RESUMO
Objetivo:
analisar as produções científicas nacionais e internacionais sobre o impacto dos bundles na prevenção de infecção da corrente sanguínea relacionada ao cateter venoso central em unidade de terapia intensiva adulta.
Método:
revisão integrativa de artigos publicados no Portal Capes, Biblioteca Virtual em Saúde, PubMed, Science Direct, Cochrane, CINAHL e SCOPUS, entre 2011 e 2016.
Resultados:
encontraram-se 16 artigos, 100% relacionados à implementação dos bundles para a inserção do cateter venoso central e 50% à manutenção deste dispositivo. O tempo de intervenção foi variado, bem como o número de medidas e o período analisado (inserção/manutenção do cateter). No entanto, a redução da infecção da corrente sanguínea relacionada ao dispositivo foi apontada em todos os estudos entre 26% e 100%.
Conclusão:
a adoção de bundle evidenciou um impacto positivo na redução da infecção. Todavia, não se observou uma relação direta entre o número de medidas descritas nos estudos ou o maior tempo de implementação e taxas mais altas de redução da infecção.
DESCRITORES:
Infecções relacionadas a cateter; Cateteres; Unidade de terapia intensiva; Infecção hospitalar; Segurança do paciente
RESUMEN
Objetivo:
analizar las producciones científicas nacionales e internacionales sobre el impacto del bundles en la prevención de infección del flujo sanguíneo relacionado al catéter venoso central en unidad de terapia intensiva adulta.
Método:
revisión integrativa de artículos publicados en el Portal Capes, Biblioteca Virtual en Salud, PubMed, Science Direct, Cochrane, CINAHL y SCOPUS, entre 2011 y 2016.
Resultados:
se encontraron 16 artículos, 100% relacionados a la implementación de los lotes para la inserción del catéter venoso central y 50% al mantenimiento de este dispositivo. El tiempo de intervención fue variado, así como el número de medidas y el período analizado (inserción / mantenimiento del catéter). Sin embargo, la reducción de la infección del flujo sanguíneo relacionado con el dispositivo fue señalada en todos los estudios entre el 26% y el 100%.
Conclusión:
la adopción del lote evidenció un impacto positivo en la reducción de la infección. Sin embargo, no se observó una relación directa entre el número de medidas descritas en los estudios o el mayor tiempo de implementación y tasas más altas de reducción de la infección.
DESCRIPTORES:
Infecciones relacionadas con catéter; Catéteres; Unidad de terapia intensiva; Infección hospitalaria; Seguridad del paciente
ABSTRACT
Objective:
to analyze the national and international scientific research regarding the impact of the bundles in the prevention of central venous catheter-related bloodstream infection in an adult intensive care unit.
Method:
integrative review of articles published in Portal Capes, Virtual Health Library, PubMed, Science Direct, Cochrane, CINAHL and SCOPUS, between 2011 and 2016.
Results:
16 articles were found, 100% related to the implementation of the bundles for the insertion of the central venous catheter and 50% to related to the maintenance of this device. The intervention time was varied, as were the number of measurements and the analyzation period analyzed (catheter insertion / maintenance). However, all studies showed that there was a reduction of between 26% e 100% of bloodstream infections related to the use of the device.
Conclusion:
the adoption of the bundle showed a positive impact on the reduction of infections. However, there was no direct relationship between the number of measures described in the studies or length of implementation time or higher rates of infection reduction.
DESCRIPTORS:
Catheter-related infections; Catheters; Intensive care unit; Hospital infection; Patient safety
INTRODUÇÃO
As infecções relacionadas à assistência à saúde (IRAS) são definidas como uma condição local ou sistêmica resultante de uma reação adversa à presença de um agente infeccioso ou sua toxina e sem evidência de que a infecção estava presente ou incubada no momento da admissão do paciente em ambiente hospitalar ou ambulatorial. São diagnosticadas, em geral, a partir de 48 horas após a internação.11 World Health Organization. Report on the burden of endemic health care-associated infection worldwide. A systematic review of the literature. [Internet]. 2011[cited 2016 Jun 07]. Available from: http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf
http://apps.who.int/iris/bitstream/10665...
Citam-se como as principais IRAS: infecções do trato respiratório, trato urinário, corrente sanguínea e sítio cirúrgico.22 Agência Nacional de Vigilância Sanitária. Medidas de prevenção de infecção relacionada à assistência à saúde. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2013:1-87.
Dados do National Healthcare Safety Network (NHSN) revelam que, entre as IRAS, a infecção da corrente sanguínea relacionada ao cateter venoso central (CVC) representa a principal causa de infecção em Unidade de Terapia Intensiva (UTI).33 National Healthcare Safety Network. NHSN Central Line-associated Bloodstream Infection Surveillance in 2014. National Center for Emerging and Zoonotic Infectious Diseases. [Internet]. 2014 Mar [cited 2016 Feb 02]. Available from: http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf
http://www.cdc.gov/nhsn/PDFs/training/tr...
Estima-se que 30.000 novos casos desta infecção ocorrem em UTIs dos Estados Unidos a cada ano.44 National Healthcare Safety Network. Patient Safety Component Manual [Internet]. 2017 Jan [cited 2017 Feb 14]. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf
https://www.cdc.gov/nhsn/pdfs/pscmanual/...
Em 2014, ocorreram na Inglaterra 26,5 infecções por 1.000 cateteres/dias. Em outros países da Europa, em torno de 13,3 infecções para 1.000 cateteres/dia.55 Mok Q. How I diagnose and manage catheter-associated blood stream infections. J Paediatr Child Health [Internet]. 2015 May [cited 2016 Jun 07]; 25(5):243-4. Available from: http://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(14)00223-6/pdf
http://www.paediatricsandchildhealthjour...
-66 Martínez-Morel HR, Sánchez-Payá J, Molina-Gómez MJ, García-Shimizu P, García RV, Villanueva-Ruiz C, et al. Catheter-related bloodstream infection: burden of disease in a tertiary hospital. J Hosp Infect [Internet]. 2014 Jul [cited 2016 Feb 02]; 87(3):165-70. Available from: http://www.sciencedirect.com/science/article/pii/S0195670114001285
http://www.sciencedirect.com/science/art...
Esta infecção está associada ao aumento do tempo de internação entre 10 a 20 dias e ao custo de, aproximadamente, US$ 30,000.00 por paciente.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
A sistematização dos dados epidemiológicos sobre a infecção da corrente sanguínea relacionada ao CVC em UTI no Brasil foi iniciada em 2010, com a criação do FormSUS. As taxas dessa infecção variaram entre 4,1 e 5,1 infecções, a cada 1.000 CVC/dia, até 2015.88 Agência Nacional de Vigilância Sanitária. Avaliação dos indicadores nacionais de infecção relacionada à assistência ano de 2014 e relatório de progresso. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2015. Os dados sobre tempo extra de permanência e custos associados não são conhecidos em publicações oficiais.99 Souza ES, Belei RA, Carrilho CMDM, Matsuo T, Yamada-Ogatta SF, Andrade G et al. Mortalidade e riscos associados a infecção relacionada à assistência à saúde. Texto Contexto Enferm [Internet]. 2015 Jan-Mar [cited 2017 Feb 14]; 24(1): 220-8. Available from: http://www.redalyc.org/pdf/714/71438421027.pdf
http://www.redalyc.org/pdf/714/714384210...
Contudo, a taxa de mortalidade por infecção relacionada ao CVC em UTI pode atingir até 69% dos pacientes.22 Agência Nacional de Vigilância Sanitária. Medidas de prevenção de infecção relacionada à assistência à saúde. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2013:1-87.
O uso de dispositivo intravascular, principalmente o CVC, constitui o principal fator de risco para a infecção da corrente sanguínea, sendo que, aproximadamente, 90% dessas estão relacionados a seu uso.33 National Healthcare Safety Network. NHSN Central Line-associated Bloodstream Infection Surveillance in 2014. National Center for Emerging and Zoonotic Infectious Diseases. [Internet]. 2014 Mar [cited 2016 Feb 02]. Available from: http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf
http://www.cdc.gov/nhsn/PDFs/training/tr...
,1010 The Joint Commission. Preventing central line-associated bloodstream infections: a global challenge, a global perspective. Oak Brook, IL: Joint Commission Resources. [Internet]. 2012 May [cited 2016 Feb 02]. Available from: https://www.jointcommission.org/assets/1/18/CLABSI_Monograph.pdf
https://www.jointcommission.org/assets/1...
As infecções da corrente sanguínea relacionadas ao CVC são consideradas, na maioria dos casos, uma complicação evitável à segurança do paciente, podendo ser prevenidas por meio de intervenções, durante a inserção e a manipulação dos cateteres. O Institute for Health Improvement promoveu, em 2004, a campanha "Salve 100.000 vidas", na qual introduziu o conceito de central line bundle, que se fundamenta na adoção de um conjunto de medidas baseadas em evidências científicas combinadas e integradas para a redução destas infecções.1111 Institute for Health Improvement. Protecting 5 million lives. Cambridge [Internet]. 2004 [cited 2016 Jun 07]. Available from: http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx
http://www.ihi.org/engage/initiatives/co...
Tais medidas são descritas pelo Center for Disease Control and Prevention (CDC) e têm sido incluídas, na prática clínica, em forma de um pacote de intervenções, denominado bundles.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
,1111 Institute for Health Improvement. Protecting 5 million lives. Cambridge [Internet]. 2004 [cited 2016 Jun 07]. Available from: http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx
http://www.ihi.org/engage/initiatives/co...
-1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
Existem várias medidas sugeridas para prevenir infecção relacionada ao CVC, que compõem os bundles, podendo ser realizadas separadamente ou em conjunto. A necessidade de cada instituição deve ser considerada prioritariamente, além do perfil do paciente atendido, dos recursos humanos e materiais, da disponibilidade de um trabalho de educação, do treinamento e da vigilância com a equipe responsável pela inserção, da manutenção e dos cuidados com os dispositivos intravenosos.1313 Labeau SO, Vandijck DM, Rello J, Adam S, Rosa A, Wenisch C, et al. Centers for Disease Control and Prevention guidelines for preventing central venous catheter-related infection: results of a knowledge test among 3405 European intensive care nurses. Crit Care Med [Internet]. 2009 Jan [cited 2016 Jun 07]; 37(1):320-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19050628
http://www.ncbi.nlm.nih.gov/pubmed/19050...
-1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
Os bundles têm sido amplamente divulgados e estão sendo implementados nas instituições hospitalares. Sua adoção tem sido apontada como eficaz na prevenção e redução da infecção da corrente sanguínea relacionada ao CVC e na melhoria da qualidade dos serviços prestados. Contudo, ainda é baixa a adesão dos profissionais a essas medidas, o que acarreta elevada incidência dessa infecção. Outra lacuna do conhecimento é a ausência de estudos que abordem o resultado da adesão dos profissionais de saúde às recomendações das práticas de prevenção dessa infecção. Por isso, estratégias que apontem subsídios para a melhoria da prática clínica e o aumento da segurança do paciente devem ser incentivadas, sobretudo aquelas voltadas ao período da inserção e manutenção do CVC.
O conhecimento das equipes responsáveis pela inserção e manutenção do CVC acerca do bundle e de seu impacto na prevenção da infecção da corrente sanguínea pode apontar evidências de que práticas seguras precisam ser cultivadas na atenção ao paciente, principalmente aqueles em condições críticas. Isso poderia ser utilizado na revisão de práticas de inserção e manipulação do CVC, refletindo em melhor qualidade da assistência e na redução da morbidade e da mortalidade decorrentes dessa infecção.
Considerando-se a importância da utilização do bundle na prática clínica para a redução das infecções da corrente sanguínea, objetivou-se analisar as produções científicas nacionais e internacionais sobre o impacto dos bundles na prevenção de infecção da corrente sanguínea relacionada ao CVC em UTI adulta.
MÉTODO
Trata-se de uma de uma revisão integrativa da literatura, cuja finalidade consistiu em reunir e sintetizar as evidências disponíveis em artigos originais produzidos sobre o tema.
Para a condução da revisão, buscou-se fundamentação no escopo das evidências científicas que compõem o foco da investigação: implementação e impacto da adoção do bundle na prática clínica, pela identificação de uma questão de enorme relevância prática. No plano concreto, adotou-se a estratégia PICO, que se estrutura da seguinte forma: P=Paciente, I=Intervenção, C=Comparação e O=Outcomes (desfecho).1515 Santos CMC, Pimenta CAM, Nobre MRC. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev Latino-Am. Enfermagem [Internet]. 2007 Jun [cited 2016 Aug 01]; 15(3):508-11. Available from: http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext&tlng=pt
http://www.scielo.br/scielo.php?pid=S010...
Com base nessa estratégia, definiu-se como pergunta de pesquisa: o que as produções científicas nacionais e internacionais apontam sobre o impacto dos bundles na prevenção de infecção da corrente sanguínea relacionada ao CVC em UTI adulta.
A busca dos artigos foi realizada pelas bibliotecas do Portal Capes e a Biblioteca Virtual em Saúde; e as bases eletrônicas de dados U.S. National Library of Medicine (PubMed), Science Direct, Cochrane, Cumulative Index to Nursing and Allied Health Literature (CINAHL) e SCOPUS.
Definiram-se como critérios de inclusão: artigos originais que abordassem o impacto dos bundles na redução de infecção da corrente sanguínea relacionada ao CVC em UTI adulta, independente do método de pesquisa empregado, além de terem sido publicados a partir 2011, por ser o ano em que o CDC publicou o último guideline sobre a prevenção de infecções relacionadas a dispositivo intravascular, excluindo todos os demais.
Foram utilizados os seguintes descritores controlados: infecções relacionadas a cateter, cateteres, unidade de terapia intensiva e infecção hospitalar. Como descritores não controlados: bundle, redução das taxas de infecção, cateter venoso central, prevenção e infecção da corrente sanguínea. Todos esses descritores foram utilizados isoladamente e em conjunto, com o auxílio dos operadores booleanos.
A partir da associação entre todos os descritores controlados e não controlados, identificaram-se 36 artigos, que, após sua leitura na íntegra, foram reduzidos a 16, considerando-se o critério de inclusão de abordagem, a implementação dos bundles e seu potencial impacto na prática clínica.
Os níveis de evidências foram caracterizados de forma hierárquica, dependendo da abordagem metodológica adotada, com base na categorização classificada em seis níveis:1616 Stetler CB, Morsi D, Rucki S, Broughton S, Corrigan B, Fitzgerald J, et al. Utilization-focused integrative reviews in a nursing service. Appl Nurs Res [Internet]. 1998 Nov [cited 2016 Mar 01]; 11(4):1-11. Available from: http://www.appliednursingresearch.org/article/S0897-1897(98)80329-7/pdf
http://www.appliednursingresearch.org/ar...
-
nível 1: evidências resultantes da meta-análise (estudos clínicos controlados e randomiza dos);
-
nível 2: evidências obtidas de estudos com delineamento experimental;
-
nível 3: evidências de estudos quase experimentais;
-
nível 4: evidências de estudos descritivos (não experimentais) ou com abordagem qualitativa;
-
nível 5: evidências provenientes de relatos de caso ou de experiência;
-
nível 6: evidências baseadas em opiniões ou consensos de especialistas.
RESULTADOS
Com base nos critérios de inclusão, a amostra final ficou constituída por 16 artigos, assim distribuídos nas bases de dados: Science Direct (5/16), Pubmed (9/16) e Cinahl (2/16). Quanto ao delineamento da pesquisa, verificaram-se estudos de coorte (16/16), nível de evidência 2, realizados na Arábia Saudita (1/16), Austrália (1/16), Bélgica (1/16), Brasil (1/16), Estados Unidos (7/16), Inglaterra (1/16), Kuait (1/16), Nova Zelândia (1/16), Suécia (1/16) e Taiwan (1/16) e publicados nos anos de 2011 (2/16), 2012 (1/16), 2013 (3/16), 2014 (7/16), 2015 (2/16) e 2016 (1/16).
Em 100% dos artigos pesquisados foram implementados bundles no período da inserção do CVC e em 50% durante sua manutenção, cujas medidas e resultados alcançados se encontram descritas no quadro 1, atendendo aos pressupostos de intervenção, comparação e desfecho, com destaque para o fato de que todos os estudos estiveram voltados para pacientes internados em UTI adulta.
Síntese das medidas implementadas para prevenção de infecção relacionada ao cateter venoso central, de acordo com o momento de sua indicação (inserção, manutenção e outras), a duração da intervenção e a taxa de redução. Belo Horizonte, MG, Brasil, 2016. (n=16)
As medidas implementadas no bundle de inserção do CVC foram: barreira máxima de precaução (uso de luva estéril, gorro, máscara, capote e campo estéril - 94% dos estudos);1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
18 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
19 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
20 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
21 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
22 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
23 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
24 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
-2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2727 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
28 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
29 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
assepsia da pele (94%);1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
18 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
19 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
20 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
21 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
22 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
23 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
24 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
-2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2727 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
28 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
29 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
higiene das mãos antes da inserção (62%);1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
24 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
25 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
26 Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
http://www.sciencedirect.com/science/art...
27 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
-2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
preferência pela veia subclávia (44%);1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2727 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
evitar veia femoral (37%);1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
remoção imediata do CVC sem indicação clínica para seu uso (37%);1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2626 Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
http://www.sciencedirect.com/science/art...
,2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
ultrassom para guiar a inserção do cateter (19%);1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
deixar o antisséptico secar antes de inserir o cateter (12%);2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
CVC impregnado com antibiótico (12%);2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
-2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
substituir o CVC que foi inserido sem técnicas assépticas em até 48 horas (12%);1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
e designar apenas profissionais qualificados para inserir o CVC (12%).2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
-2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
O bundle de manutenção compreendeu: verificação diária da necessidade de permanência do CVC (87%);1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2929 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
desinfecção do hub antes de administrar medicamentos (62%);1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
monitorar o local de inserção (50%);1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2222 Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
http://www.sciencedirect.com/science/art...
,2929 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
substituição do curativo com gaze estéril a cada dois dias e curativo transparente a cada sete dias ou sempre que estiverem sujo, solto ou úmido (50%);1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
higiene das mãos antes da manipulação (37%);1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
e assepsia da pele ao trocar o curativo (25%).1818 Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
http://www.iqg.com.br/pbsp/img_up/013058...
,3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
Outras medidas que também compuseram os bundle foram referidas nos artigos, sendo: treinamento e educação permanente aos profissionais que inserem e manipulam os CVC em 56%;1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
26 Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
http://www.sciencedirect.com/science/art...
27 Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
http://www.ncbi.nlm.nih.gov/pubmed/24837...
28 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
29 Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
e feedback dos resultados, apontados em 31%.1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2121 Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2424 Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
http://www.sciencedirect.com/science/art...
,2828 Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
http://www.sciencedirect.com/science/art...
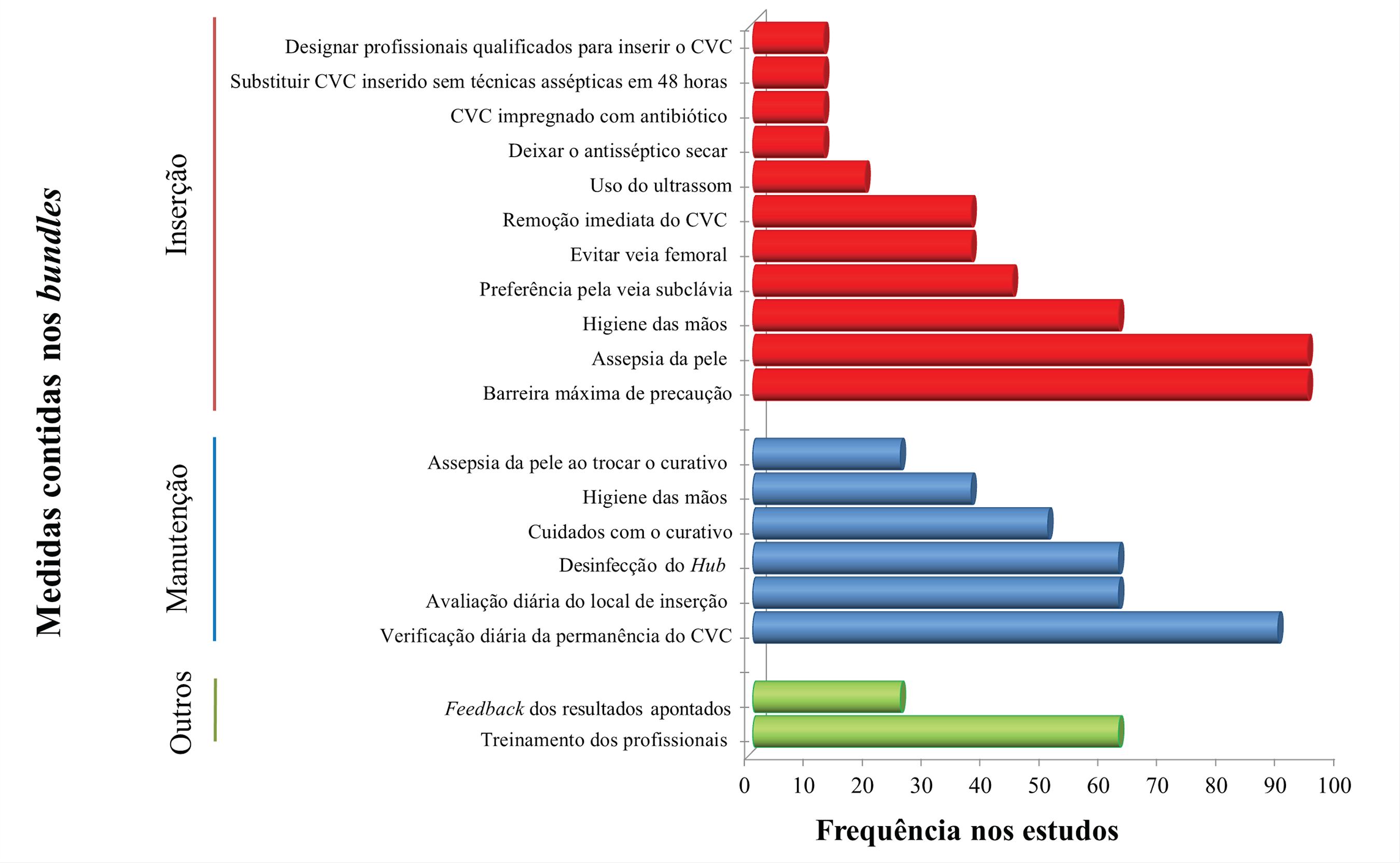
A frequência com que foram descritas as medidas nos estudos estão apresentadas na figura 1.
Frequência das medidas contidas nos bundles (intervenções), observados nos estudos publicados. Belo Horizonte, MG, Brasil, 2016
As medidas contidas no bundle para prevenir infecção relacionada ao CVC foram classificadas de acordo com os níveis de evidências e divididas em categorias IA, IB, IC e II, e com o assunto não resolvido.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
Essas classificações são utilizadas para demonstrar quais medidas preventivas apresentam melhores evidências científicas para aplicabilidade na prática clínica, de forma isolada ou ao comporem um bundle. Assim, associou-se a frequência das medidas adotadas nos estudos analisados ao momento de sua indicação com base nos níveis de evidências, de acordo com a figura 2.
Frequência das medidas adotadas nos estudos analisados, por nível de evidência. Belo Horizonte, MG, Brasil, 2016
Relacionou-se, também, a quantidade de medidas que compuseram o bundle em cada estudo com a duração da intervenção e a taxa de redução das infecções da corrente sanguínea relacionada ao CVC após a implementação do bundle. Os resultados estão expostos na figura 3.
Frequência das medidas adotadas nos estudos analisados, por duração da intervenção e taxa de redução. Belo Horizonte, MG, Brasil, 2016
O impacto do bundle na redução dos custos das infecções foi mensurado apenas em dois artigos, apontando-se uma economia de US$ 539.902,00 e US$ 198.600,00 em cada um deles após sua implementação.1414 Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
http://www.ncbi.nlm.nih.gov/pubmed/24576...
,1919 Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
http://www.sciencedirect.com/science/art...
Apesar de não ser objetivo deste estudo, ressalta-se que os agentes relacionados à causa das infecções da corrente sanguínea em decorrência do CVC foram descritos em apenas 31% dos estudos, citando-se: Staphylococcus coagulase negativa, Staphylococcus aureus, Enterococcus spp, Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa e Candida spp.1212 Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
http://www.ncbi.nlm.nih.gov/pubmed/26138...
,1717 Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
http://www.sciencedirect.com/science/art...
,2020 Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
http://www.ncbi.nlm.nih.gov/pmc/articles...
,2323 Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
http://www.ncbi.nlm.nih.gov/pubmed/24485...
,2525 Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
http://www.ncbi.nlm.nih.gov/pmc/articles...
Foram encontradas nos estudos 19 medidas que compuseram os bundles para prevenir as infecções da corrente sanguínea relacionadas ao CVC. Destas, 11 foram utilizadas para a inserção do cateter, seis durante a manutenção e dois em educação continuada e feedback dos resultados como parte global do processo.
Medidas classificadas com níveis de evidências IA foram menos utilizadas para compor os bundles. Por exemplo, para: inserção do CVC: preferência pela veia subclávia (44%), evitar a inserção na femoral (37%), remoção imediata do CVC sem indicação clínica (37%), CVC impregnado com antibiótico (12%) e designar apenas profissionais qualificados para inserir o CVC (12%). Durante a manutenção do cateter: assepsia da pele ao trocar o curativo (25%). E, como outras medidas: treinamento e educação continuada dos profissionais (62%) e feedback dos resultados (31%).
DISCUSSÃO
O risco de infecção da corrente sanguínea também está relacionado com o sítio anatômico de inserção do cateter,77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
com destaque maior para inserção na femoral e menor para subclávia, cujo fator preponderante é a quantidade e diversidade de microrganismos encontrados em cada uma das regiões supracitadas.3030 Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
http://www.ncbi.nlm.nih.gov/pubmed/25758...
O cateterismo na veia subclávia tem sido associado a uma menor taxa de infecção, em comparação com a femoral. Estudos realizados em UTIs nos Estados Unidos, ao compararem as complicações infecciosas e a colonização desses dois sítios de inserção, constataram que a incidência de complicações infecciosas pela femoral foi 3,75 maior que na subclávia e que a taxa de colonização do cateter foi de 20% para femoral e 4% para subclávia.3232 Merrer J, Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically III patients a randomized controlled trial. JAMA [Internet]. 2001 Aug [cited 2016 May 07]; 286(6):700-7. Available from: http://jama.jamanetwork.com/article.aspx?articleid=194073
http://jama.jamanetwork.com/article.aspx...
-3333 Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med [Internet]. 2015 Sep [cited 2016 May 07]; 373:1220-9. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1500964#t=article
http://www.nejm.org/doi/full/10.1056/NEJ...
Outro achado se refere à não ênfase absoluta na atenção à remoção imediata do CVC sem indicação clínica. As diretrizes do CDC recomendam fortemente tal medida, visto que o risco de desenvolver infecção da corrente sanguínea aumenta a cada dia de uso.3434 Burdeu G, Currey J, Pilcher D. Idle central venous catheter-days pose infection risk for patients after discharge from intensive care. Am J Infect Control [Internet]. 2014 Apr [cited 2016 Jun 07]; 42(4):453-55. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313013692
http://www.sciencedirect.com/science/art...
Em um hospital universitário nos Estados Unidos verificou a permanência e a indicação do CVC, chegando à seguinte inferência: para 1.433 cateteres dia, 25% não tinham indicação para uso.3535 Tejedor SC, Tong D, Stein J, Payne C, Dressler D, Xue W et al. Temporary central venous catheter utilization patterns in a large tertiary care center: tracking the "idle central venous catheter". Infect Control Hosp Epidemiol [Internet]. 2012 Jan [cited 2016 May 13]; 33(1):50-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22173522
http://www.ncbi.nlm.nih.gov/pubmed/22173...
De forma semelhante, em outra realidade norte americana, o percentual de pacientes que utilizavam o CVC de forma desnecessária foi de 48,9%.3636 Tiwari MM, Hermsen ED, Charlton ME, Anderson JR, Rupp ME. Inappropriate intravascular device use: a prospective study. J Hosp Infect [Internet]. 2011 Jun [cited 2016 Jun 07]; 78(2):128-32. Available from: http://www.sciencedirect.com/science/article/pii/S0195670111001149
http://www.sciencedirect.com/science/art...
O uso do cateter sem indicação clínica é considerado um fator de risco e as taxas de infecção da corrente sanguínea podem ser reduzidas drasticamente se os CVCs forem avaliados diariamente, para se verificar a necessidade e o tempo de uso e, assim, serem removidos imediatamente quando não mais necessários.3636 Tiwari MM, Hermsen ED, Charlton ME, Anderson JR, Rupp ME. Inappropriate intravascular device use: a prospective study. J Hosp Infect [Internet]. 2011 Jun [cited 2016 Jun 07]; 78(2):128-32. Available from: http://www.sciencedirect.com/science/article/pii/S0195670111001149
http://www.sciencedirect.com/science/art...
A assepsia do local de inserção do CVC,com solução com clorexidina alcóolica >0,5%, a cada troca de curativos tem sido recomendada pela diretriz do CDC para prevenção da infecção relacionada ao CVC, por reduzir a carga microbiana local. A clorexidina é amplamente utilizada como um antisséptico nos cuidados de saúde, devido a sua excelente atividade antimicrobiana, a seu efeito residual prolongado e a sua rápida ação. As taxas de infecção da corrente sanguínea podem ser reduzidas de forma significativa quando a assepsia é realizada a cada troca de curativo.3737 Weber DJ, Rutala WA. Central line-associated bloodstream infections: prevention and management. Infect Dis Clin North Am [Internet]. 2011 Mar [cited 2016 May 01]; 5(1):77-102. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21315995
http://www.ncbi.nlm.nih.gov/pubmed/21315...
-3838 Chen W, Li S, Li L, Wu X, Zhang W. Effects of daily bathing with chlorhexidine and acquired infection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus: a meta-analysis. J Thorac Dis. 2013 Aug [cited 2016 Jun 15]; 5(4):518-24. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755671/
http://www.ncbi.nlm.nih.gov/pmc/articles...
Com a limpeza diária do sítio de inserção do CVC com clorexidina 2% durante um ano de intervenção, foi possível obter uma redução de 58% das taxas de infecção em uma UTI de um hospital público em Chicago.3939 Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med [Internet]. 2007 Oct [cited 2016 Jun 15]; 167(19):2073-9. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=413356
http://archinte.jamanetwork.com/article....
De forma semelhante, também em Chicago, a mesma intervenção proporcionou uma redução de 99% das infecções.4040 Munoz-Price LS, Hota B, Stemer A, Weinstein RA. Prevention of bloodstream infections by use of daily chlorhexidine baths for patients at a long-term acute care hospital. Infect Control Hosp Epidemiol [Internet]. 2009 Nov [cited 2016 Jun 15]; 30(11):1031-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19751155
http://www.ncbi.nlm.nih.gov/pubmed/19751...
Utilizando projeto similar, uma redução de 50% na incidência de Enterococcus ssp resistentes a vancomicina e 32% para Staphylococcus aureus resistente a meticilina em um período de seis meses.4141 Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med [Internet]. 2009 Jun [cited 2016 Jun 15]; 37(6):1858-65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19384220
http://www.ncbi.nlm.nih.gov/pubmed/19384...
O uso de clorexidina alcóolica a cada troca de curativos tem sido considerado uma prática simples de implementar, com baixo custo e grande impacto na redução das infecções da corrente sanguínea.4141 Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med [Internet]. 2009 Jun [cited 2016 Jun 15]; 37(6):1858-65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19384220
http://www.ncbi.nlm.nih.gov/pubmed/19384...
Os programas de educação permanente e de treinamento dos profissionais de saúde têm demonstrado eficácia na prevenção e redução das infecções relacionadas ao CVC, além de melhorarem a qualidade dos serviços prestados. Para garantir a qualidade desses programas, devem-se incluir: técnicas adequadas à inserção e manutenção do CVC, avaliação periódica do conhecimento, adesão em relação às medidas adotadas, vigilância e notificação das infecções, feedback dos resultados obtidos quanto à redução das infecções e auditoria dos processos e resultados.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
,4242 Chesshyre E, Goff Z, Bowen A, Carapetis J. The prevention, diagnosis and management of central venous line infections in children. J infect [Internet]. 2015 Jun [cited 2016 Jul 07]; 71(1):59-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25934326
http://www.ncbi.nlm.nih.gov/pubmed/25934...
-4343 Cherry RA, West CE, Hamilton MC, Rafferty CM, Hollenbeak CS, Caputo GM. Reduction of central venous catheter associated blood stream infections following implementation of a resident oversight and credentialing policy. Patient Saf Surg [Internet]. 2011 Jun [cited 2016 Jun 07]; 5:2-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123176/
http://www.ncbi.nlm.nih.gov/pmc/articles...
Uma intervenção educacional na equipe multidisciplinar na UTI de um hospital de Saint Louis nos Estados Unidos, com duração de três anos, em que foram abordadas as medidas recomendadas durante a inserção e manutenção do CVC, resultou na redução de 66% das taxas de infecções da corrente sanguínea.4444 Zack J. Zeroing in on zero tolerance for central line-associated bacteremia. Am J Infect Control [Internet]. 2008 Dec [cited 2016 Jul 07]; 36(10):176. Available from: http://www.sciencedirect.com/science/article/pii/S0196655308007992
http://www.sciencedirect.com/science/art...
Por isso, torna-se também importante designar apenas profissionais treinados que demonstrem competência para inserção e manutenção do CVC,77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
além de prever um treinamento com abordagem global e multidisciplinar, incluindo intervenções comportamentais e educacionais em toda a equipe envolvida na inserção e manutenção desses cateteres.4545 Esposito S, Purrello SM, Bonnet E, Noveli A, Tripodi F, Pascale R. et al. Central venous catheter-related biofilm infections: an up-to-date focus on meticillin-resistant Staphylococcus aureus. J Glob Antimicrob Resist [Internet]. 2013 Apr [cited 2016 Jul 07]; 1(1):71-8. Available from: https://www.researchgate.net/publication/236889298
https://www.researchgate.net/publication...
Outras medidas também compuseram os bundles e apresentaram um nível de evidência IB, sendo fortemente recomendadas para implementação,77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
citando-se: barreira máxima de precaução, assepsia da pele, higiene das mãos antes da inserção, uso do ultrassom para guiar a inserção do cateter, deixar o antisséptico secar antes de inserir o cateter e substituir o CVC inserido sem técnicas assépticas em até 48 horas. As medidas associadas à manutenção do cateter foram: verificar a necessidade de permanência do CVC, monitorar o local de inserção, desinfecção do hub antes de administrar medicamentos, substituição do curativo com gaze estéril a cada dois dias e curativo transparente a cada sete dias ou sempre que estiverem sujo, solto ou úmido e higiene das mãos antes da manipulação.
A barreira máxima de precaução consiste na paramentação com luva estéril, gorro, máscara, capote e campo estéril, o que contribui para diminuir a contaminação pela microbiota do profissional e do ambiente para o paciente no momento da inserção do CVC e o subsequente risco de infecção.4646 Matsui Y, Shimatani M, Kuzuhara K, Miyazaki Y, Horiuchi T, Tajima Y, et al. Three-year prospective, observational study of central line-associated bloodstream infections in a 600-bed Japanese acute care hospital. Am J Infect Control [Internet]. 2015 Feb [cited 2016 Jul 07]; 43(5):294-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25737305
http://www.ncbi.nlm.nih.gov/pubmed/25737...
O mesmo ocorre quando se faz assepsia da pele antes da inserção do cateter, em que é recomendado o uso da clorexidina alcóolica >0,5%, que deve ser deixada secar antes de inserir o CVC. Dessa forma, irá promover um efeito residual e reduzir a propagação de microrganismos extraluminal em direção ao local de inserção do cateter.4747 Garcia R. Surgical skin antisepsis. Perioperative Nursing Clinics [Internet]. 2011 Dec [cited 2016 Jul 07]; 5(4):457-77. Available from: http://www.periopnursing.theclinics.com/article/S1556-7931(10)00064-1/pdf
http://www.periopnursing.theclinics.com/...
A higienização das mãos constitui uma das principais medidas para prevenir as IRAS. Por isso, torna-se essencial higienizá-las antes da inserção e manipulação do CVC, para minimizar a propagação de microrganismos patogênicos pelas mãos dos profissionais de saúde e a consequente contaminação do cateter.4848 World Health Organization. Evidence for Hand Hygiene Guidelines. [Internet]. 2016 [cited 2016 Jul 07]. Available from: http://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/
http://www.who.int/gpsc/tools/faqs/evide...
-4949 Garret Jr JH. Summary of evidence-based practices for bloodstream infection prevention across the health care continuum of care for vascular access clinicians: addressing the 3 common sources of health care-associated infection transmission. J Vasc Access [Internet]. 2016 Jun [cited 2016 Jul 07]; 21(2):72-4. Available from: http://www.sciencedirect.com/science/article/pii/S1552885516300265
http://www.sciencedirect.com/science/art...
O uso do ultrassom para guiar a inserção do CVC tem sido utilizado na prática clínica para minimizar a ocorrência de complicações mecânicas, como hemorragia, pneumotórax, arritmias e punção arterial. Além disso, tem demonstrado ser capaz de reduzir o tempo de duração do procedimento e o número de tentativas desnecessárias para canular a veia.5050 Ozakin E, Can R, Acar N, Balogu Kaya F, Cevik AA. An evaluation of complications in ultrasound-guided central venous catheter insertion in the emergency department. Turk J Emerg Med [Internet]. 2014 Feb [cited 2016 Jul 10]; 14(2):53-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909866/
http://www.ncbi.nlm.nih.gov/pmc/articles...
-5151 Bayci AWL, Mangla J, Jenkins CS, Ivascu FA, Robbins JM. Novel educational module for subclavian central venous catheter insertion using real-time ultrasound guidance. J Surg Educ [Internet]. 2015 Nov-Dec [cited 2016 Jul 10]; 72(6):1217-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26481424
http://www.ncbi.nlm.nih.gov/pubmed/26481...
Quando a adesão à técnica asséptica não puder ser garantida, ou seja, cateteres inseridos em situação de emergência, estes devem ser substituídos em até 48 horas, devido ao aumento da possibilidade de infecção da corrente sanguínea.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
Verificar a necessidade de permanênciado CVC torna-se importante para que haja o acompanhamento dos dias de uso do cateter pelo paciente, visto que o tempo de permanência é um fator de risco para as infecções da corrente sanguínea e, também, permite que o CVC possa ser removido imediatamente quando não tiver mais indicação clínica para seu uso. O local de inserção também deve ser monitorado. Se o paciente apresentar sensibilidade no local, febre ou outra manifestação sugestiva de infecção, o CVC deve ser avaliado e considerado como possível fonte de infecção.77 Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
http://www.cdc.gov/hicpac/pdf/guidelines...
A desinfecção do hub antes de administrar medicamentos deve ser feita pela fricção alcóolica por 15 a 30 segundos, a fim de se evitar/reduzir a propagação dos microrganismos presentes no hub para o lúmen interno do cateter.5252 Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, et al. Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect [Internet]. 2014 Jan [cited 2016 Jul 10]; 86(1):1-70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24330862
http://www.ncbi.nlm.nih.gov/pubmed/24330...
Devido à sua relevância, esta medida tornou-se uma campanha da Association for Professionals in Infection Control and Epidemiology, denominada "Scrub the Hub", cujas finalidades eram: reduzir as infecções, educar, conscientizar e incentivar os profissionais a desinfetar o hub cuidadosamente antes de qualquer manipulação. Desde então, tem sido amplamente divulgada e recomendada.5353 Association for professionals in infection control and epidemiology. Guide to the elimination of catheter-related bloodstream infections. Washington [Internet]. 2009 [cited 2016 Jul 10]. Available from: http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf
http://www.apic.org/Resource_/Eliminatio...
-5454 Sannoh S, Clones B, Munoz J, Montecalvo M, Parvez B. A multimodal approach to central venous catheter hub care can decrease catheter-related bloodstream infection. Am J Infect Control [Internet]. 2010 Aug [cited 2016 Jul 20]; 36(8):424-29. Available from: http://www.sciencedirect.com/science/article/pii/S0196655309009493
http://www.sciencedirect.com/science/art...
Os curativos oclusivos devem ser substituídos conforme recomendado, pois a umidade da pele e a presença de sujidade e secreções promovem um ambiente propício ao crescimento microbiano. O curativo feito com gaze estéril deve ser trocado em até 48 horas, devido à dificuldade de visualizar o local de inserção e à possibilidade de umedecer-se durante o banho. O curativo transparente semipermeável de poliuretano permite a visualização do local de inserção e, por isso, requer trocas menos frequentes, podendo ficar até sete dias ou sempre que estiver sujo, solto ou úmido.5555 Frasca D, Dahyot-Fizelier C, Mimoz O. Prevention of central venous catheter-related infection in the intensive care unit. Crit Care [Internet]. 2010 Mar [cited 2016 Jul 20]; 14:212. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2887105/
http://www.ncbi.nlm.nih.gov/pmc/articles...
56 Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O'Grady NP, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol [Internet]. 2014 Jul [cited 2016 Jul 20]; 35(7):753-71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24915204
http://www.ncbi.nlm.nih.gov/pubmed/24915...
-5757 Oliveira FJG, Caetano JA, Silva VM, Almeida PC, Rodrigues AB, Siqueira JF. O uso de indicadores clínicos na avaliação das práticas de prevenção e controle de infecção de corrente sanguínea. Texto Contexto Enferm [Internet]. 2015 Out-Dez [cited 2016 Set 14]; 24(4):1018-26. Available from: http://www.scielo.br/pdf/tce/v24n4/pt_0104-0707-tce-24-04-01018.pdf.
http://www.scielo.br/pdf/tce/v24n4/pt_01...
A implementação e a adesão das medidas contidas nos bundles, além de reduzirem as taxas de infecção, têm grande impacto econômico nos custos gerados pelas infecções, como comprovado por alguns estudos analisados, que atestaram uma redução de US$ 539.902,00 e US$ 198.600,00 em relação às infecções da corrente sanguínea relacionadas ao CVC. Estimativas do NHSN e do CDC demonstraram que os custos anuais gerados pelas IRAS foram de aproximadamente US$ 9,8 bilhões. Dentre as IRAS, destacam-se as infecções da corrente sanguínea, com um custo por tratamento de US$ 45.814,00. Quando essas infecções estão associadas a um microrganismo resistente, por exemplo, Staphylococcus aureus resistente a meticilina, esse custo aumenta para US$ 58.614,00. Esses dados demonstram a necessidade de promover maiores progressos na prevenção dessas infecções, bem como de investigar e melhorar a qualidade dos serviços prestados e esforços políticos.5858 Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections a meta-analysis of costs and financial impact on the us health care system. JAMA Intern Med [Internet]. 2013 Dec [cited 2016 Jul 20]; 173(22):2039-46. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=1733452
http://archinte.jamanetwork.com/article....
CONCLUSÃO
A implementação dos bundles reduz as infecções da corrente sanguínea relacionadas ao CVC, independente do tempo de intervenção e da quantidade de medidas utilizadas. No entanto, constataram-se variações nos estudos em relação a: números de medidas implementadas, tempo de duração e redução das taxas de infecção. Não se observou uma relação direta entre o número de medidas descritas nos estudos ou do maior tempo de implementação, e as maiores taxas de redução da infecção. Possivelmente, esse achado não pode ser explicado diretamente, devido a aspectos que não foram apresentados pelos autores dos estudos analisados, como motivação das equipes, cultura institucional de segurança, feedback dos resultados aos profissionais e treinamentos.
REFERÊNCIAS
-
1World Health Organization. Report on the burden of endemic health care-associated infection worldwide. A systematic review of the literature. [Internet]. 2011[cited 2016 Jun 07]. Available from: http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf
» http://apps.who.int/iris/bitstream/10665/80135/1/9789241501507_eng.pdf -
2Agência Nacional de Vigilância Sanitária. Medidas de prevenção de infecção relacionada à assistência à saúde. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2013:1-87.
-
3National Healthcare Safety Network. NHSN Central Line-associated Bloodstream Infection Surveillance in 2014. National Center for Emerging and Zoonotic Infectious Diseases. [Internet]. 2014 Mar [cited 2016 Feb 02]. Available from: http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf
» http://www.cdc.gov/nhsn/PDFs/training/training-CLABSI-2014-with-answers-BW.pdf -
4National Healthcare Safety Network. Patient Safety Component Manual [Internet]. 2017 Jan [cited 2017 Feb 14]. Available from: https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf
» https://www.cdc.gov/nhsn/pdfs/pscmanual/pcsmanual_current.pdf -
5Mok Q. How I diagnose and manage catheter-associated blood stream infections. J Paediatr Child Health [Internet]. 2015 May [cited 2016 Jun 07]; 25(5):243-4. Available from: http://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(14)00223-6/pdf
» http://www.paediatricsandchildhealthjournal.co.uk/article/S1751-7222(14)00223-6/pdf -
6Martínez-Morel HR, Sánchez-Payá J, Molina-Gómez MJ, García-Shimizu P, García RV, Villanueva-Ruiz C, et al. Catheter-related bloodstream infection: burden of disease in a tertiary hospital. J Hosp Infect [Internet]. 2014 Jul [cited 2016 Feb 02]; 87(3):165-70. Available from: http://www.sciencedirect.com/science/article/pii/S0195670114001285
» http://www.sciencedirect.com/science/article/pii/S0195670114001285 -
7Center for Disease Control and Prevetion. Guideline for the Prevention of Intravascular Catheter-Related Infections, 2011. Atlanta [Internet]. 2011 [cited 2016 Jun 07]. Available from: http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf
» http://www.cdc.gov/hicpac/pdf/guidelines/bsi-guidelines-2011.pdf -
8Agência Nacional de Vigilância Sanitária. Avaliação dos indicadores nacionais de infecção relacionada à assistência ano de 2014 e relatório de progresso. Brasília (DF): Agência Nacional de Vigilância Sanitária, 2015.
-
9Souza ES, Belei RA, Carrilho CMDM, Matsuo T, Yamada-Ogatta SF, Andrade G et al. Mortalidade e riscos associados a infecção relacionada à assistência à saúde. Texto Contexto Enferm [Internet]. 2015 Jan-Mar [cited 2017 Feb 14]; 24(1): 220-8. Available from: http://www.redalyc.org/pdf/714/71438421027.pdf
» http://www.redalyc.org/pdf/714/71438421027.pdf -
10The Joint Commission. Preventing central line-associated bloodstream infections: a global challenge, a global perspective. Oak Brook, IL: Joint Commission Resources. [Internet]. 2012 May [cited 2016 Feb 02]. Available from: https://www.jointcommission.org/assets/1/18/CLABSI_Monograph.pdf
» https://www.jointcommission.org/assets/1/18/CLABSI_Monograph.pdf -
11Institute for Health Improvement. Protecting 5 million lives. Cambridge [Internet]. 2004 [cited 2016 Jun 07]. Available from: http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx
» http://www.ihi.org/engage/initiatives/completed/5MillionLivesCampaign/Pages/default.aspx -
12Salama MF, Jamal W, Mousa HA, RotimI V. Implementation of central venous catheter bundle in an intensive care unit in Kuwait: effect on central line-associated bloodstream infections. J Infect Public Health [Internet]. 2016 Jan-Feb [cited 2016 Jun 07]; 9(1):34-41. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26138518
» http://www.ncbi.nlm.nih.gov/pubmed/26138518 -
13Labeau SO, Vandijck DM, Rello J, Adam S, Rosa A, Wenisch C, et al. Centers for Disease Control and Prevention guidelines for preventing central venous catheter-related infection: results of a knowledge test among 3405 European intensive care nurses. Crit Care Med [Internet]. 2009 Jan [cited 2016 Jun 07]; 37(1):320-3. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19050628
» http://www.ncbi.nlm.nih.gov/pubmed/19050628 -
14Sacks GD, Diggs BS, Hadjizacharia P, Green D, Salim A, Malinoski DJ. Reducing the rate of catheter-associated bloodstream infections in a surgical intensive care unit using the Institute for Healthcare Improvement central line bundle. Am J Surg [Internet]. 2014 Jun [cited 2016 Mar 02]; 207(6):817-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24576582
» http://www.ncbi.nlm.nih.gov/pubmed/24576582 -
15Santos CMC, Pimenta CAM, Nobre MRC. A estratégia PICO para a construção da pergunta de pesquisa e busca de evidências. Rev Latino-Am. Enfermagem [Internet]. 2007 Jun [cited 2016 Aug 01]; 15(3):508-11. Available from: http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext&tlng=pt
» http://www.scielo.br/scielo.php?pid=S0104-11692007000300023&script=sci_arttext&tlng=pt -
16Stetler CB, Morsi D, Rucki S, Broughton S, Corrigan B, Fitzgerald J, et al. Utilization-focused integrative reviews in a nursing service. Appl Nurs Res [Internet]. 1998 Nov [cited 2016 Mar 01]; 11(4):1-11. Available from: http://www.appliednursingresearch.org/article/S0897-1897(98)80329-7/pdf
» http://www.appliednursingresearch.org/article/S0897-1897(98)80329-7/pdf -
17Kim JS, Holtom P, Vigen C. Reduction of catheter-related bloodstream infections through the use of a central venous line bundle: epidemiologic and economic consequences. Am J Infect Control [Internet]. 2011 Oct [cited 2016 Jun 07]; 39(8):640-6. Available from: http://www.sciencedirect.com/science/article/pii/S0196655311000903
» http://www.sciencedirect.com/science/article/pii/S0196655311000903 -
18Longmate AG, Ellis KS, Boyle L, Maher S, Cairns CJS, Lloyd SM, et al. Elimination of central-venous-catheterrelated bloodstream infections from the intensive care unit. BMJ Qual Saf. 2011 May [cited 2016 Apr 10]; 20:174-80. Available from: http://www.iqg.com.br/pbsp/img_up/01305809324.pdf
» http://www.iqg.com.br/pbsp/img_up/01305809324.pdf -
19Burden AR, Torjman MC, Dy GE, Jaffe JD, Littiman JJ, Nawar F, et al. Prevention of central venous catheter-related bloodstream infections: is it time to add simulation training to the prevention bundle? J Clinical Anesthesia [Internet]. 2012 Nov [cited 2016 Apr 10]; 24(7): 555-60. Available from: http://www.sciencedirect.com/science/article/pii/S0952818012002450
» http://www.sciencedirect.com/science/article/pii/S0952818012002450 -
20Cherifi S, Gerard M, Arias S, Byl B. A multicenter quasi-experimental study: impact of a central line infection control program using auditing and performance feedback in five Belgian intensive care units. Antimicrob Resist Infect Control [Internet]. 2013 Dec [cited 2016 Apr 10]; 2(1):33. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4029143/ -
21Exline MC, Ali NA, Zikri N, Mangino JE, Torrence K, Vermillion B, et al. Beyond the bundle journey of a tertiary care medical intensive care unit to zero central line-associated bloodstream infections. Crit Care [Internet]. 2013 Mar [cited 2016 Apr 10]; 17(2):41. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733431/ -
22Hocking C, Pirret AM. Using a combined nursing and medical approach to reduce the incidence of central line associated bacteraemia in a New Zealand critical care unit: a clinical audit. Intensive and Crit Care Nurs [Internet]. 2013 Jun [cited 2016 Apr 10]; 29(3):137-46. Available from: http://www.sciencedirect.com/science/article/pii/S0964339712001279
» http://www.sciencedirect.com/science/article/pii/S0964339712001279 -
23Hammarskjöld F, Berg S, Hanberger H, Taxbro K, Malmvall B. Sustained low incidence of central venous catheter-related infections over six years in a Swedish hospital with an active central venous catheter team. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 10]; 42(2):122-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24485369
» http://www.ncbi.nlm.nih.gov/pubmed/24485369 -
24Klintworth G, Stafford J, O'Connor M, Jeong T, Hamley L, Watson K, et al. Beyond the intensive care unit bundle: implementation of a successful hospital-wide initiative to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 11]; 42(6):685-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314001710
» http://www.sciencedirect.com/science/article/pii/S0196655314001710 -
25Tang HJ, Lin HL, Lin YH, Leung PO, Chuang YC, Lai CC. The impact of central line insertion bundle on central line associated bloodstream infection. BMC Infect Dis [Internet]. 2014 Jul [cited 2016 Apr 11]; 14(1):1-6. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085375/ -
26Mazi W, Begum Z, Abdulla D, Hesham A, Maghari S, Assiri A, et al. Central line-associated bloodstream infection in a trauma intensive care unit: impact of implementation of Society for Healthcare Epidemiology of America/Infectious Diseases Society of America practice guidelines. Am J Infect Control [Internet]. 2014 Aug [cited 2016 Apr 12]; 42(8):865-7. Available from: http://www.sciencedirect.com/science/article/pii/S0196655314007974
» http://www.sciencedirect.com/science/article/pii/S0196655314007974 -
27Allen GB, Miller V, Nicholas C, Hess S, Cordes MK, Fortune JB, et al. A multitiered strategy of simulation training, kit consolidation, and electronic documentation is associated with a reduction in central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Jun [cited 2016 Apr 12]; 42(6):643-4. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24837115
» http://www.ncbi.nlm.nih.gov/pubmed/24837115 -
28Thom KA, Li S, Custer M, Preas MA, Rew CD, Cafeo C, et al. Successful implementation of a unit-based quality nurse to reduce central line-associated bloodstream infections. Am J Infect Control [Internet]. 2014 Feb [cited 2016 Apr 12]; 42(2):139-43. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313012029
» http://www.sciencedirect.com/science/article/pii/S0196655313012029 -
29Menegueti MG, Ardison KMM, Bellissimo-Rodrigues F, Gaspar GG, Martins-Filho AO, et al. The impact of implementation of bundle to reduce catheter-related bloodstream infection rates. J Clin Med Res [Internet]. 2015 Nov [cited 2016 Apr 12]; 7(11):857-61. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4596267/ -
30Entesari-Tatafi D, Bailey NOMJ, Chonghaile MNI, Lamb-Jenkins J, Athan E. Effectiveness of a care bundle to reduce central line-associated bloodstream infections. Med J Aust [Internet]. 2015 Mar [cited 2016 Apr 12]; 202 (5):247-9. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25758694
» http://www.ncbi.nlm.nih.gov/pubmed/25758694 -
31Polderman KH, Girbes AJ. Central venous catheter use. Part 1: mechanical complications. Intensive Care Med [Internet]. 2002 Jan [cited 2016 May 07]; 28(1):1-17. Available from: http://www.ncbi.nlm.nih.gov/pubmed/11818994
» http://www.ncbi.nlm.nih.gov/pubmed/11818994 -
32Merrer J, Jonghe B, Golliot F, Lefrant JY, Raffy B, Barre E, et al. Complications of femoral and subclavian venous catheterization in critically III patients a randomized controlled trial. JAMA [Internet]. 2001 Aug [cited 2016 May 07]; 286(6):700-7. Available from: http://jama.jamanetwork.com/article.aspx?articleid=194073
» http://jama.jamanetwork.com/article.aspx?articleid=194073 -
33Parienti JJ, Mongardon N, Mégarbane B, Mira JP, Kalfon P, Gros A, et al. Intravascular complications of central venous catheterization by insertion site. N Engl J Med [Internet]. 2015 Sep [cited 2016 May 07]; 373:1220-9. Available from: http://www.nejm.org/doi/full/10.1056/NEJMoa1500964#t=article
» http://www.nejm.org/doi/full/10.1056/NEJMoa1500964#t=article -
34Burdeu G, Currey J, Pilcher D. Idle central venous catheter-days pose infection risk for patients after discharge from intensive care. Am J Infect Control [Internet]. 2014 Apr [cited 2016 Jun 07]; 42(4):453-55. Available from: http://www.sciencedirect.com/science/article/pii/S0196655313013692
» http://www.sciencedirect.com/science/article/pii/S0196655313013692 -
35Tejedor SC, Tong D, Stein J, Payne C, Dressler D, Xue W et al. Temporary central venous catheter utilization patterns in a large tertiary care center: tracking the "idle central venous catheter". Infect Control Hosp Epidemiol [Internet]. 2012 Jan [cited 2016 May 13]; 33(1):50-7. Available from: http://www.ncbi.nlm.nih.gov/pubmed/22173522
» http://www.ncbi.nlm.nih.gov/pubmed/22173522 -
36Tiwari MM, Hermsen ED, Charlton ME, Anderson JR, Rupp ME. Inappropriate intravascular device use: a prospective study. J Hosp Infect [Internet]. 2011 Jun [cited 2016 Jun 07]; 78(2):128-32. Available from: http://www.sciencedirect.com/science/article/pii/S0195670111001149
» http://www.sciencedirect.com/science/article/pii/S0195670111001149 -
37Weber DJ, Rutala WA. Central line-associated bloodstream infections: prevention and management. Infect Dis Clin North Am [Internet]. 2011 Mar [cited 2016 May 01]; 5(1):77-102. Available from: http://www.ncbi.nlm.nih.gov/pubmed/21315995
» http://www.ncbi.nlm.nih.gov/pubmed/21315995 -
38Chen W, Li S, Li L, Wu X, Zhang W. Effects of daily bathing with chlorhexidine and acquired infection of methicillin-resistant Staphylococcus aureus and vancomycin-resistant Enterococcus: a meta-analysis. J Thorac Dis. 2013 Aug [cited 2016 Jun 15]; 5(4):518-24. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755671/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3755671/ -
39Bleasdale SC, Trick WE, Gonzalez IM, Lyles RD, Hayden MK, Weinstein RA. Effectiveness of chlorhexidine bathing to reduce catheter-associated bloodstream infections in medical intensive care unit patients. Arch Intern Med [Internet]. 2007 Oct [cited 2016 Jun 15]; 167(19):2073-9. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=413356
» http://archinte.jamanetwork.com/article.aspx?articleid=413356 -
40Munoz-Price LS, Hota B, Stemer A, Weinstein RA. Prevention of bloodstream infections by use of daily chlorhexidine baths for patients at a long-term acute care hospital. Infect Control Hosp Epidemiol [Internet]. 2009 Nov [cited 2016 Jun 15]; 30(11):1031-5. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19751155
» http://www.ncbi.nlm.nih.gov/pubmed/19751155 -
41Climo MW, Sepkowitz KA, Zuccotti G, Fraser VJ, Warren DK, Perl TM, et al. The effect of daily bathing with chlorhexidine on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus, and healthcare-associated bloodstream infections: results of a quasi-experimental multicenter trial. Crit Care Med [Internet]. 2009 Jun [cited 2016 Jun 15]; 37(6):1858-65. Available from: http://www.ncbi.nlm.nih.gov/pubmed/19384220
» http://www.ncbi.nlm.nih.gov/pubmed/19384220 -
42Chesshyre E, Goff Z, Bowen A, Carapetis J. The prevention, diagnosis and management of central venous line infections in children. J infect [Internet]. 2015 Jun [cited 2016 Jul 07]; 71(1):59-75. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25934326
» http://www.ncbi.nlm.nih.gov/pubmed/25934326 -
43Cherry RA, West CE, Hamilton MC, Rafferty CM, Hollenbeak CS, Caputo GM. Reduction of central venous catheter associated blood stream infections following implementation of a resident oversight and credentialing policy. Patient Saf Surg [Internet]. 2011 Jun [cited 2016 Jun 07]; 5:2-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123176/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3123176/ -
44Zack J. Zeroing in on zero tolerance for central line-associated bacteremia. Am J Infect Control [Internet]. 2008 Dec [cited 2016 Jul 07]; 36(10):176. Available from: http://www.sciencedirect.com/science/article/pii/S0196655308007992
» http://www.sciencedirect.com/science/article/pii/S0196655308007992 -
45Esposito S, Purrello SM, Bonnet E, Noveli A, Tripodi F, Pascale R. et al. Central venous catheter-related biofilm infections: an up-to-date focus on meticillin-resistant Staphylococcus aureus. J Glob Antimicrob Resist [Internet]. 2013 Apr [cited 2016 Jul 07]; 1(1):71-8. Available from: https://www.researchgate.net/publication/236889298
» https://www.researchgate.net/publication/236889298 -
46Matsui Y, Shimatani M, Kuzuhara K, Miyazaki Y, Horiuchi T, Tajima Y, et al. Three-year prospective, observational study of central line-associated bloodstream infections in a 600-bed Japanese acute care hospital. Am J Infect Control [Internet]. 2015 Feb [cited 2016 Jul 07]; 43(5):294-8. Available from: http://www.ncbi.nlm.nih.gov/pubmed/25737305
» http://www.ncbi.nlm.nih.gov/pubmed/25737305 -
47Garcia R. Surgical skin antisepsis. Perioperative Nursing Clinics [Internet]. 2011 Dec [cited 2016 Jul 07]; 5(4):457-77. Available from: http://www.periopnursing.theclinics.com/article/S1556-7931(10)00064-1/pdf
» http://www.periopnursing.theclinics.com/article/S1556-7931(10)00064-1/pdf -
48World Health Organization. Evidence for Hand Hygiene Guidelines. [Internet]. 2016 [cited 2016 Jul 07]. Available from: http://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/
» http://www.who.int/gpsc/tools/faqs/evidence_hand_hygiene/en/ -
49Garret Jr JH. Summary of evidence-based practices for bloodstream infection prevention across the health care continuum of care for vascular access clinicians: addressing the 3 common sources of health care-associated infection transmission. J Vasc Access [Internet]. 2016 Jun [cited 2016 Jul 07]; 21(2):72-4. Available from: http://www.sciencedirect.com/science/article/pii/S1552885516300265
» http://www.sciencedirect.com/science/article/pii/S1552885516300265 -
50Ozakin E, Can R, Acar N, Balogu Kaya F, Cevik AA. An evaluation of complications in ultrasound-guided central venous catheter insertion in the emergency department. Turk J Emerg Med [Internet]. 2014 Feb [cited 2016 Jul 10]; 14(2):53-8. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909866/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4909866/ -
51Bayci AWL, Mangla J, Jenkins CS, Ivascu FA, Robbins JM. Novel educational module for subclavian central venous catheter insertion using real-time ultrasound guidance. J Surg Educ [Internet]. 2015 Nov-Dec [cited 2016 Jul 10]; 72(6):1217-23. Available from: http://www.ncbi.nlm.nih.gov/pubmed/26481424
» http://www.ncbi.nlm.nih.gov/pubmed/26481424 -
52Loveday HP, Wilson JA, Pratt RJ, Golsorkhi M, Tingle A, Bak A, et al. Epic3: national evidence-based guidelines for preventing healthcare-associated infections in NHS hospitals in England. J Hosp Infect [Internet]. 2014 Jan [cited 2016 Jul 10]; 86(1):1-70. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24330862
» http://www.ncbi.nlm.nih.gov/pubmed/24330862 -
53Association for professionals in infection control and epidemiology. Guide to the elimination of catheter-related bloodstream infections. Washington [Internet]. 2009 [cited 2016 Jul 10]. Available from: http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf
» http://www.apic.org/Resource_/EliminationGuideForm/259c0594-17b0-459d-b395-fb143321414a/File/APIC-CRBSI-Elimination-Guide.pdf -
54Sannoh S, Clones B, Munoz J, Montecalvo M, Parvez B. A multimodal approach to central venous catheter hub care can decrease catheter-related bloodstream infection. Am J Infect Control [Internet]. 2010 Aug [cited 2016 Jul 20]; 36(8):424-29. Available from: http://www.sciencedirect.com/science/article/pii/S0196655309009493
» http://www.sciencedirect.com/science/article/pii/S0196655309009493 -
55Frasca D, Dahyot-Fizelier C, Mimoz O. Prevention of central venous catheter-related infection in the intensive care unit. Crit Care [Internet]. 2010 Mar [cited 2016 Jul 20]; 14:212. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2887105/
» http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2887105/ -
56Marschall J, Mermel LA, Fakih M, Hadaway L, Kallen A, O'Grady NP, et al. Strategies to prevent central line-associated bloodstream infections in acute care hospitals: 2014 update. Infect Control Hosp Epidemiol [Internet]. 2014 Jul [cited 2016 Jul 20]; 35(7):753-71. Available from: http://www.ncbi.nlm.nih.gov/pubmed/24915204
» http://www.ncbi.nlm.nih.gov/pubmed/24915204 -
57Oliveira FJG, Caetano JA, Silva VM, Almeida PC, Rodrigues AB, Siqueira JF. O uso de indicadores clínicos na avaliação das práticas de prevenção e controle de infecção de corrente sanguínea. Texto Contexto Enferm [Internet]. 2015 Out-Dez [cited 2016 Set 14]; 24(4):1018-26. Available from: http://www.scielo.br/pdf/tce/v24n4/pt_0104-0707-tce-24-04-01018.pdf
» http://www.scielo.br/pdf/tce/v24n4/pt_0104-0707-tce-24-04-01018.pdf -
58Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections a meta-analysis of costs and financial impact on the us health care system. JAMA Intern Med [Internet]. 2013 Dec [cited 2016 Jul 20]; 173(22):2039-46. Available from: http://archinte.jamanetwork.com/article.aspx?articleid=1733452
» http://archinte.jamanetwork.com/article.aspx?articleid=1733452
Datas de Publicação
-
Publicação nesta coleção
2018
Histórico
-
Recebido
23 Set 2016 -
Aceito
20 Mar 2017