmail.com
IIPhysical Therapist, Master's Program Graduate in Rehabilitation Sciences from the Federal University of Health Sciences of Porto Alegre (UFCSPA), physiotherapist of Association for Assistance to Disabled Children (AACD/RS), Porto Alegre, RS -Brazil, e-mail: anesimon@yahoo.com.br
IIIPhysical Therapist, Master's Program at the Graduate in Child and Adolescent Federal University of Rio Grande do Sul, physiotherapist of Association for Assistance to Disabled Children (AACD/RS), Porto Alegre, RS -Brazil, e-mail: camigrazziotin@gmail.com
IVPhysiotherapist graduated from the University of Caxias do Sul (UCS), physiotherapist Association Dr. Bartholomeu Tacchini-Hospital Tacchini, Bento Gonçalves, RS -Brazil, e-mail: moguipostal@yahoo.com.br
VPhysiotherapist, PhD in Medicine Pediatrics and Child Health from the Pontifical Catholic University of Rio Grande do Sul (PUCRS), Physiotherapist and Physiotherapy Studies Center for Functionality and Integration (CENEFFI), Porto Alegre, RS -Brazil, e-mail: smanacero@uol.com.br
VIPhysiotherapist graduated from Methodist University (IPA), Student of Neuroevolutivo Bobath Centre for Studies and Physiotherapy for Functionality and Integration (CENEFFI), Porto Alegre, RS -Brazil, e-mail: renataramos@live.com
ABSTRACT
INTRODUCTION: Cerebral palsy is a disorder characterized by an abnormal activity, movement and posture development. The Bobath concept is one of the most used methods for the neuropediatric rehabilitation and is based on the acquisition of sensorimotor skills according to the normal sequence of the psychomotor development.
OBJECTIVE: In this study, we explore the relationship between electromyographic signal (EMG) in muscles involved in the cervical control in the frontal, sagittal and transversal planes and facilitation techniques using key points of control, which is part of the Bobath approach.
MATERIALS AND METHODS: The methodology was quantitative applied in a case study of one child, seven years old, with Cerebral palsy and West syndrome diagnosis. The surface EMG activity of muscle groups involved in the cervical control (extensors, flexors and lateral flexors) was collected under therapeutic handling using key points of control in ventral decubitus on the wedge and in lateral decubitus along 5 seconds.
RESULTS: The EMG signal from extensors and flexors muscles was augmented under therapeutic handling for weight bearing using the hip joint as key point of control in both decubitus. Although the EMG basal signal in the ventral position had been intensified during the weight bearing, the EMG activity was higher when the handling was performed using the lateral position.
CONCLUSION: We concluded that the therapeutic handling for weigh bearing using the hip joint as key point of control induced the facilitation of cervical control. The use of the lateral position as well as the repetition of this position in a maintained way, since the correct alignment position is observed, should be able to induce higher facilitation of cervical control than weigh bearing in ventral position on the wedge.
Keywords: Cerebral palsy. Physical therapy modalities. Electromyography.
Introduction
Cerebral palsy (CP) is a disorder characterized by abnormal development of movement and postural activity due to non-progressive brain damage during fetal development or childhood (1). Individuals afflicted with this injury may present with a variety of sensorimotor problems. Some primary problems are directly related to the injured central nervous system (CNS), affecting muscle tone, balance, strength, and selectivity. However, secondary problems, including muscle contractures and bone deformities, may develop slowly over time in response to the primary problems (2). Current studies estimate a worldwide prevalence of two to three affected individuals per 1000 live births (3).
Along with the primary motor problems, there may be several associated disorders including mental retardation, seizures, hearing loss, visual deficits, speech disorders, behavioral disorders, swallowing and feeding problems, respiratory problems, and incontinence (3). Impairment-associated stresses between the occurrences of seizures are present in 15% to 55% of patients with CP (4). West syndrome is considered a type of epilepsy marked by the occurrence of spasms, interrupted development, and hypsarrhythmic patterns in electroencephalograms (5).
Several techniques and therapeutic methods have been developed to promote the rehabilitation of sensorimotor disorders consequent to CP. The Bobath concept was developed during the 1950s and has remained an accepted practice throughout the years due to its dynamic adaptability in the face of new neuroscientific approaches. This approach is based on rehabilitation for solving functional problems and focuses on recovery of sensorimotor body segments affected in opposition to motion compensation (6, 7).
The Bobath concept is characterized by a particular way of observing, analyzing, and interpreting motor performance for a given task. It also always respects the sequence required for the acquisition of skills within normal psychomotor development. Although its clinical application is based on individualized reasoning instead of applying standardized techniques to all, its precepts can be grouped into strategies inhibition, stimulation, and facilitation. The use of information relating to improving motor performance is described as facilitation. This allows movements to be more successful in relation to postural orientation, movement components, functional sequences, the recognition of a task, and the motivation to complete it (6). Through the facilitation techniques, the individual experiences movements that are not completely passive, but still cannot be accomplished alone. The objective is to make the activity possible, since it requires a response and it allows this to happen (7). This can be used for activation of a specific muscle in preparation for a volitional activity. It also serves to stabilize a body part or body segment to reduce muscle activity not relevant to the execution of a certain task (6).
Children who develop normally have different patterns of postural adjustment compared with children with CP. In children with CP, activities are limited by muscle synergies that help to increase or decrease the success of the task (8). The development of head control is the most basic motor skill acquisition process. Head control depends on the ability to integrate vestibular and proprioceptive afferents to the motor command efferent pathways for ventral-medial postural control. Its development is essential for modulating reflexes triggered by activation of sensory receptors located in the head. This may result in tonic modifications that interfere with the maintenance of posture and the generation of voluntary movements.
In normal motor development, complete control of the head is only achieved at six months of age after the child is able to have coordinated control of flexors, extensors and flexor sides (9).
Physical therapy methods are used for the treatment of neuromotor disorders arising from CP. However, positive clinical results stemming from these methods still need quantifying. Electromyography (EMG) is a technical resource developed for evaluating and recording electrical activity produced by contractions of striated skeletal muscles. By recording electromyographic data it is possible to infer the variations in polarization of the muscle fiber membranes located between the recording electrodes and measure muscle activity for a particular task or posture (10, 11).
Given the above information, to broaden the understanding of techniques facilitating head control, the aim of this study was to investigate the electromyographic activity of muscles involved in head control in the frontal, sagittal and transverse planes. This was performed through handling at key points on the control objective transfer of weight and body stability.
Materials and methods
Participant
A seven-year-old female diagnosed with cerebral palsy and West syndrome was used in this study. A clinical evaluation found an athetoid-spastic component, a topographic change of tone in quadriplegia, and a graduate V motor level, according to the Classification System Gross Motor Function (12). This study was approved by the Ethics Committee on Human Research of the Federal University of Health Sciences of Porto Alegre UFCSPA, in the opinion paragraph: 1463/11. Data were collected after providing information about the research objectives and informed consent was obtained from responsible person.
Data collection
For the EMG signal, a Miotool 400 (Miotec; Brazil) device was used with a sampling frequency of 2000Hz/canal with four channels and connected to a computer (DELL, Vostro 1400, Windows Vista), through Miographs software. The signal capture was performed using Ag/AgCl electrodes with self-adhesive bipolar configurations, diameter 2.2 cm, manufactured by Miotrace. The center to center distance between the electrodes was 20 mm, as recommended by SENIAM (13). To carry out the collection there was a reduction of skin impedance by aseptic and light abrasion with cotton soaked in alcohol (70%), based on the guidelines of the International Society of Electrophysiology and Kinesiology. To follow the trajectory of the muscle action potential, ensuring a better ability to get the EMG signal, the electrodes were positioned along the muscle fibers (14).
The electrodes were positioned to allow the capture of EMG signals from muscles involved in the control of the head. To check the activity of the extensor muscle, cervical and thoracic electrodes were placed over the muscle bellies, 2 cm lateral to the vertebral spinous processes at the levels of C7 and T10. The record of flexor control was obtained by capturing the muscle activity signal for the sternocleidomastoid (SCM) muscle, taking into account the activity of the flexor muscle control in the frontal and sagittal planes (8.15; Fig. 1 A). The reference electrode was attached to the left tibial tuberosity.
The postures used during the registration of the signals were: I) Posture 1 prone, with the support of the ventral trunk over a wedge placement of 25 cm, glenohumeral flexion range of motion approximately 90º (Fig. 1 B); II) Posture 2 in right lateral decubit on the floor, glenohumeral abduction range of motion of approximately 60º. This position was held in stabilizing the elbow key point on the side of the support due to the inability of active control of the shoulder girdle, seeking better alignment (Fig 1 C).
The recording of muscle activity at rest was obtained after the child was placed in the positions described above. The second record of muscle activity was performed by handling at key points of control for weight transfer over the hip, as illustrated in Figure 1. The signal capture was carried out over five seconds for each position, with the participation of a researcher handling the child in all postures and another evaluator collecting the signs.
Data Analysis
The signal was treated through the use of a fourth-order Butterworth filter with a cutoff frequency and type bandpass of 20450 Hz, for the acquisition of the full spectrum of the EMG record and gain1000 Hz (13). After conducting the normalization by peaks, the signal used was the root mean square (RMS), which assesses the level of activity of the EMG signal (16). For each record, in all postures and muscles evaluated, we used the highest value obtained by the EMG.
Results
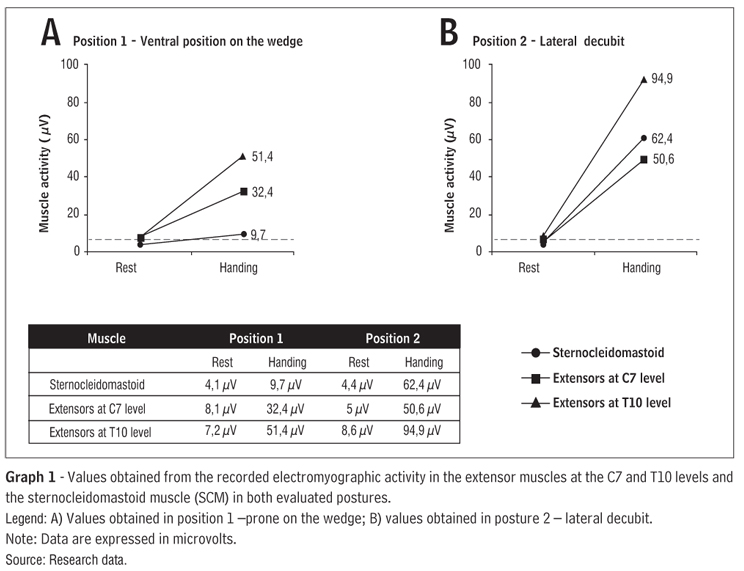
The electromyographic signal of the extensor and flexor muscles in the cervical region was intensified by handling for weight transfer in hip key points in both postures. The base signal was taken at rest in the prone position on the wedge and was expanded during the weight transfer to the hip in the three points assessed. Recording of the electromyographic signal at all points evaluated (SCM, C7, and T10) was highest in position 2 when compared to position 1 (Graph 1). Results are expressed as mean values of RMS electromyographic signal.
Discussion
The results showed increased electromyographic signals throughout handling in both positions and in all segments/muscles evaluated, when compared to the signal recorded at rest. Overall, the increased muscle activity at all evaluated points was higher when taking weight on the hip was held in position 2 (lateral) compared to taking weight in position 1 (prone on the wedge).
The Bobath concept neuroevolutivo is widely used for the treatment rehabilitation sensorimotor sequelae after lesions (17, 18). Among other techniques, it uses the exchanges in posture sequentially, obeying the order of acquisition of motor skills along the normal psychomotor development (NPMD) milestones (6). The ventral and lateral decubit postures are adopted by children during the NPMD. The reactions development rectification occurs initially in the prone position by enhancing the activity of the extensor muscles of the neck and upper trunk.
The control of the flexor muscles in the sagittal and frontal regions develops, thus requiring coordinated activity between these muscle groups at the end of the sixth month,, as a sign of the maturity of head control (9, 19, 20).
This concept is often chosen primarily for the treatment of the sequelae of sensorimotor CP. However, most studies aimed at the quantification of the results by means of facilitation techniques have methodological limitations making it impossible to draw conclusions about its effectiveness as a treatment (17, 21). Furthermore, much of the available literature exposes the positive effects of the concept only in adult patients with acquired brain injury (22, 23).
The Bobath concept advocates the use of manual control through the therapist's handling at key points to induce, limit, modulate, or restore typical movement patterns within the context of a specific task. A major barrier in evaluating the therapeutic efficacy of this concept is the lack of unification of handlings and postures used during therapy (21). In this context, the EMG recording becomes an attractive tool for the quantification of stimulus-response techniques for facilitating the acquisition of reactions in different forms of posture rectification and confirming the usefulness of physical therapy rehabilitation techniques (24, 25).
In this study we observed that the transfer of weight to the hip was able to induce facilitation of cervical control. The transfer and maintenance of body weight in regions opposite to that want increased muscular activity, seems to be the basis of the facilitation process of rectification reactions, allowing greater control of muscle activity, motor skill development, and posture correction. The handle used in this study is based on the fact that biomechanical weight transfer at the hip facilitates the development of the muscle torque required for lifting and straightening the head in both decubitus. This provides the child with their first experiences in sensorimotor satisfactory rectification in these postures, the first step for subsequent acquisition of motor skill neck control (6).
One hypothesis that could support the increased muscle activity by facilitating transfer of weight is that by handling, power would put the mechanical advantage of muscles in length-tension. This allows the sarcomeres to remain at a more facilitatory length for establishing actin-myosin bridges, muscle contraction, and consequent generation of tension.
Muscle activity in the studied region was greater when weight transfer occurred obliquely (child positioned in the lateral decubit position) as opposed to a weight shift only vertically (obtained in the ventral posture on the wedge). Possibly, the weight transfer, when performed obliquely to the plane of support, resulted in a greater ability to facilitate SCM muscle activity. The activation of the SCM is crucial in the development of cervical control and head movement in the sagittal, frontal, and transverse planes. Additionally, it facilitates subsequent maturation of head control during NPMD (26). The SCM typically has a reduced activity in children with abnormal tone type spasticity. This is because motor development does not occur satisfactorily due to the difficulty in overcoming the standard trunk extender, resulting from changes in modulation of pathways ventral-medial motion control (26).
Responses to sensory feedback provided by the therapist's hands could also represent the beginning of an evoked response in the CNS, not only reactive, but proactively to the tactile stimuli of pressure. The power generation mechanism of movement programs or the generation of a specific engine would be made possible by facilitating the handlings in different positions; this is due to the construction of the motor engram that depends on previous sensory-motor experience (27).
Handling key points of control weight transfer in the hip resulted in increased EMG activity in all muscle segments analyzed and in both decubitus. The facilitation seems to be more pronounced when the weight is supported obliquely to the support base. Thus, the adoption of the lateral decubit could be more beneficial to the acquisition of neck control (28).
Our hypothesis was that the use of the lateral decubit, repeated and sustained, with proper handling, alignment, and weight transfer, may facilitate more muscle activity in the neck and upper trunk than handling in the prone position on the wedge. The results presented here have direct implications in the process of neurological rehabilitation of children, as lateral decubit handling could be more beneficial for the development of head control that transfers the weight on the prone position on the wedge. Since this is a cross-sectional analysis of only one case, more research is needed to elucidate the effects of these posture-handling facilitations on the acquisition and maintenance of cervical control in all planes of motion.
References
- 1. Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, Dan B, et al. Proposed definition and classification of cerebral palsy. Dev Med Child Neurol. 2005;47(8):571-6.
- 2. Camerota F, Galli M, Celletti C, Vimercati S, Cimolin V, Tenore N, et al. Quantitative effects of repeated muscle vibrations on gait pattern in a 5-year-old child with cerebral palsy. Case Report Med. 2011;2011:359126.
- 3. Berker AN, Yalcin MS. Cerebral palsy: orthopedic aspects and rehabilitation. Pediatr Clin North Am. 2008;55(5):1209-25.
- 4. Wallace SJ. Epilepsy in cerebral palsy. Dev Med Child Neurol. 2001;43(10):713-7.
- 5. Asano E, Chugani DC, Juhasz C, Muzik O, Chugani HT. Surgical treatment of West syndrome. Brain Dev. 2001;23(7):668-76.
- 6. Graham JV, Eustace C, Brock K, Swain E, Irwin-Carruthers S. The Bobath concept in contemporary clinical practice. Top Stroke Rehabil. 2009;16(1):57-68.
- 7. Kollen BJ, Lennon S, Lyons B, Wheatley-Smith L, Scheper M, Buurke JH, et al. The effectiveness of the Bobath concept in stroke rehabilitation: what is the evidence? Stroke. 2009;40(4):e89-97.
- 8. Bigongiari A, de Andrade e Souza F, Franciulli PM, Sel R Neto, Araujo RC, Mochizuki L. Anticipatory and compensatory postural adjustments in sitting in children with cerebral palsy. Hum Mov Sci. 2011;30(3):648-57.
- 9. Bly L. Components of normal movement during the first year of life and abnormal motor development. Chicago: NDT; 1993.
- 10. Gosselin G, Rassoulian H, Brown I. Effects of neck extensor muscles fatigue on balance. Clin Biomech. 2004;19(5):473-9.
- 11. Christie A, Greig Inglis J, Kamen G, Gabriel DA. Relationships between surface EMG variables and motor unit firing rates. Eur J Appl Physiol. 2009;107(2):177-85.
- 12. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214-23.
- 13. Hermens HJ, Freriks B, Disselhorst-Klug C, Rau G. Development of recommendations for SEMG sensors and sensor placement procedures. J Electromyogr Kinesiol. 2000;10(5):361-74.
- 14. Young AJ, Hargrove LJ, Kuiken TA. The effects of electrode size and orientation on the sensitivity of myoelectric pattern recognition systems to electrode shift. IEEE Trans Biomed Eng. 2011;58(9):2537-44.
- 15. Cioni M, Pisasale M, Abela S, Belfiore T, Micale M. Physiological electromyographic activation paterns of trunk muscles during walking. The Open Rehabilitation Journal. 2010;3:136-42.
- 16. Robertson DGE, Caldwell GE, Hamill J, Kamen G, Whittlesey SN. Research methods in biomechanics. Champaign: Human Kinetics; 2004.
- 17. Paci M. Physiotherapy based on the Bobath concept for adults with post-stroke hemiplegia: a review of effectiveness studies. J Rehabil Med. 2003;35(1):2-7.
- 18. Huseyinsinoglu BE, Ozdincler AR, Krespi Y. Bobath Concept versus constraint-induced movement therapy to improve arm functional recovery in stroke patients: a randomized controlled trial. Clin Rehabil. 2012;26(8):705-15.
- 19. Forssberg H. Neural control of human motor development. Curr Opin Neurobiol. 1999;9(6):676-82.
- 20. Dudek-Shriber L, Zelazny S. The effects of prone positioning on the quality and acquisition of developmental milestones in four-month-old infants. Pediatr Phys Ther. 2007;19(1):48-55.
- 21. Levin MF, Panturin E. Sensorimotor integration for functional recovery and the Bobath approach. Motor Control. 2011;15(2):285-301.
- 22. Wang RY, Chen HI, Chen CY, Yang YR. Efficacy of Bobath versus orthopaedic approach on impairment and function at different motor recovery stages after stroke: a randomized controlled study. Clin Rehabil. 2005;19(2):155-64.
- 23. Kim B, Gerlinde H, Gerhard R, Susan C. Does physiotherapy based on the Bobath concept, in conjunction with a task practice, achieve greater improvement in walking ability in people with stroke compared to physiotherapy focused on structured task practice alone? A pilot randomized controlled trial. Clin Rehabil. 2011;25(10):903-12.
- 24. Mayston MJ, Harrison LM, Stephens JA. A neurophysiological study of mirror movements in adults and children. Ann Neurol. 1999;45(5):583-94.
- 25. Crow J, Pizzari T, Buttifant D. Muscle onset can be improved by therapeutic exercise: a systematic review. Phys Ther Sport. 2011;12(4):199-209.
- 26. Bly L. Motor skill acquisition in the first year: an illustrated guide to normal development. San Antonio: Therapy Skill Builders; 1993.
- 27. Velickovic TD, Perat MV. Basic principles of the neurodevelopmental treatment. Medicina. 2005;42(41):112-20.
- 28. Ratliff-Schaub K, Hunt CE, Crowell D, Golub H, Smok-Pearsall S, Palmer P, et al. Relationship between infant sleep position and motor development in preterm infants. J Dev Behav Pediatr. 2001;22(5):293-9.
Publication Dates
-
Publication in this collection
03 Feb 2014 -
Date of issue
Dec 2013
History
-
Received
18 July 2012 -
Accepted
26 Sept 2013