Abstracts
Patients who have undergone bariatric surgery are at increased risk of developing nutritional deficiencies from limited food intake and absorption of different nutrients. A systematic review of several database websites (PubMed and ISI Web of Science) was conducted from September 1983 to April 2010 to identify literature related to micronutrient deficiencies occurring after bariatric surgery. Keywords used individually or in various combinations in the search were bariatric surgery, obesity, vitamin/mineral deficiencies, protein deficiency, nutrient absorption and nutrient supplementation. Literature suggests that to prevent or treat nutritional deficiencies resulting from anatomical changes due to surgical techniques nutritional supplementation is usually necessary. The success of oral nutritional supplementation to correct or prevent nutritional deficiencies depends on several factors. Thus, to understand how nutrients can be administered is very important for clinical practice. This review aims to provide help for the best selection of nutrients to ensure an adequate replacement of nutrients in patients who have undergone bariatric surgery.
Deficiency diseases; bariatric surgery; gastric bypass; dietary supplements
Pacientes submetidos à cirurgia bariátrica apresentam maior risco de desenvolver deficiências nutricionais pela limitação na ingestão e absorção de diferentes nutrientes. Desta forma, realizamos uma revisão sistemática no PubMed e ISI Web of Science incluindo artigos de setembro de 1983 a abril de 2010 para identificar as principais deficiências nutricionais após a cirurgia bariátrica e de que forma ocorre o seu tratamento. As palavras-chave utilizadas individualmente ou em associação foram: cirurgia bariátrica, obesidade, deficiência de vitamina/mineral, deficiência de proteína, absorção de nutrientes e suplementação de nutrientes. A literatura sugere que para prevenir ou tratar as deficiências nutricionais decorrentes das alterações anatômicas provocadas pelas técnicas cirúrgicas é necessário o uso de suplementação nutricional. O sucesso da suplementação nutricional oral em corrigir ou prevenir as deficiências nutricionais depende de vários fatores. Assim, compreender as formas pelas quais os nutrientes podem ser administrados é muito importante na prática clínica. Essa revisão tem como objetivo auxiliar a melhor seleção de nutrientes de forma a garantir uma reposição adequada dos nutrientes em pacientes submetidos à cirurgia bariátrica.
Deficiências nutricionais; cirurgia bariátrica; derivação gástrica; suplementos dietéticos
REVIEW ARTICLE
IPh.D Student in Sciences of Nutrition, Universidade Federal de Viçosa - UFV; Specialist Degree Associated with Baratric Surgery from Sociedade Brasileira de Cirurgia Bariátrica e Metabólica - SBCBM, Viçosa, MG
IINutritionist; Postgraduate in Functional Nutrition (VP Consultoria); Ph.D Student in Sciences of Nutrition, UFV, Viçosa, MG
IIIPh.D. in Physiology and Nutrition, Universidad de Navarra and Post-doctorate, Luoisina State University; Professor and Coordinator of Post-Graduation of Sciences of Nutrition, UFV, MG
IVPh.D. in Science and Food Technology, UFV; Post-Doctorate and Researcher Study Group on Nutrition and Obesity, UFV, MG
Corresponding author
ABSTRACT
Patients undergoing bariatric surgery are at increased risk of developing nutritional deficiencies from the limited intake and absorption of different nutrients. Thus, a systematic review on PubMed and ISI Web of Science was conducted, including articles from September 1983 to April 2010, to identify literature regarding nutritional deficiencies following bariatric surgery and how treatment is carried out. The keywords used individually or in combinations were: bariatric surgery, obesity, vitamin/mineral deficiencies, protein deficiency, nutrient absorption, and nutrient supplementation. The literature suggests the use of nutritional supplementation to prevent or treat nutritional deficiencies resulting from anatomical changes due to surgical techniques. The success of oral nutritional supplementation in correcting or preventing nutritional deficiencies depends on several factors. Thus, it is very important in clinical practice to understand how the nutrients can be administered. This review aims is to assist in better selecting the nutrients to ensure an appropriate nutrient replacement in patients undergoing bariatric surgery.
Keywords: Nutritional deficiencies; bariatric surgery; gastric bypass; dietary supplements.
Introduction
Currently, bariatric surgery is considered the most effective tool in severe obesity control and treatment. The surgery benefits include healing or marked improvement of chronic diseases, such as hypertension, diabetes and hyperlipidemia1. However, it must be noted that surgical treatment of obesity is not confined to surgery.
In vivo studies have demonstrated that some nutritional deficiencies encompassing vitamin D2-4, vitamin A5,6 and zinc are concomitantly present in obesity, possibly by playing important role in adiposity regulation or in appetite regulation mechanisms. Thus, a careful planning for clinical-nutritional follow-up is essential. Both pre- and early and late postoperatory is extremely important for treatment success10. In this setting, the phrase "healthy weight loss" has been well applied.
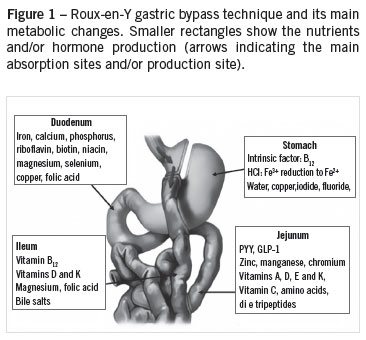
The implications of surgical procedures on the patient's nutritional status are specifically due to anatomical and physiological changes impairing absorption pathways and/or food intake. A good understanding of gastrointestinal tract absorption physiology is very important to understand potential nutritional deficiencies following surgery (Figure 1)10,11.
The main type of bariatric surgery currently performed is the Roux-en-Y gastric bypass (RYGB)12, a mixed surgical technique by restricting the gastric cavity size and hence the amount of food ingested and by reducing the bowel surface in contact with the food (dysabsorption).
The poor nutrient absorption is one of the explanations for the weight loss reached by using dysabsorptive techniques, such as the biliopancreatic diversion with duodenal switch (BPD), with 25% of protein and 72% of fat no longer being absorbed13. Automatically, nutrients depending on dietary fat to be absorbed, such as liposoluble vitamins and zinc, are more susceptible to malabsorption from this kind of procedure14.
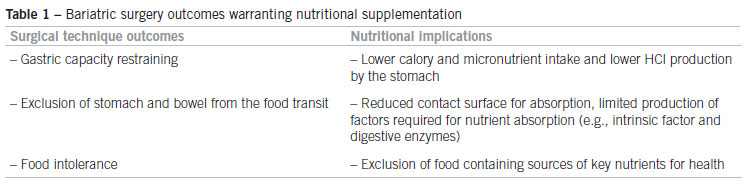
Vitamins and minerals are essential factors and cofactors in many biological processes regulating directly or indirectly the body weight (Table 1). The metabolic benefits of these micronutrients in controlling the weight loss include regulation of appetite, hunger, nutrient absorption, metabolic rate, lipid and carbohydrate metabolism, the functions of thyroid and adrenal glands, energy store, glucose homeostasis, and neural activities among others. Thus, the "adequacy" of micronutrients is important not only for health maintenance, but also for achieving maximum success in maintaining long-term weight loss13.
The symptoms of micronutrient deficiency are usually nonspecific in subclinical levels, and the physical exam may not be reliable for an early diagnosis without a laboratory confirmation. Thus, specific clinical signs are only noticeable in a developed phase of the deficiency15.
Considering the increasing number of bariatric surgeries currently performed and the presence of nutritional deficiencies found in these patients, we will address in this review a few nutrition supplementation forms currently proposed in literature with the purpose of better selecting the nutrients and ensure the appropriate replacement of nutrients.
Methodology
A systematic review in several data bases, such as PubMed (US National Library of Medicine, Bethesda, MD) and ISI Web of Science (Science Citation Index Expanded) was conducted. The following keywords were used individually or in combinations: bariatric surgery, obesity, gastric bypass, dietary supplement, vitamin deficiencies, mineral deficiencies, and nutrient absorption. Sixty-eight articles, published between September 1983 and April 2010, were selected, including two meta-analysis and two international guidelines for clinical practice in bariatric surgery. Only two studies were not conducted in humans.
Nutritional supplementation
Micronutrient deficiencies are the main changes that put the surgical procedure success at risk16. Prevention of vitamin and mineral deficiencies requires long-term patient's follow-up and understanding of the functions of these micronutrients in human body, in addition to the deficiency signs and symptoms. The long-term nutritional supplementation, although so stressed as an important conduct, still represents a hindrance to success in surgical treatment of obesity17.
The regular use of a nutritional supplementation has been advocated when appropriately done: at least five times a week13. However, only 33% of patients comply with that recommendation, and 7.7% stop using the multivitamins/minerals two years after surgery18.
The replacement and incorporation of micronutrients from food into the body is the most appropriate way to keep the body stores within the desirable level. However, a few factors warrant the nutritional supplementation in patients undergoing bariatric surgery (Table1). Therefore, the use of an appropriate multivitamin/mineral daily dose is a way to ensure the appropriate nutritional support of micronutrients for a good functioning of processes assisting in body weight regulation13.
The concern with micronutrient bioavailability influences on the supplementation efficacy. Accordingly, it is important to consider the quantitative and qualitative composition of marketed supplements. When choosing a supplement, consider:
- pH (acid or alkaline): required gastrointestinal pH to solubilize the nutrient;
- qualitative composition of the supplement: aqueous solution, capsule, powder;
- dependence of gastrointestinal enzymes assisting in some micronutrient absorption;
- bowel integrity and absorption surface;
- administration route: oral, intramuscular or intravenous, according to degree of nutritional deficiency;
- quantity and micronutrient type present in the composition.
With the advent of compounding pharmacies, it is possible to prepare vitamin and mineral formulations in several combinations, using the desired dose and at times with a similar or lower cost than commercial standard multivitamins. When opting for this form of supplementation, the clinician should be aware of the prescription form.
Other considerations are important when recommending multivitamins/minerals already marketed (Table 2). Usually folic acid and vitamin B12 are present in lower amounts and the formulations contain moderate doses of folate (200 - 400 mcg) and low doses of vitamin B12 (5-50 mcg). All patients undergoing BYGB and BPD should be supplemented with multivitamins/minerals as fully as possible, including liposoluble vitamins and minerals19.
It is important to remember that some nutrients require a specialized mixture to obtain maximum absorption. For instance, iron is better absorbed in an acid environment and liposoluble vitamins require a lipid source. In addition, certain nutrients are preferentially absorbed at proximal bowel while others at the distal bowel, as demonstrated in Figure 1. Thus, the kind or surgical procedure performed also influence the care in nutritional supplement choice. In Roux-en-Y gastric bypass (RYGB), e.g., there is a prevalence of vitamin B12, iron, and folic acid deficiencies14. On the other hand, following biliopancreatic diversion/duodenal swich (BPD/DS), only 28% of lipids ingested are absorbed20.
Starting multivitamin/mineral supplementation or isolate iron replacement has been recommended soon after hospital discharge13. However, some hospitals have already made such supplementation available in the early postoperative period (48 hours).
Isolate supplementation of vitamins and/or minerals is used in cases of nutritional deficiency diagnosis or when there is a purpose of reducing the interaction with other nutrients that could impair their absorption (Table 3). In this case, the clinician and nutritionist determine whether a multivitamin/mineral supplementation may remain or not concurrently with deficiency therapy. Below we will report studied forms of supplementation after bariatric surgery.
Thiamine
Thiamine deficiency may occur acutely following any type of bariatric surgery in patients presenting with longstanding vomiting and is associated with severe neurological symptoms that could even be irreversible21-23.
Thiamine deficiency following bariatric surgery has been treated together with other B complex vitamins and magnesium to achieve maximum thiamine absorption and appropriate neurological function24.
The first symptoms of neuropathy can often be resolved by oral supplementation with thiamine 20-30 mg/day until symptoms subside. When there are signs of a more advanced neuropathy or in the presence of persisting vomiting, 50-100 mg/day intravenously or intramuscularly may be required.
In the presence of the Wernicke-Korsakoff syndrome, a supplementation above 100 mg/day is required25. This syndrome is characterized by signs such as ophthalmolplegia (lateral rectus muscle and conjugate gaze palsy or weakness), ataxia (ambulation or posture impairment and slow gait), and mental and conscience disorders.
Most common risk factors associated with thiamine deficiency are: weight loss percentage, gastric symptoms persistence (nausea and vomiting), non-adherence to nutritional follow-up, the reduction of albumin and transferrin, the presence of jejunoileal bypass26. Many reported cases are related to prolonged vomiting, starvation and, more often, alcoholism26-28.
Vitamin B12
Vitamin B12 deficiency has been often reported following RYGB, with its incidence varying between 12% and 75%29-32. Low vitamin B12 levels can be seen at six months postoperatively, but they occur mostly at one year or more when liver storages is found to be depleted32. High prevalence of such a deficiency has also been reported ten years after the surgery33.
Regarding vitamin B12 absorption, it is important to remember that initially it needs to be liberated from the food source (particularly red meat).
The releasing is facilitated by the presence of gastric acid. Free vitamin B12 then binds to R-protein in the stomach and is cleaved in the duodenum to bind intrinsic factor (IF). The B12-IF complex circulates intact through the gastrointestinal tract to its absorption site (ileum). Marcuard et al.34 observed low IF levels in 53% of patients with vitamin deficiency after RYGB.
The frequent absence of symptoms in the presence of vitamin B12 deficiency and the irreversible neurologic damage risk13 require a careful decision about supplementing or not the vitamin in a preventive manner. Vitamin B12 is present in the nutritional composition of most multivitamins commercially available, however, the amounts vary widely.
Vitamina B12 deficiency is usually defined as levels below 200 pg/mL. However, about 50% of patients with clear deficiency signs and symptoms show normal levels35. Regarding prevention, a 350 mcg/day oral dose could prevent deficiency in 95% of patients32. and a 500 a 1,000 mcg/day dose has been used to treat the deficiency11,18.
Currently, B12 supplementation is also commercially available as a spray to be applied sublingually. This kind of supplementation is presented as nanoparticles to increase vitamin absorption and bioavailability. Although vitamin B12 deficiency occurs only after a few months from bariatric surgery, a good clinical practice has been preventively administering 1000 mg vitamin B12 parenterally over the preoperative period36.
Folic acid
Folic acid deficiency has been observed mainly after RYGB. It can manifest as macrocytic anemia, leukopenia, thrombocytopenia, glossitis, or megaloblastic bone marrow. Most of the time, folic acid deficiency occurs after bariatric surgery due to reduced intake and not resulting from poor absorption37.
Although less frequent than vitamin B12 deficiency, low levels of folic acid have been reported between 6% and 65% of patients undergoing RYGB29,38,39 and can easily be treated by oral supplementation37.
Folic acid absorption occurs preferably in the duodenum, but it can also occur along the entire small bowel length due to a physiological adaptation after surgery. Vitamin B12 is required to convert methyl-tetrahydrofolic acid (inactive) into tetrahydrofolic acid (active). Therefore, vitamin B12 deficiency can result from folic acid deficiency30,37.
In general, folic acid deficiency is treated with 1,000 mg/day of folic acid (orally) for one to two months40 and can be prevented with a supplement containing 200% the recommended daily value (800 mg/day). This level can also benefit the fetus in case of an unaware pregnancy in the post-operatory phase. A supplementation higher than 1,000 mg/day can "mask" a vitamin B12 deficiency diagnosis, thereof the importance of monitoring the vitamin blood levels mostly when high folic acid dose supplementation is adopted13.
Iron
Anemia can affect two-thirds of patients undergoing bariatric surgery, usually caused by iron deficiency. In patients undergoing RYGB, the deficiency ranges from 20% to 49%32,37,40. Among superobese patients, anemia is reported in 35-74% and iron deficiency can reach 52% in late postoperative period41.
In patients undergoing bariatric surgery, the amount of daily intake of elemental iron (ferrous sulfate or ferrous fumarate) should reach 40 to 100 mg/day although the long-term prophylactic treatment efficacy is unknown32.
The amount of elemental iron present in most commercial multivitamins is usually small (10 to 20 mg per tablet), which is considered insufficient to prevent iron deficiency in patients undergoing RYGB. The current recommendations include administering 40 to 65 mg elemental iron daily (200-400 mg ferrous sulphate). In women of childbearing age, the recommendations increase to 100 mg elemental iron daily (400 to 800 mg ferrous sulphate)10,35,42. Thus, the anemia clinical course, laboratory value changes, age, gender, and reproductive considerations should be analyzed.
On the other hand, iron deficiency treatment requires supplementation up to 300 mg/day, usually three to four tablets containing 50 to 65 mg elemental iron13. When treatment fails or in the presence of severe anemia, intravenous doses of an iron hydroxide-saccharose complex are required (20 mg elemental iron per mL)43,44.
Currently, commercially available multivitamins, mainly in the United States, lack iron in their composition to ensure that this replacement must be performed in isolation and at different times of day. It is important to considerer the different absorption characteristics of various iron supplementation types available in the market:
Ferrous fumarate: 33% elemental iron, usually well tolerated by patients and showing good mineral absorption.
Ferrous sulphate: only 20% elemental iron and showing larger gastrointestinal effects.
Ferronyl: 98% elemental iron. Elemental iron with reduced particles.
Ideally, the iron supplement should be accompanied by vitamin C and fruto-oligosaccharides to prevent constipation, improve intestinal flora, and provide better absorption of the mineral. Other important consideration is related to iron interaction with other elements, such as calcium and phytate45, and it is important to supplement it alone and in the fasting state. In addition, copper deficiency can cause anemia, with some authors recommending supplementation with 900 mg/day copper or an additional supplementation with 50 to 200 mg/day according to the surgical technique used.
Calcium and vitamin D
Calcium and vitamin D supplementation has been recommended in most weight loss therapies in order to prevent bone reabsorptioin46. The preferable way of supplementing has been widely discussed in clinical practice. In the presence of a less acid environment, such as the small stomach after a bariatric surgery, calcium carbonate absorption becomes impaired47.
A meta-analysis suggests calcium citrate is more bioavailable than calcium carbonate, around 22% to 27%48. In patients undergoing RYGB, calcium citrate (500 mg/day associated with 125 IU vitamin D3-cholecalciferol), demonstrated a greater increase in calcium serum levels and greater reduction in parathyroid hormone (PTH) than the same amounts of calcium carbonate supplemented49. PTH is the main regulator of calcium homeostasis in mammals and also acts in forming 1,25 (OH)2D, a metabolite responsible for almost all actions of vitamin D. High calcium levels inhibit PTH release, while low calcium levels leads to increased PTH release by parathyroid glads50. Furthermore, calcium absorption occurs in the bowel under vitamin D influence51.
A vitamin D deficiency after bariatric surgery has been reported among 50-80% of the cases14,52-54. Some studies demonstrated that over 50% of patients that show vitamin D deficiency after bariatric surgery used multivitamins containing 400-800 IU of vitamin D per day.14,52,53 Other studies found a postoperative supplementation with 1,200 mg/day calcium carbonate and 400 to 800 IU vitamin D3 (cholecalciferol) present in multivitamins/minerals was not enough to prevent high levels of PTH and bone reabsorption46,55,56. Thus, over 50% of patients undergoing RYGB showed calcium deficiency in the presence of that supplementation pattern57. However, increasing calcium citrate doses from 1000 mg to 1700/day (including 400 IU of vitamin D) could reduce bone loss even in the presence or weight loss58. Thus, the current calcium supplementation recommendation in the postoperative phase varies according to the surgical technique applied.
Regarding vitamin D, when a deficiency is present preoperatively, the supplementation with 5000 IU of oral cholecalciferol once a week for eight weeks is recommended59. Postoperatively, the same dose was not enough to treat vitamin D deficiency60. Thus, there is no appropriate dose for all patients undergoing bariatric surgery yet. However, doses as high as 5000 IU/day have been found safe and potentially required to treat the secondary hyperparathyroidism present in some patients. We suggest it is appropriate to start supplementation with 2000 IU/day of vitamin D postoperatively, preferably as vitamin D3 (cholecalciferol). Attention should be given to other factors such as patients taking anticonvulsants, glucocorticoids, heparin, or cholestyramine with a higher risk for bone disease.
Vitamin A and vitamin E
Yearly monitoring of liposoluble nutrients should be obtained after disabsorptive procedures. The recommendation of 50,000 IU of vitamin A every other week has been suggested to correct most deficiency cases19. In their study, Sugerman et al.61 reported that supplementation of 10,000 IU of vitamin A was sufficient to prevent any deficiency. Actually, the doses used in treating vitamin A deficiency vary according to the signs and symptoms presented. In the absence of corneal changes, the supplementation with 10,000 to 25,000 IU/day is recommended until there is clinical improvement of symptoms (normally between 1 and 2 weeks); in the presence of corneal changes, 50,000 to 100,000 IU/day (intramuscularly) for 2 weeks are required13. It is also important to assess iron and copper deficiency, as it can hamper the resolution of vitamin A deficiency.
Regarding vitamin E, there is no therapeutic recommendation considered ideal or clearly defined. The potential antioxidant effects of vitamin E can be achieved with supplementation of 100 to 400 IU/day13.
Proteins
Protein deficiency is the most often reported among macronutrientes. It is observed mainly after disabsorptive or mixed surgical techniques (DBP/DS and RYGB)13. Only 57% of the ingested protein is estimated to be absorbed after bowel bypass10,62.
The hypoalbuminemia (albumin < 3.5 g/dL) after RYGB may vary from 13% two years after the surgery63 to 27.9% after ten years33 or it might even be absent in the first months64-66.
Some experts recommend 70 g/day of protein during caloric restriction to lose weight67. However, many bariatric surgery programs recommend 60 to 80 g/day of protein or 1.0 to 1.5 g/kg of optimum body weight, although the exact requirements have not been defined yet. The patient should be instructed to use high biological value powder protein supplements 48 hours after the surgery.
Meat, poultry, fish, eggs, milk and dairy should be encouraged still in the first postoperative months according to the diet evolution protocol. Protein intake should be periodically evaluated in each nutritional visit. In the presence of clinical or subclinical protein deficiency, even in the absence of vomiting or food intolerance, the patients must be treated with hyperproteic diet68.
Protein modules are widely available on the market. However, factors such as flavor, texture, solubilization, absorption, and cost are considered important when choosing the supplements. The amine acid profile should be given priority when the supplement is the only protein source in the diet. Whey protein can be an excellent choice, since it has high level of branched-chain amine acids, which are important to prevent muscle tissue degradation, remain stable in the stomach, are rapidly digested, and lactose-free. Currently, there is a hydrolyzed whey protein product which reduces allergenicity and improves absorption.
Conclusion
There are no absolutely appropriate recommendations to prevent or treat most nutritional deficiencies after bariatric surgery yet; however, it is clear that preventive supplementation has been increasingly important in this setting.
Many factors are involved in causing such deficiencies. Even before any surgical intervention, obesity can be associated with subclinical nutritional deficiencies that could be aggravated after the anatomical and physiological changes caused in gastrointestinal tract. In addition, there is a limitation and/or change in the dietary intake. Therefore, nutritional supplementation becomes a necessary alternative therapy, contributing to weight loss in a healthy manner and, in most cases, it should be evaluated individually.
The preventive use of multivitamins/minerals should compound the care protocol in all patients undergoing bariatric surgery, mainly in those undergoing techniques involving a certain degree of dysabsorption. The treatment of these patients' nutritional deficiencies should consider micronutrient megadoses due to lower bioavailability resulting from physiological changes provided by the surgical techniques. Further studies are required to establish an effective dose to treat nutritional deficiencies following bariatric surgery.
Acknowledgements
The authors thank the Fundação de Amparo à Pesquisa do Estado do Maranhão (FAPEMA), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and the Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
References
- 1. Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, Fahrbach K, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004; 292(14):1724-37.
- 2. Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000; 72(3):690-3.
- 3. Snijder MB, van Dam RM, Visser M, Deeg DJH, Dekker JM, Bouter LM, et al. Adiposity in Relation to Vitamin D Status and Parathyroid Hormone Levels: A Population-Based Study in Older Men and Women. J Clin Endocrinol Metab. 2005; 90(7):4119-23.
- 4. Botella-Carretero JI, Alvarez-Blasco F, Villafruela JJ, Balsa JA, Vázquez C, Escobar-Morreale HF. Vitamin D deficiency is associated with the metabolic syndrome in morbid obesity. Clin Nutr. 2007; 26(5):573-80.
- 5. Ribot J, Felipe F, Bonet ML, Palou A. Changes of adiposity in response to vitamin a status correlate with changes of PPAR [gamma] 2 expression. Obesity. 2001; 9(8):500-9.
- 6. Zulet M, Puchau B, Hermsdorff H, Navarro C, Martinéz J. Vitamin A intake is inversely related with adiposity in healthy young adults. J Nutr Sci Vitaminol. 2008; 54(3):347-52.
- 7. Lee RG, Rains TM, Tovar-Palacio C, Beverly JL, Shay NF. Zinc deficiency increases hypothalamic neuropeptide Y and neuropeptide Y mRNA levels and does not block neuropeptide Y-induced feeding in rats. J Nutr. 1998; 128(7):1218-23.
- 8. Chen M-D, Lin P-Y. Zinc-Induced hyperleptinemia relates to the amelioration of sucrose-induced obesity with zinc repletion. Obes Res. 2000; 8(7):525-9.
- 9. Ozata M, Mergen M, Oktenli C, Aydin A, Yavuz Sanisoglu S, Bolu E, et al. Increased oxidative stress and hypozincemia in male obesity. Clin Biochem. 2002; 35(8):627-31.
- 10. Parkes E. Nutritional management of patients after bariatric surgery. Am J Med Sci. 2006; 331(4):207-13.
- 11. Shikora SA, Kim JJ, Tarnoff ME. Nutrition and gastrointestinal complications of bariatric surgery. Nutr Clin Pract. 2007; 22(1):29-40.
- 12. Hydock C. A brief overview of bariatric surgical procedures currently being used to treat the obese patient. Crit Care Nurs. 2005; 28(2):217-26.
- 13. Aills L, Blankenship J, Buffington C, Furtado M, Parrott J. ASMBS Allied Health Nutritional Guidelines for the Surgical Weight Loss Patient. Surg Obes Relat Dis. 2008; 4(5 Suppl):S73-108.
- 14. Slater G, Ren C, Siegel N, Williams T, Barr D, Wolfe B, et al. Serum fat-soluble vitamin deficiency and abnormal calcium metabolism after malabsorptive bariatric surgery. J Gastrointest Surg. 2004; 8(1):48-55.
- 15. Kasper DL, Braunwald E, Hauster S,Longo D, Jameson JL, Fauci AS. Harrisons principles of internal medicine. Disorders of vitamin and mineral metabolism: identifying vitamin deficiencies. 16th ed. Berkshire: Mcgraw Hill; 2006.
- 16. Kumpf VJ, Slocum K, Binkley J, Jensen G. Complications after bariatric surgery: survey evaluating impact on the practice of specialized nutrition support. Nutr Clin Pract. 2007; 22(6):673-8.
- 17. Mechanick J, Kushner R, Sugerman H, Gonzalez-Campoy M, Collazo-Clavell M, Guven S, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery. Medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Endocr Pract. 2008; 4(1):109-84.
- 18. Brolin RE, Gorman JH, Gorman RC, Petschenik AJ, Bradley LJ, Kenler HA, et al. Are vitamin B12 and folate deficiency clinically important after Roux-en-Y gastric bypass? J Gastrointest Surg. 1998; 2(5):436-42.
- 19. Ledoux S, Msika S, Moussa F, Larger E, Boudou P, Salomon L, et al. Comparison of nutritional consequences of conventional therapy of obesity, adjustable gastric banding, and gastric bypass. Obes Surg. 2006; 16(8):1041-9.
- 20. Scopinaro N, Adami GF, Marinari GM, Gianetta E, Traverso E, Friedman D, et al. Biliopancreatic diversion. World J Surg. 1998; 22(9):936-46.
- 21. Juhasz-Pocsine K, Rudnicki SA, Archer RL, Harik SI. Neurologic complications of gastric bypass surgery for morbid obesity. Neurology. 2007; 68(21):1843-50.
- 22. Claudio Lopes Chaves L, Faintuch J, Kahwage S, de Assis Alencar F. A cluster of polyneuropathy and Wernicke-Korsakoff syndrome in a bariatric unit. Obes Surg. 2002; 12(3):328-34.
- 23. Chang C, Adams-Huet B, Provost D. Acute Post-Gastric Reduction Surgery (APGARS) Neuropathy. Obes Surg. 2004; 14(2):182-9.
- 24. Thiamin. The Linus Pauling Institute Micronutrient Information Center. [cited 2010 sept 20]. Available from: http://lpi.oregonstate.edu/infocenter/vitamins/thiamin/index.html
- 25. Alves LFA, Gonçalves RM, Cordeiro GV, Lauria MW, Ramos AV. Beribéri pós bypass gástrico: uma complicação não tão rara. Relato de dois casos e revisão da literatura. Arq Bras Endocrinol Metab. 2006; 50:564-8.
- 26. Thaisetthawatkul P, Collazo-Clavell ML, Sarr MG, Norell JE, Dyck PJB. A controlled study of peripheral neuropathy after bariatric surgery. Neurology. 2004; 63(8):1462-70.
- 27. Gollobin C, Marcus W. Bariatric beriberi. Obes Surg. 2002; 12(3):309-11.
- 28. Nautiyal A, Singh S, Alaimo DJ. Wernicke encephalopathy-an emerging trend after bariatric surgery. Am J Med. 2004; 117(10):804-5.
- 29. MacLean LD, Rhode BM, Shizgal HM. Nutrition following gastric operations for morbid obesity. Ann Surg. 1983; 198(3):347-55.
- 30. Halverson JD. Micronutrient deficiencies after gastric bypass for morbid obesity. Am Surg. 1986; 52(11):594-8.
- 31. Rhode BM, Arseneau P, Cooper BA, Katz M, Gilfix BM, MacLean LD. Vitamin B-12 deficiency after gastric surgery for obesity. Am J Clin Nutr. 1996; 63(1):103-9.
- 32. Brolin RE, Gorman JH, Gorman RC, Petschenik AJ, Bradley LJ, Kenler HA, et al. Are vitamin B12 and folate deficiency clinically important after roux-en-Y gastric bypass? J Gastrointest Surg. 1998; 2(5):436-42.
- 33. Ho T, et al. Long-term results after laparoscopic roux-en-Y gastric bypass: 10-year follow-up. Surg Obes Relat Dis 2009; 5:Abstract PL-211.
- 34. Marcuard SP, Sinar DR, Swanson MS, Silverman JF, Levine JS. Absence of luminal intrinsic factor after gastric bypass surgery for morbid obesity. Dig Dis Sci. 1989; 34(8):1238-42.
- 35. Malinowski SS. Nutritional and metabolic complications of bariatric surgery. Am J Med Sci. 2006; 331(4):219-25.
- 36. Shankar P, Boylan M, Sriram K. Micronutrient deficiencies after bariatric surgery. Nutrition. 2010; 26(11-12):1031-7.
- 37. Amaral JF, Thompson WR, Caldwell MD, Martin HF, Randall HT. Prospective hematologic evaluation of gastric exclusion surgery for morbid obesity. Ann Surg. 1985; 201(2):186-93.
- 38. Boylan LM, Sugerman HJ, Driskell JA. Vitamin E, vitamin B-6, vitamin B-12, and folate status of gastric bypass surgery patients. J Am Diet Assoc. 1988; 88(5):579-85.
- 39. Dixon JB, Dixon ME, OBrien PE. Elevated homocysteine levels with weight loss after Lap-Band surgery: higher folate and vitamin B12 levels required to maintain homocysteine level. Int J Obes Relat Metab Disord. 2001; 25(2):219-27.
- 40. Brolin RE, Gorman RC, Milgrim LM, Kenler HA. Multivitamin prophylaxis in prevention of post-gastric bypass vitamin and mineral deficiencies. Int J Obes. 1991; 15(10):661-7.
- 41. Brolin RE, LaMarca LB, Kenler HA, Cody RP. Malabsorptive gastric bypass in patients with superobesity. J Gastrointest Surg. 2002; 6(2):195-203; discussion 4-5.
- 42. Fujioka K. Follow-up of nutritional and metabolic problems after bariatric surgery. Diabetes Care. 2005; 28(2):481-4.
- 43. Brolin RE, Gorman JH, Gorman RC, Petschenik AJ, Bradley LB, Kenler HA, et al. Prophylactic iron supplementation after Roux-en-Y gastric bypass: a prospective, double-blind, randomized study. Arch Surg. 1998; 133(7):740-4.
- 44. Seema V, Walid B, Edgard B, Fadi N, Heather M, Jeffrey N, et al. Need for parenteral iron therapy after bariatric surgery. Surg Obes Relat Dis. 2008; 4(6):715-9.
- 45. Lobo AS, Tramonte VLC. Efeitos da suplementação e da fortificação de alimentos sobre a biodisponibilidade de minerais. Rev Nutr. 2004; 17(1):107-13.
- 46. Coates PS, Fernstrom JD, Fernstrom MH, Schauer PR, Greenspan SL. Gastric bypass surgery for morbid obesity leads to an increase in bone turnover and a decrease in bone mass. J Clin Endocrinol Metab. 2004 ; 89(3):1061-5.
- 47. Recker RR. Calcium absorption and achlorhydria. N Engl J Med. 1985; 313(2):70-3.
- 48. Sakhaee K, Bhuket T, Adams-Huet B, Rao DS. Meta-analysis of calcium bioavailability: a comparison of calcium citrate with calcium carbonate. Am J Ther. 1999; 6(6):313-21.
- 49. Tondapu P, Provost D, Adams-Huet B, Sims T, Chang C, Sakhaee K. Comparison of the absorption of calcium carbonate and calcium citrate after Roux-en-Y gastric bypass. Obes Surg. 2009; 19(9):1256-61.
- 50. Oliveira JHAd, Bracco OL, Kayath M, Guarniero R. Teriparatida (PTH[1-34]rh): uma nova perspectiva no tratamento da osteoporose. Acta Ortop Bras. 2003; 11(1):184-9.
- 51. Moreira RO, Duarte MPC, Farias MLF. Distúrbios do eixo calcio-PTH-vitamina D nas doenças hepáticas crônicas. Arq Bras Endocrinol Metab. 2004; 48(4):443-50.
- 52. Newbury L, Dolan K, Hatzifotis M, Low N, Fielding G. Calcium and vitamin D depletion and elevated parathyroid hormone following biliopancreatic diversion. Obes Surg. 2003; 13(8):893-5.
- 53. Ybarra J, Sánchez-Hernández J, Gich I, De Leiva A, Rius X, Rodríguez-Espinosa J, et al. Unchanged hypovitaminosis D and secondary hyperparathyroidism in morbid obesity after bariatric surgery. Obes Surg. 2005; 15(3):330-5.
- 54. Johnson JM, Maher JW, DeMaria EJ, Downs RW, Wolfe LG, Kellum JM. The long-term effects of gastric bypass on vitamin D metabolism. Ann Surg. 2006; 243(5):701-5.
- 55. Pugnale N, Giusti V, Suter M, Zysset E, Heraief E, Gaillard RC, et al. Bone metabolism and risk of secondary hyperparathyroidism 12 months after gastric banding in obese pre-menopausal women. Int J Obes Relat Metab Disord. 2003; 27(1):110-6.
- 56. Goode LR, Brolin RE, Chowdhury HA, Shapses SA. Bone and gastric bypass surgery: effects of dietary calcium and vitamin D. Obes Res. 2004; 12(1):40-7.
- 57. Riedt CS, Brolin RE, Sherrell RM, Field MP, Shapses SA. True fractional calcium absorption is decreased after Roux-en-Y gastric bypass surgery. Obesity. 2006; 14(11):1940-8.
- 58. Riedt CS, Cifuentes M, Stahl T, Chowdhury HA, Schlussel Y, Shapses SA. Overweight postmenopausal women lose bone with moderate weight reduction and 1 g/day calcium intake. J Bone Miner Res. 2005; 20(3):455-63.
- 59. Flancbaum L, Belsley S, Drake V, Colarusso T, Tayler E. Preoperative nutritional status of patients undergoing Roux-en-Y gastric bypass for morbid obesity. J Gastrointest Surg. 2006; 10(7):1033-7.
- 60. Goldner W, Stoner J, Lyden E, Thompson J, Taylor K, Larson L, et al. Finding the optimal dose of vitamin D following Roux-en-Y gastric bypass: a prospective, randomized pilot clinical trial. Obes Surg. 2009; 19:173-9.
- 61. Sugerman H, Kellum J, DeMaria E. Conversion of proximal to distal gastric bypass for failed gastric bypass for super obesity. J Gastrointest Surg. 1997; 1(6):517-25.
- 62. Mango VL, Frishman WH. Physiologic, psychologic, and metabolic consequences of bariatric surgery. Cardiol Rev. 2006; 14(5):232-7
- 63. Brolin R, LaMarca L, Kenler H, Cody R. Malabsorptive gastric bypass in patients with superobesity. J Gastrointest Surg. 2002; 6(2):195-205.
- 64. Skroubis G, Sakellaropoulos G, Pouggouras K, Mead N, Nikiforidis G, Kalfarentzos F. Comparison of nutritional deficiencies after Roux-en-Y gastric bypass and after biliopancreatic diversion with Roux-en-Y gastric bypass. Obes Surg. 2002; 12(4):551-8.
- 65. Brolin RE, Kenler HA, Gorman JH, Cody RP. Long-limb gastric bypass in the superobese. A prospective randomized study. Ann Surg. 1992; 215(4):387-95.
- 66. Skroubis G, Anesidis S, Kehagias I, Mead N, Vagenas K, Kalfarentzos F. Roux-en-Y gastric bypass versus a variant of biliopancreatic diversion in a non-superobese population: prospective comparison of the efficacy and the incidence of metabolic deficiencies. Obes Surg. 2006; 16(4):488-95.
- 67. Mahan L, Escott-Stump S. Medical nutrition therapy for anemia: Krause's food, nutrition, and diet therapy. 10th ed. Philadelphia: Saunders; 2000.
- 68. Mason EE. Starvation injury after gastric reduction for obesity. World J Surg. 1998; 22(9):1002-7.
Bariatric surgery: how and why to supplement
Publication Dates
-
Publication in this collection
25 Feb 2011 -
Date of issue
Feb 2011
History
-
Accepted
12 Oct 2010 -
Received
09 Aug 2010