Abstract
Introduction:
Alternative testing for X-rays in the assessment of the spine have the advantage of not causing radiation problems, but need to be validated.
Objective:
To propose a clinical test for assessment of the cervical spine based on the frontal-mental line inclination, identifying its concurrent validity in relation to the gold standard and determining its clinical applicability.
Method:
The present study was separated into two phases: (1) Test of Frontal-mental Line Inclination’s (TFMLI) validation protocol (evaluation of head position using X-ray analysis and computerized photogrammetry and assessment of cervical curvature using X-ray analysis and the TFMLI) (n = 35); (2) testing the possibility of performing the TFMLI with a universal goniometer (n = 23).
Results:
In phase 1, for the evaluation of head position, the gold standard and photogrammetry showed high and significant correlation (r = 0.602; p < 0.001). When evaluating cervical curvature, the gold standard and the TFMLI showed high and significant correlation (r = 0.597; p = 0.019). In phase 2, for the evaluation of head position, photogrammetry and goniometry showed high and significant correlation (rs = 0.662; p < 0.001). For the evaluation of cervical curvature, the TFMLI performed with photographs and with goniometry showed almost perfect and significant correlation (r = 0.969; p < 0.001).
Conclusion:
The TFMLI is suitable for an initial evaluation of the cervical spine posture of individuals with anterior head position and can be applied in clinical practice with the use of a universal goniometer.
Keywords:
Cervical Vertebrae; Neck; Evaluation; Validation Studies; Lordosis
Resumo
Introdução:
Testes alternativos ao exame de Raio-X na avaliação da coluna vertebral têm a vantagem de não causarem problemas devido a radiação, mas necessitam ser validados.
Objetivo:
Propor um teste clínico para avaliação da coluna cervical, baseado na inclinação do eixo frontal-mentoniano, identificar sua validade concorrente em relação ao padrão ouro e determinar sua aplicabilidade clínica.
Método:
O presente estudo foi separado em duas fases: (1) protocolo de validação do Teste de Inclinação do Eixo Frontal-Mentoniano (TFMLI) (avaliação da posição da cabeça por meio de Raios-X e fotogrametria computadorizada e avaliação da curvatura cervical por meio de Raios-X e pelo TFMLI) (n = 35); (2) testagem da possibilidade de realizar o TFMLI com um goniômetro universal (n = 23).
Resultados:
Na fase 1, para avaliação da posição da cabeça, o padrão ouro e a fotogrametria mostraram alta e significativa correlação (r = 0,602; p < 0,001). Para avaliação da curvatura cervical, o padrão ouro e o TFMLI mostraram alta e significativa correlação (r = 0,597; p = 0,019). Na fase 2, para avaliação da posição da cabeça, a fotogrametria e a goniometria mostraram correlação alta e significativa (rs = 0,662; p < 0,001). Para avaliação da curvatura cervical, o TFMLI realizado por meio de fotografias e por meio de goniometria apresentaram correlação praticamente perfeita e significativa (r = 0,969; p < 0,001).
Conclusão:
O TFMLI é adequado para uma avaliação inicial da postura da coluna cervical de indivíduos que apresentem uma posição de cabeça anterior e pode ser aplicado na prática clínica através do uso de um goniômetro universal.
Palavras-chave:
Vértebras Cervicais; Pescoço; Avaliação; Estudos de Validação; Lordose
Resumen
Introducción:
Las pruebas alternativas de rayos X en la evaluación de la columna vertebral tienen la ventaja de no causar problemas de radiación, pero deben validarse.
Objetivo:
Proponer un ensayo clínico para la evaluación de la columna cervical basada en la inclinación de la línea frontal-mental, identificar su validez concurrente en relación con el patrón oro y determinar su aplicabilidad clínica.
Métodos:
El presente estudio se separó en dos fases: (1) protocolo de validación do Prueba de Inclinación del Eje Frontal-Mentoniano (TFMLI) (evaluación de la posición de la cabeza mediante rayos X y mediante fotogrametría computarizada y evaluación de la curvatura cervical usando Rayos X y TFMLI) (n = 35); (2) probando la posibilidad de realizar TFMLI con un goniómetro universal (n = 23).
Resultados:
En la fase 1, para la evaluación de la posición de la cabeza, el patrón oro y la fotogrametría mostraron una correlación alta y significativa (r = 0,602; p < 0,001). Al evaluar la curvatura cervical, el patrón de oro y TFMLI mostraron una correlación alta y significativa (r = 0,597; p = 0,019). En la fase 2, para la evaluación de la posición de la cabeza, la fotogrametría y la goniometría mostraron una correlación alta y significativa (rs = 0,662; p < 0,001). Para la evaluación de la curvatura cervical, el TFMLI realizado mediante fotografías y por goniometría presentó una correlación casi perfecta y significativa (r = 0,969; p < 0,001).
Conclusión:
El TFMLI es adecuado para una evaluación inicial de la postura de la columna cervical de individuos que presentan una posición anterior de la cabeza y se puede aplicar en la práctica clínica mediante el uso de un goniómetro universal.
Palabras clave:
Vértebras Vervicales; Cuello; Evaluación; Estudios de Validación; Lordosis
Introduction
The cervical spine has the necessary lordotic curvature to compensate the thoracic spine’s kyphosis11. Gay RE. The curve of spine cervical. J Manipulative Physiol Ther. 1993;16(9):591-4. which is associated with the neutral position of the head22. Mani S, Sharma S, Omar B, Ahmad K, Muniandy Y, Singh DKA. Quantitative measurements of forward head posture in a clinical settings: a technical feasibility study. Eur J Physiother. 2017;19(3):119-23.. An increase or decrease in physiological cervical lordosis may not necessarily imply an abnormal head position, although there is the expectation of a “straight” cervical spine, for example, being associated with a previously projected head. Moreover, considering that abnormalities in the cervical spine may be associated with pain and impaired range of motion, it is understood that these signs and symptoms could be reversed with improved posture33. Saunders ES, Woggon D, Cohen C, Robinson DH. Improvement of cervical lordosis and reduction of forward head posture with anterior head weighting and proprioceptive balancing protocols. J Vertebr Subluxation Res. 2003;1-5.), (44. Lennon J, Shealy CN, Cady RK, Matta W, Cox R, Simpson WF. Postural and respiratory modulation of autonomic function, pain and health. AJPM. 1994;4(1):36-9.. Thus, an initial assessment that considers the position of the cervical spine and head is one of the first steps in the intervention of cervical spine disorders.
The X-ray examination, although considered a gold standard for spinal assessment55. Allen S, Parent E, Khorasani M, Hill DL, Lou E, Raso JV. Validity and reliability of active shape models for the estimation of cobb angle in patients with adolescent idiopathic scoliosis. J Digit Imaging. 2008;21(2):208-18.), (66. Tayyab NA, Samartzis D, Altiok H, Shuff CE, Lubicky JP, Herman J, et al. The reliability and diagnostic value of radiographic criteria in sagittal spine deformities: comparison of the vertebral wedge ratio to the segmental cobb angle. Spine. 2007;32(16):451-9., can often lead to problems due to radiation exposure77. Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE. Breast cancer mortality after diagnostic radiography: findings from the U.S. scoliosis cohort study. Spine. 2000;26(16):2052-63.), (88. Hoffman D, Lonstein J, Morin M, Visscher W, Harris B, Boice J. Breast cancer in women with scoliosis exposed to multiple diagnostic x-rays. J Natl Cancer Inst. 1989;81(17):1307-12.. Intervals of at least six months between these exams have been recommended to avoid any kind of adverse effect. However, in clinical practice, the interval between assessments is usually shorter, precisely to follow the clinical evolution99. Furlanetto TS, Candotti CT, Comerlato T, Loss JF. Validating a postural evaluation method developed using a digital image-based postural assessment (DIPA) software. Comput Methods Programs Biomed. 2012;108(1):203-12.. In this context, professionals opt for non-invasive cervical spine assessment alternatives, such as photogrammetry1010. Döhnert MB, Tomasi E. Validity of computed photogrammetry for detecting idiopathic scoliosis in adolescents. Rev Bras Fisioter. 2008;12(4):290-7., visual assessment of photographs1111. Alfonso-Peñaloza Y, Cepeda-López J, Navarro-Valencia M, Tirado-Todaro A, Quintero-Moya S, Ramírez P, et al. Reproducibilidad interevaluador del formato de observación sistemática de la alineación corporal en estudiantes universitarios. Fisioterapia. 2013;35(4):154-66., 3D scanning system - Metrecom1212. Black K, McClure P, Polansky M. The influence of different sitting positions on cervical and lumbar posture. Spine. 1996;21(1):65-70., 3D posture ultrasound system1313. Prushansky T, Geller S, Avraham A, Furman C, Sela L. Angular and linear spinal parameters associated with relaxed and erect postures in healthy subjects. Physiother Theory Pract. 2013;29(3):249-57., flexicurve ruler1414. Harrison DE, Haas JW, Cailliet R, Harrison DD, Holland B, Janik TJ. Concurrent validity of flexicurve instrument measurements: sagittal skin contour of the cervical spine compared with lateral cervical radiographic measurements. J Manipulative Physiol Ther. 2005;28(8):597-603., as well as clinical tests such as the cervical straightening test1515. Santos A. Diagnóstico clínico postural: um guia prático. 6th ed. São Paulo: Summus; 2011.. Generally, in physical therapy practice, the clinical tests with or without the use of measurement instruments are the most commonly applied due to their lower costs.
Despite being proposed to assist in the construction of postural clinical reasoning, in general, these tests do not have evidence of validation, as far as it is known. Thus, in this context, the main objectives of the present study were: to propose a clinical test performed with photogrammetry for assessment of the cervical spine based on the frontal-mental line inclination and to identify its concurrent validity in relation to the gold standard. As a secondary objective, the study intends to determine the clinical applicability of this test using a goniometer.
Methods
Study type and sample
The sample was divided into two groups: (1) Validation group, to assess the concurrent validity of the test of frontal-mental line inclination (TFMLI) and (2) Group for the practical application of the TFMLI. The inclusion criterion in the first group was to submit a request for X-ray examination of the cervical spine and to be aged between 18 and 60 years old. The inclusion criterion in the second group was to be aged between 18 and 60 years old. The exclusion criterion was lack of clarity of the X-ray examination images. The present study was approved by the Research Ethics Committee of the University where it was performed, under number 514.875.
The sample size of both groups was calculated in the G* power software (version 3.1.7), based on the z-test family (Pearson correlation coefficient for dependent samples), assuming a two-tailed test, 0.6 correlation expectation, 0.5 effect size, 0.05 α, and 80% power, resulting in a minimum sample of 23 participants in each group. All subjects initially participated in anamnesis to confirm the inclusion and exclusion criteria and to collect characterization data (sex, age, height and body mass).
Test proposition
To perform the TFMLI, the individual should be placed in a dorsal decubitus position on a flat surface. If the line drawn between a point on the nasal bone, between the eyes (frontal point), and a point on the mental protuberance, on the chin (mental point), is not parallel to the surface, the cervical spine curvature may be abnormal. However, this test depends on an initial assessment of head posture because the purpose of the TFMLI is to identify how the individuals’ cervical curvature behaves in relation to the head’s position.
TFMLI’s validation protocol
The first phase of this study consisted of the TFMLI’s validation protocol, which was divided into two stages: (stage 1) assessment of head position using X-ray examinations and photogrammetry and (stage 2) assessment of cervical curvature using X-ray examinations and the TFMLI. The X-ray examinations were performed by a radiology technician and the other assessments were conducted by a chiropractor. Only the Validation group, composed of 35 individuals, participated in both steps.
In stage 1, due to the lack of evidence in the literature on the validation of head position assessment using photogrammetry, a comparison was made with the angles provided by the X-rays, to better consolidate the head position analysis protocol. To perform the X-ray examinations in the sagittal plane, with side-to-side incidence, the individual was positioned sitting on a bench according to their postural pattern, i.e., maintaining their usual seated posture. The X-ray examinations were always performed by the same professional with experience with postural assessment in images and, for the analysis of head position, a line connecting the point of the auditory meatus with the spinous process of the seventh cervical vertebra (C7) and a horizontal line starting from that point were drawn, as suggested by Raine and Twomey1616. Raine S, Twomey L. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust J Physiother. 1994;40(1):25-32. (Figure 1a).
Still in stage 1, the software Digital Image-based Postural Assessment (DIPA©), version 3.1, was used in the head position’s photogrammetry. To this end, the palpation and placement of reflexive markers were initially performed on the anatomical points of interest, as suggested by the protocol99. Furlanetto TS, Candotti CT, Comerlato T, Loss JF. Validating a postural evaluation method developed using a digital image-based postural assessment (DIPA) software. Comput Methods Programs Biomed. 2012;108(1):203-12.. Soon after, the individual was placed in an upright position for the photographic record in the right sagittal plane. The photographs were analyzed in the DIPA© software (available at www.ufrgs.br/biomec), the anatomical points having been scanned based on the reflective markers in the pictures. For the present study, only the result for head position was used, the angle of which is composed by a line drawn from the spinous process of C7 to the right tragus and a line beginning from the spinous process of C7, parallel to the ground and perpendicular to the plumb line, as suggested by Watson and Trott1717. Watson DH, Trott PH. Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13(4):272-84. (Figure 1b).
In both the X-ray examinations and photogrammetry, normality ranged from 50° to 60º, characterizing a neutral head position. When the angle was <50°, the head position was classified as anterior1818. Thomas K, Cureton T. Bodily posture as an indicator of fitness. Res Q. 1941;12(Suppl 2):348-67..
In stage 2, the Cobb method was used to assess cervical curvature from X-ray examinations, which is considered a gold standard for analysis of sagittal plane curvatures and can be used at any vertebral level1919. Vrtovec T, Pernuš F, Likar B. A review of methods for quantitative evaluation of spinal curvature. Eur Spine J. 2009;18(5):593-607.. In the present study, the center point of the anterior and posterior tubercles of the first cervical vertebra (C1); the lower anterior corner and the lower posterior corner of the C7 vertebral body were marked on the radiographs. The Cobb angle (CA) was calculated by crossing the lines connecting the points marked in C1 and C72020. Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000;25(16):2072-8., using the classification proposed by Yochum and Rowe2121. Yochum T, Rowe LJ. Essentials of skeletal radiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1996.: straight (cervical curvature with angle < 35º), normal (angle between 35° and 45°) and hyperlordosis (cervical curvature with angle > 45°).
Still in stage 2, the assessment of the cervical curvature was performed using the TFMLI. Initially, two anatomical points were palpated and identified with reflexive markers: (1) point on the nasal bone, between the eyes (frontal point) and (2) point on the mental protuberance, on the chin (mental point). After marking these points, the individual was placed in dorsal decubitus position on a flat surface (stretcher) and asked to look toward the ceiling. The photographic record was made using a digital camera (Samsung, model L100, 4.1 megapixels) coupled to a tripod and positioned at a horizontal distance of 2.80 m in relation to the individual. In this assessment, the plumb line was aligned, in terms of depth, with the individual’s frontal point.
The TFMLI analysis was performed in the MATLAB software® version 7.5 using a protocol specially developed for this study. Initially, the frontal and mental points in the photographs were scanned. To obtain the angle provided by the TFMLI, known as the frontal-mental line inclination (FMLI), a line joining these two points and another horizontal line perpendicular to the plumb line were drawn. The angle between these lines was used to classify the posture of the cervical spine, negative angles suggesting a decreased cervical curvature, i.e., straight (Figure 1d), and positive angles suggesting increased cervical curvature, i.e., hyperlordosis (Figure 1e).
Analysis of head position and analysis of cervical curvature: (a) Angle of head position using X-ray examination; (b) Angle of head position using photogrammetry; (c) Angle of head position using goniometry; (d) Angle of cervical curvature using the TFMLI indicating a decrease in cervical curvature; (e) Angle of cervical curvature using the TFMLI indicating an increase in cervical curvature and (f) Angle of cervical curvature using the TFMLI with a goniometer.
The application of the TFMLI proposed in this study requires the utilization of equipment (photographic camera, tripod, plumb line, reflective markers and software for the analysis of photos), which does not make it attractive for use in clinical practice. To solve this problem, the second phase of this research consisted of checking the possibility of performing this test using a universal goniometer (Trident), instead of the scanned photograph.
A total of 23 individuals participated in this phase of the research, which consisted of two assessment stages: (stage 1) assessment of head posture using photogrammetry and using a goniometer, and (stage 2) assessment of cervical curvature by means of the TFMLI using a photograph and using a goniometer. Both assessments were performed by the same evaluator, in the same day and place.
In stage 1, the assessment of head posture by means of photogrammetry using the DIPA© software was performed, as previously described. After the photographic recording of the individual in the upright position in the right sagittal plane with the reflexive markers, he/she was asked to remain in the same position and the head posture’s angle was measured using a universal goniometer of the Trident brand. The instrument was positioned with its axis in the lateral projection of the spinous process of C7, the fixed arm was positioned parallel to the ground and perpendicular to the plumb line, while the movable arm of the goniometer was positioned in the right tragus direction (Figure 1c).
In stage 2, to assess the cervical curvature, the two anatomical points of the TFMLI were palpated and identified with reflexive markers in the individual’s body, them being: (1) frontal point and (2) mental point. After marking these points, the individual was placed in a dorsal position on a stretcher (flat surface) for the photographic record of the TFMLI, following the same pattern previously described for the test. Soon after this photographic record and with the individual in the same position, the TFMLI was assessed with the universal goniometer of the Trident brand. In this assessment, the goniometer’s axis was positioned in the projection of the frontal point marker, in the side-to-side plane, with the stationary arm parallel to the ground and the moving arm pointing to the mental point marker (Figure 1f).
Statistical treatment
Statistical calculations were performed in the SPSS software (version 20.0), using descriptive (mean, standard deviation and frequency distribution) and inferential statistics (α < 0.05 was adopted in all analyses). To confirm the normality of the data, Shapiro-Wilk’s test was used. The concurrent validity of the TFMLI, correlation level and agreement between the gold standard (CA) and FMLI angles were evaluated using: Pearson’s Product-Moment Correlation Test, Paired t-Test, Root Mean Square Error (RMS error). A Simple Regression Analysis allowed the adjustment of the FMLI values in relation to the CA values. To evaluate the clinical application of TFMLI with a universal goniometer, Pearson’s Product-Moment Correlation Test or Spearman’s Correlation Test and RMS error were used. The correlation coefficients were classified according to Hopkins2222. Hopkins WG. A new view of statistics. 1997 [cited 2016 Aug 25]. Available from: https://bit.ly/2RJr3U4
https://bit.ly/2RJr3U4...
: very low (between 0.0 and 0.1), low (between 0.1 and 0.3), moderate (between 0.3 and 0.5), high (between 0.5 and 0.7), very high (between 0.7 and 0.9) and practically perfect (between 0.9 and 1).
Results
TFMLI validation
In the phase of the TFMLI’s validation, 22 women (63%) and 13 men (37%) were evaluated. To simplify the head position evaluation methodology, comparisons between X-ray examinations (the gold standard) and photogrammetry were performed at the first stage of the validation (Table 1). These two methodologies have high correlation and low RMS Error, not requiring the use of radiography to assess the position of the head.
With the validation of the use of photogrammetry for the analysis of head position, its methodology was used to categorize the individuals into two groups: group with anterior head position (n = 15) and group with non-anterior head position (n = 20). This classification was applied in all analyses. The anthropometric characteristics of the sample divided by groups are described in Table 2.
TFMLI validation: mean and standard deviation (SD) of the anthropometric characteristics, Cobb angle (CA), frontal-mental line inclination (FMLI) and frontal-mental line inclination adjusted according to CA (adjusted FMLI); Pearson’s Product-Moment Correlation Test (r) and RMS error for sample divided into groups: group with anterior head position and group with non-anterior head position
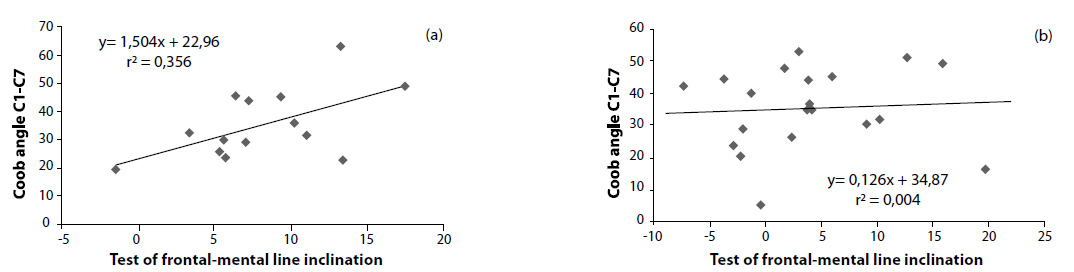
A simple regression analysis between CA and FMLI (Figure 2a) made it possible to predict the adjusted FMLI’s values for individuals with anterior head position. When individuals had non-anterior head position, it was not possible to predict the FMLI values (Figure 2b).
The results of the concurrent validation of the TFMLI demonstrated that, on average, the FMLI values were lower than the CA values before adjustment and that the adjusted FMLI obtained values similar to the CA’s. Also, the RMS error was very low in both groups when the FMLI values were corrected, indicating a minimal difference between the angles and consequently the high accuracy of the adjusted FMLI (Table 2). In addition, T Test showed no significant difference in both groups and only the group with anterior head position showed a high correlation between CA and adjusted FMLI (Table 2).
Correlation between the frontal-mental line inclination and Cobb angle C1-C7: (a) group with anterior head position, (b) group with non-anterior head position.
In the phase of verification of the TFMLI’s clinical applicability, 19 women (82.6%) and 4 men (17.4%) were evaluated and their anthropometric characteristics were presented in Table 3. In relation to the first stage of this phase, the results of the head posture evaluation showed that the values obtained using photogrammetry and using goniometry showed a high and significant correlation (rs = 0.662, p < 0.001*) (Table 3), indicating that the assessment of head position can be performed in clinical practice with the use of a universal goniometer.
In relation to the second stage of the clinical applicability of TFMLI, the results show that the values of the angles obtained from the photographs and the angles obtained from the goniometry showed a significant and practically perfect correlation (r = 0.969; p < 0.001*) (Table 3), indicating that the FMLI can also be performed in clinical practice with a universal goniometer.
Clinical applicability of TFMLI (n = 27): mean and standard deviation (SD) of the anthropometric and head position (HP) angles obtained using photogrammetry and goniometry and frontal-mental line inclination (FMLI) obtained using photogrammetry and goniometry; Pearson’s Product-Moment Correlation Test (r) or Spearman’s Correlation Test (rs) and RMS error
Discussion
The cervical spine is the region of the vertebral column with the greatest mobility2323. Miyazaki M, Hymanson HJ, Morishita Y, He W, Zhang H, Wu G, et al. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. 2008;33(23):870-6.), (2424. Kapandji I. Fisiologia articular: esquemas comentados de mecânica humana. 6th ed. Rio de Janeiro: Guababara-Koogan; 2008. and its structures are difficult to palpate, increasing the chance of errors in the evaluation of this region’s measurements. These errors may be the reason for the lack of valid and reproducible non-invasive cervical evaluation instruments. In this sense, the TFMLI, a test that evaluates the presence of physiological cervical lordosis based on salient points with easy palpation, minimizes this potential source of error in the evaluation of the cervical spine.
Some examples of non-invasive instruments that evaluate the cervical spine are the Metrecom System1212. Black K, McClure P, Polansky M. The influence of different sitting positions on cervical and lumbar posture. Spine. 1996;21(1):65-70., the 3D Ultrasound Posture System1313. Prushansky T, Geller S, Avraham A, Furman C, Sela L. Angular and linear spinal parameters associated with relaxed and erect postures in healthy subjects. Physiother Theory Pract. 2013;29(3):249-57., flexicurve2525. Greendale GA, Nili NS, Huang MH, Seeger L, Karlamangla AS. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporos Int. 2011;22(6):1897-905. and photogrammetry2626. Iunes DH, Castro FA, Salgado HS, Moura IC, Oliveira AS, Bevilaqua-Grossi D. Confiabilidade intra e interexaminadores e repetibilidade da avaliação postural pela fotogrametria. Rev Bras Fisioter. 2005;9(3):327-34.. However, none of their alternative assessment methods has shown concurrent validity to date2727. McFarland C, Wang-Price S, Richard S. Clinical measurements of cervical lordosis using flexirule and inclinometer methods in individuals with and without cervical spine dysfunction: a reliability and validity study. J Back Musculoskelet Rehabil. 2015;28(2):295-302.. The TFMLI, because of its confirmed validity (Table 1, Table 2, Figure 2) in relation to the gold standard, has been shown as a viable non-invasive method for evaluation of the cervical spine. Even so, it should be noted that the TFMLI still lacks reproducibility studies, which may test its ability to be used by different evaluators or by the same evaluator on different evaluation days.
From the methodological point of view, when performing the TFMLI, the physiotherapist will need to adjust the angular value (FMLI) obtained in the test using the equations available in Figure 2, according to the respective head positions of the patient. For instance, in a hypothetical patient with anterior head position and whose TFMLI culminated in 6.9° FMLI, when using the equation y = 1.504x + 22.96, it can be concluded that the cervical curvature angle is 33.3°, equivalent to Cobb’s. Additionally, cervical spine posture can be classified according to theoretical references. In the present study, the interpretation of this result would lead to conclude that this hypothetical patient would have a straight cervical spine2121. Yochum T, Rowe LJ. Essentials of skeletal radiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1996.. However, it should be emphasized that the limitation of this test is that it only allows assessing the cervical spine of individuals with the head in the anterior position.
Frontal head posture is the most common finding in clinical practice regarding the assessment of this region and is generally associated with cervical pain, which is highly disabling2828. Soares JC, Weber P, Trevisan ME, Trevisan CM, Rossi AG. Correlação entre postura da cabeça , intensidade da dor e índice de incapacidade cervical em mulheres com queixa de dor cervical. Fisioter Pesq. 2012;19(1):68-72.. However, this change may be related to different cervical curvature positions. For instance, individuals whose head protrudes beyond the plumb line may have cervical hyperlordosis or even normal curvature1515. Santos A. Diagnóstico clínico postural: um guia prático. 6th ed. São Paulo: Summus; 2011.. In this sense, a test like the TFMLI aids precisely in the investigation of this variable, assisting in the decision-making for choosing the appropriate treatment.
The TFMLI does not consider the plumb line test described by Kendall, McCreary and Provance2929. Kendall FP, McCreary E, Provance P. Músculos, provas e funções. 4th ed. Barueri: Manole; 1995. to assess head position, but rather the relation of the ear tragus with C7, as suggested by Raine and Twomey1616. Raine S, Twomey L. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust J Physiother. 1994;40(1):25-32.. Haas et al.3030. Haas AL, Bracht K, Stöggl T, Brunner R. Which reference line describes head position best? Physiother Rehabil. 2016;1(2). sought to investigate the relationship of head position with plumb line defined by Kendall, McCreary and Provance2929. Kendall FP, McCreary E, Provance P. Músculos, provas e funções. 4th ed. Barueri: Manole; 1995. in the sagittal plane and concluded that the reference line of Kendall, McCreary and Provance2929. Kendall FP, McCreary E, Provance P. Músculos, provas e funções. 4th ed. Barueri: Manole; 1995. does not align with the plumb line passing through the mass center, making the methodological use of plumb line as a reference for postural analysis questionable. Furthermore, individuals whose whole body projects beyond the plumb line do not necessarily have frontal head posture, which strengthens the idea of distinguishing head position from the relation between the ear tragus and C71616. Raine S, Twomey L. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust J Physiother. 1994;40(1):25-32..
One limitation of the TFMLI is the need to use equipment and software, since it is based on photographs, making the assessment extensive and even impracticable to be performed in a non-research-related environment. Precisely to minimize this limitation, the possibility of using a universal goniometer instead of the photograph was tested in the present study. The results of the phase of applicability of the TFMLI showed that this test and the head position angle obtained with a goniometer, which is a practical instrument that is easy to handle, very cheap and accessible for physiotherapists, correlate with those obtained from the photographic record (Table 3). It should be noted that, in addition to the practically perfect correlation between the result of the goniometer and of the photograph, the low RMS error found attests to the accuracy of the FMLI and the head position angle measured by the goniometer.
Furthermore, a limitation of the study is the absence of the temporo-mandibular joint’s (TMJ) evaluation, because the TMJ may change the position of the chin and cause errors in the test since one of the reference points in the TFMLI is located on the chin. Another limitation was not having evaluated the reliability of the TFMLI. Nevertheless, it is assumed that the TFMLI can be considered an easy clinical test that requires little instrumentation and assists in the construction of postural clinical reasoning, providing valid and accurate information for evaluating the cervical spine as well as being applicable in clinical practice, with the use of a goniometer to perform the test.
Conclusion
It is concluded that the TFMLI, performed by analyzing a photographic record in a software is adequate for an initial assessment of the cervical spine posture of individuals with anterior head position since (1) the high correlation with the gold standard and (2) the low RMS error demonstrate the accuracy of this alternative method.
In addition, the TFMLI can be easily applied in clinical practice with the use of a universal goniometer since it showed (1) high and practically perfect correlation in the assessment of head position and cervical spine curvature in relation to photogrammetry, respectively, and (2) low RMS error.
References
-
1Gay RE. The curve of spine cervical. J Manipulative Physiol Ther. 1993;16(9):591-4.
-
2Mani S, Sharma S, Omar B, Ahmad K, Muniandy Y, Singh DKA. Quantitative measurements of forward head posture in a clinical settings: a technical feasibility study. Eur J Physiother. 2017;19(3):119-23.
-
3Saunders ES, Woggon D, Cohen C, Robinson DH. Improvement of cervical lordosis and reduction of forward head posture with anterior head weighting and proprioceptive balancing protocols. J Vertebr Subluxation Res. 2003;1-5.
-
4Lennon J, Shealy CN, Cady RK, Matta W, Cox R, Simpson WF. Postural and respiratory modulation of autonomic function, pain and health. AJPM. 1994;4(1):36-9.
-
5Allen S, Parent E, Khorasani M, Hill DL, Lou E, Raso JV. Validity and reliability of active shape models for the estimation of cobb angle in patients with adolescent idiopathic scoliosis. J Digit Imaging. 2008;21(2):208-18.
-
6Tayyab NA, Samartzis D, Altiok H, Shuff CE, Lubicky JP, Herman J, et al. The reliability and diagnostic value of radiographic criteria in sagittal spine deformities: comparison of the vertebral wedge ratio to the segmental cobb angle. Spine. 2007;32(16):451-9.
-
7Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE. Breast cancer mortality after diagnostic radiography: findings from the U.S. scoliosis cohort study. Spine. 2000;26(16):2052-63.
-
8Hoffman D, Lonstein J, Morin M, Visscher W, Harris B, Boice J. Breast cancer in women with scoliosis exposed to multiple diagnostic x-rays. J Natl Cancer Inst. 1989;81(17):1307-12.
-
9Furlanetto TS, Candotti CT, Comerlato T, Loss JF. Validating a postural evaluation method developed using a digital image-based postural assessment (DIPA) software. Comput Methods Programs Biomed. 2012;108(1):203-12.
-
10Döhnert MB, Tomasi E. Validity of computed photogrammetry for detecting idiopathic scoliosis in adolescents. Rev Bras Fisioter. 2008;12(4):290-7.
-
11Alfonso-Peñaloza Y, Cepeda-López J, Navarro-Valencia M, Tirado-Todaro A, Quintero-Moya S, Ramírez P, et al. Reproducibilidad interevaluador del formato de observación sistemática de la alineación corporal en estudiantes universitarios. Fisioterapia. 2013;35(4):154-66.
-
12Black K, McClure P, Polansky M. The influence of different sitting positions on cervical and lumbar posture. Spine. 1996;21(1):65-70.
-
13Prushansky T, Geller S, Avraham A, Furman C, Sela L. Angular and linear spinal parameters associated with relaxed and erect postures in healthy subjects. Physiother Theory Pract. 2013;29(3):249-57.
-
14Harrison DE, Haas JW, Cailliet R, Harrison DD, Holland B, Janik TJ. Concurrent validity of flexicurve instrument measurements: sagittal skin contour of the cervical spine compared with lateral cervical radiographic measurements. J Manipulative Physiol Ther. 2005;28(8):597-603.
-
15Santos A. Diagnóstico clínico postural: um guia prático. 6th ed. São Paulo: Summus; 2011.
-
16Raine S, Twomey L. Posture of the head, shoulders and thoracic spine in comfortable erect standing. Aust J Physiother. 1994;40(1):25-32.
-
17Watson DH, Trott PH. Cervical headache: an investigation of natural head posture and upper cervical flexor muscle performance. Cephalalgia. 1993;13(4):272-84.
-
18Thomas K, Cureton T. Bodily posture as an indicator of fitness. Res Q. 1941;12(Suppl 2):348-67.
-
19Vrtovec T, Pernuš F, Likar B. A review of methods for quantitative evaluation of spinal curvature. Eur Spine J. 2009;18(5):593-607.
-
20Harrison DE, Harrison DD, Cailliet R, Troyanovich SJ, Janik TJ, Holland B. Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine. 2000;25(16):2072-8.
-
21Yochum T, Rowe LJ. Essentials of skeletal radiology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1996.
-
22Hopkins WG. A new view of statistics. 1997 [cited 2016 Aug 25]. Available from: https://bit.ly/2RJr3U4
» https://bit.ly/2RJr3U4 -
23Miyazaki M, Hymanson HJ, Morishita Y, He W, Zhang H, Wu G, et al. Kinematic analysis of the relationship between sagittal alignment and disc degeneration in the cervical spine. 2008;33(23):870-6.
-
24Kapandji I. Fisiologia articular: esquemas comentados de mecânica humana. 6th ed. Rio de Janeiro: Guababara-Koogan; 2008.
-
25Greendale GA, Nili NS, Huang MH, Seeger L, Karlamangla AS. The reliability and validity of three non-radiological measures of thoracic kyphosis and their relations to the standing radiological Cobb angle. Osteoporos Int. 2011;22(6):1897-905.
-
26Iunes DH, Castro FA, Salgado HS, Moura IC, Oliveira AS, Bevilaqua-Grossi D. Confiabilidade intra e interexaminadores e repetibilidade da avaliação postural pela fotogrametria. Rev Bras Fisioter. 2005;9(3):327-34.
-
27McFarland C, Wang-Price S, Richard S. Clinical measurements of cervical lordosis using flexirule and inclinometer methods in individuals with and without cervical spine dysfunction: a reliability and validity study. J Back Musculoskelet Rehabil. 2015;28(2):295-302.
-
28Soares JC, Weber P, Trevisan ME, Trevisan CM, Rossi AG. Correlação entre postura da cabeça , intensidade da dor e índice de incapacidade cervical em mulheres com queixa de dor cervical. Fisioter Pesq. 2012;19(1):68-72.
-
29Kendall FP, McCreary E, Provance P. Músculos, provas e funções. 4th ed. Barueri: Manole; 1995.
-
30Haas AL, Bracht K, Stöggl T, Brunner R. Which reference line describes head position best? Physiother Rehabil. 2016;1(2).
Publication Dates
-
Publication in this collection
13 May 2019 -
Date of issue
2019
History
-
Received
16 Apr 2018 -
Accepted
27 Nov 2018