Abstracts
Streptococcus mutans is specifically suppressed by intensive treatment with chlorhexidine gel, but the time for recolonization and the effect on other oral bacteria are not totally clear. In this study, recolonization of mutans streptococci was evaluated in nine healthy adult volunteers, who were highly colonized with this microorganism. Stimulated saliva was collected before (baseline) and at 1, 7, 14, 21 and 28 days after application of 1% chlorhexidine gel on volunteers' teeth for two consecutive days. On each day, the gel was applied using disposable trays for 3 x 5 min with intervals of 5 min between each application. Saliva was plated on blood agar to determine total microorganisms (TM); on mitis salivarius agar to determine total streptococci (TS) and on mitis salivarius agar plus bacitracin to determine mutans streptococci (MS). Chlorhexidine was capable of reducing the counts of MS and the proportion of MS with regard to total microorganisms (%MS/TM) (p<0.05), but these values did not differ statistically from baseline (p>0.05) after 14 days for MS and 21 days for %MS/TM. The counts of TM and TS and the proportion of MS to total streptococci did not differ statistically from baseline (p>0.05) after chlorhexidine treatment. The results suggest that the effect of chlorhexidine gel treatment on suppression of mutans streptococci is limited to less than a month in highly colonized individuals.
chlorhexidine; mutans streptococci ; saliva
Streptococcus mutans é especificamente suprimido pelo tratamento intensivo com clorexidina em gel, mas o tempo de recolonização e o efeito em outras bactérias orais não está totalmente claro. Nesse estudo, a recolonização de estreptococos do grupo mutans foi avaliado em nove voluntários adultos saudáveis, os quais eram altamente colonizados por esse microrganismo. Saliva estimulada foi coletada antes (baseline) e 1, 7, 14, 21 e 28 dias após a aplicação de clorexidina em gel a 1% nos dentes dos voluntários por dois dias consecutivos. Em cada dia, o gel foi aplicado utilizando moldeiras descartáveis por 3 x 5 min com intervalos de 5 min entre cada aplicação. A saliva foi inoculada em ágar sangue para determinação dos microrganismos totais (MT); em mitis salivarius ágar para determinação dos estreptococos totais (ET) e em meio mitis salivarius com bacitracina para determinar a contagem de estreptococos do grupo mutans (EGM). O tratamento com clorexidina foi capaz de reduzir as contagens de EGM e a proporção de EGM em relação aos microrganismos totais (%EGM/MT) (p<0,05), mas esses valores não diferiram estatisticamente do baseline (p>0,05) após 14 dias para EGM e 21 dias para %EGM/MT. As contagens de MT e ET e a proporção de EGM em relação a estreptococos totais não difereriram estatisticamente do baseline (p>0,05) após o tratamento com clorexidina. Os resultados sugerem que o efeito do tratamento com clorexidina em gel na supressão de estreptococos do grupo mutans é limitado a menos de um mês em indivíduos altamente colonizados.
Introduction
Fluoride has been the most successful substance used to control caries but it does not have strong antibacterial effect (1)1 1. Tenuta LM, Cury JA. Fluoride: its role in dentistry. Braz Oral Res 2010;24:9-17., so that the use of nonfluoride caries preventive agents (2)2 2. Rethman MP, Beltrán-Aguilar ED, Billings RJ, Hujoel PP, Katz BP, Milgrom P, et al.. Nonfluoride caries-preventive agents: executive summary of evidence-based clinical recommendations. J Am Dent Assoc 2011;142:1065-1071., like chlorhexidine (CHX), has been a clinical option to improve the anticaries effect of fluoride.
Mutans streptococci, the main microorganisms related to dental caries (3)3 3. Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev 1986;50:353-380., are particularly sensitive to chlorhexidine (4)4 4. Emilson GC. Potential efficacy of chlorhexidine against mutans streptococci and human dental caries. J Dent Res 1994;73:682-691.. This antimicrobial agent has been thoroughly researched in terms of its caries-inhibition effect (5)5 5. Twetman S. Antimicrobials in future caries control? A review with special reference to chlorhexidine treatment. Caries Res 2004;38:223-229.. Clinical trials have shown that CHX reduces mutans streptococcal counts in relation to those of other bacteria in plaque and saliva ( 66 6. Attin R, Tuna A, Attin T, Brunner E, Noack MJ. Efficacy of differently concentrated chlorhexidine varnishes in decreasing mutans streptococci and lactobacilli counts. Arch Oral Biol 2003;48:503-509. , 77 7. Derks A, Frencken J, Bronkhorst E, Kuijpers-Jagtman AM, Katsaros C. Effect of chlorhexidine varnish application on mutans streptococci counts in orthodontic patients. Am J Orthod Dentofacial Orthop 2008;133:435-439 ). The antibacterial action of CHX is based on its adsorption onto bacterial surfaces. At low concentrations, the bacteriostatic effect is based on disturbance of bacterial cell functions, enzymes and cell receptors, and at high concentrations, CHX causes cytoplasmic precipitation or coagulation (8)8 8. Jones CG. Chlorhexidine: is it still the gold standard? Periodontol2000 1997;15:55-62.. Also, it inhibits the action of glycosyltransferase, the enzyme responsible for polysaccharide synthesis, favouring accumulation of bacteria on the dental surface, and has effects on sugar transport and acid production in oral bacteria ( 99 9. Marsh PD, Keevil CW, McDermid AS, Williamson MI, Ellwood DC. Inhibition by the antimicrobial agent chlorhexidine of acid production and sugar transport in oral streptococcal bacteria. Arch Oral Biol 1983;28:233-240. , 1010. Gerardu VA, Buijs MJ, Ten Cate JM, van Loveren C. Effect of an intensified treatment with 40% chlorhexidine varnish on plaque acidogenicity. Clin Oral Investig 2006;11:77-81. ).
Ribeiro et al. (11)11. Ribeiro LGM, Hashizume LN, Maltz M. The effect of different formulations of chlorhexidine in reducing levels of mutans streptococci in the oral cavity: a systematic review of the literature. J Dent 2007;35:359-370., studying different formulations of chlorhexidine on the reduction of mutans streptococci levels in the oral cavity, showed that a significant reduction can be achieved through intensive treatment (3-4 daily applications over 2 days) or through daily application for 10 and 14 days with 1% gel. However, given the large individual variation in response to treatment, MS levels must be re-assessed during the course of treatment. Indeed, the main clinical problem with the use of chlorhexidine is the difficulty in suppressing or eliminating mutans streptococci for an extended period of time.
The data available so far is not clear about neither the re-colonization time of mutans streptococci after treatment with CHX gel nor its effects on other oral bacteria. Thus, the aim of this study was to evaluate the time for recolonization of mutans streptococci, total streptococci and total microorganisms after intensive treatment with CHX gel.
Material and Methods
Experimental Design
This study was approved by the Research and Ethics Committee of Piracicaba Dental School - University of Campinas, Brazil (Protocol #039/2006) and nine adult volunteers took part in this research. Stimulated saliva was collected before (baseline) and after 1, 7, 14, 21 and 28 days of treatment with 1% CHX gel, which consisted in three applications of gel for 5 min using disposable trays with intervals of 5 min between each application for two consecutive days. After each time, microbiological analyses were done in collected saliva. For the statistical analysis, the volunteer was considered as an experimental block.
Volunteers
Nine healthy adult volunteers (20-34 years old, 5 male and 4 female) participated in this study. The inclusion criteria comprised counts of mutans streptococci in saliva ≥105 colony-forming units (CFU) per mL and ability to comply with the experimental protocol. The exclusion criteria included antibiotic use for the last 2 months before starting the study, use of any form of medication that modifies salivary secretion, use of fixed or removable orthodontic appliance, periodontal disease and general/systemic illness. Informed written consent was obtained prior to the commencement of the study.
CHX Treatment
Prior to the CHX applications, the volunteers brushed their teeth and used interdental floss under professional supervision. A gel containing 1% digluconate chlorhexidine (prepared in a pharmacy) was applied to the volunteers' teeth, using double disposables trays, three times for 5 min with intervals of 5 min between each application for two consecutive days. During the whole experimental period, all subjects were asked to continue their normal oral hygiene procedures but to avoid using any antimicrobial products.
Saliva Sampling and Microbiological Analysis
Stimulated saliva samples were collected in the morning within fasting condition and without previous teeth brushing at baseline (before CHX application) and after 1, 7, 14, 21 and 28 days of CHX treatment. Whole saliva was diluted in sterile 0.9% NaCl in series up to 105 and 3 drops of 20 μL of each dilution were dispensed on blood agar to determine total microorganisms (TM); mitis salivarius agar (Difco, Sparks, M.D., USA) to determine total streptococci (TS); mitis salivarius agar plus 0.2 units/mL of bacitracin (MSB) to determine mutans streptococci (MS) (12)12. Gold OG, Jordan HV, van Houte J. A selective medium for Streptococcus mutans. Arch Oral Biol 1973;18:1357-1364.. Plates were incubated for 48 h at 37 °C in 10% CO2. The blood agar plates were additionally incubated for 24 h at 37 °C in aerobiosis. Colony-forming units (CFU) were counted and the results expressed as CFU/mL of stimulated saliva, percentage of mutans streptococci in relation to total microorganism (%MS/TM) and percentage of mutans streptococci in relation to total streptococci (%MS/TS).
Statistical Analysis
The volunteers considered as statistical blocks. The assumptions of equality of variances and normal distribution of errors were checked for all the response variables tested, and those that did not satisfy these assumptions were transformed (13)13. Box GEP, Hunter JS, Hunter WG. Statistics for experimenters: design, innovation, and discovery. 2nd ed. New York: John Wiley &Sons Inc; 2005.. The counts of TM, TS, MS and %MS/TM and %MS/TS were transformed by log10. These transformed variables were submitted to ANOVA followed by Dunnet test. The SPSS software system (version 12.0) was used and the significance level was set at 5%.
Results
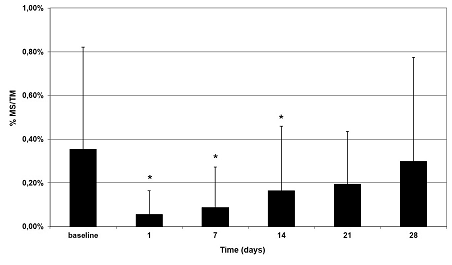
The treatment with CHX was able to reduce significantly the counts of MS and the %MS/TM (p<0.05) after 1 and 7 days after application, however the counts of MS and the %MS/TM did not differ from baseline after 14 and 21 days, respectively (Figs. 1 and 2). The counts of TM, TS and %MS/TS (Table 1) did not show any statistical difference between baseline and after CHX treatment irrespective to times evaluated (p>0.05).
Means of MS counts in saliva (CFU/mL) in relation to time. Asterisk indicate statistical difference between baseline and days after CHX treatments (p<0.05). Bars denote standard deviation, n=9.
%MS/TM in saliva in relation to time. Asterisk indicate statistical difference between baseline and days after CHX treatments (p<0.05). Bars denote standard deviation, n=9.
Discussion
In the present research, we assessed the recolonization of MS and the effect on other oral bacteria after intensive treatment with CHX. The use of the concentration of 1% was already used in previous studies evaluating the effect of CHX gel on MS levels in the saliva and/or dental biofilm, but with different protocols ( 1414. Twetman S, Grindefjord M. Mutans streptococci suppression by chlorhexidine gel in toddlers. American J Dent 1999;12:89-91. , 1515. Rocha EP, Francisco SB, Del Bel Cury AA, Cury JA. Longitudinal study of the influence of removable partial denture and chemical control on the levels of Streptococcus mutans in saliva. J Oral Rehabil 2003;30:131-138. ). This concentration was chosen, since increasing the concentration of CHX gel up to 5% does not appear to enhance its ability to lower MS levels (16)16. Schaeken MJ, de Jong MH, Franken HC, van der Hoeven JS. Effects of highly concentrated stannous fluoride and chlorhexidine regimes on human dental plaque flora. J Dent Res 1986;65:57-61.. The effect of CHX in reducing salivary levels of SM observed in the present research is in agreement with the recognized sensivity of these microorganisms to CHX (17)17. Emilson C. Effect of chlorhexidine gel treatment on Streptococcus mutans population in human saliva and dental plaque. Scand J Dent Res 1981;89:239-246..
Previous research reported that a single-session intensive treatment regimen using 1% CHX gel (three 5-min applications) produced a significant decrease in MS levels for a period of only 3 days at most (18)18. Emilson CG, Gisselsson H, Birkhed D. Recolonisation pattern of mutans streptococci after suppression by three different modes of chlorhexidine gel application. Eur J Oral Sci 1999;107:170-175.. In our protocol, we used 1% CHX gel (three 5-min applications) for 2 consecutive days with a longer period of decrease in MS counts (14 days). However, this time was lower than that found by Maltz et al. (19)19. Maltz M, Zickert I, Krasse B. Effect of intensive treatment with chlorhexidine on number of Streptococcus mutans in saliva. Scand J Dent Res 1981;89:445-449., who studied the effect of an intensive treatment regimen involving four applications on the first day and three on the second and 24 weeks after finishing treatment, 20% of the volunteers still displayed lower levels than those detected prior to application of 1% CHX gel. As we can observe, the time for MS re-appears in the oral cavity after CHX treatment is extremely variable, ranging from few days up to weeks. The reason is probably due to a large between-individual variation in time of MS recolonization (19).
Although a slight decrease occurred in TM counts at least after one day of treatment, the absence of statistical effect suggest that the recolonization of those bacteria is very fast. Additionally, since rich non-specific media were used (MSA and blood agar for TS and TM, respectively), high counts of those bacteria was found and CHX may have not a great effect over them. Although the number and level of colonized sites in the oral cavity is directly reflected by the salivary counts (20)20. Lindquist B, Emilson CG. Distribution and prevalence of mutans streptococci in the human dentition. J Dent Res 1990;69:1160-1166., it must be emphasized that we assessed the CHX effect on saliva and different pattern could be found in dental biofilm levels of bacteria (21)21. Simón-Soro A, Tomás I, Cabrera-Rubio R, Catalan MD, Nyvad B, Mira A. Microbial geography of the oral cavity. J Dent Res 2013;92:616-621..
Based on the data found, a significant reduction in the level of MS can be achieved through intensive treatment (3 daily applications over 2 days). Nevertheless, given the individual variation in response to treatment observed, it is advisable the reassessment of MS levels during treatment if this protocol is used.
The results suggest that the effect of chlorhexidine gel treatment on suppression of mutans streptococci is limited to less than a month in highly colonized individuals.
Acknowledgements
The study was supported by The São Paulo State Research Foundation (FAPESP - Process #05/03090-4). The authors acknowledge the volunteers for their valuable participation.
-
11. Tenuta LM, Cury JA. Fluoride: its role in dentistry. Braz Oral Res 2010;24:9-17.
-
22. Rethman MP, Beltrán-Aguilar ED, Billings RJ, Hujoel PP, Katz BP, Milgrom P, et al.. Nonfluoride caries-preventive agents: executive summary of evidence-based clinical recommendations. J Am Dent Assoc 2011;142:1065-1071.
-
33. Loesche WJ. Role of Streptococcus mutans in human dental decay. Microbiol Rev 1986;50:353-380.
-
44. Emilson GC. Potential efficacy of chlorhexidine against mutans streptococci and human dental caries. J Dent Res 1994;73:682-691.
-
55. Twetman S. Antimicrobials in future caries control? A review with special reference to chlorhexidine treatment. Caries Res 2004;38:223-229.
-
66. Attin R, Tuna A, Attin T, Brunner E, Noack MJ. Efficacy of differently concentrated chlorhexidine varnishes in decreasing mutans streptococci and lactobacilli counts. Arch Oral Biol 2003;48:503-509.
-
77. Derks A, Frencken J, Bronkhorst E, Kuijpers-Jagtman AM, Katsaros C. Effect of chlorhexidine varnish application on mutans streptococci counts in orthodontic patients. Am J Orthod Dentofacial Orthop 2008;133:435-439
-
88. Jones CG. Chlorhexidine: is it still the gold standard? Periodontol2000 1997;15:55-62.
-
99. Marsh PD, Keevil CW, McDermid AS, Williamson MI, Ellwood DC. Inhibition by the antimicrobial agent chlorhexidine of acid production and sugar transport in oral streptococcal bacteria. Arch Oral Biol 1983;28:233-240.
-
10Gerardu VA, Buijs MJ, Ten Cate JM, van Loveren C. Effect of an intensified treatment with 40% chlorhexidine varnish on plaque acidogenicity. Clin Oral Investig 2006;11:77-81.
-
11Ribeiro LGM, Hashizume LN, Maltz M. The effect of different formulations of chlorhexidine in reducing levels of mutans streptococci in the oral cavity: a systematic review of the literature. J Dent 2007;35:359-370.
-
12Gold OG, Jordan HV, van Houte J. A selective medium for Streptococcus mutans. Arch Oral Biol 1973;18:1357-1364.
-
13Box GEP, Hunter JS, Hunter WG. Statistics for experimenters: design, innovation, and discovery. 2nd ed. New York: John Wiley &Sons Inc; 2005.
-
14Twetman S, Grindefjord M. Mutans streptococci suppression by chlorhexidine gel in toddlers. American J Dent 1999;12:89-91.
-
15Rocha EP, Francisco SB, Del Bel Cury AA, Cury JA. Longitudinal study of the influence of removable partial denture and chemical control on the levels of Streptococcus mutans in saliva. J Oral Rehabil 2003;30:131-138.
-
16Schaeken MJ, de Jong MH, Franken HC, van der Hoeven JS. Effects of highly concentrated stannous fluoride and chlorhexidine regimes on human dental plaque flora. J Dent Res 1986;65:57-61.
-
17Emilson C. Effect of chlorhexidine gel treatment on Streptococcus mutans population in human saliva and dental plaque. Scand J Dent Res 1981;89:239-246.
-
18Emilson CG, Gisselsson H, Birkhed D. Recolonisation pattern of mutans streptococci after suppression by three different modes of chlorhexidine gel application. Eur J Oral Sci 1999;107:170-175.
-
19Maltz M, Zickert I, Krasse B. Effect of intensive treatment with chlorhexidine on number of Streptococcus mutans in saliva. Scand J Dent Res 1981;89:445-449.
-
20Lindquist B, Emilson CG. Distribution and prevalence of mutans streptococci in the human dentition. J Dent Res 1990;69:1160-1166.
-
21Simón-Soro A, Tomás I, Cabrera-Rubio R, Catalan MD, Nyvad B, Mira A. Microbial geography of the oral cavity. J Dent Res 2013;92:616-621.
Publication Dates
-
Publication in this collection
Nov-Dec 2014
History
-
Received
08 July 2014 -
Accepted
24 Nov 2014