Abstract
The aim of this study was to evaluate the effect of varying the diameter, connection type and loading on stress distribution in the cortical bone for implants with a high crown-implant ratio. Six 3D models were simulated with the InVesalius, Rhinoceros 3D 4.0 and SolidWorks 2011 software programs. Models were composed of bone from the posterior mandibular region; they included an implant of 8.5 mm length, diameter Ø 3.75 mm or Ø 5.00 mm and connection types such as external hexagon (EH), internal hexagon (IH) and Morse taper (MT). Models were processed using the Femap 11.2 and NeiNastran 11.0 programs and by using an axial force of 200 N and oblique force of 100 N. Results were recorded in terms of the maximum principal stress. Oblique loading showed high stress in the cortical bone compared to that shown by axial loading. The results showed that implants with a wide diameter showed more favorable stress distribution in the cortical bone region than regular diameter, regardless of the connection type. Morse taper implants showed better stress distribution compared to other connection types, especially in the oblique loading. Thus, oblique loading showed higher stress concentration in cortical bone tissue when compared with axial loading. Wide diameter implant was favorable for improved stress distribution in the cortical bone region, while Morse taper implants showed lower stress concentration than other connections.
Key Words:
dental implant; bone tissue; mechanical stress; finite element analysis
Resumo
O objetivo deste estudo foi avaliar o efeito da variação do diâmetro e dos tipos de conexão na distribuição do estresse no osso cortical para implantes com a proporção coroa-implante. Seis modelos 3D foram simulados com os programas InVesalius, Rhinoceros 3D 4.0 e SolidWorks 2011. Os modelos foram compostos de osso da região mandibular posterior. Foram incluídos implantes de 8,5 mm de comprimento, diâmetro Ø 3,75 mm ou Ø 5,00 mm, e tipos de conexão como hexágono externo (EH), hexágono interno (IH) e cone Morse (MT). Os modelos foram processados usando os programas Femap 11.2 e NeiNastran 11.0 e usando uma força axial de 200 N e força oblíqua de 100 N. Os resultados foram registrados em termos da tensão principal máxima. O carregamento oblíquo mostrou alta tensão no osso cortical em comparação com a carga axial. Os resultados mostraram que os implantes com maior diâmetro apresentaram distribuição de tensões mais favorável, independentemente do tipo de conexão, enquanto que os implantes cone Morse apresentaram melhores distribuição de tensões comparado aos outros tipos de conexão, especialmente no carregamento oblíquo. Assim, os implantes de maior diâmetro foram mais favoráveis para distribuição das tensões na região de tecido ósseo cortical, enquanto que os implantes cone Morse apresentam menores concentrações de tensões do que as outras conexões.
Introduction
The placement of implants in the posterior mandible with reduced bone availability is a challenge for dental implantology. The options that can facilitate placement of conventional implants include use of bone graft and/or lateralization of the inferior alveolar nerve; however, this modality of treatment is associated with high costs and morbidity. Therefore, the use of short implants may be an alternative, viable and effective treatment option 11 Lemos, CA; Ferro-Alves, ML; Okamoto, R; Mendonça, MR; Pellizzer, EP. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J Dent 2016;47:8-17..
Short implants with wide diameter may increase survival rates 22 Karthikeyan, I; Desai, SR; R Singh, R. Short implants: A systematic review. J Indian Soc Periodontol 2012;16:302-312.; additionally, it is more acceptable than surgical placement of bone grafts in the posterior jaw 33 Esposito, M; Cannizzaro, G; Soardi, E; Pistilli, R; Piattelli, M; Corvino, V; et al.. Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm-long, 4 mm-wide implants or by longer implants in augmented bone. Preliminary results from a pilot randomized controlled trial. Eur J Oral Implantol 2012;5:19-33.. However, there is concern regarding the longevity of these implants from a biomechanical perspective 44 Vasco, MA; Hecke, MB; Bezzon, OL. Analysis of short implants and lateralization of the inferior alveolar nerve with 2-stage dental implants by finite element method. J Craniofac Surg 2011;22:2064-2071.. The incidence of oblique loads at short implants can impact longevity 55 Chang, SH; Lin, CL; Lin, YS; Hsue, SS; Huang, SR. Biomechanical comparison of a single short and wide implant with monocortical or bicortical engagement in the atrophic posterior maxilla and a long implant in the augmented sinus. Int J Oral Maxillofac Implants2012;27:102-111., mainly owing to the increase in crown-implant ratio 66 Garaicoa-Pazmiño, C; Suárez-López del Amo, F; Monje, A; Catena, A; I. Ortega-Oller, I; Galindo-Moreno, P, et al.. Influence of crown/implant ratio on marginal bone loss: A systematic review. J Periodontol 2014;85:1214-1221., which increases stress concentration in the bone tissue around the implant 77 Moraes, SL; Verri, FR; Santiago, Jr JF; Almeida, DA; de Mello, CC; Pellizzer, EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J 2013;24:635-641..
In addition to diameter, the connection type is an important factor in the biomechanics of implant placement. Studies have shown that implants with a conical internal connection (Morse taper) exhibit better stress distribution in the bone tissue when compared with external hexagon implants 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.,99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.; however, this outcome remains controversial, as in one study Morse taper did not reduce the microstrain in the bone tissue around the implants 1010 Nishioka, RS; Vasconcellos, LG; Melo Nishioka, GN. Comparative strain gauge analysis of external and internal hexagon, Morse taper, and influence of straight and offset implant configuration. Implant Dent 2011;20:24-32.. Thus, due to the small number of studies that have investigated the effect of diameter and connection type, the aim of this study was to evaluate the effect of varying the diameter and connection type on stress distribution in the cortical bone tissue for implants with a high crown-implant ratio. Three null hypotheses were tested: 11 Lemos, CA; Ferro-Alves, ML; Okamoto, R; Mendonça, MR; Pellizzer, EP. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J Dent 2016;47:8-17. there is no difference in stress distribution between regular and wide diameter; 22 Karthikeyan, I; Desai, SR; R Singh, R. Short implants: A systematic review. J Indian Soc Periodontol 2012;16:302-312. different connections produce similar stress distribution outcomes; 33 Esposito, M; Cannizzaro, G; Soardi, E; Pistilli, R; Piattelli, M; Corvino, V; et al.. Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm-long, 4 mm-wide implants or by longer implants in augmented bone. Preliminary results from a pilot randomized controlled trial. Eur J Oral Implantol 2012;5:19-33. the loading direction does not influence on the stress distribution.
Materials and Methods
Experimental Design
This study was designed to investigate three variation factor: The difference in diameter (Ø 3.75 mm and Ø 5.00 mm), connection type (external hexagon (EH), internal hexagon (IH), and Morse taper (MT)) and loading condition (axial and oblique). The six models that were simulated are presented in Table 1 and Figure 1. This methodology follows described as previous research 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.,99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.,1111 Verri, FR; R.S., Cruz; Lemos ,CA; Souza Bati, VE; Almeida, DA; Verri, AC; et al.. Influence of bicortical techniques in internal connection plac VEed in pre-maxillary area by 3D finite element analysis. Comput Methods Biomech Biomed Engin 2016;13:1-8..
Three-Dimensional (3D) Finite Element Modeling
The 3D finite element analysis (FEA) methodology used here follows that of previous studies 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.,99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.,1111 Verri, FR; R.S., Cruz; Lemos ,CA; Souza Bati, VE; Almeida, DA; Verri, AC; et al.. Influence of bicortical techniques in internal connection plac VEed in pre-maxillary area by 3D finite element analysis. Comput Methods Biomech Biomed Engin 2016;13:1-8.. Each model was composed of a bone block of the mandibular area around the second molar (2º M) and the trabecular bone in the center was surrounded by 1 mm of cortical bone. Information for the bone block was obtained by computerized tomography already obtained through a database, only used to facilitate the reproduction of details and design of simulated bone tissue. Modeling was performed with InVesalius software (CTI Renato Archer, Campinas, SP, Brazil) and surface simplification was accomplished with Rhinoceros 4.0 software (NURBS Modeling for Windows, Seattle, WA, USA).
The implant design was obtained from a simplified version of the original implant connection (Conexão Sistemas de Prótese Ltda, Aruja, SP, Brazil), with different geometries (external hexagon; internal hexagon and Morse taper), a diameter of Ø 3.75 and Ø 5 mm and a length of 8.5 mm that included their specific abutments. The implant and abutment geometries were simplified by a 3D computer-aided design software (SolidWorks 2010; SolidWorks Corp, Waltham,MA, USA) and Rhinoceros 4.0 CAD.
The crown was configured from artificial molar tooth (Odontofix Indústria e Comércio de Material Odontológico Ltda., Ribeirão Preto, SP, Brazil) and digitized using a 3D scanner (MDX-20; Roland DG, São Paulo SP, Brazil). Images were exported to Rhinoceros 4.0 CAD software for modeling. Occlusal surface details were added using the SolidWorks CAD software package (SolidWorks). Prosthesis were simulated with a screw for external and internal connection. Morse taper connection received dental prosthesis cemented (cement layer: 0.03 mm thickness) retained. The height of the crown simulated for all models was 15 mm, which resulted in a crown-implant ratio close to 2:1 (high crown-implant ratio).
After modeling the solids, geometries were exported to FEA software for pre- and post-processing (FEMAP 11.2, Siemens PLM, Santa Ana, CA, USA), to obtain meshes of tetrahedral parabolic solid elements with ten nodes in which different numbers of nodes and elements for each model (Table 1). The mechanical properties of each simulated material were attributed to the meshes by using previously published values in the literature (Table 2) (7-9). All materials were assumed to be homogeneous, isotropic and linearly elastic.
All contacts were simulated as symmetric welds, except for the abutment/implant and single-unit crown contacts that were simulated by symmetric contacts. Constraint definitions were established as fixed in the axes (x, y and z) at the mesial and distal surfaces of the cortical and trabecular bone. All other model surfaces were unrestricted. The applied axial force was 200 N at a specific four points on the internal slope of the cusps, whereas the oblique load was divided into two loading points applied in the internal slope of lingual cusps with 100 N.
Finally, the analysis was carried out using the FEMAP 11.1.2 finite element software and exported to the NeiNastran 9.2 (Noran Engineering, Westminster, CO, USA) software for calculations at a dedicated workstation (Sun Microsystems Inc., São Paulo, SP, Brazil). Results were entered again in FEMAP 11.1.2 software for visualization and post-processing of the maps. The results were then imported and visualized in the maximum principal stress maps (MPa) to analyze the stress distribution in the cortical bone tissue.
Results
Diameter of Implant
Under axial loading, implants with wide diameter showed a decrease compressive stress in the cortical bone when compared to implants with regular diameter, independently of connection type. This difference is even more evident in oblique loading, since implants with regular diameter showed increase of tensile stress concentration compared to wide diameter implants (Figs. 2 and 3).
Maximum principal stress values under cortical bone in the models under axial load and oblique load.
Peak maximum of stress for external hexagon, internal hexagon and Morse taper implant under axial and oblique load.
Connection Type
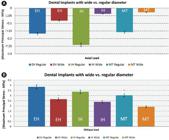
In the axial loading, MT and EH implants showed lower compressive stress than IH implant for regular diameter implants in axial loading, but in the wide diameter implants MT and IH implants showed lower compressive stress than EH (Fig. 4A). Oblique loading showed higher tensile compared to axial loading, EH and IH implants showed a higher tensile stress than MT implants, regardless of the implant diameter (Fig. 4B).
Means of stress in the cortical bone tissue in models with different connections and different diameter under axial load (A) and oblique load (B).
Region and Loading Analysis
In analysis of the different regions (mesial, distal, buccal and lingual) under axial loading, the proximal region (mesial and distal) had a higher compressive stress than the buccal and lingual area for both connection types, with higher compressive stress in the IH implants compared to other connections (Fig. 5A). Regarding oblique loading, higher tensile stress concentration was observed in distal and buccal area, with highest tensile stress in buccal of EH implants (Fig. 5B). Regardless of connection type and diameter, oblique loading showed higher tensile stress compared to axial loading which presented low compression stress in the analyzed models.
Means of stress in the different regions of cortical bone tissue with different connections.
Discussion
The results of this study do not support the first hypothesis tested; regardless of connection type, implants with a wide diameter showed more favorable biomechanical behavior when compared to implants with regular diameter. These results corroborate previous biomechanical studies that found a lower stress concentration for wide diameter implants 99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.,1212 Li, T; Yang, X; Zhang, D; Zhou, H; Shao, J; Ding, Y; et al.. Analysis of the biomechanical feasibility of a wide implant in moderately atrophic maxillary sinus region with finite element method. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:e1-8.,1313 Mohammed Ibrahim, M; Thulasingam, C; Nasser, KS; Balaji, V; Rajakumar, M; Rupkumar, P. Evaluation of design parameters of dental implant shape, diameter and length on stress distribution: A finite element analysis. J Indian Prosthodont Soc 2011;11:165-171.,1414 Baggi, L; Cappelloni, I; Di Girolamo, M; Maceri, F; Vairo, G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. J Prosthet Dent 2008;100:422-431., especially in short implants 1212 Li, T; Yang, X; Zhang, D; Zhou, H; Shao, J; Ding, Y; et al.. Analysis of the biomechanical feasibility of a wide implant in moderately atrophic maxillary sinus region with finite element method. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:e1-8..
Clinically, a lower stress concentration may contribute to lower marginal bone loss around the wide diameter implants 1515 Ozgur, GO; Kazancioglu, HO; Demirtas ,N; Deger, S; Ak, G. Risk factors associated with implant marginal bone loss: A retrospective 6-year follow-up study. Implant Dent 2016;25:122-127.,1616 Ibañez, C; Catena, A; Galindo-Moreno, P; Noguerol, B; Magán-Fernández, A; Mesa, F. Relationship between long-term marginal bone loss and bone quality, implant width, and surface. Int J Oral Maxillofac Implants 2016;31:398-405.. Thus, the use of implants with wide diameter should be indicated, especially when a discrepancy in the crown-implant ratio may directly increase stress concentration in the bone tissue 77 Moraes, SL; Verri, FR; Santiago, Jr JF; Almeida, DA; de Mello, CC; Pellizzer, EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J 2013;24:635-641.. There are situations in which the lack of adequate bone thickness can preclude the use of implants with a wide diameter, making it necessary to instead perform bone grafting 1717 Felice, P; Cannizzaro, G; Barausse, C; Pistilli, R; Esposito, M. Short implants versus longer implants in vertically augmented posterior mandibles: A randomized controlled trial with 5-year after loading follow-up. Eur J Oral Implantol 2014;7:359-369.; however, bone grafting in the mandibular region is associated with increased risk of complications and morbidity, which may limit its surgical benefits 1717 Felice, P; Cannizzaro, G; Barausse, C; Pistilli, R; Esposito, M. Short implants versus longer implants in vertically augmented posterior mandibles: A randomized controlled trial with 5-year after loading follow-up. Eur J Oral Implantol 2014;7:359-369.,1818 Esposito, M; Pistilli, R; Barausse, C; Felice, P. Three-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Eur J Oral Implantol 2014;7:383-395.. Thus, in situations where it is not possible to the use wide diameter implants, the alternative approach may involve using the most suitable connection type from a biomechanical point of view.
Further, this study rejected the second hypothesis, as there was a significant difference in stress distribution between the connection types. Specifically, Morse taper implants were biomechanically more favorable than other connections, especially during oblique loading. External hexagon implants under oblique loading showed greater stress in the cortical bone tissue, regardless of the diameter. Biomechanical superiority of Morse taper implants has been reported in the literature 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.,99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.. This connection has a favorable design with greater internal stability than that of other connection types (owing to better mechanical imbrication), which allows centralization of stress on the implant body and reduces stress in the cortical bone region 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.,99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300..
The unfavorable biomechanical behavior of the external hexagon implant may be due to the connection being out of the implant, which reduces the centralization of stress in the implant body, especially in the oblique loading 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.; further, it might contribute to increased stress in the bone tissue around the implant neck due to close contact with the cortical bone. Additionally, the width and/or height of the hexagon can contribute to the increase in stress concentration in the bone tissue region 1919 Gil, FJ; Aparicio, C; Manero, JM; Padros, A. Influence of the height of the external hexagon and surface treatment on fatigue life of commercially pure titanium dental implants. Int J Oral Maxillofac Implants 2009;24:583-590.. Therefore, the use of external hexagon implants should be avoided, especially in situations where there is an increase in the crown-implant ratio 77 Moraes, SL; Verri, FR; Santiago, Jr JF; Almeida, DA; de Mello, CC; Pellizzer, EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J 2013;24:635-641.,2020 Bayraktar, M; Gultekin, BA; Yalcin, S; Mijiritsky, E. Effect of crown to implant ratio and implant dimensions on periimplant stress of splinted implant-supported crowns: a finite element analysis. Implant Dent 2013;22:406-413., or in cases where use implants with a wide diameter is not feasible, since stress concentration in the cortical bone could exceed the physiological limits and consequently accelerate the bone resorption process, which could compromise the rehabilitation.
Regarding the applied loading, it was possible to observe higher stress concentration in the region of the cortical bone tissue for the oblique when compared to axial loading, rejecting the third hypothesis. These results are consistent with the literature 77 Moraes, SL; Verri, FR; Santiago, Jr JF; Almeida, DA; de Mello, CC; Pellizzer, EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J 2013;24:635-641.,88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.,99 Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.,1212 Li, T; Yang, X; Zhang, D; Zhou, H; Shao, J; Ding, Y; et al.. Analysis of the biomechanical feasibility of a wide implant in moderately atrophic maxillary sinus region with finite element method. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:e1-8.,2121 Papavasiliou, G; Kamposiora, P; Bayne SC; Felton, DA. Three-dimensional finite element analysis of stress-distribution around single tooth implants as a function of bony support, prosthesis type, and loading during function. J Prosthet Dent 1996;76:633-640.. This fact may be due to oblique loading tends to increase stress concentration on (compression) and against (tensile) the loading direction 88 Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.. Oblique loading should be considered more harmful to bone tissue, which may contribute to higher values of bone resorption over time. Thus, it is important to perform a rigorous occlusal adjustment to transfer the centric contacts allowing a distribution in the long axis of the implant, avoiding an oblique overload in the peri-implant region 77 Moraes, SL; Verri, FR; Santiago, Jr JF; Almeida, DA; de Mello, CC; Pellizzer, EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J 2013;24:635-641..
In addition to the factors analyzed in this study, other variables can compromise the biomechanical behavior of implant-supported prostheses, such as the increase in occlusal force relative to the direction of loading 2222 Ormianer, Z; Palti, A; Demiralp, B; Heller, G; Lewinstein, I; Khayat, PG. Implant-supported first molar restorations: Correlation of finite element analysis with clinical outcomes. Int J Oral Maxillofac Implants 2012;27:e1-e12.. However, all models analyzed in this study showed development of compressive and tensile stresses within physiological limits for human cortical bone (72 - 76 MPa for tensile stress, 140 - 170 MPa for compressive stress) 2121 Papavasiliou, G; Kamposiora, P; Bayne SC; Felton, DA. Three-dimensional finite element analysis of stress-distribution around single tooth implants as a function of bony support, prosthesis type, and loading during function. J Prosthet Dent 1996;76:633-640..
The finite element method has been used in dentistry to achieve greater understanding of biomechanical behavior and can be carefully extrapolated to clinical settings 2323 Van Staden, RC; Gua, H; Loo, YC. Application of the finite element method in dental implant research. Comput. Methods Biomech. Biomed. Engin2006;9:257-270.. Thus, when combined with well-designed clinical studies, the results of the current study could guide new strategies for addressing challenges associated with managing stress distribution in implant dentistry. However, the results should be interpreted with caution due to limitations such as factors related to the methodology, computer simulation and linearity elastic analysis, which consider bone tissue to be isotropic and homogenous and apply static occlusal loading 2424 Verri, FR; Cruz, RS; Souza Batista, VE; Almeida, DA; Verri AC, CA; et al.. Can the modeling for simplification of a dental implant surface affect the accuracy of 3D finite element analysis?. Comput Methods Biomech Biomed Engin 2016;19:1665-1672.,2525 Huang, CC; LanTH; Lee, HE; Wang, CH. The biomechanical analysis of relative position between implant and alveolar bone: Finite element method. J Periodontol 2011;82:489-496. Therefore, additional controlled and randomized clinical studies should be conducted in order to fully explore and evaluate the clinical implications of various biomechanical parameters in implant dentistry.
Within the limitation of this study can conclude that the increase in diameter was favorable for improved stress distribution in the cortical bone region, regardless of the connection type. Morse taper implants were associated with lower stress concentration than other connections, especially during oblique loading.
Acknowledgements
The authors acknowledge the Research Foundation of the State of São Paulo (FAPESP - Grant 2009/16164-7) and The Renato Archer Research Center, Campinas, SP, Brazil.
References
-
1Lemos, CA; Ferro-Alves, ML; Okamoto, R; Mendonça, MR; Pellizzer, EP. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J Dent 2016;47:8-17.
-
2Karthikeyan, I; Desai, SR; R Singh, R. Short implants: A systematic review. J Indian Soc Periodontol 2012;16:302-312.
-
3Esposito, M; Cannizzaro, G; Soardi, E; Pistilli, R; Piattelli, M; Corvino, V; et al.. Posterior atrophic jaws rehabilitated with prostheses supported by 6 mm-long, 4 mm-wide implants or by longer implants in augmented bone. Preliminary results from a pilot randomized controlled trial. Eur J Oral Implantol 2012;5:19-33.
-
4Vasco, MA; Hecke, MB; Bezzon, OL. Analysis of short implants and lateralization of the inferior alveolar nerve with 2-stage dental implants by finite element method. J Craniofac Surg 2011;22:2064-2071.
-
5Chang, SH; Lin, CL; Lin, YS; Hsue, SS; Huang, SR. Biomechanical comparison of a single short and wide implant with monocortical or bicortical engagement in the atrophic posterior maxilla and a long implant in the augmented sinus. Int J Oral Maxillofac Implants2012;27:102-111.
-
6Garaicoa-Pazmiño, C; Suárez-López del Amo, F; Monje, A; Catena, A; I. Ortega-Oller, I; Galindo-Moreno, P, et al.. Influence of crown/implant ratio on marginal bone loss: A systematic review. J Periodontol 2014;85:1214-1221.
-
7Moraes, SL; Verri, FR; Santiago, Jr JF; Almeida, DA; de Mello, CC; Pellizzer, EP. A 3-D finite element study of the influence of crown-implant ratio on stress distribution. Braz Dent J 2013;24:635-641.
-
8Faria Almeida, DA; Pellizzer, EP; Verri, FR; Santiago, JFJr; Carvalho, PS. Influence of tapered and external hexagon connections on bone stresses around tilted dental implants: Three-dimensional finite element method with statistical analysis. J Periodontol2014;85:261-269.
-
9Santiago, JF Jr; Verri FR; Almeida, DA; Souza Batista, VE; Lemos, CA; Pellizzer, EP. Finite element analysis on influence of implant surface treatments, connection and bone types. Mater Sci Eng C Mater Biol Appl 2016;63:292-300.
-
10Nishioka, RS; Vasconcellos, LG; Melo Nishioka, GN. Comparative strain gauge analysis of external and internal hexagon, Morse taper, and influence of straight and offset implant configuration. Implant Dent 2011;20:24-32.
-
11Verri, FR; R.S., Cruz; Lemos ,CA; Souza Bati, VE; Almeida, DA; Verri, AC; et al.. Influence of bicortical techniques in internal connection plac VEed in pre-maxillary area by 3D finite element analysis. Comput Methods Biomech Biomed Engin 2016;13:1-8.
-
12Li, T; Yang, X; Zhang, D; Zhou, H; Shao, J; Ding, Y; et al.. Analysis of the biomechanical feasibility of a wide implant in moderately atrophic maxillary sinus region with finite element method. Oral Surg Oral Med Oral Pathol Oral Radiol 2012;114:e1-8.
-
13Mohammed Ibrahim, M; Thulasingam, C; Nasser, KS; Balaji, V; Rajakumar, M; Rupkumar, P. Evaluation of design parameters of dental implant shape, diameter and length on stress distribution: A finite element analysis. J Indian Prosthodont Soc 2011;11:165-171.
-
14Baggi, L; Cappelloni, I; Di Girolamo, M; Maceri, F; Vairo, G. The influence of implant diameter and length on stress distribution of osseointegrated implants related to crestal bone geometry: A three-dimensional finite element analysis. J Prosthet Dent 2008;100:422-431.
-
15Ozgur, GO; Kazancioglu, HO; Demirtas ,N; Deger, S; Ak, G. Risk factors associated with implant marginal bone loss: A retrospective 6-year follow-up study. Implant Dent 2016;25:122-127.
-
16Ibañez, C; Catena, A; Galindo-Moreno, P; Noguerol, B; Magán-Fernández, A; Mesa, F. Relationship between long-term marginal bone loss and bone quality, implant width, and surface. Int J Oral Maxillofac Implants 2016;31:398-405.
-
17Felice, P; Cannizzaro, G; Barausse, C; Pistilli, R; Esposito, M. Short implants versus longer implants in vertically augmented posterior mandibles: A randomized controlled trial with 5-year after loading follow-up. Eur J Oral Implantol 2014;7:359-369.
-
18Esposito, M; Pistilli, R; Barausse, C; Felice, P. Three-year results from a randomised controlled trial comparing prostheses supported by 5-mm long implants or by longer implants in augmented bone in posterior atrophic edentulous jaws. Eur J Oral Implantol 2014;7:383-395.
-
19Gil, FJ; Aparicio, C; Manero, JM; Padros, A. Influence of the height of the external hexagon and surface treatment on fatigue life of commercially pure titanium dental implants. Int J Oral Maxillofac Implants 2009;24:583-590.
-
20Bayraktar, M; Gultekin, BA; Yalcin, S; Mijiritsky, E. Effect of crown to implant ratio and implant dimensions on periimplant stress of splinted implant-supported crowns: a finite element analysis. Implant Dent 2013;22:406-413.
-
21Papavasiliou, G; Kamposiora, P; Bayne SC; Felton, DA. Three-dimensional finite element analysis of stress-distribution around single tooth implants as a function of bony support, prosthesis type, and loading during function. J Prosthet Dent 1996;76:633-640.
-
22Ormianer, Z; Palti, A; Demiralp, B; Heller, G; Lewinstein, I; Khayat, PG. Implant-supported first molar restorations: Correlation of finite element analysis with clinical outcomes. Int J Oral Maxillofac Implants 2012;27:e1-e12.
-
23Van Staden, RC; Gua, H; Loo, YC. Application of the finite element method in dental implant research. Comput. Methods Biomech. Biomed. Engin2006;9:257-270.
-
24Verri, FR; Cruz, RS; Souza Batista, VE; Almeida, DA; Verri AC, CA; et al.. Can the modeling for simplification of a dental implant surface affect the accuracy of 3D finite element analysis?. Comput Methods Biomech Biomed Engin 2016;19:1665-1672.
-
25Huang, CC; LanTH; Lee, HE; Wang, CH. The biomechanical analysis of relative position between implant and alveolar bone: Finite element method. J Periodontol 2011;82:489-496
Publication Dates
-
Publication in this collection
Jan-Feb 2018
History
-
Received
11 Mar 2017 -
Accepted
11 Sept 2017