ABSTRACT
Objective:
to analyze the scientific production on the use of Personal Protective Equipment by Nursing professionals during the care provided in the hospital environment.
Method:
this is a scoping review, based on the 2020 Joanna Briggs Institute Manual and guided by PRISMA-PCR. PUBMED, EMBASE, CINAHL, LILACS, BDENF, SCOPUS and WEB of SCIENCE were used as databases, choosing a search period corresponding to the last 20 years. Data collection took place from September to October 2021. The study protocol is available in the Open Science Framework: https://osf.io/7d8q9/files/. Studies on the use of Personal Protective Equipment in direct care provided by the Nursing team in hospitals were included; and those that addressed reviews, theses and dissertations in other settings were excluded, as well as studies not available in full.
Results:
the sample consisted of 26 documents. The items most cited and with the highest adherence in the studies were procedure gloves, while use of goggles was the least mentioned. The following stand out among the factors that facilitate PPE use by nurses: interpersonal relationships, knowledge, workload, standardization of guidelines, and participation of the care team in management decisions.
Conclusion:
the need to educate the professionals using behavioral knowledge as a strategy, as well as maintenance of communication in the sectors to avoid contamination, the influence of workload and the standardization of guidelines are necessary in the hospital health services to increase health professionals' engagement towards the biosafety practices.
DESCRIPTORS:
Personal protective equipment; Professional practice; Health personnel; Nursing; Precaution; Occupational risks; Occupational health
RESUMEN
Objetivo:
analizar la producción científica sobre el uso del Equipo de Protección Personal en profesionales de Enfermería durante la atención provista en el ámbito hospitalario.
Método:
revisión de alcance basada en el Manual del Joanna Briggs Institute de 2020 y guiada por PRISMA-PCR. Se utilizaron las bases de datos PUBMED, EMBASE, CINAHL, LILACS, BDENF, SCOPUS y WEB of SCIENCE, eligiéndose los últimos 20 años como período de búsqueda. Los dados fueron recolectados de septiembre a octubre de 2021. El protocolo del estudio se encuentra disponible en Open Science Framework: https://osf.io/7d8q9/files/. Se incluyeron estudios sobre el uso del Equipo de Protección Personal en la atención directa provista por el equipo de Enfermería en hospitales y se excluyó a los que tenían como tema revisiones, tesis y disertaciones en otros ámbitos, al igual que estudios no disponibles en formato de texto completo.
Resultados:
la muestra estuvo compuesta por 26 documentos. Los elementos de protección más citados y con mayor adhesión en los estudios fueron los guantes de procedimiento, mientras que las gafas protectoras fueron las menos mencionadas. Entre los factores que facilitan el uso del PPE en los profesionales de Enfermería se destacan las relaciones interpersonales, el conocimiento, la carga de trabajo, la estandarización de las pautas y la participación del equipo asistencial en las decisiones gerenciales.
Conclusión:
la necesidad de educar a los profesionales empleando como estrategia el conocimiento conductual, mantener la comunicación entre los sectores para para evitar la contaminación, la influencia de la carga de trabajo, y la estandarización de las pautas son medidas necesarias en los servicios de salud hospitalaria para mejorar el nivel de compromiso de los profesionales de la salud con las prácticas de bioseguridad.
DESCRIPTORES:
Equipo de protección personal; Práctica profesional; Personal de salud; Enfermería; Precaución; Riesgos ocupacionales; Salud laboral
RESUMO
Objetivo:
analisar a produção científica sobre o uso de equipamento de proteção individual pelos profissionais da enfermagem durante a assistência no âmbito hospitalar.
Método:
trata-se de uma revisão de escopo, baseada no Manual Institute Joanna Briggs de 2020 e norteado pelo PRISMA-PCR. Utilizou-se como base de dados PUBMED, EMBASE, CINAHL, LILACS, BDENF, SCOPUS e WEB of SCIENCE, sendo o período de busca escolhido nos últimos 20 anos. A coleta de dados ocorreu de setembro a outubro de 2021. Protocolo de estudo disponível em Framework: https://osf.io/7d8q9/files/. Foram incluídos estudos sobre o uso dos Equipamentos de Proteção Individual na assistência direta da equipe de enfermagem nos hospitais e excluídos aqueles que abordassem em outros cenários, revisões, teses, dissertações e estudos não disponíveis na íntegra.
Resultados:
a amostra foi composta por 26 documentos. O equipamento mais citado e com maior adesão nos estudos foram as luvas de procedimento, enquanto que o uso dos óculos foi o menor. Dos fatores que facilitam o uso dos EPIs pelos enfermeiros destacam-se as relações interpessoais, conhecimento, carga de trabalho, padronização das diretrizes e participação da equipe assistencial nas decisões gerenciais.
Conclusão:
a necessidade de educação dos profissionais utilizando como estratégia o conhecimento comportamental, a manutenção da comunicação nos setores para evitar a contaminação, a influência da carga de trabalho, a padronização das diretrizes são necessárias nos serviços de saúde hospitalar para aumentar o engajamento dos profissionais de saúde às práticas de biossegurança.
DESCRITORES:
Equipamentos de proteção individual; Prática profissional; Pessoal de saúde; Enfermagem; Precaução; Riscos ocupacionais; Saúde do trabalhador
INTRODUCTION
Occupational Health is a field that seeks to integrate knowledge between work relationships and the health and disease process.11. Fernandes MA, Castro SFF, Furtado NI, Araújo EC, Lemos GP, Oliveira ALCB. Utilização de equipamentos de proteção individual: interfaces com o conhecimento dos profissionais de saúde. Rev Prev Infec Saúde [Internet]. 2017 [cited 2021 Oct 28];3(1):16-21. Available from: https://revistas.ufpi.br/index.php/nupcis/article/view/6209
https://revistas.ufpi.br/index.php/nupci...
Associated with this area, biosafety is understood as a set of measures to prevent or eliminate the risks that may compromise human, environmental or animal health.² It was disseminated internationally in the 1970s with publications by the Center for Disease Control and Prevention (CDC) on the precaution categories.33. Ministério da Saúde (BR). Norma Regulamentadora (NR-6) [Internet]. 2022 [cited 2022 Apr 07]. Available from: https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-6-nr-6
https://www.gov.br/trabalho-e-previdenci...
In Brazil, biosafety was regulated in the 90s, with Regulatory Norm (Norma Regulamentadora, NR) 32 standing out for this study, which provides for the use of Personal Protective Equipment (PPE) for health professionals.44. Ministério do Trabalho e Emprego (BR). NR 32 - Segurança e Saúde no Trabalho em Serviços de Saúde [Internet]. 2020 [cited 2022 Mar 31]. Available from: https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-32-nr-32
https://www.gov.br/trabalho-e-previdenci...
Concern about biological risks arose from the verification of health problems in health professionals while handling microorganisms and in direct patient care, such as in outbreaks, epidemics and pandemics. The Acquired Immunodeficiency Syndrome (AIDS) epidemic in the 1980s stands out in the literature,55. Souza RT, Bica CG, Mondadori CS, Ranzi AD. Evaluation of occupational accidents with biological materials in medical residents, academics and interns of school hospital of Porto Alegre. Rev Bras Educ Med [Internet]. 2012 [cited 2021 Oct 06];36(1):118-24. Available from: https://doi.org/10.1590/S0100-55022012000100016
https://doi.org/10.1590/S0100-5502201200...
as well as tuberculosis,66. Pustiglione M, Galesi VMN, Santos LAR, Bombarda S, Tognini S, Freitas AC, et al. Tuberculosis in health care workers: a problem to be faced. Rev Med [Internet]. 2020 [cited 2021 Oct 07];99(1):16-26. Available from: https://doi.org/10.11606/issn.1679-9836.v99i1p16-26
https://doi.org/10.11606/issn.1679-9836....
MERS-CoV, Ebola, SARS-CoV and bird flu,77. Suwantarat N, Apisarnthanarak A. Risks to healthcare workers with emerging diseases: lessons from MERS-CoV, Ebola, SARS, and avian flu. Curr Opin Infect Dis [Internet]. 2015 [cited 2021 Oct 07];28(4):349-61. Available from: https://doi.org/10.1097/QCO.0000000000000183
https://doi.org/10.1097/QCO.000000000000...
COVID-1988. Nafisah SAB, Mzahim BY, Aleid BS, Sheerah SA, Almatrafi DQ, Ciottone GR, et al. The risk of coronavirus to healthcare providers during aerosol-generating procedures: A systematic review and meta-analysis. Ann Thorac Med [Internet]. 2021 [cited 2021 Oct 07];16(2):165-71. Available from: https://doi.org/10.4103/atm.ATM_497_20
https://doi.org/10.4103/atm.ATM_497_20...
and exposure to chemical risks,99. Yu E. Occupational exposure in health care personnel to antineoplastic drugs and initiation of safe handling in Hong Kong: a literature review. J Infus Nurs [Internet]. 2020 [cited 2021 Oct 06];43(3):121-33. Available from: https://doi.org/10.1097/NAN.0000000000000361
https://doi.org/10.1097/NAN.000000000000...
such as administration of antineoplastics.
When contaminated during their work practice, health professionals suffer negative impacts on their physical and psychological health, safety and morals, as well as on patients' trust. Thus, it is understood that there is a need to adequately protect these professionals from contagious-infectious diseases1010. Liu M, Cheng SZ, Xu KW, Yang Y, Zhu QT, Zhang H, et al. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in Wuhan, China: cross sectional study. BMJ [Internet]. 2020 [cited 2021 Oct 07];369:m2195. Available from: https://doi.org/10.1136/bmj.m2195
https://doi.org/10.1136/bmj.m2195...
and in handling cytotoxic agents that are harmful to their health.1111. Costa AG, Costa MS, Ferreira ES, Sousa PC, Santos MM, Lima DE, et al. Knowledge of Nursing Professional on the Safety of the Oncological Patient in Chemoterapy. Rev Bras Cancerol [Internet]. 2019 [cited 2021 Oct 07];65(1):e-04274. Available from: https://doi.org/10.32635/2176-9745.RBC.2019v65n1.274
https://doi.org/10.32635/2176-9745.RBC.2...
As a biosafety strategy, PPE use allows mitigating occupational risks and possible acidentes.1212. Bastos APS, Brito MAR, Ferreira JLR, Ferreira JGOR, Araujo VSC, Val HMC, et al. Equipamentos de proteção individual e a adesão do conhecimento dos profissionais e acadêmicos: revisão integrativa. Rev Eletro Acer Saúde [Internet]. 2020 [cited 2021 Sep 30];27(53):e3764. Available from: https://doi.org/10.25248/reas.e3764.2020
https://doi.org/10.25248/reas.e3764.2020...
-1313. Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet [Internet]. 2020 [cited 2021 Sep 11];395(10223):514-23. Available from: https://doi.org/10.1016/S0140-6736(20)30154-9
https://doi.org/10.1016/S0140-6736(20)30...
Nursing stands out among the teams working in health services, consisting of nurses, technicians and assistants who provide direct care to all patients. Therefore, in their work practice, these professionals are routinely more exposed and vulnerable to diseases while handling patients' secretions/excretions and contaminated surfaces,1414. Araújo TM, Caetano JÁ, Barros LM, Lima AC, da Costa RM, Monteiro VA. Acidentes de trabalho com exposição a material biológico entre os profissionais de Enfermagem. Rev Enferm Refer [Internet]. 2012 [cited 2021 Oct 29];3(7):7-14. Available from: https://www.redalyc.org/articulo.oa?id=388239966004
https://www.redalyc.org/articulo.oa?id=3...
in addition to preparation and handling of potentially toxic medications.
In the literature there are studies that address biosafety prevention measures,1515. Silva OM, Cabral DB, Marin SM, Bitencourt JVO, Vargas MAO, Meschial WC. Biosafety measures to prevent COVID-19 in healthcare professionals: an integrative review. Rev Bras Enferm [Internet]. 2022 [cited 2021 Sep 30];75(1):e20201191. Available from: https://doi.org/10.1590/0034-7167-2020-1191
https://doi.org/10.1590/0034-7167-2020-1...
as well as PPE use during the care provided by health professionals.1616. Hrdinová N, Saibertová S, Pokorná A. The use of personal protective equipment in a biosafety level 2 prospective observational study. Crit Care Nurs Q [Internet]. 2021 [cited 2021 Sep 30];44(4):403-12. Available from: https://doi.org/10.1097/CNQ.0000000000000377
https://doi.org/10.1097/CNQ.000000000000...
-1818. Garcia GPA, Fracarolli IFL, Santos HEC, Souza VRS, Cenzi CM, Marziale MHP. Use of personal protective equipment to care for patients with COVID-19: scoping review. Rev Gaucha Enferm [Internet]. 2021 [cited 2021 Sep 30];42(spe):e20200150. Available from: https://doi.org/10.1590/1983-1447.2021.20200150
https://doi.org/10.1590/1983-1447.2021.2...
Currently, a large part of the literature addresses the COVID-19 context and much has been seen in the media about shortage of materials for the professionals during this pandemic, including Brazil.
In addition to the socioeconomic context, it is understood from the professional practice that other factors can influence PPE use or non-use, such as perception of risk and vulnerability to exposure at work. In this sense, it becomes necessary to seek diverse evidence to corroborate (or not) this knowledge of the practice about which factors can influence PPE use.
Thus, the following guiding question is formulated for the study: which is the scientific knowledge available in the literature on PPE use by the Nursing team during direct care in the hospital environment? To answer this question, the objective was to analyze the scientific production on PPE use by the Nursing team during the care provided in the hospital environment.
METHOD
This is a scoping review, which allows mapping the key concepts that support a given research area, main sources and types of evidence available.1919. Mays N, Roberts E, Popay J. Synthesising research evidence. In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the organisation and delivery of health services: research methods. London: Routledge; 2001. p. 188-20. [cited 2021 Sep 30]. Available form: Available form: https://researchonline.lshtm.ac.uk/id/eprint/15408
https://researchonline.lshtm.ac.uk/id/ep...
In this case, regarding PPE use during the care provided by the Nursing team in the hospital environment.
For this purpose, the methodological recommendations set forth in the Joanna Briggs Institute (JBI) Reviewer’s Manual on scoping reviews2020. Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: Scoping Reviews. In: Aromataris E, Munn Z, editors. JBI Manual for evidence synthesis. 2020. p. 408-46 [cited 2021 Aug 15]. Available from: https://doi.org/10.46658/JBIMES-20-01
https://doi.org/10.46658/JBIMES-20-01...
and the items from the Preferred Reporting Items for Systematic reviews and Meta-Analyses extension for Scoping Reviews-PRISMA-ScR flowchart2121. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med [Internet]. 2018 [cited 2021 Oct 30];169(7):467-73. Available from: https://doi.org/10.7326/M18-0850
https://doi.org/10.7326/M18-0850...
were used. A protocol was developed for this research and published in the Open Science Framework system available at the following address: https://osf.io/7d8q9/files/.
To establish the search strategy, the PCC acronym was used, where P (target population) - Nursing professionals, C (concept) - Use of Personal Protective Equipment, and C (context) - Direct care provided in hospitals.
Definition of the descriptors and databases was carried out together with a librarian who also validated the research protocol. To define the descriptors, the Health Sciences Descriptors (Descritores em Ciências da Saúde, DeCS) page of the Virtual Health Library (Biblioteca Virtual em Saúde, BVS) were consulted in Portuguese and Spanish, as well as the Medical Subject Headings (MeSH) in English, with the following choices: "Equipamento de Proteção Individual", "Equipo de Protección Personal", "Personal Protective Equipment"[Mesh], "Prática Profissional", "Práctica Profesional" "Professional Practice"[Mesh], "Pessoal de Saúde" "Health Personnel"[Mesh].
When the Enfermagem, Enfermeria and Nursing descriptors were used, the number of studies was considerably reduced. Thus, it was preferred to define the search strategy with “Health Personnel”. The databases used for the search were the following: National Library of Medicine (PUBMED), EMBASE, Cumulative Index to Nursing and Allied Health Literature (CINAHL), SCOPUS, Web of Science (WoS), Latin American and Caribbean Literature in Health Sciences (Literatura Latino-Americana e do Caribe em Ciências da Saúde, LILACS), as well as the National Nursing Database (Base de Dados Nacionais da Enfermagem, BDENF) and the Scientific Electronic Library Online (SciELO). The search strategy used for each database is available in supplement 1.
In all the databases, filters for language, type of material and period of time were used, considering the inclusion criteria. These were as follows: studies that addressed Nursing team professionals (nurses, and nursing technicians and assistants) working in direct patient care in hospitals, outpatient clinics, wards, surgical centers, intensive and emergency care units, and that used PPE items during the assistance provided. As for the outcome, PPE items and barrier/restraint devices (coat/apron and foot protector) were considered22. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária. Resolução RDC nº 302, de 13 de outubro de 2005. Dispõe sobre Regulamento Técnico para funcionamento de Laboratórios Clínicos [Internet]. 2005 [cited 2022 Apr 07]. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/anvisa/2005/anexo/anexo_res0302_13_10_2005.pdf
http://bvsms.saude.gov.br/bvs/saudelegis...
-44. Ministério do Trabalho e Emprego (BR). NR 32 - Segurança e Saúde no Trabalho em Serviços de Saúde [Internet]. 2020 [cited 2022 Mar 31]. Available from: https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-32-nr-32
https://www.gov.br/trabalho-e-previdenci...
regarding standard precautions and against contact, droplets and aerosols, in outbreaks, epidemics and pandemics; in the face of contagious-infectious and work-related diseases, exposure to radiation in operating rooms; as well as in administration of medications (antineoplastics, antibiotics, antivirals) and in the prevention of Healthcare-Associated Infections.
As for the research period, the intention was to map the knowledge in the literature of the last 20 years, justified by the political aspects about the occupational safety culture in Brazil and in the world. Thus, the period defined was from September 30th, 2001, to September 30th, 2021, in Portuguese, English and Spanish.
The exclusion criteria considered were as follows: studies that were presented in the form of books, literature reviews, abstracts, congress materials, editorials and duplicates, as well as those that were not available in full or online. In addition, there was exclusion of studies that addressed basic health units, home context, pre-care, private practice or other health institutions such as vaccination clinics and laboratories; aimed at students, residents and visitors, in addition to those that addressed other types of PPE items such as helmets and hearing protective devices.
As for the study sources, primary studies were considered in general, in order to understand PPE use in the global and national spectrum; a search was also carried out in the gray literature through the frameworks established by regulatory bodies such as the World Health Organization (WHO), the Center for Disease Control and Prevention (CDC) and the Ministry of Health (Ministério da Saúde, MS) used in the articles selected for this review. The search was carried out in September 2021. Data collection took place from September to October 2021.
Three reviewers were in charge of selecting the studies, with two (RKS and TLS) independently performing the selection and evaluation processes and the third reviewer (NG) being consulted for any and all discrepancies identified in the process. A pre-test was carried out with all three reviewers with the evaluation of ten studies, in full, selected from two databases (five from each one) to ensure consensus of the entire team regarding the eligibility criteria.
Subsequently, we proceeded to select the studies first by titles and abstracts, considering the eligibility criteria already described. The studies selected in this first stage were imported into the EndNote web® software. At a second moment, full reading of the studies was carried out for selection of the final sample. The materials chosen for full reading were organized in an Excel® spreadsheet. To refine the data collection instrument, a pre-analysis was performed with five studies for each reviewer.
The variables chosen for analysis were the following: database, name of the journal, authors, year, title in the original language, country, objective in the original language, type of study described by the original authors; whether it was a single-center or multicenter study, number of participants, profession of the participants, inclusion and exclusion criteria, training time of the participants, whether any type of measuring instrument was used, whether any theoretical-methodological framework was used, type of analysis, types of PPE, context of PPE use indicated by the authors, biological or pharmacological agent, and interventions (if any). Diverse information was also extracted on the conditions that facilitate or hinder PPE use, individual, work and organizational factors and the main results. This process of extracting the results and mapping was carried out in a descriptive way.
To categorize the results, the research results presented by Cunhaet al.2222. Cunha QB, Camponogara S, Freitas EO, Pinno C, Dias GL, Cesar MP. Fatores que interferem na adesão às precauções padrão por profissionais da saúde: revisão integrativa. Enferm Foco [Internet]. 2017 [cited 2021 Oct 24];8(1):72-6. Available from: https://doi.org/10.21675/2357-707X.2017.v8.n1.980
https://doi.org/10.21675/2357-707X.2017....
were used as a basis, which are related to the conditions that facilitate and/or hinder adherence to PPE use, in terms of the individual, work and organizational aspects.
RESULTS
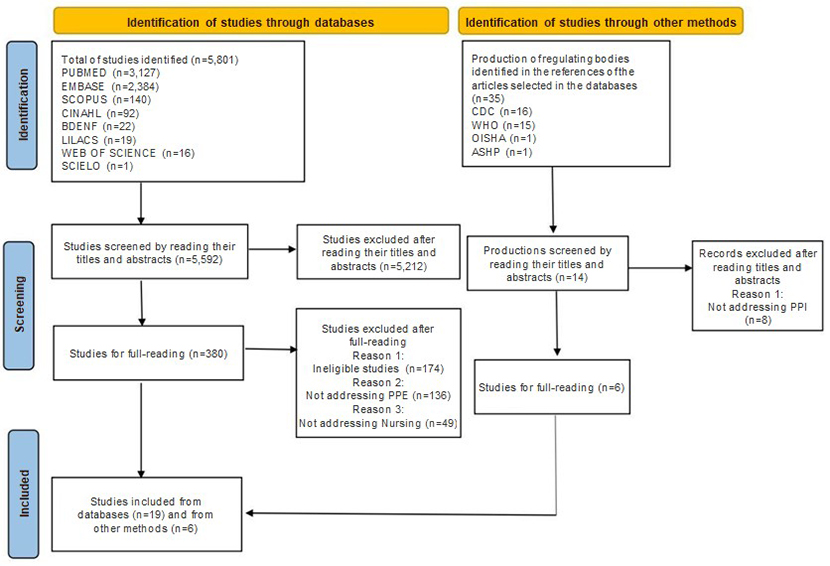
A total of 5,801 publications were identified in the databases and 11 through the frameworks set forth by the regulatory bodies of the studies selected, as shown in Figure 1.
Flowchart of the search and selection processes corresponding to the studies of the current scoping review, adapted from PRISMA-ScR2323. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021 [cited 2021 Oct 17];372:71. Available from: https://doi.org/10.1136/bmj.n71
https://doi.org/10.1136/bmj.n71... . Florianópolis, SC, Brazil, 2021.
Of the 19 articles included in the final sample, ten were identified in PUBMED2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
-3333. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
https://doi.org/10.1188/16.ONF.43-03AP...
, three in LILACS/BDENF,3434. Castro AF, Rodrigues MCS. Auditoria de práticas de precauções-padrão e contato em Unidade de Terapia Intensiva. Rev Esc Enferm USP [Internet]. 2019 [cited 2021 Oct 16];53:e03508. Available from: https://doi.org/10.1590/S1980-220X2018018603508
https://doi.org/10.1590/S1980-220X201801...
-3636. Villarinho MV, Padilha MICS. Risco ao acidente ocupacional no cuidado às pessoas internadas por HIV/AIDS, em Florianópolis-SC, Brasil (1986-2006). Rev Enferm UFSM [Internet]. 2014 [cited 2021 Sep 30];4(4):689-699. Available from: https://doi.org/10.5902/2179769212536
https://doi.org/10.5902/2179769212536...
and two in SCOPUS,3737. Chen HC, Lu ZY, Lee SH. Nurses’ experiences in safe handling of chemotherapeutic agents: the Taiwan case. Cancer Nurs [Internet]. 2016 [cited 2021 Oct 15];39(5):E29-38. Available from: https://doi.org/10.1097/NCC.0000000000000314
https://doi.org/10.1097/NCC.000000000000...
-3838. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
https://doi.org/10.1016/j.jhin.2007.05.0...
EMBASE3939. Anwar MM, Ahmed DM, Elareed HR, Abdel-Latif RA, Sheemy MS, Kamel NM, et al. Screening for latent tuberculosis among healthcare workers in an egyptian hospital using tuberculin skin test and quantiFERON-TB gold in-tube test. Indian J Occup Environ Med [Internet]. 2019 [cited 2021 Sep 30];23(3):106-11. Available from: https://doi.org/10.4103/ijoem.IJOEM_184_19
https://doi.org/10.4103/ijoem.IJOEM_184_...
-4040. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
https://doi.org/10.2147/DHPS.S289025...
and CINAHL4141. Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care [Internet]. 2015 [cited 2021 Oct 16];60(10):1409-17. Available from: https://doi.org/10.4187/respcare.03817
https://doi.org/10.4187/respcare.03817...
-4242. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
https://doi.org/10.1080/15459624.2014.91...
each. Six publications were chosen in the gray literature: three from the CDC,4343. Center for Disease Control and Prevention. The National Institute for Occupational Safety and Health. Hazardous Drug Exposures in Health Care [Internet]. 2016 [cited 2021 Oct 24]. Available from: https://www.cdc.gov/niosh/topics/hazdrug/
https://www.cdc.gov/niosh/topics/hazdrug...
-4545. Center for Disease Control and Prevention. Personal protective equipment for health care workers who work with hazardous drugs [Internet]. Cincinnat (OH): NIOSH ; 2008 [cited 2021 Oct 24]. Available from: https://stacks.cdc.gov/view/cdc/5762
https://stacks.cdc.gov/view/cdc/5762...
two from the WHO4646. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks [Internet]. Genève (CH): WHO; 2009 [cited 2021 Oct 30]. 62 p. Available from: https://apps.who.int/iris/handle/10665/44203
https://apps.who.int/iris/handle/10665/4...
-4747. World Health Organization. Prevention of hospital-acquired infections: a practical guide [Internet]. Genève (CH): WHO ; 2002 [cited 2021 Nov 04]. 64 p. Available from: https://apps.who.int/iris/handle/10665/67350
https://apps.who.int/iris/handle/10665/6...
and one from the American Society of Health-system Pharmacists (ASHP).4848. American Society of Health-System Pharmacists. ASHP Guidelines on handling hazardous drugs. Am J Health Syst Pharm [Internet]. 2006 [cited 2021 Oct 25];63:1172-119. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
https://www.ashp.org/-/media/assets/poli...
The United States of America stands out among the most predominant countries with 10 studies published in the scientific literature4141. Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care [Internet]. 2015 [cited 2021 Oct 16];60(10):1409-17. Available from: https://doi.org/10.4187/respcare.03817
https://doi.org/10.4187/respcare.03817...
-4242. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
https://doi.org/10.1080/15459624.2014.91...
,2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
-2727. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
https://doi.org/10.1111/j.1365-2648.2010...
,3333. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
https://doi.org/10.1188/16.ONF.43-03AP...
and from the gray literature4343. Center for Disease Control and Prevention. The National Institute for Occupational Safety and Health. Hazardous Drug Exposures in Health Care [Internet]. 2016 [cited 2021 Oct 24]. Available from: https://www.cdc.gov/niosh/topics/hazdrug/
https://www.cdc.gov/niosh/topics/hazdrug...
-4646. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks [Internet]. Genève (CH): WHO; 2009 [cited 2021 Oct 30]. 62 p. Available from: https://apps.who.int/iris/handle/10665/44203
https://apps.who.int/iris/handle/10665/4...
,4848. American Society of Health-System Pharmacists. ASHP Guidelines on handling hazardous drugs. Am J Health Syst Pharm [Internet]. 2006 [cited 2021 Oct 25];63:1172-119. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
https://www.ashp.org/-/media/assets/poli...
(Chart 1). As for the years of publication of the studies, they are presented in a diversified way with greater predominance of 2019 (n=4) and 2016 (n=3).
Most of the studies had a quantitative and cross-sectional approach,2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
,2626. Hessels AJ, Weaver SH. Missed opportunities: the development and testing of standard precaution case vignettes. J Infus Nurs [Internet]. 2019 [cited 2021 Oct 16];42(2):70-74. Available from: https://doi.org/10.1097/NAN.0000000000000314
https://doi.org/10.1097/NAN.000000000000...
-3030. Rozenbojm MD, Nichol K, Spielmann S, Holness DL. Hospital unit safety climate: relationship with nurses' adherence to recommended use of facial protective equipment. Am J Infect Control [Internet]. 2015 [cited 2021 Oct 16];43(2):115-20. Available from: https://doi.org/10.1016/j.ajic.2014.10.027
https://doi.org/10.1016/j.ajic.2014.10.0...
,3333. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
https://doi.org/10.1188/16.ONF.43-03AP...
-3535. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
https://doi.org/10.1590/0034-7167-2016-0...
,3838. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
https://doi.org/10.1016/j.jhin.2007.05.0...
-4242. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
https://doi.org/10.1080/15459624.2014.91...
followed by qualitative research studies,2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
,3131. Sissolak D, Marais F, Mehtar S. TB infection prevention and control experiences of South African nurses-a phenomenological study. BMC Public Health [Internet]. 2011 [cited 2021 Oct 18];11:262. Available from: https://doi.org/10.1186/1471-2458-11-262
https://doi.org/10.1186/1471-2458-11-262...
-3232. Suliman M, Aloush S, Aljezawi M, AlBashtawy M. Knowledge and practices of isolation precautions among nurses in Jordan. Am J Infect Control [Internet]. 2018 [cited 2021 Sep 28];46(6):680-84. Available from: https://doi.org/10.1016/j.ajic.2017.09.023
https://doi.org/10.1016/j.ajic.2017.09.0...
,3636. Villarinho MV, Padilha MICS. Risco ao acidente ocupacional no cuidado às pessoas internadas por HIV/AIDS, em Florianópolis-SC, Brasil (1986-2006). Rev Enferm UFSM [Internet]. 2014 [cited 2021 Sep 30];4(4):689-699. Available from: https://doi.org/10.5902/2179769212536
https://doi.org/10.5902/2179769212536...
,3737. Chen HC, Lu ZY, Lee SH. Nurses’ experiences in safe handling of chemotherapeutic agents: the Taiwan case. Cancer Nurs [Internet]. 2016 [cited 2021 Oct 15];39(5):E29-38. Available from: https://doi.org/10.1097/NCC.0000000000000314
https://doi.org/10.1097/NCC.000000000000...
and only one mixed-methods study.2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
Although most of the authors include the definitions of the approaches and/or method, some did not do so.2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
,3838. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
https://doi.org/10.1016/j.jhin.2007.05.0...
Of the studies conducted, 55% (n=11) were multicenter, 35% (n=7) single-center and 10% (n=2) were anonymous online surveys.
In relation to the Nursing team professionals, most of the studies (n=16) addressed only nurses2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
,2626. Hessels AJ, Weaver SH. Missed opportunities: the development and testing of standard precaution case vignettes. J Infus Nurs [Internet]. 2019 [cited 2021 Oct 16];42(2):70-74. Available from: https://doi.org/10.1097/NAN.0000000000000314
https://doi.org/10.1097/NAN.000000000000...
-2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
-3333. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
https://doi.org/10.1188/16.ONF.43-03AP...
,3737. Chen HC, Lu ZY, Lee SH. Nurses’ experiences in safe handling of chemotherapeutic agents: the Taiwan case. Cancer Nurs [Internet]. 2016 [cited 2021 Oct 15];39(5):E29-38. Available from: https://doi.org/10.1097/NCC.0000000000000314
https://doi.org/10.1097/NCC.000000000000...
-4040. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
https://doi.org/10.2147/DHPS.S289025...
and the number of participants varied from 203131. Sissolak D, Marais F, Mehtar S. TB infection prevention and control experiences of South African nurses-a phenomenological study. BMC Public Health [Internet]. 2011 [cited 2021 Oct 18];11:262. Available from: https://doi.org/10.1186/1471-2458-11-262
https://doi.org/10.1186/1471-2458-11-262...
to 1,500.2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
Two studies2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
,3535. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
https://doi.org/10.1590/0034-7167-2016-0...
included the Nursing team (technicians and assistants) as well as other professionals, such as physical therapists, physicians and dentists. The training time of the professionals cited in the studies varied from 1 to 20 years.
Two papers were based on behavioral theories such as the Social Cognitive Theory2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
and the Health Beliefs Model.2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
Others resorted to qualitative approach frameworks (ethnography,3737. Chen HC, Lu ZY, Lee SH. Nurses’ experiences in safe handling of chemotherapeutic agents: the Taiwan case. Cancer Nurs [Internet]. 2016 [cited 2021 Oct 15];39(5):E29-38. Available from: https://doi.org/10.1097/NCC.0000000000000314
https://doi.org/10.1097/NCC.000000000000...
phenomenology3131. Sissolak D, Marais F, Mehtar S. TB infection prevention and control experiences of South African nurses-a phenomenological study. BMC Public Health [Internet]. 2011 [cited 2021 Oct 18];11:262. Available from: https://doi.org/10.1186/1471-2458-11-262
https://doi.org/10.1186/1471-2458-11-262...
and oral history3636. Villarinho MV, Padilha MICS. Risco ao acidente ocupacional no cuidado às pessoas internadas por HIV/AIDS, em Florianópolis-SC, Brasil (1986-2006). Rev Enferm UFSM [Internet]. 2014 [cited 2021 Sep 30];4(4):689-699. Available from: https://doi.org/10.5902/2179769212536
https://doi.org/10.5902/2179769212536...
) for data collection and analyses.
In the evaluation of the questionnaires and/or instruments, in addition to those for the collection of sociodemographic data, the studies used the Standard Precautions Adherence Scale translated and validated in Brazil,3535. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
https://doi.org/10.1590/0034-7167-2016-0...
the Practice Environment Scale and Nursing Work Index,2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
and the Hazardous Drug Handling Questionnaire.3333. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
https://doi.org/10.1188/16.ONF.43-03AP...
Two studies4040. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
https://doi.org/10.2147/DHPS.S289025...
-4141. Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care [Internet]. 2015 [cited 2021 Oct 16];60(10):1409-17. Available from: https://doi.org/10.4187/respcare.03817
https://doi.org/10.4187/respcare.03817...
used different modules of the Health and Safety Practices Survey of Healthcare Workers research study to identify knowledge and practices for safe handling of cytotoxic drugs4040. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
https://doi.org/10.2147/DHPS.S289025...
and knowledge of the dangerous effects of aerosol medications.4141. Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care [Internet]. 2015 [cited 2021 Oct 16];60(10):1409-17. Available from: https://doi.org/10.4187/respcare.03817
https://doi.org/10.4187/respcare.03817...
In addition, other studies resorted to instruments based on previous publications about standard precautions,2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
factors associated with self-protective behavior at work,3030. Rozenbojm MD, Nichol K, Spielmann S, Holness DL. Hospital unit safety climate: relationship with nurses' adherence to recommended use of facial protective equipment. Am J Infect Control [Internet]. 2015 [cited 2021 Oct 16];43(2):115-20. Available from: https://doi.org/10.1016/j.ajic.2014.10.027
https://doi.org/10.1016/j.ajic.2014.10.0...
the 2007 CDC isolation precautions guidelines3232. Suliman M, Aloush S, Aljezawi M, AlBashtawy M. Knowledge and practices of isolation precautions among nurses in Jordan. Am J Infect Control [Internet]. 2018 [cited 2021 Sep 28];46(6):680-84. Available from: https://doi.org/10.1016/j.ajic.2017.09.023
https://doi.org/10.1016/j.ajic.2017.09.0...
and indicators from hospital infection quality assessment manuals.3434. Castro AF, Rodrigues MCS. Auditoria de práticas de precauções-padrão e contato em Unidade de Terapia Intensiva. Rev Esc Enferm USP [Internet]. 2019 [cited 2021 Oct 16];53:e03508. Available from: https://doi.org/10.1590/S1980-220X2018018603508
https://doi.org/10.1590/S1980-220X201801...
As for the types of PPE and barrier devices addressed in the results, they are described in Chart 1. Six studies2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
,3131. Sissolak D, Marais F, Mehtar S. TB infection prevention and control experiences of South African nurses-a phenomenological study. BMC Public Health [Internet]. 2011 [cited 2021 Oct 18];11:262. Available from: https://doi.org/10.1186/1471-2458-11-262
https://doi.org/10.1186/1471-2458-11-262...
-3232. Suliman M, Aloush S, Aljezawi M, AlBashtawy M. Knowledge and practices of isolation precautions among nurses in Jordan. Am J Infect Control [Internet]. 2018 [cited 2021 Sep 28];46(6):680-84. Available from: https://doi.org/10.1016/j.ajic.2017.09.023
https://doi.org/10.1016/j.ajic.2017.09.0...
,3636. Villarinho MV, Padilha MICS. Risco ao acidente ocupacional no cuidado às pessoas internadas por HIV/AIDS, em Florianópolis-SC, Brasil (1986-2006). Rev Enferm UFSM [Internet]. 2014 [cited 2021 Sep 30];4(4):689-699. Available from: https://doi.org/10.5902/2179769212536
https://doi.org/10.5902/2179769212536...
,4343. Center for Disease Control and Prevention. The National Institute for Occupational Safety and Health. Hazardous Drug Exposures in Health Care [Internet]. 2016 [cited 2021 Oct 24]. Available from: https://www.cdc.gov/niosh/topics/hazdrug/
https://www.cdc.gov/niosh/topics/hazdrug...
,4646. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks [Internet]. Genève (CH): WHO; 2009 [cited 2021 Oct 30]. 62 p. Available from: https://apps.who.int/iris/handle/10665/44203
https://apps.who.int/iris/handle/10665/4...
did not specifically address any PPE item, although they contextualize their use in the practice.
Presentation of the reference number, country and type of Personal Protective Equipment addressed. Florianópolis, SC, Brazil, 2021.
In relation to the context, the studies included health and safety in the face of biological and pharmacological agents. As for diseases and/or biological agents, the following were identified: Tuberculosis,2727. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
https://doi.org/10.1111/j.1365-2648.2010...
,3131. Sissolak D, Marais F, Mehtar S. TB infection prevention and control experiences of South African nurses-a phenomenological study. BMC Public Health [Internet]. 2011 [cited 2021 Oct 18];11:262. Available from: https://doi.org/10.1186/1471-2458-11-262
https://doi.org/10.1186/1471-2458-11-262...
,3939. Anwar MM, Ahmed DM, Elareed HR, Abdel-Latif RA, Sheemy MS, Kamel NM, et al. Screening for latent tuberculosis among healthcare workers in an egyptian hospital using tuberculin skin test and quantiFERON-TB gold in-tube test. Indian J Occup Environ Med [Internet]. 2019 [cited 2021 Sep 30];23(3):106-11. Available from: https://doi.org/10.4103/ijoem.IJOEM_184_19
https://doi.org/10.4103/ijoem.IJOEM_184_...
HIV/AIDS,3636. Villarinho MV, Padilha MICS. Risco ao acidente ocupacional no cuidado às pessoas internadas por HIV/AIDS, em Florianópolis-SC, Brasil (1986-2006). Rev Enferm UFSM [Internet]. 2014 [cited 2021 Sep 30];4(4):689-699. Available from: https://doi.org/10.5902/2179769212536
https://doi.org/10.5902/2179769212536...
,3838. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
https://doi.org/10.1016/j.jhin.2007.05.0...
Hepatitis B and Hepatitis C,3838. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
https://doi.org/10.1016/j.jhin.2007.05.0...
Clostridium Difficile, MRSA, Chickenpox, Flu and Meningococcal Meningitis2727. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
https://doi.org/10.1111/j.1365-2648.2010...
and COVID-19.2424. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
https://doi.org/doi:10.1111/inr.12662...
As for the medications, antineoplastics,3333. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
https://doi.org/10.1188/16.ONF.43-03AP...
,3737. Chen HC, Lu ZY, Lee SH. Nurses’ experiences in safe handling of chemotherapeutic agents: the Taiwan case. Cancer Nurs [Internet]. 2016 [cited 2021 Oct 15];39(5):E29-38. Available from: https://doi.org/10.1097/NCC.0000000000000314
https://doi.org/10.1097/NCC.000000000000...
,4040. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
https://doi.org/10.2147/DHPS.S289025...
,4242. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
https://doi.org/10.1080/15459624.2014.91...
,4444. Center for Disease Control and Prevention. Preventing Occupational Exposures to Antineoplastic and other hazardous drugs in health care settings [Internet]. Cincinnat (OH): NIOSH; 2004 [cited 2021 Oct 24]. 50 p. Available from: https://www.cdc.gov/niosh/docs/2004-165/pdfs/2004-165.pdf
https://www.cdc.gov/niosh/docs/2004-165/...
-4545. Center for Disease Control and Prevention. Personal protective equipment for health care workers who work with hazardous drugs [Internet]. Cincinnat (OH): NIOSH ; 2008 [cited 2021 Oct 24]. Available from: https://stacks.cdc.gov/view/cdc/5762
https://stacks.cdc.gov/view/cdc/5762...
,4848. American Society of Health-System Pharmacists. ASHP Guidelines on handling hazardous drugs. Am J Health Syst Pharm [Internet]. 2006 [cited 2021 Oct 25];63:1172-119. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
https://www.ashp.org/-/media/assets/poli...
air sprayers4141. Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care [Internet]. 2015 [cited 2021 Oct 16];60(10):1409-17. Available from: https://doi.org/10.4187/respcare.03817
https://doi.org/10.4187/respcare.03817...
and cytotoxics4343. Center for Disease Control and Prevention. The National Institute for Occupational Safety and Health. Hazardous Drug Exposures in Health Care [Internet]. 2016 [cited 2021 Oct 24]. Available from: https://www.cdc.gov/niosh/topics/hazdrug/
https://www.cdc.gov/niosh/topics/hazdrug...
were studied.
Some studies addressed standard precautions,2626. Hessels AJ, Weaver SH. Missed opportunities: the development and testing of standard precaution case vignettes. J Infus Nurs [Internet]. 2019 [cited 2021 Oct 16];42(2):70-74. Available from: https://doi.org/10.1097/NAN.0000000000000314
https://doi.org/10.1097/NAN.000000000000...
,2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
,3232. Suliman M, Aloush S, Aljezawi M, AlBashtawy M. Knowledge and practices of isolation precautions among nurses in Jordan. Am J Infect Control [Internet]. 2018 [cited 2021 Sep 28];46(6):680-84. Available from: https://doi.org/10.1016/j.ajic.2017.09.023
https://doi.org/10.1016/j.ajic.2017.09.0...
,3434. Castro AF, Rodrigues MCS. Auditoria de práticas de precauções-padrão e contato em Unidade de Terapia Intensiva. Rev Esc Enferm USP [Internet]. 2019 [cited 2021 Oct 16];53:e03508. Available from: https://doi.org/10.1590/S1980-220X2018018603508
https://doi.org/10.1590/S1980-220X201801...
-3535. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
https://doi.org/10.1590/0034-7167-2016-0...
mask use in a general context2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
and face protection for communicable respiratory diseases.2929. Nichol K, McGeer A, Bigelow P, O'Brien-Pallas L, Scott J, Holness DL. Behind the mask: determinants of nurse's adherence to facial protective equipment. Am J Infect Control [Internet]. 2013 [cited 2021 Oct 16];41(1):8-13. Available from: https://doi.org/10.1016/j.ajic.2011.12.018
https://doi.org/10.1016/j.ajic.2011.12.0...
-3030. Rozenbojm MD, Nichol K, Spielmann S, Holness DL. Hospital unit safety climate: relationship with nurses' adherence to recommended use of facial protective equipment. Am J Infect Control [Internet]. 2015 [cited 2021 Oct 16];43(2):115-20. Available from: https://doi.org/10.1016/j.ajic.2014.10.027
https://doi.org/10.1016/j.ajic.2014.10.0...
In relation to frequency, the most used PPE items were gloves with 83.4% (n=501) and the least used were goggles, with 8.8% (n=53). Of the nurses who wore goggles, nearly 50% had already had contact with splashes.3838. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
https://doi.org/10.1016/j.jhin.2007.05.0...
In another study, it was observed that the use of goggles, masks and protective clothing presented less compliance, unlike gloves, due to their availability and accessibility in the sectors.2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
In the intensive care unit, the highest PPE adherence rate by the multiprofessional team in relation to the number of procedures observed corresponded to the use of gloves, followed by aprons, surgical masks and goggles. The authors attributed these results to the fact that a large percentage of the patients hospitalized during the collection period were under contact precautions. They also described that the rate of correct answers regarding PPE use in the procedures was below 50%, justified by the unnecessary use of masks in some procedures and by non-use of goggles in others (such as tracheal aspiration), which would be mandatory.3434. Castro AF, Rodrigues MCS. Auditoria de práticas de precauções-padrão e contato em Unidade de Terapia Intensiva. Rev Esc Enferm USP [Internet]. 2019 [cited 2021 Oct 16];53:e03508. Available from: https://doi.org/10.1590/S1980-220X2018018603508
https://doi.org/10.1590/S1980-220X201801...
In another Brazilian study, conducted with a sample of 54 Nursing team professionals, the authors found that the items on the scale with the highest score (lower adherence to standard precautions) were disposal of sharps in proper containers, use of disposable gloves when there is risk of blood or other secretions, handling of other sharps (scalpel, for example), and that the item with the highest adherence to the precautions was the one that addresses needle recapping to puncture patients' veins. However, it is noted that 25 of the 54 participants stated never recapping needles.3535. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
https://doi.org/10.1590/0034-7167-2016-0...
Regarding protection against exposure to antineoplastics, the most consistent PPE use corresponded to gloves and masks as personal protective measures. The authors indicated that no professional in the study used all the PPE items required for the preparation, administration and disposal stages. Almost 70% of the sample of nurses reported lack of training to handle this type of medication,4040. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
https://doi.org/10.2147/DHPS.S289025...
although the guideline set forth by the American Society of Health-System Pharmacists recommends the use of double gloves or chemotherapy gloves when administering antineoplastics to ensure workers' safety4848. American Society of Health-System Pharmacists. ASHP Guidelines on handling hazardous drugs. Am J Health Syst Pharm [Internet]. 2006 [cited 2021 Oct 25];63:1172-119. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
https://www.ashp.org/-/media/assets/poli...
and, preferably, for all drug handling processes.
In another study4242. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
https://doi.org/10.1080/15459624.2014.91...
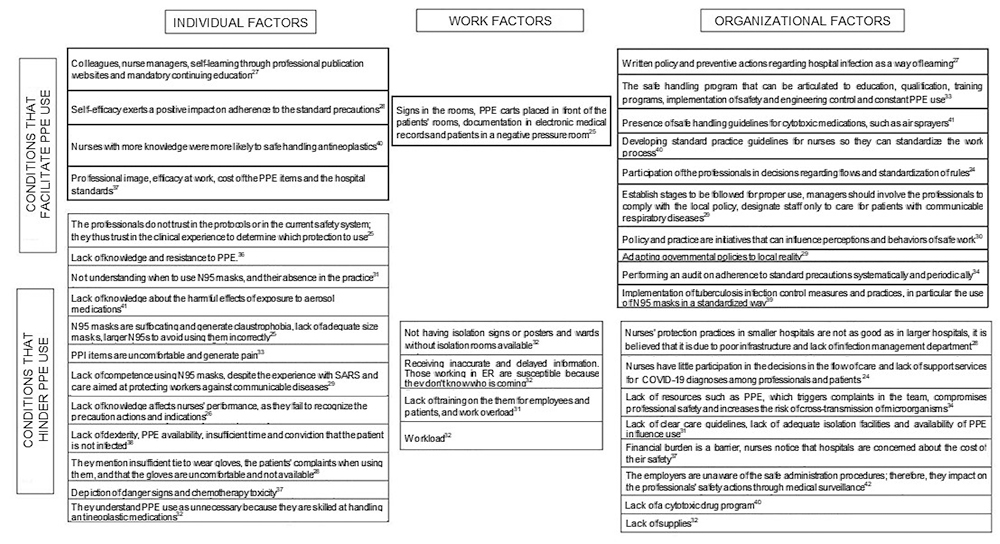
regarding handling of antineoplastics, it was identified that 98% (n=2,069) of the participants always exchanged damaged gloves immediately after contamination, and that 85% (n=1,972) wore gloves during chemotherapy and a non-absorbent apron with a closed front and tight cuffs. In addition, 59% (n=1,762) of the participants reported never wearing double gloves, 78% (n=1,886) not wearing protective goggles, 95% (n=1,953) respirators, 93% (n=1,997) foot protectors and 94% (n=1,995), caps. Figure 2 presents the results obtained from the sample on the conditions that facilitate and hinder PPE use.
Presentation of the results of the conditions that facilitate and hinder PPE use by the Nursing team in the hospital environment. Florianópolis, SC, Brazil, 2021.
In addition, the nurses who perceived the organization's support in relation to health and safety were twice as likely to report adherence to the use of respiratory protection masks.2929. Nichol K, McGeer A, Bigelow P, O'Brien-Pallas L, Scott J, Holness DL. Behind the mask: determinants of nurse's adherence to facial protective equipment. Am J Infect Control [Internet]. 2013 [cited 2021 Oct 16];41(1):8-13. Available from: https://doi.org/10.1016/j.ajic.2011.12.018
https://doi.org/10.1016/j.ajic.2011.12.0...
Regarding the organizational factors, as reasons for not using chemotherapy gloves, the nurses mentioned low skin exposure, that PPE items were not offered by their employers, and that they were not part of the institution's protocol. In turn, in relation to the use of non-absorbent aprons, it was identified that no professional uses them. Regarding goggles and respirators, the respondents increasingly asserted the following: that they were not part of the protocol, little skin exposure, and that an engineering control was being used.4242. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
https://doi.org/10.1080/15459624.2014.91...
When it comes to the professionals' experience, no statistically significant difference was identified between Nursing professionals with less and more than six years of experience. However, it was noticed that the professionals with more than 10 years of experience were more adherent to washing their hands after removing the disposable gloves than those with less than six years of experience. Overall, adherence to the standard precautions in this study was considered to be intermediate.3535. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
https://doi.org/10.1590/0034-7167-2016-0...
In the results of the current review, excessive PPE use was identified in situations in which there is no indication; the most used were surgical masks,2727. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
https://doi.org/10.1111/j.1365-2648.2010...
aprons,2828. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
https://doi.org/10.1016/j.ijid.2009.03.0...
respiratory protection masks2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
,2727. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
https://doi.org/10.1111/j.1365-2648.2010...
and sterile gloves.2727. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
https://doi.org/10.1111/j.1365-2648.2010...
It was observed that few nurses, 20.2% (n=17), were following the standard infection control precautions and that a reduced number was following the transmission-based isolation precautions: 11.9% (n=10).3232. Suliman M, Aloush S, Aljezawi M, AlBashtawy M. Knowledge and practices of isolation precautions among nurses in Jordan. Am J Infect Control [Internet]. 2018 [cited 2021 Sep 28];46(6):680-84. Available from: https://doi.org/10.1016/j.ajic.2017.09.023
https://doi.org/10.1016/j.ajic.2017.09.0...
The type of unit was a significant predictor of adherence to respiratory protection masks by the emergency room nurses, as 60% reported that they are less likely to use such masks when compared to intensive care nurses. This is explained due to the fast-paced and hectic work environment, more focused on making diagnoses, managing crises and dealing with unforeseen events.2929. Nichol K, McGeer A, Bigelow P, O'Brien-Pallas L, Scott J, Holness DL. Behind the mask: determinants of nurse's adherence to facial protective equipment. Am J Infect Control [Internet]. 2013 [cited 2021 Oct 16];41(1):8-13. Available from: https://doi.org/10.1016/j.ajic.2011.12.018
https://doi.org/10.1016/j.ajic.2011.12.0...
Therefore, the Emergency Room was shown to be the locus with the lowest adherence to N95 masks.2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
In addition, the literature shows that the Nursing team is responsible for implementing infection control practices in patient care, with nurses being responsible for the Hospital Infection Control Commission, in its various functions, identifying Nursing adherence to the established policies.4747. World Health Organization. Prevention of hospital-acquired infections: a practical guide [Internet]. Genève (CH): WHO ; 2002 [cited 2021 Nov 04]. 64 p. Available from: https://apps.who.int/iris/handle/10665/67350
https://apps.who.int/iris/handle/10665/6...
DISCUSSION
In the current review it was sought to know what has been produced in the literature about PPE use by Nursing professionals in the hospital environment, considering the initial milestones of the public policies on safety at work.
The sample was heterogeneous in terms of the objectives, number of professionals included, time of experience and instruments used; however, there was predominance of cross-sectional studies, evidencing that there is a gap in intervention studies for PPE use or for the adoption of guidelines by Nursing professionals. As expected, there is a greater number of international publications on the theme. Considering that Brazil is a continental country with different realities and cultures, it is suggested to advance in the conduction of research studies related to PPE use by the Nursing team.
The hospital scenario is complex, consisting of a multiprofessional team with different specialties and organizational cultures. Thus, various factors can contribute to adherence or non-adherence to the instituted policies.
From the individual factors, the influence of colleagues and supervisors for PPE use is recognized. Choice to use it or not is individual, although there are shared values and beliefs that can be decisive in the personal choices. As also already mentioned, the perception of contamination risk along with work relationships must be observed and can be a strategy for the development of prevention measures, as well as of measures for improving adherence and promote behavioral changes4949. Neves HCC, Ribeiro LCM, Souza ACS, Munari DB, Medeiros M. The influence of interpersonal relationships in adherance to the use of Personal Protective Equipment. Saúde Transform Soc [Internet]. 2011 [cited 2021 Oct 25];2(1):84-93. Available from: https://incubadora.periodicos.ufsc.br/index.php/saudeetransformacao/article/view/512
https://incubadora.periodicos.ufsc.br/in...
. The literature shows that future training programs should consider increasing the perception of self-efficacy and knowledge about the protection strategies used.5050. Mortada E, Abdel-Azeem A, Al Showair A, Zalat MM. Preventive behaviors towards Covid-19 pandemic among healthcare providers in Saudi Arabia using the protection motivation theory. Risk Manag Healthc Policy [Internet]. 2021 [cited 2021 Oct 24];14:685-94. Available from: https://doi.org/10.2147/RMHP.S289837
https://doi.org/10.2147/RMHP.S289837...
Regarding the conditions that hinder PPE use at the individual level, lack of knowledge is recognized as a reality present among nurses in the face of the standard precautions, despite recognizing the need to use such items.5151. Faria LBG, Santos CTB, Faustino AM, Oliveira LMAC, Cruz KCT. Conhecimento e adesão do enfermeiro às precauções padrão em unidades críticas. Texto Contexto Enferm [Internet]. 2019 [cited 2021 Oct 24];28:e20180144. Available from: https://doi.org/10.1590/1980-265X-TCE-2018-0144
https://doi.org/10.1590/1980-265X-TCE-20...
As for the adherence findings of this review, high adherence to gloves and low adherence to goggles prevailed; however, no studies were found that substantiate low adherence to the use of goggles during the care provided, although it is suggested that this is related to the fact that the professionals do not perceive them as necessary despite being established in the regulatory and biosafety standards.
From the work factors, visual communication, such as signposts, available materials, adequate communication of patient information/conditions and training, is recognized as important in adherence to PPE use.
Nurses play a managerial role in organizing the work of their team and the unit5252. Chughtai AA, Seale H, Islam MS, Owais M, Macintyre CR. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19). Int J Nurs Stud [Internet]. 2020 [cited 2021 Sep 18];105:103567. Available from: https://doi.org/10.1016/j.ijnurstu.2020.103567
https://doi.org/10.1016/j.ijnurstu.2020....
. As pointed out in the review sample guideline,4848. American Society of Health-System Pharmacists. ASHP Guidelines on handling hazardous drugs. Am J Health Syst Pharm [Internet]. 2006 [cited 2021 Oct 25];63:1172-119. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
https://www.ashp.org/-/media/assets/poli...
nurses participate in hospital infection control commissions that should assist in adequacy of the hospital units, as well as facilitate the training processes of other professionals working in the institution. In addition to educational interventions and improvement of the work environment, diverse research results suggest that the workload should also be evaluated for the professionals to use PPE items5353. Aloush SM. Does educating nurses with ventilator-associated pneumonia prevention guidelines improve their compliance? Am J Infect Control [Internet]. 2017 [cited 2021 Oct 24];45(9):969-73. Available from: https://doi.org/10.1016/j.ajic.2017.04.009
https://doi.org/10.1016/j.ajic.2017.04.0...
.
From the organizational aspects, there is also the challenge faced by hospitals regarding the financial burden. The literature mentions that the daily costs to maintain PPE items in Intensive Care Units increased by nearly 500% at the beginning of the COVID-19 pandemic.5454. Oliveira ACC, Magalhães NCV, Silva PAAA, Barja PR, Viriato A. Gestão hospitalar de equipamentos de proteção individual no enfrentamento à pandemia COVID19. Braz J Dev [Internet]. 2021 [cited 2021 Oct 06];7(3):23814-31. Available from: https://doi.org/10.34117/bjdv7n3-203
https://doi.org/10.34117/bjdv7n3-203...
As there was no forecast of an epidemic and, therefore, no financial planning for such an expense, many units were left without PPE items, as seen in the world's media. Associated with this, the impact on the production of PPE items in China due to the pandemic was evident.
Although few studies addressed accessibility to PPE items by the professionals, the results showed that the most expensive PPE items, such as N95 masks, are stored further away to avoid misuse.2525. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
https://doi.org/10.1016/j.ajic.2019.04.1...
Therefore, the need to intervene in educating the Nursing team professionals is recognized, so that they can elucidate use of this PPE.
As for the managerial actions, the PPE adherence audit is recognized, so that it can monitor use by the Nursing team. However, this surveillance action has the Hawthorne effect as a negative aspect, which could be reduced by using camcorders.5555. Oliveira AC, Paula AO. Monitoração da adesão à higienização das mãos: uma revisão de literatura. Acta Paul Enferm [Internet]. 2011 [cited 2021 Sep 28];24(3):407-13. Available from: https://doi.org/10.1590/S0103-21002011000300016
https://doi.org/10.1590/S0103-2100201100...
Interesting results on adherence to PPE in the face of handling dangerous drugs shows detectable levels of antineoplastic medications in the urine of the professionals who handle them, an assessment made through biological monitoring, which characterizes permanence of occupational exposure.5656. United States Department of Labor. Occupational Health and Safety Administration. OSHA Technical Manual [Internet]. 2016 [cited 2021 Oct 05]. Available from: https://www.osha.gov/otm
https://www.osha.gov/otm...
However, as seen in the results, there are guidelines that recommend and guide proper PPE use when it comes to toxic medications.
This biological monitoring process is carried out through the safe handling program, a monitoring practice that is also applied to biological agents, as in the case of COVID-19.5757. Gallasch CH, Cunha ML, Pereira LAS, Silva-Junior JS. Prevention related to the occupational exposure of health professionals workers in the COVID-19 scenario. Rev Enferm UERJ [Internet]. 2020 [cited 2021 Oct 24];28:e49596. Available from: https://doi.org/10.12957/reuerj.2020.49596
https://doi.org/10.12957/reuerj.2020.495...
However, no studies were found that addressed this practice in management. This care measure can also be applied to the professionals who take care of patients with tuberculosis, through admission and annual screening, performing chest X-rays and serological tests.3939. Anwar MM, Ahmed DM, Elareed HR, Abdel-Latif RA, Sheemy MS, Kamel NM, et al. Screening for latent tuberculosis among healthcare workers in an egyptian hospital using tuberculin skin test and quantiFERON-TB gold in-tube test. Indian J Occup Environ Med [Internet]. 2019 [cited 2021 Sep 30];23(3):106-11. Available from: https://doi.org/10.4103/ijoem.IJOEM_184_19
https://doi.org/10.4103/ijoem.IJOEM_184_...
Therefore, the importance of professional care regarding handling of these drugs is emphasized through training and standardization grounded on occupational safety and on protection of the patients, the workers and the environment.5858. Batista KC, Sousa KHJF, Ruas CAS, Zeitoune RCG. Conhecimentos sobre drogas antineoplásicas: implicações para a saúde do trabalhador de enfermagem em hospital geral. Rev Bras Enferm [Internet]. 2021 [cited 2021 Sep 30];75(3):e20210025. Available from: https://doi.org/10.1590/0034-7167-2021-0025
https://doi.org/10.1590/0034-7167-2021-0...
In addition to these aspects, the importance of PPE availability and permanent education is highlighted5959. Sousa KR, Miranda MAL. Percepção dos profissionais de enfermagem sobre o uso dos equipamentos de proteção individual na emergência. Com Cienc Saúde [Internet]. 2021 [cited 2021 Oct 24];32(2):49-60. Available from: https://revistaccs.escs.edu.br/index.php/comunicacaoemcienciasdasaude/article/view/797
https://revistaccs.escs.edu.br/index.php...
, reinforcing the results of the current review, which point out that there is a need for nurses to participate in the clinical practice in the decisions/elaboration of managerial aspects, thus helping to survey the real needs of the team6060. Prado PR, Ventura CAA, Rigotti AR, Reis RK, Zamarioli CM, Souza FB, Gimenes FRE. Linking worker safety to patient safety: recommendations and bioethical issues for the care of patients in the COVID-19 pandemic. Texto Contexto Enferm [Internet]. 2021 [cited 2021 Oct 30];30:e20200535. Available from: https://doi.org/10.1590/1980-265X-TCE-2020-0535
https://doi.org/10.1590/1980-265X-TCE-20...
. Actions and interventions must be articulated by the management of the units and service managers in a way that can favor the safety climate and, consequently, the safety culture of professionals and patients alike.5757. Gallasch CH, Cunha ML, Pereira LAS, Silva-Junior JS. Prevention related to the occupational exposure of health professionals workers in the COVID-19 scenario. Rev Enferm UERJ [Internet]. 2020 [cited 2021 Oct 24];28:e49596. Available from: https://doi.org/10.12957/reuerj.2020.49596
https://doi.org/10.12957/reuerj.2020.495...
The results of the current review indicate potential studies in order to verify adherence or non-adherence to PPE use by Nursing professionals, mainly bringing the individual, work and organizational aspects to light. Intervention studies help with evidence and, consequently, with practices. As for the Nursing practice, the results indicate that interpersonal relationships, leadership and organization are fundamental for adherence. With regard to teaching, it can be reinforced that nurses are educators and producers of knowledge.
CONCLUSION
The conditions that favor PPE use are geared towards education related to behavioral knowledge; in the face of adherence to PPE, gloves were identified as with greater adherence and goggles as less adhered to; a gap found was in relation to the investigation of low adherence to protection goggles in the assistance provided.
As for work, visual communication was identified as favorable; and sectors that demand dynamics, such as emergency rooms, and workload, as factors that exert negative influences on PPE use. As for the organization, it is worth incorporating managerial practices in relation to the working conditions and standardization of diverse information, as well as including healthcare professionals in the decision-making process. There is concern for workers handling dangerous drugs; however, a gap was found in relation to studies that address the monitoring program for the surveillance of occupational exposure.
ACKNOWLEDGMENT
To Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) for their financial support.
REFERENCES
- 1. Fernandes MA, Castro SFF, Furtado NI, Araújo EC, Lemos GP, Oliveira ALCB. Utilização de equipamentos de proteção individual: interfaces com o conhecimento dos profissionais de saúde. Rev Prev Infec Saúde [Internet]. 2017 [cited 2021 Oct 28];3(1):16-21. Available from: https://revistas.ufpi.br/index.php/nupcis/article/view/6209
» https://revistas.ufpi.br/index.php/nupcis/article/view/6209 - 2. Ministério da Saúde (BR). Agência Nacional de Vigilância Sanitária. Resolução RDC nº 302, de 13 de outubro de 2005. Dispõe sobre Regulamento Técnico para funcionamento de Laboratórios Clínicos [Internet]. 2005 [cited 2022 Apr 07]. Available from: http://bvsms.saude.gov.br/bvs/saudelegis/anvisa/2005/anexo/anexo_res0302_13_10_2005.pdf
» http://bvsms.saude.gov.br/bvs/saudelegis/anvisa/2005/anexo/anexo_res0302_13_10_2005.pdf - 3. Ministério da Saúde (BR). Norma Regulamentadora (NR-6) [Internet]. 2022 [cited 2022 Apr 07]. Available from: https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-6-nr-6
» https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-6-nr-6 - 4. Ministério do Trabalho e Emprego (BR). NR 32 - Segurança e Saúde no Trabalho em Serviços de Saúde [Internet]. 2020 [cited 2022 Mar 31]. Available from: https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-32-nr-32
» https://www.gov.br/trabalho-e-previdencia/pt-br/composicao/orgaos-especificos/secretaria-de-trabalho/inspecao/seguranca-e-saude-no-trabalho/ctpp-nrs/norma-regulamentadora-no-32-nr-32 - 5. Souza RT, Bica CG, Mondadori CS, Ranzi AD. Evaluation of occupational accidents with biological materials in medical residents, academics and interns of school hospital of Porto Alegre. Rev Bras Educ Med [Internet]. 2012 [cited 2021 Oct 06];36(1):118-24. Available from: https://doi.org/10.1590/S0100-55022012000100016
» https://doi.org/10.1590/S0100-55022012000100016 - 6. Pustiglione M, Galesi VMN, Santos LAR, Bombarda S, Tognini S, Freitas AC, et al. Tuberculosis in health care workers: a problem to be faced. Rev Med [Internet]. 2020 [cited 2021 Oct 07];99(1):16-26. Available from: https://doi.org/10.11606/issn.1679-9836.v99i1p16-26
» https://doi.org/10.11606/issn.1679-9836.v99i1p16-26 - 7. Suwantarat N, Apisarnthanarak A. Risks to healthcare workers with emerging diseases: lessons from MERS-CoV, Ebola, SARS, and avian flu. Curr Opin Infect Dis [Internet]. 2015 [cited 2021 Oct 07];28(4):349-61. Available from: https://doi.org/10.1097/QCO.0000000000000183
» https://doi.org/10.1097/QCO.0000000000000183 - 8. Nafisah SAB, Mzahim BY, Aleid BS, Sheerah SA, Almatrafi DQ, Ciottone GR, et al. The risk of coronavirus to healthcare providers during aerosol-generating procedures: A systematic review and meta-analysis. Ann Thorac Med [Internet]. 2021 [cited 2021 Oct 07];16(2):165-71. Available from: https://doi.org/10.4103/atm.ATM_497_20
» https://doi.org/10.4103/atm.ATM_497_20 - 9. Yu E. Occupational exposure in health care personnel to antineoplastic drugs and initiation of safe handling in Hong Kong: a literature review. J Infus Nurs [Internet]. 2020 [cited 2021 Oct 06];43(3):121-33. Available from: https://doi.org/10.1097/NAN.0000000000000361
» https://doi.org/10.1097/NAN.0000000000000361 - 10. Liu M, Cheng SZ, Xu KW, Yang Y, Zhu QT, Zhang H, et al. Use of personal protective equipment against coronavirus disease 2019 by healthcare professionals in Wuhan, China: cross sectional study. BMJ [Internet]. 2020 [cited 2021 Oct 07];369:m2195. Available from: https://doi.org/10.1136/bmj.m2195
» https://doi.org/10.1136/bmj.m2195 - 11. Costa AG, Costa MS, Ferreira ES, Sousa PC, Santos MM, Lima DE, et al. Knowledge of Nursing Professional on the Safety of the Oncological Patient in Chemoterapy. Rev Bras Cancerol [Internet]. 2019 [cited 2021 Oct 07];65(1):e-04274. Available from: https://doi.org/10.32635/2176-9745.RBC.2019v65n1.274
» https://doi.org/10.32635/2176-9745.RBC.2019v65n1.274 - 12. Bastos APS, Brito MAR, Ferreira JLR, Ferreira JGOR, Araujo VSC, Val HMC, et al. Equipamentos de proteção individual e a adesão do conhecimento dos profissionais e acadêmicos: revisão integrativa. Rev Eletro Acer Saúde [Internet]. 2020 [cited 2021 Sep 30];27(53):e3764. Available from: https://doi.org/10.25248/reas.e3764.2020
» https://doi.org/10.25248/reas.e3764.2020 - 13. Chan JF, Yuan S, Kok KH, To KK, Chu H, Yang J, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet [Internet]. 2020 [cited 2021 Sep 11];395(10223):514-23. Available from: https://doi.org/10.1016/S0140-6736(20)30154-9
» https://doi.org/10.1016/S0140-6736(20)30154-9 - 14. Araújo TM, Caetano JÁ, Barros LM, Lima AC, da Costa RM, Monteiro VA. Acidentes de trabalho com exposição a material biológico entre os profissionais de Enfermagem. Rev Enferm Refer [Internet]. 2012 [cited 2021 Oct 29];3(7):7-14. Available from: https://www.redalyc.org/articulo.oa?id=388239966004
» https://www.redalyc.org/articulo.oa?id=388239966004 - 15. Silva OM, Cabral DB, Marin SM, Bitencourt JVO, Vargas MAO, Meschial WC. Biosafety measures to prevent COVID-19 in healthcare professionals: an integrative review. Rev Bras Enferm [Internet]. 2022 [cited 2021 Sep 30];75(1):e20201191. Available from: https://doi.org/10.1590/0034-7167-2020-1191
» https://doi.org/10.1590/0034-7167-2020-1191 - 16. Hrdinová N, Saibertová S, Pokorná A. The use of personal protective equipment in a biosafety level 2 prospective observational study. Crit Care Nurs Q [Internet]. 2021 [cited 2021 Sep 30];44(4):403-12. Available from: https://doi.org/10.1097/CNQ.0000000000000377
» https://doi.org/10.1097/CNQ.0000000000000377 - 17. Cavalcante WS, Almeida AGS, Lima AA, Nunes ICM, Nagliate PC, Sarmento PA. Recomendações quanto ao uso de máscaras/respiradores de proteção por profissionais de saúde em risco de exposição ao sars-cov-2: scoping review. Res Soc Dev [Internet]. 2021 [cited 2021 Sep 30];10(1):e16710111628. Available from: https://doi.org/10.33448/rsd-v10i1.11628
» https://doi.org/10.33448/rsd-v10i1.11628 - 18. Garcia GPA, Fracarolli IFL, Santos HEC, Souza VRS, Cenzi CM, Marziale MHP. Use of personal protective equipment to care for patients with COVID-19: scoping review. Rev Gaucha Enferm [Internet]. 2021 [cited 2021 Sep 30];42(spe):e20200150. Available from: https://doi.org/10.1590/1983-1447.2021.20200150
» https://doi.org/10.1590/1983-1447.2021.20200150 - 19. Mays N, Roberts E, Popay J. Synthesising research evidence. In: Fulop N, Allen P, Clarke A, Black N, editors. Studying the organisation and delivery of health services: research methods. London: Routledge; 2001. p. 188-20. [cited 2021 Sep 30]. Available form: Available form: https://researchonline.lshtm.ac.uk/id/eprint/15408
» https://researchonline.lshtm.ac.uk/id/eprint/15408 - 20. Peters MDJ, Godfrey C, McInerney P, Munn Z, Tricco AC, Khalil H. Chapter 11: Scoping Reviews. In: Aromataris E, Munn Z, editors. JBI Manual for evidence synthesis. 2020. p. 408-46 [cited 2021 Aug 15]. Available from: https://doi.org/10.46658/JBIMES-20-01
» https://doi.org/10.46658/JBIMES-20-01 - 21. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med [Internet]. 2018 [cited 2021 Oct 30];169(7):467-73. Available from: https://doi.org/10.7326/M18-0850
» https://doi.org/10.7326/M18-0850 - 22. Cunha QB, Camponogara S, Freitas EO, Pinno C, Dias GL, Cesar MP. Fatores que interferem na adesão às precauções padrão por profissionais da saúde: revisão integrativa. Enferm Foco [Internet]. 2017 [cited 2021 Oct 24];8(1):72-6. Available from: https://doi.org/10.21675/2357-707X.2017.v8.n1.980
» https://doi.org/10.21675/2357-707X.2017.v8.n1.980 - 23. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ [Internet]. 2021 [cited 2021 Oct 17];372:71. Available from: https://doi.org/10.1136/bmj.n71
» https://doi.org/10.1136/bmj.n71 - 24. Santos JLG, Balsanelli AP, Freitas EO, Menegon FHA, Carneiro IA, Lazzari DD, et al. Work environment of hospital nurses during the COVID‐19 pandemic in Brazil. Int Nurs Rev [Internet]. 2021 [cited 2021 Sep 18];68(2):228-37. Available from: https://doi.org/doi:10.1111/inr.12662
» https://doi.org/doi:10.1111/inr.12662 - 25. Fix GM, Reisinger HS, Etchin A, McDannold S, Eagan A, Findley K, et al. Health care workers’ perceptions and reported use of respiratory protective equipment: a qualitative analysis. Am J Infect Control [Internet]. 2019 [cited 2021 Oct 06];47(10):1162-66. Available from: https://doi.org/10.1016/j.ajic.2019.04.174
» https://doi.org/10.1016/j.ajic.2019.04.174 - 26. Hessels AJ, Weaver SH. Missed opportunities: the development and testing of standard precaution case vignettes. J Infus Nurs [Internet]. 2019 [cited 2021 Oct 16];42(2):70-74. Available from: https://doi.org/10.1097/NAN.0000000000000314
» https://doi.org/10.1097/NAN.0000000000000314 - 27. Landers T, McWalters J, Behta M, Bufe G, Ross B, Vawdrey DK, et al. Terms used for isolation practices by nurses at an academic medical center. J Adv Nurs [Internet]. 2010 [cited 2021 Oct 16];66(10):2309-19. Available from: https://doi.org/10.1111/j.1365-2648.2010.05398.x
» https://doi.org/10.1111/j.1365-2648.2010.05398.x - 28. Luo Y, He GP, Zhou JW, Luo Y. Factors impacting compliance with standard precautions in nursing, China. Int J Infect Dis [Internet]. 2010 [cited 2021 Sep 18];14(12):e1106-14. Available from: https://doi.org/10.1016/j.ijid.2009.03.037
» https://doi.org/10.1016/j.ijid.2009.03.037 - 29. Nichol K, McGeer A, Bigelow P, O'Brien-Pallas L, Scott J, Holness DL. Behind the mask: determinants of nurse's adherence to facial protective equipment. Am J Infect Control [Internet]. 2013 [cited 2021 Oct 16];41(1):8-13. Available from: https://doi.org/10.1016/j.ajic.2011.12.018
» https://doi.org/10.1016/j.ajic.2011.12.018 - 30. Rozenbojm MD, Nichol K, Spielmann S, Holness DL. Hospital unit safety climate: relationship with nurses' adherence to recommended use of facial protective equipment. Am J Infect Control [Internet]. 2015 [cited 2021 Oct 16];43(2):115-20. Available from: https://doi.org/10.1016/j.ajic.2014.10.027
» https://doi.org/10.1016/j.ajic.2014.10.027 - 31. Sissolak D, Marais F, Mehtar S. TB infection prevention and control experiences of South African nurses-a phenomenological study. BMC Public Health [Internet]. 2011 [cited 2021 Oct 18];11:262. Available from: https://doi.org/10.1186/1471-2458-11-262
» https://doi.org/10.1186/1471-2458-11-262 - 32. Suliman M, Aloush S, Aljezawi M, AlBashtawy M. Knowledge and practices of isolation precautions among nurses in Jordan. Am J Infect Control [Internet]. 2018 [cited 2021 Sep 28];46(6):680-84. Available from: https://doi.org/10.1016/j.ajic.2017.09.023
» https://doi.org/10.1016/j.ajic.2017.09.023 - 33. Callahan A, Ames NJ, Manning ML, Touchton-Leonard K, Yang L, Wallen GR. Factors influencing nurses’ use of hazardous drug safe-handling precautions. Oncol Nurs Forum [Internet]. 2016 [cited 2021 Oct 15];43(3):342-49. Available from: https://doi.org/10.1188/16.ONF.43-03AP
» https://doi.org/10.1188/16.ONF.43-03AP - 34. Castro AF, Rodrigues MCS. Auditoria de práticas de precauções-padrão e contato em Unidade de Terapia Intensiva. Rev Esc Enferm USP [Internet]. 2019 [cited 2021 Oct 16];53:e03508. Available from: https://doi.org/10.1590/S1980-220X2018018603508
» https://doi.org/10.1590/S1980-220X2018018603508 - 35. Ferreira LA, Peixoto CD, Paiva L, Silva QCG, Rezende MP, Barbosa MH. Adesão às precauções padrão em um hospital de ensino. Rev Bras Enferm [Internet]. 2017 [cited 2021 Oct 16];70(1):96-103. Available from: https://doi.org/10.1590/0034-7167-2016-0138
» https://doi.org/10.1590/0034-7167-2016-0138 - 36. Villarinho MV, Padilha MICS. Risco ao acidente ocupacional no cuidado às pessoas internadas por HIV/AIDS, em Florianópolis-SC, Brasil (1986-2006). Rev Enferm UFSM [Internet]. 2014 [cited 2021 Sep 30];4(4):689-699. Available from: https://doi.org/10.5902/2179769212536
» https://doi.org/10.5902/2179769212536 - 37. Chen HC, Lu ZY, Lee SH. Nurses’ experiences in safe handling of chemotherapeutic agents: the Taiwan case. Cancer Nurs [Internet]. 2016 [cited 2021 Oct 15];39(5):E29-38. Available from: https://doi.org/10.1097/NCC.0000000000000314
» https://doi.org/10.1097/NCC.0000000000000314 - 38. Ganczak M, Szych Z. Surgical nurses and compliance with personal protective equipment. J Hosp Infect [Internet]. 2007 [cited 2021 Oct 16];66(4):346-51. Available from: https://doi.org/10.1016/j.jhin.2007.05.007
» https://doi.org/10.1016/j.jhin.2007.05.007 - 39. Anwar MM, Ahmed DM, Elareed HR, Abdel-Latif RA, Sheemy MS, Kamel NM, et al. Screening for latent tuberculosis among healthcare workers in an egyptian hospital using tuberculin skin test and quantiFERON-TB gold in-tube test. Indian J Occup Environ Med [Internet]. 2019 [cited 2021 Sep 30];23(3):106-11. Available from: https://doi.org/10.4103/ijoem.IJOEM_184_19
» https://doi.org/10.4103/ijoem.IJOEM_184_19 - 40. Asefa S, Aga F, Dinegde NG, Demie TG. Knowledge and practices on the safe handling of cytotoxic drugs among oncology nurses working at tertiary teaching hospitals in Addis Ababa, Ethiopia. Drug Healthc Patient Saf [Internet]. 2021 [cited 2021 Oct 16];13:71-80. Available from: https://doi.org/10.2147/DHPS.S289025
» https://doi.org/10.2147/DHPS.S289025 - 41. Tsai RJ, Boiano JM, Steege AL, Sweeney MH. Precautionary practices of respiratory therapists and other health-care practitioners who administer aerosolized medications. Respir Care [Internet]. 2015 [cited 2021 Oct 16];60(10):1409-17. Available from: https://doi.org/10.4187/respcare.03817
» https://doi.org/10.4187/respcare.03817 - 42. Boiano JM, Steege AL, Sweeney MH. Adherence to safe handling guideline by heath care workers who administer antineoplastic drugs. J Occup Environ Hyg [Internet]. 2014 [cited 2021 Oct 30];11(11):728-40. Available from: https://doi.org/10.1080/15459624.2014.916809
» https://doi.org/10.1080/15459624.2014.916809 - 43. Center for Disease Control and Prevention. The National Institute for Occupational Safety and Health. Hazardous Drug Exposures in Health Care [Internet]. 2016 [cited 2021 Oct 24]. Available from: https://www.cdc.gov/niosh/topics/hazdrug/
» https://www.cdc.gov/niosh/topics/hazdrug/ - 44. Center for Disease Control and Prevention. Preventing Occupational Exposures to Antineoplastic and other hazardous drugs in health care settings [Internet]. Cincinnat (OH): NIOSH; 2004 [cited 2021 Oct 24]. 50 p. Available from: https://www.cdc.gov/niosh/docs/2004-165/pdfs/2004-165.pdf
» https://www.cdc.gov/niosh/docs/2004-165/pdfs/2004-165.pdf - 45. Center for Disease Control and Prevention. Personal protective equipment for health care workers who work with hazardous drugs [Internet]. Cincinnat (OH): NIOSH ; 2008 [cited 2021 Oct 24]. Available from: https://stacks.cdc.gov/view/cdc/5762
» https://stacks.cdc.gov/view/cdc/5762 - 46. World Health Organization. Global health risks: mortality and burden of disease attributable to selected major risks [Internet]. Genève (CH): WHO; 2009 [cited 2021 Oct 30]. 62 p. Available from: https://apps.who.int/iris/handle/10665/44203
» https://apps.who.int/iris/handle/10665/44203 - 47. World Health Organization. Prevention of hospital-acquired infections: a practical guide [Internet]. Genève (CH): WHO ; 2002 [cited 2021 Nov 04]. 64 p. Available from: https://apps.who.int/iris/handle/10665/67350
» https://apps.who.int/iris/handle/10665/67350 - 48. American Society of Health-System Pharmacists. ASHP Guidelines on handling hazardous drugs. Am J Health Syst Pharm [Internet]. 2006 [cited 2021 Oct 25];63:1172-119. Available from: https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx
» https://www.ashp.org/-/media/assets/policy-guidelines/docs/guidelines/handling-hazardous-drugs.ashx - 49. Neves HCC, Ribeiro LCM, Souza ACS, Munari DB, Medeiros M. The influence of interpersonal relationships in adherance to the use of Personal Protective Equipment. Saúde Transform Soc [Internet]. 2011 [cited 2021 Oct 25];2(1):84-93. Available from: https://incubadora.periodicos.ufsc.br/index.php/saudeetransformacao/article/view/512
» https://incubadora.periodicos.ufsc.br/index.php/saudeetransformacao/article/view/512 - 50. Mortada E, Abdel-Azeem A, Al Showair A, Zalat MM. Preventive behaviors towards Covid-19 pandemic among healthcare providers in Saudi Arabia using the protection motivation theory. Risk Manag Healthc Policy [Internet]. 2021 [cited 2021 Oct 24];14:685-94. Available from: https://doi.org/10.2147/RMHP.S289837
» https://doi.org/10.2147/RMHP.S289837 - 51. Faria LBG, Santos CTB, Faustino AM, Oliveira LMAC, Cruz KCT. Conhecimento e adesão do enfermeiro às precauções padrão em unidades críticas. Texto Contexto Enferm [Internet]. 2019 [cited 2021 Oct 24];28:e20180144. Available from: https://doi.org/10.1590/1980-265X-TCE-2018-0144
» https://doi.org/10.1590/1980-265X-TCE-2018-0144 - 52. Chughtai AA, Seale H, Islam MS, Owais M, Macintyre CR. Policies on the use of respiratory protection for hospital health workers to protect from coronavirus disease (COVID-19). Int J Nurs Stud [Internet]. 2020 [cited 2021 Sep 18];105:103567. Available from: https://doi.org/10.1016/j.ijnurstu.2020.103567
» https://doi.org/10.1016/j.ijnurstu.2020.103567 - 53. Aloush SM. Does educating nurses with ventilator-associated pneumonia prevention guidelines improve their compliance? Am J Infect Control [Internet]. 2017 [cited 2021 Oct 24];45(9):969-73. Available from: https://doi.org/10.1016/j.ajic.2017.04.009
» https://doi.org/10.1016/j.ajic.2017.04.009 - 54. Oliveira ACC, Magalhães NCV, Silva PAAA, Barja PR, Viriato A. Gestão hospitalar de equipamentos de proteção individual no enfrentamento à pandemia COVID19. Braz J Dev [Internet]. 2021 [cited 2021 Oct 06];7(3):23814-31. Available from: https://doi.org/10.34117/bjdv7n3-203
» https://doi.org/10.34117/bjdv7n3-203 - 55. Oliveira AC, Paula AO. Monitoração da adesão à higienização das mãos: uma revisão de literatura. Acta Paul Enferm [Internet]. 2011 [cited 2021 Sep 28];24(3):407-13. Available from: https://doi.org/10.1590/S0103-21002011000300016
» https://doi.org/10.1590/S0103-21002011000300016 - 56. United States Department of Labor. Occupational Health and Safety Administration. OSHA Technical Manual [Internet]. 2016 [cited 2021 Oct 05]. Available from: https://www.osha.gov/otm
» https://www.osha.gov/otm - 57. Gallasch CH, Cunha ML, Pereira LAS, Silva-Junior JS. Prevention related to the occupational exposure of health professionals workers in the COVID-19 scenario. Rev Enferm UERJ [Internet]. 2020 [cited 2021 Oct 24];28:e49596. Available from: https://doi.org/10.12957/reuerj.2020.49596
» https://doi.org/10.12957/reuerj.2020.49596 - 58. Batista KC, Sousa KHJF, Ruas CAS, Zeitoune RCG. Conhecimentos sobre drogas antineoplásicas: implicações para a saúde do trabalhador de enfermagem em hospital geral. Rev Bras Enferm [Internet]. 2021 [cited 2021 Sep 30];75(3):e20210025. Available from: https://doi.org/10.1590/0034-7167-2021-0025
» https://doi.org/10.1590/0034-7167-2021-0025 - 59. Sousa KR, Miranda MAL. Percepção dos profissionais de enfermagem sobre o uso dos equipamentos de proteção individual na emergência. Com Cienc Saúde [Internet]. 2021 [cited 2021 Oct 24];32(2):49-60. Available from: https://revistaccs.escs.edu.br/index.php/comunicacaoemcienciasdasaude/article/view/797
» https://revistaccs.escs.edu.br/index.php/comunicacaoemcienciasdasaude/article/view/797 - 60. Prado PR, Ventura CAA, Rigotti AR, Reis RK, Zamarioli CM, Souza FB, Gimenes FRE. Linking worker safety to patient safety: recommendations and bioethical issues for the care of patients in the COVID-19 pandemic. Texto Contexto Enferm [Internet]. 2021 [cited 2021 Oct 30];30:e20200535. Available from: https://doi.org/10.1590/1980-265X-TCE-2020-0535
» https://doi.org/10.1590/1980-265X-TCE-2020-0535
-
ORIGIN OF THE ARTICLE
Extracted from the dissertation - Assessment of nurses' beliefs related to the use of respiratory protection masks to prevent COVID-19 in the Intensive Care Units from the South of the country, presented at the Graduate Program in Nursing, Universidade Federal de Santa Catarina, in 2021.
Publication Dates
-
Publication in this collection
01 Aug 2022 -
Date of issue
2022
History
-
Received
26 Nov 2021 -
Accepted
13 May 2022