Abstract
Introduction:
In the Chronic Obstructive Pulmonary Disease (COPD) both pulmonary and systemic condition increase dyspnea, intolerance to exercise and inactivity.
Objective:
To evaluate possible association between Hand Grip Strength (HGS) and the distance covered in the Six-Minute Walk Test (6MWT) in patients with Chronic Obstructive Pulmonary Disease (COPD).
Methods:
A cross-sectional study that evaluated 34 patients with COPD from moderate to very severe stages. The HGS test was performed with a manual hydraulic dynamometer (Jamar®, California, USA) with three bilateral measures, allowing 60-seconds rest time in-between measurements. Afterwards, the patients were submitted to the 6MWT along a 30-meters level corridor following the rules of the American Thoracic Society.
Results:
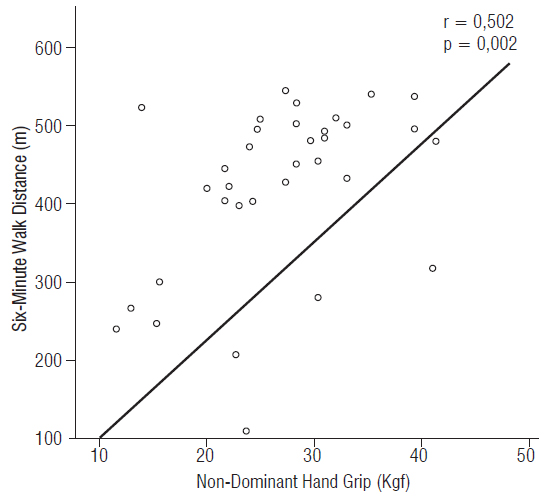
Average age 62.7±7.2 years old, body mass index 26.7±6.9 Kg/m². The value of the HGS in the dominant hand was 28.0±8.7 Kgf and in the non-dominant hand was 26.7±7.7 Kgf (99.2% of the predicted value and 106.3% of the predicted value, respectively). The subjects covered in average 421.0±110.4 meters in the 6MWT and there has been detected direct and significant correlation between the distance covered and the HGS of the dominant hand (r=0,430; p=0,011) and non-dominant (r=0,502; p=0,002). The patients with COPD that presented lower HGS also covered less distance in the 6MWT.
Conclusion:
The hand grip strength was directly associated with the functional capacity assessed through the distance covered in the Six-Minute Walk Test in the evaluated trial.
Keywords:
Hand Strength; Exercise Test; Pulmonary Disease; Chronic Obstructive
Resumo
Introdução:
Nos portadores de Doença Pulmonar Obstrutiva Crônica (DPOC), a disfunção pulmonar, as manifestações sistêmicas e o aumento da dispneia podem conduzir à piora progressiva do condicionamento físico, à inatividade e intolerância ao exercício físico.
Objetivo:
avaliar possível associação entre a força de preensão palmar (FPP) e a distância percorrida no Teste de Caminhada de Seis Minutos (TC6M) em portadores de DPOC.
Métodos:
Estudo transversal que avaliou 34 portadores de DPOC com estadiamento entre moderado a muito severo. A FPP foi realizada com dinamômetro hidráulico manual (Jamar®, Califórnia, EUA) com três medidas bilateralmente, respeitando um tempo de descanso de 60 segundos entre as medidas. Posteriormente, os pacientes foram submetidos ao TC6M em um corredor plano de 30 metros, seguindo as normas da American Thoracic Society.
Resultados:
Média de idade de 62,7±7,2 anos, índice de massa corporal 26,7±6,9 Kg/m². O valor da FPP na mão dominante foi 28,0±8,7 Kgf e da mão não dominante foi 26,7±7,7 Kgf (99,2% do predito e 106,3% do predito, respectivamente). Os sujeitos percorreram em média 421,0±110,4 metros no TC6M tendo sido detectada correlação direta e significativa entre a distância percorrida e a FPP da mão dominante (r=0,430; p=0,011) e não-dominante (r=0,502; p=0,002). Os portadores de DPOC que apresentaram menor FPP apresentaram menor distância no TC6M.
Conclusão:
A força de preensão palmar esteve diretamente associada à capacidade funcional avaliada através da distância percorrida no Teste de Caminhada de Seis Minutos na amostra avaliada.
Palavras-chave:
Força da mão; Teste de Esforço; Doença Pulmonar; Obstrutiva Crônica
Introduction
The Chronic Obstructive Pulmonary Disease (COPD) is characterized by persistent and progressive obstruction of the superior airways, associated with an enhanced chronic inflammatory response to inhalation of pollutants/particles or noxious gases11. GOLD - Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnoses, Management, and Prevention of Chronic Obstructive Pulmonary Disease (updated 2015).. The inflammatory cells are active and there is an increase in pro-inflammatory plasma cytokine levels in the systemic circulation, causing oxidative stress that will result in musculoskeletal disorders and reduction of the functional capacity22. Borel B, Provencher S, Saey D, Maltais, F. Responsiveness of Various Exercise-Testing Protocols to Therapeutic Interventions in COPD. Pulm Med. 2013;2013:410748.. The pulmonary dysfunction, the systemic manifestations and the increase of dyspnea can lead to progressive worsening of the physical conditioning, inactivity and physical exercise intolerance33. Sun KS, Lin MS, Chen YJ, Chen YY, Chen SCC, Chen W. Is asymptomatic peripheral arterial disease associated with walking endurance in patients with COPD? Int J Chron Obstruct Pulmon Dis. 2015;10:1487-92..
As a result, the COPD patient adopts a more sedentary lifestyle that worsens the quality of life and is the determining factor to the progression of the disease22. Borel B, Provencher S, Saey D, Maltais, F. Responsiveness of Various Exercise-Testing Protocols to Therapeutic Interventions in COPD. Pulm Med. 2013;2013:410748.), (44. Pepin V, Saey D, Laviolette L, Maltais F. Exercise capacity in chronic obstructive pulmonary disease: mechanisms of limitation. COPD. 2007;4(3):195-204.. The evaluation of the physical performance of patients with COPD by using sub-maximal and non-invasive tests, like the Six-Minute Walk Test (6MWT), besides being easy to apply, can also reflect in activities of daily life, physical fitness, functional capacity55. Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/ American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428-46., as well as monitor the effectiveness of several treatments due to its good correlation with the maximal oxygen uptake (VO2max)66. Pires SR, Oliveira AC, Parreira VF, Britto RR. Teste de caminhada de seis minutos em diferentes faixas etárias e índices de massa corporal. Rev Bras Fisioter. 2007;11(2):147-51.. Another important method to evaluate the changes of peripheral muscle strength, as this is one of the most important extra pulmonary manifestations of the COPD physiopathology77. Rausch-Osthoff AK, Kohler M, Sievi NA, Clarenbach CF, van Gestel AJ. Association between peripheral muscle strength, exercise performance, and physical activity in daily life in patients with Chronic Obstructive Pulmonary Disease. Multidiscip Respir Med. 2014;9(1):37., is the Hand Grip Strength (HGS). The HGS has as principle to estimate the musculoskeletal function through good reproducibility for the measurement of maximal manual voluntary handgrip strength, being considered a good index for overall muscle strength, and it can also reflect the impairment of the functional capacity88. Martin FG, Nebuloni CC, Najas MS. Correlação entre estado nutricional e força de preensão palmar em idosos. Rev Bras Geriatr Gerontol. 2012;15(3):493-504..
We hypothesized that the reduction of hand grip strength is associated with the decrease of functional capacity in patients with COPD. Therefore, our objective was to evaluate the association between hand grip strength and the distance covered in the Six-Minute Walk Test in patients with Chronic Obstructive Pulmonary Disease.
Methods
This descriptive, prospective and transversal study was carried out in the Pulmonary Rehabilitation Program at the Santa Cruz Hospital. It was approved by the Research Ethics Committee of the University of Santa Cruz do Sul (protocol number 435093/2013). The study population was composed of patients diagnosed with COPD in accordance with the international criteria11. GOLD - Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnoses, Management, and Prevention of Chronic Obstructive Pulmonary Disease (updated 2015)..
There were forty-one COPD patients eligible in the program, however, only Thirty-four met the following inclusion criteria: age between 40 and 80 years old, with clinical diagnosis of COPD through the pulmonary function test by spirometry and clinically stable. COPD patients with musculoskeletal disorders, neurological sequelae that would affect the locomotor system and cognitive deficit, skin lesions on the feet and/or superior limbs, exacerbations of the disease within the 30 days prior to the study and the ones with lung cancer diagnosis, were excluded.
Clinical Variables
Analysis of the expiratory volume forced in the 1º second (FEV1), relation expiratory volume forced in the 1º second/vital capacity forced (FEV1/VCF), Socio-demographic and clinical data (gender, age, Body Mass Index - BMI, time of the diagnosis of the COPD, smoking history, dyspnea by the scale Medical Research Council - MRC and index of BODE - Body Mass-Index: Airflow Obstruction, Dyspnea and Exercise Capacity).
Handgrip Strength
The HGS test was performed with a manual hydraulic dynamometer (Jamar®, California, USA), following the recommendations of The American Society of Hands Therapists. The patients remained seated, with the shoulder abducted, elbow flexed at 90º, forearm in neutral position of prono-supination and the wrist joint between 0º and 30º of dorsiflexion. Three bilateral measures were taken, allowing 60 seconds rest time in-between measurements, and the average of the measurements of each participant was separately calculated. The values obtained compared with the ones predicted as reported by Luna-Heredia et al.99. Luna-Heredia E, Martín-Peña G, Ruiz-Galiana J. Handgrip dynamometry in healthy adults. Clin Nutr. 2005;24(2):250-8. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-7..
6MWT
The 6MWT was performed according to the American Thoracic Society standards to measure the distance the study participants were able to walk within a 6-minute period1010. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-7.. The study participants were asked to walk as far as possible at a self-determined speed. No other guidance was provided. The test was carried out by an experienced physical therapist. The percentage predicted in the 6MWT distance was calculated considering gender, age, height, and weight of each subject based on the equation by Enright, et al.1111. Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783-5..
Statistical analysis
The software SPSS (version 20.0) was used to verify the normality of the distribution of data through the test of Shapiro-Wilk, and the results were shown in frequency, average ± standard deviation. The association between the variables was analyzed by using Spearman’s correlation test and the analysis of the variance for multiple comparisons (ANOVA) by using the post hoc of Tukey test. It was considered significant a p < 0.05.
Results
The clinical characteristics and the performance of the 34 COPD patients in the tests are shown in Table 1.
Direct correlations were observed between the measures of the HGS of the dominant hand and the non-dominant hand with the distance covered in the 6MWT in meters (r = 0.430 p = 0.011) and (r = 0.502; p = 0.002), respectively (Figure 1 and 2).
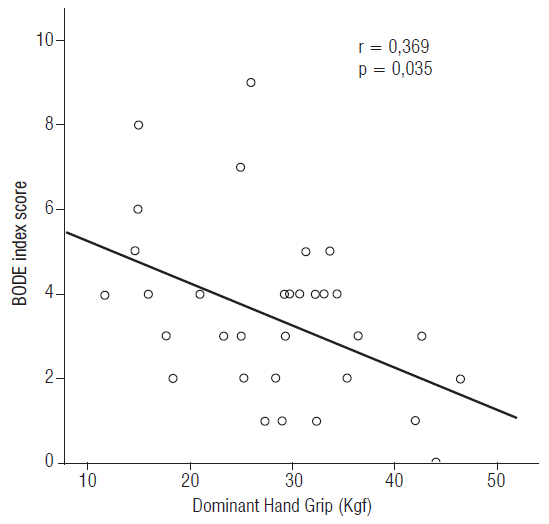
The HGS also correlated itself significantly and inversely with the BODE Index (Figure 3). It is possible to observe a reduction of HGS related with the worsening of the patients quality of life, which was determined by the quartiles of the BODE index, as described in Table 2, although no significant statistical difference was found (values of p ranging between 0.18 and 0.96).
Discussion
Our study aimed to analyze the association between hand grip strength and the distance covered in the 6MWT by patients with COPD and we found that the changes that occurred in HGS are directly related with the subject´s worsening of survival range in the performance of this test. Our results meet the literature that states that hand grip strength and 6MWT are reduced in patients with COPD particularly in those with hyperinflation1414. Cortopassi F, Divo M, Pinto-Plata V, Celli B. Resting handgrip force and impaired cardiac function at rest and during exercise in COPD patients. Respir Med. 2011;105(5):748-54. and patients with mainly moderate and severe COPD experience a loss of peripheral muscle strength and endurance, exercise capacity and general quality of life1515. Calik-Kutukcu E, Savci S, Saglam M, Vardar-Yagli N, Inal-Ince D, Arikan H, et al. A comparison of muscle strength and endurance, exercise capacity, fatigue perception and quality of life in patients with chronic obstructive pulmonary disease and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014;14:6..
The loss of muscle strength of COPD patients can be related to exercise restrictions which reflect alterations in the respiratory tract, cardiovascular, neuromuscular and neurosensory system in highly variable combinations with multifactorial interactions1515. Calik-Kutukcu E, Savci S, Saglam M, Vardar-Yagli N, Inal-Ince D, Arikan H, et al. A comparison of muscle strength and endurance, exercise capacity, fatigue perception and quality of life in patients with chronic obstructive pulmonary disease and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014;14:6.), (1616. Rabinovich RA, Vilaró J, Roca J. Evaluation exercise tolerance in COPD patients: the 6-minute walking test. Arch Bronconeumol. 2004;40(2):80-5.. The changes in the peripheral musculature strength and in muscle mass can be associated with a systemic inflammation, reduction of the capillaries in the fibers, and also with the oxidative stress1515. Calik-Kutukcu E, Savci S, Saglam M, Vardar-Yagli N, Inal-Ince D, Arikan H, et al. A comparison of muscle strength and endurance, exercise capacity, fatigue perception and quality of life in patients with chronic obstructive pulmonary disease and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014;14:6.), (1717. Nussbaumer-Ochsner Y, Rabe KF. Systemic manifestations of COPD. Chest. 2011;139(1):165-73., which is more accentuated in the lower limbs.
On the other hand, our results meet the findings of those in the studies, that states that the muscular strength of the upper limbs of COPD patients can be preserved in the distal muscles, due to the fact that they are used in the daily activities, and reduced in the proximal muscles due to increased dyspnea during the activity sustained by the arm1818. Malaguti C, Napolis LM, Villaça D, Neder JA, Nery LE, Dal Corso S. Relationship between peripheral muscle structure and function in patients with chronic obstructive pulmonary disease with different nutritional status. J Strength Cond Res. 2011;25(7):1795-803.), (1919. Miranda EF, Malaguti C, Dal Corso S. Peripheral muscle dysfunction in COPD: lower limbs versus upper limbs. J Bras Pneumol. 2011;37(3):380-8.), (2020. Oliveira MF, Zelt JT, Jones JH, Hirai DM, O’Donnell DE, Verges S, et al. Does impaired O2 delivery during exercise accentuate central and peripheral fatigue in patients with coexistent COPD-CHF? Front Physiol. 2015;5:514.. However, studies highlight that there is a very strong correlation between the HGS and the strength of the other peripheral muscles, like the ones evaluated by the strength of the flexors of the elbow and the knee, as well as the respiratory muscle strength (maximal inspiratory muscle pressure and maximum voluntary ventilation)1515. Calik-Kutukcu E, Savci S, Saglam M, Vardar-Yagli N, Inal-Ince D, Arikan H, et al. A comparison of muscle strength and endurance, exercise capacity, fatigue perception and quality of life in patients with chronic obstructive pulmonary disease and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014;14:6.), (2121. Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM. Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am Geriatr Soc. 2003;51(5):636-41.. In COPD the supply of oxygen to the peripheral and respiratory muscles may be deficient as a result of hypoxemia2222. Santos DB, Viegas CAA. Correlation of levels of obstruction in COPD with lactate and six-minute walk test. Rev Port Pneumol. 2009;15(1):11-25..
The response obtained in the 6MWT reflects the effort made in daily life activities and the short distance covered in this test translates such limitations2121. Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM. Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am Geriatr Soc. 2003;51(5):636-41.. This is because the intolerance to exercise of these subjects is of multifactorial construction involving more work and oxygen consumption by the respiratory muscles, the dysfunction of the skeletal muscles of the lower limbs and the mechanism of lung dynamic hyperinflation, acting alone or in conjunction2323. Nonato NL, Díaz O, Nascimento AO, Dreyse J, Jardim JR, Lisboa C. Behavior of Quality of Life (SGRQ) in COPD Patients According to BODE Scores. Arch Bronconeumol. 2015;51(7):315-21..
In the same way that the 6MWT influences the BODE index, we found, in our study, a direct association of HGS with the worsening of this index and the consequent worsening of survival of COPD patients. The BODE is considered an index of multidimensional2424. Moreira MAF, Medeiros GA, Boeno FP, Sanches PRS, Silva Jr DP, Müller AF. Oxygen desaturation during the six-minute walk test in COPD patients. J Bras Pneumol. 2014;40(3):222-8.), (2525. Chen X, May B, Di YM, Zhang AL, Lu C, Xue CC, et al. Oral Chinese herbal medicine combined with pharmacotherapy for stable COPD: a systematic review of effect on bode index and six minute walk test. PloS One. 2014;9(3):e91830., classification of the severity of COPD2626. Sferrazza Papa GF, Battaglia S, Solidoro P. Novelties in COPD prognosis: evolution of survival indexes. Minerva Med. 2015;106(2 Suppl 2):9-16.), (2727. Silva JRG, Vasconcelos TB, Macena RHM, Bastos VPD, Morano MTAP, Rocha EMM, et al. Análise do índice BODE em pacientes com DPOC severa submetidos a um programa de reabilitação pulmonar. J Health Biol Sci. 2013;1(3):108-15. where a score of 3 points or more is associated with an increase of mortality and exacerbation rates in patients with COPD2828. Martin JM, Carrizo SJ, Casanova C, Martinez-Camblor P, Soriano JB, Agusti AG, et al. Prediction of risk of COPD exacerbations by the BODE index. Respir Med. 2009;103(3):373-8.), (2929. Dreyse J, Díaz O, Repetto PB, Morales A, Saldías F, Lisboa C. Do frequent moderate exacerbations contribute to progression of chronic obstructive pulmonary disease in patients who are ex-smokers? Int J Chron Obstruct Pulmon Dis. 2015;10:525-33.), (3030. Mantoani LC, Hernandes NA, Guimarães MM, Vitorasso RL, Probst VS, Pitta F. Does the BODE index reflect the level of physical activity in daily life in patients with COPD? Rev Bras Fisioter. 2011;15(2):131-7..
Some limitations can be observed in our study, such as the sample size which does not allow us for many inferences and future perspectives, making it possible to evaluate the effectiveness of pulmonary rehabilitation thru improvement of muscle strength and consequently, the performance in the 6MWT.
Conclusion
The hand grip strength was directly associated with the performance in the Six-Minute Walk Test in our study, where the patients with COPD that presented a lower HGS in the dominant and non-dominant hand also covered less distance and worsening of survival. Further studies are necessary to identify how much the hand grip strength can influence the performance in the 6MWT in this population.
Support and funding
University of Santa Cruz do Sul-UNISC, DECIT/SCTIE-MS/FAPERGS/CNPq 1264-2551/13-1 and Hospital Santa Cruz - RS.
References
-
1GOLD - Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnoses, Management, and Prevention of Chronic Obstructive Pulmonary Disease (updated 2015).
-
2Borel B, Provencher S, Saey D, Maltais, F. Responsiveness of Various Exercise-Testing Protocols to Therapeutic Interventions in COPD. Pulm Med. 2013;2013:410748.
-
3Sun KS, Lin MS, Chen YJ, Chen YY, Chen SCC, Chen W. Is asymptomatic peripheral arterial disease associated with walking endurance in patients with COPD? Int J Chron Obstruct Pulmon Dis. 2015;10:1487-92.
-
4Pepin V, Saey D, Laviolette L, Maltais F. Exercise capacity in chronic obstructive pulmonary disease: mechanisms of limitation. COPD. 2007;4(3):195-204.
-
5Holland AE, Spruit MA, Troosters T, Puhan MA, Pepin V, Saey D, et al. An official European Respiratory Society/ American Thoracic Society technical standard: field walking tests in chronic respiratory disease. Eur Respir J. 2014;44(6):1428-46.
-
6Pires SR, Oliveira AC, Parreira VF, Britto RR. Teste de caminhada de seis minutos em diferentes faixas etárias e índices de massa corporal. Rev Bras Fisioter. 2007;11(2):147-51.
-
7Rausch-Osthoff AK, Kohler M, Sievi NA, Clarenbach CF, van Gestel AJ. Association between peripheral muscle strength, exercise performance, and physical activity in daily life in patients with Chronic Obstructive Pulmonary Disease. Multidiscip Respir Med. 2014;9(1):37.
-
8Martin FG, Nebuloni CC, Najas MS. Correlação entre estado nutricional e força de preensão palmar em idosos. Rev Bras Geriatr Gerontol. 2012;15(3):493-504.
-
9Luna-Heredia E, Martín-Peña G, Ruiz-Galiana J. Handgrip dynamometry in healthy adults. Clin Nutr. 2005;24(2):250-8. ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-7.
-
10ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-7.
-
11Enright PL. The six-minute walk test. Respir Care. 2003;48(8):783-5.
-
12Cuppari L. Guia de Medicina Ambulatorial e Hospitalar: Nutrição Clínica no Adulto. São Paulo: Manole; 2002.
-
13Pereira CA, Sato T, Rodrigues CS. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol. 2007;33(4):397-406.
-
14Cortopassi F, Divo M, Pinto-Plata V, Celli B. Resting handgrip force and impaired cardiac function at rest and during exercise in COPD patients. Respir Med. 2011;105(5):748-54.
-
15Calik-Kutukcu E, Savci S, Saglam M, Vardar-Yagli N, Inal-Ince D, Arikan H, et al. A comparison of muscle strength and endurance, exercise capacity, fatigue perception and quality of life in patients with chronic obstructive pulmonary disease and healthy subjects: a cross-sectional study. BMC Pulm Med. 2014;14:6.
-
16Rabinovich RA, Vilaró J, Roca J. Evaluation exercise tolerance in COPD patients: the 6-minute walking test. Arch Bronconeumol. 2004;40(2):80-5.
-
17Nussbaumer-Ochsner Y, Rabe KF. Systemic manifestations of COPD. Chest. 2011;139(1):165-73.
-
18Malaguti C, Napolis LM, Villaça D, Neder JA, Nery LE, Dal Corso S. Relationship between peripheral muscle structure and function in patients with chronic obstructive pulmonary disease with different nutritional status. J Strength Cond Res. 2011;25(7):1795-803.
-
19Miranda EF, Malaguti C, Dal Corso S. Peripheral muscle dysfunction in COPD: lower limbs versus upper limbs. J Bras Pneumol. 2011;37(3):380-8.
-
20Oliveira MF, Zelt JT, Jones JH, Hirai DM, O’Donnell DE, Verges S, et al. Does impaired O2 delivery during exercise accentuate central and peripheral fatigue in patients with coexistent COPD-CHF? Front Physiol. 2015;5:514.
-
21Rantanen T, Volpato S, Ferrucci L, Heikkinen E, Fried LP, Guralnik JM. Handgrip strength and cause-specific and total mortality in older disabled women: exploring the mechanism. J Am Geriatr Soc. 2003;51(5):636-41.
-
22Santos DB, Viegas CAA. Correlation of levels of obstruction in COPD with lactate and six-minute walk test. Rev Port Pneumol. 2009;15(1):11-25.
-
23Nonato NL, Díaz O, Nascimento AO, Dreyse J, Jardim JR, Lisboa C. Behavior of Quality of Life (SGRQ) in COPD Patients According to BODE Scores. Arch Bronconeumol. 2015;51(7):315-21.
-
24Moreira MAF, Medeiros GA, Boeno FP, Sanches PRS, Silva Jr DP, Müller AF. Oxygen desaturation during the six-minute walk test in COPD patients. J Bras Pneumol. 2014;40(3):222-8.
-
25Chen X, May B, Di YM, Zhang AL, Lu C, Xue CC, et al. Oral Chinese herbal medicine combined with pharmacotherapy for stable COPD: a systematic review of effect on bode index and six minute walk test. PloS One. 2014;9(3):e91830.
-
26Sferrazza Papa GF, Battaglia S, Solidoro P. Novelties in COPD prognosis: evolution of survival indexes. Minerva Med. 2015;106(2 Suppl 2):9-16.
-
27Silva JRG, Vasconcelos TB, Macena RHM, Bastos VPD, Morano MTAP, Rocha EMM, et al. Análise do índice BODE em pacientes com DPOC severa submetidos a um programa de reabilitação pulmonar. J Health Biol Sci. 2013;1(3):108-15.
-
28Martin JM, Carrizo SJ, Casanova C, Martinez-Camblor P, Soriano JB, Agusti AG, et al. Prediction of risk of COPD exacerbations by the BODE index. Respir Med. 2009;103(3):373-8.
-
29Dreyse J, Díaz O, Repetto PB, Morales A, Saldías F, Lisboa C. Do frequent moderate exacerbations contribute to progression of chronic obstructive pulmonary disease in patients who are ex-smokers? Int J Chron Obstruct Pulmon Dis. 2015;10:525-33.
-
30Mantoani LC, Hernandes NA, Guimarães MM, Vitorasso RL, Probst VS, Pitta F. Does the BODE index reflect the level of physical activity in daily life in patients with COPD? Rev Bras Fisioter. 2011;15(2):131-7.
Publication Dates
-
Publication in this collection
Jul-Sep 2017
History
-
Received
03 Dec 2015 -
Accepted
25 Oct 2016