Abstracts
C-reactive protein (CRP) is an acute-phase protein whose requests have been growing exponentially in several countries, including Brazil. In this study, the use of CRP in several clinical situations was reviewed by a group of physicians comprised by specialists in internal medicine, medical emergencies, intensive care, screening, and laboratory medicine, aiming to analyze the applicable literature and to propose guidelines for a more rational use of this laboratory test. The result was the creation of flowcharts guiding CRP request, adjusted to four different healthcare environments, namely, intensive care units, emergency room, wards, and outpatient clinics. These flowcharts, as well as a more detailed discussion on several clinical recommendations for the test, are presented in this study.
CRP; C-reactive protein; Laboratory tests; Clinical use
A proteína C reativa (PCR) é uma das proteínas de fase aguda cuja solicitação tem crescido de forma exponencial em vários países, incluindo o Brasil. Neste estudo, a utilidade da PCR em diversas situações clínicas foi revisada por um grupo de médicos composto por especialistas em Medicina Interna, Emergências Médicas, Terapia Intensiva, Rastreamento e Medicina Laboratorial com o objetivo de analisar a literatura pertinente e propor diretrizes para o uso mais racional desse exame laboratorial. O resultado foi a criação de fluxogramas orientadores da solicitação de PCR adaptados a quatro ambientes assistenciais diferentes, sendo eles unidades de terapia intensiva, pronto-socorro, enfermarias e ambulatórios. Esses fluxogramas e uma discussão mais detalhada sobre as diversas indicações clínicas do exame são apresentados neste estudo.
Proteína C reativa; Exames laboratoriais; Uso clínico
REVIEW ARTICLE
C-reactive protein: clinical applications and proposals for a rational use*
Francisco J.B. AguiarI; Mario Ferreira-JúniorII; Maria M. SalesIII; Luiz M. Cruz-NetoI; Luiz A.M. FonsecaIV; Nairo M. SumitaIII; Nilo J.C. DuarteIII; Arnaldo LichtensteinII; Alberto J.S. DuarteIII
IClinical Emergency Assistance, Hospital das Clínicas, Medical School, Universidade de São Paulo (USP), São Paulo, SP, Brazil
IIGeneral Practice and Propaedeutics, Hospital das Clínicas, Medical School, USP, São Paulo, SP, Brazil
IIICentral Laboratory Division-LIM03, Hospital das Clínicas, Medical School, USP, São Paulo, SP, Brazil
IVImmunology Department, Hospital das Clínicas, Medical School, USP, São Paulo, SP, Brazil
Corresponding author at
ABSTRACT
C-reactive protein (CRP) is an acute-phase protein whose requests have been growing exponentially in several countries, including Brazil. In this study, the use of CRP in several clinical situations was reviewed by a group of physicians comprised by specialists in internal medicine, medical emergencies, intensive care, screening, and laboratory medicine, aiming to analyze the applicable literature and to propose guidelines for a more rational use of this laboratory test. The result was the creation of flowcharts guiding CRP request, adjusted to four different healthcare environments, namely, intensive care units, emergency room, wards, and outpatient clinics. These flowcharts, as well as a more detailed discussion on several clinical recommendations for the test, are presented in this study.
Keywords: CRP; C-reactive protein; Laboratory tests; Clinical use
Clinical use of C-reactive protein and the erythrocyte sedimentation rate
C-reactive protein (CRP) is one of the acute-phase proteins (APPs), which are those whose serum level increases or decreases by at least 25% during inflammatory conditions. However, despite the name, they can also change during chronic inflammatory processes. Perrakos and Vincent identified 3,370 references, including clinical and experimental studies of 178 different APPs used as sepsis biomarkers.1 Nonetheless, there are only two tests based on APPs measurement widely used today: erythrocyte sedimentation rate (ESR) and CRP.
ESR, which is the rate at which erythrocytes fall through plasma, depends on the concentration of fibrinogen (which is an APP), and is an indirect measure of this concentration. It is influenced by the shape, size, and number of erythrocytes, as well as by other plasma components, such as immunoglobulins. This may result in inaccuracy and error.2
CRP was discovered in 1930 and received this name because it reacted with the C-polysaccharide of pneumococcus in the acute phase of pneumococcal pneumonia. CRP measurement is, therefore, a direct determination of an APP and, in the presence of inflammatory conditions, its serum levels change rapidly and its variation is wider than that of ESR. During postoperative periods, it shows sensitivity to detect complications higher than increases in ESR, leukocytes, heart rate, or fever.3 Unlike ESR, CRP measurement does not change in the presence of anemia, polycythemia, spherocytosis, macrocytosis, congestive heart failure, or hypergammaglobulinemia.3 These characteristics are increasing CRP use in place of ESR, despite greater experience and familiarity with the latter. None of the tests are typically useful when assessing conditions with vague clinical presentation, although they are frequently used in this context; in any case, they should not be used to screen inflammation in asymptomatic individuals (possible exception: risk stratification for cardiovascular disease). In the presence of suggestive clinical evidence, it can be useful to screen for inflammatory conditions, however, without accurately distinguishing the etiologic mechanism. Increases occurr not only in infections, but also in the presence of systemic inflammation caused by rheumatoid arthritis, myocardial infarction, necrotizing pancreatitis, multiple trauma, neoplasias, vasculitis, and even possibly in some cases of serotonin syndrome, only to mention some conditions.
Often, CRP and ESR are used to establish baselines and subsequently to monitor the evolution of infectious, autoimmune, and other diseases.
Dynamics of C-reative protein
CRP is predominantly secreted by the liver and starts four to six hours after the stimulus; it duplicates every eight hours, and peaks within 36 to 50 hours. CRP has a plasma half-life of 19 hours, and even after a single stimulus, as in a trauma or surgery, it may take several days to return to the baselines.4 For this reason, serial measurements over several days are more useful than isolated results.5 Thus, it is possible to note CRP's limitations for monitoring of critical patients, as its level can be low or normal in the first 12 hours of fever in infectious processes. Conversely, due to its long half-life, it may remain high during the initial recovery phase, although some authors suggest that non-reduction after 48 to 72 hours of treatment or postoperative period requires a re-evaluation.4,5
Clinical conditions and change profiles
Generally, mild inflammations and viral infections lead to increases to the range of 10 to 40 mg/L, while more severe inflammations and bacterial infections lead to serum levels between 40 to 200 mg/L.6 In the present study, concentrations of CRP are expressed in mg/L, but they can also be expressed in mg/dL. There are studies evidencing that a serum level of 100 mg/L would have a sensitivity of 80% to 85% for bacterial infection;2 however, severe viral infections may also result in increases of the serum level.5
Some authors suggest 50 to 100 mg/L as an optimal serum level to separate sepsis from systemic inflammatory response syndrome (SIRS).4 Povoa7 evidenced that a cutoff serum level of 50 mg/L increases the chance of sepsis by four-fold. Pierrakos,1 however, did not recommend the use of CRP to separate sepsis from inflammatory conditions, deeming it inaccurate for this purpose. The problem is not only the dynamics of CRP variations, already mentioned, but also the lack of a "gold standard" for the diagnosis of sepsis, which is defined by the association between clinical and laboratory data. In general, this makes the determination of biomarkers' sensitivity and specificity harder in this clinical condition. In fact, some studies adopt culture-positive results as a gold standard, which is also questionable, as cases of culture-negative sepsis1 are frequent.
Also widely used in monitoring rheumatic diseases, CRP has the specific characteristic of not showing any increase with the activity of systemic lupus erythematous, except in the presence of serositis,8 chronic polyarthritis, or vasculitis with tissue infarction.9 In the absence of these characteristics, an increase suggests infection, and ESR should be chosen to detect the activity of the disease. Discrepancies like these are not rare among the variations of these active phase evidences; this is expected, as cytokines influence APP synthesis by hepatocytes, and serum levels of cytokines and other modulators of inflammatory responses vary pursuant to the disease and stage of clinical evolution. Other situations in which CRP may remain between 10 and 20 mg/L or even not increase are scleroderma, dermatomyositis, and ulcerative colitis.5
It can be concluded that there is not a single test to detect inflammation, and multiple measurements of CRP and ESR are frequently used. The interpretation will take into account several factors, among them the time profile of variations and the clinical context.
Currently, there is a high-sensitivity method (HS) for measurement of CRP concentrations. It measures CRP exactly the same as the conventional test, but is capable of detecting much lower CRP concentrations (detection limit of 0.03 mg/L). The main practical consequence of the new methodology was expressed in the JUPITER study (Justification for the Use of Statins in Primary Prevention: an Intervention Trial Evaluating Rosuvastatin) published in 2008.10 This interventional trial followed almost 18,000 individuals and observed that statins reduced infarctions and cerebrovascular accidents in individuals without any heart disease or hypercholesterolemia, but with changes in serum level obtained through HS-CRP. Regardless of controversies regarding the amount of evidence, HS-measurement has been used since then to support the decision to use statins in primary prevention. The pharmaceutical company that manufactures rosuvastatin financed the study, and its main author is connected to the laboratory, in addition of holding patents related to the use of inflammatory biomarkers to treat heart diseases, including the use of the HS method for cardiovascular risk assessment.9
The HS method has also been used to prognosticate stable coronary disease and acute coronary syndrome.11-18 However, these results are being questioned.19
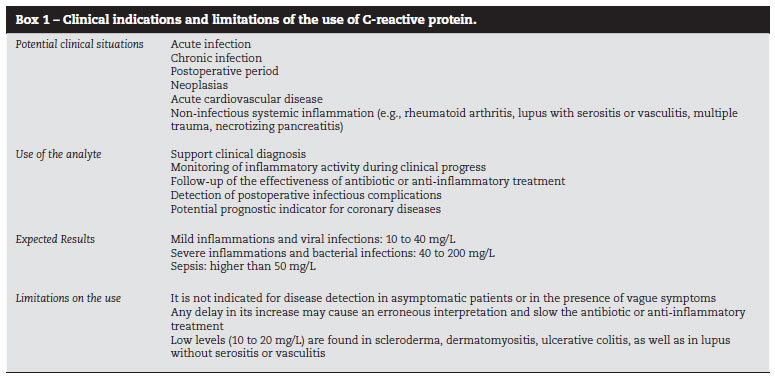
These data show that the measurement of CRP can be useful to the physician if wisely requested; they also show that knowledge of CRP dynamics, as well as its limitations, is critical for the interpretation of its results. Clinical indications for the use of CRP, as well as some limitations, can be found in Box 1.
Healthcare singularities of intensive care units (ICUs), wards, emergency rooms (ERs), and general outpatient clinics
ICUs, wards, ERs, and outpatient clinics are different environments, serving a spectrum ranging from critical patients in an ICU to healthy individuals seeking an outpatient clinic for medical check-ups. The prevalence and severity of diseases differ greatly among these places. This fact has consequences on requests for tests and their interpretation, e.g.: the lower the probability of the disease, the higher will be the probability for a positive test to be a false positive, a frequent situation in asymptomatic outpatients. Inversely, in patients presenting serious conditions with a high probability of comorbidities, a negative test has a higher probability of being a false negative. These principles are applied to the interpretation of any test (except in the unusual event of a test with sensitivity and/or specificity of 100%).
Serial measurement (at minimum time intervals of 24 hours) should be restricted to critically ill patients. Some of these patients are in coma and/or on mechanical ventilation, i.e., with conditions that make clinical evaluation harder; in this environment, the increased risk of infections associated with procedures and clinical conditions justifies this initiative.
Even with the limitations mentioned above, in the Hospital das Clínicas, Medical School, Universidade de São Paulo, in São Paulo, a tertiary level hospital comprising several environments, such as outpatient clinics, wards, ICUs and an ER, the number of CRP requests jumped from 50,365 in 2006 to 254,817 in 2011, representing an increase of 405%. The highest annual relative increase (70%) occurred between 2006 and 2007, before the publication of the JUPITER study, whose recommendations led to an increase in the HS-CRP measurement method. The highest number of CRP requests occurs in the ER and ICUs. Part of this increase is not supported by a proper clinical indication and this entails increasing costs, with no benefits to the patients.
A study by Santos et al., regarding CRP requests in an ER of a university hospital, where a significant increase was also verified, found that 25% of the requests were related to the diagnostic investigation of pneumonia, and 13.5% were related to investigation of fever.20
Justifications and objectives
Considering that the number of requests for serum measurement of CRP is proving to be excessive and often inappropriate, resulting in distress and risks to patients, in addition to increasing costs, it was decided to perform this study, whose objectives are to contribute to:
Improve the quality of care provided to patients by reducing the distress caused by blood collections, by reducing the chance of false positive results, and by limiting any mistaken diagnostic and/or therapeutic consequences.
Improve medical knowledge, by offering guidelines regarding the indications for CRP requests, and reducing excessive requests in order to make this practice more reasonable and effective.
Reduce laboratory expenses with this analyte, allowing for the implementation of other diagnostic parameters, including those evidencing inflammation and infection.
Method and procedure
In September 2010, the Central Laboratory Division (Divisão de Laboratório Central -DLC) of the HC-FMUSP gathered a multidisciplinary group of specialists in internal medicine, medical emergencies, intensive care, outpatient clinic, and laboratory medicine aiming at studying ways to improve the pattern of requests for laboratory tests and, thus, try to avoid or mitigate risks associated with their inappropriate use, such as, e.g.: spoliation of patient; overdiagnosis; mistaken diagnoses (false positive and false negative); overtreatment; patient depression or anxiety; poor cost-effective methods; and waste of financial resources.
Coordinated by the Director of the DLC, eight physicians were invited - all working at HC-FMUSP, with experience in assisting patients in their respective areas, and with the support of three residents in internal medicine and laboratory medicine- to prepare the "Rational Use of Clinical Laboratory" project. As part of the project development, the group met on a weekly basis, from January to December, 2011, to analyze studies, recommendations, and guidelines published in the national and international scientific literature, and to discuss and establish practical criteria involving the request, at first, for the following laboratory tests: 1) HS and regular CRP; 2) ionic and total calcium; 3) thyroid-stimulating hormone (TSH, and free T4); 4) vitamin D; 5) blood cultures for aerobic and anaerobic microorganisms. The tests above were chosen because they are among the most requested in the HC-FMUSP, being part of curve A, which comprises laboratory tests whose sum corresponds to 80% of the DLC's demand. However, the purpose of this study was only to analyze and establish flowcharts to guide the rational use of high-sensitivity CRP or conventional CRP, leaving other tests mentioned above, also studied by this group, for later considerations.
Thus, the study was based on publications regarding the measurements of CRP through conventional methods and HS, directed to:
Clinical practice in the contexts of urgent care, emergency, ward, and ambulatory medicine; medical assistance; or preventive medicine;
Undergraduate and postgraduate medical schools;
Analysis of the financial impact of the tests requested.
It was a non-systematic review of the literature, in which the following keywords were used: C-reactive protein, high-sensitivity C-reactive protein, infection, inflammation, coronary disease. The 76 studies chosen were divided among the participants of the groups, and were presented and discussed during the weekly two-hour meetings, while their findings were recorded and systematized by the resident in laboratory medicine.
The decision flowchart was the manner by which the group decided to consolidate and present the results of its work. The reasons that led to such decision were: a) ease of viewing the situations in which CRP requests are indicated, and those in which its repetition is allowed/recommended; b) adaptation for use in different medical contexts (ICU, ER, ward, outpatient clinic); c) potential improvement or detailing based on basic clinical situations, both general and specific, in a single flowchart; d) dynamism and explanatory potential, which allows for the inclusion of alerts, electronically blocking unnecessary repetitions. Additionally, the decision flowchart, which summarizes both the formal scientific knowledge accumulated and published and the clinical experience of the participants in the working group, may facilitate dialogue with personnel of other areas also involved in the test request, such as, e.g., information technology (IT), management, operational, and cost control departments of the clinical laboratory itself.
The drawing of each step of the flowchart was carefully planned, analyzed, and discussed by the group, and the definition of its current format, presented herein, corresponds to the internal consensus resulting from the analysis of available scientific evidence based on the clinical practice of all participants.
The value of the experiences based on evidences20,21 and the establishment of guidelines22 in order to rationalize and eventually reduce unnecessary test requests is demonstrated in some studies. Thus, by acting in a teaching hospital, in addition to exploring the teaching potential of flowcharts, the group sought to associate its implementation with discussions regarding the use and interpretation of CRP with undergraduate students, residents, and medical staff.
Results and comments
Figs. 1 and 2 present the decision flowcharts for CRP requests in several contexts of medical assistance: ICU, ER, ward, and outpatient clinic.
Fig. 1 shows the recommendations for measurement in ICU patients. Considering the clinical vulnerability of some of these patients and the risks associated with certain procedures, daily CRP measurement may be useful for the complementary diagnosis of acute infections. Monitoring of its daily curve (at minimum time intervals of 24 hours), with verification of a trend of reduction or increase, provided additional data to the daily clinical evaluation of the patient. Measurement should not be performed in intervals shorter than 24 hours. HS-measurement is never indicated for evaluation of a potential infectious complication.
Recently, HS-CRP measurement was suggested as a prognostic indicator of cardiac outcomes in individuals with stable coronary disease (SCD) or acute coronary syndrome (ACS); however, current scientific evidences are not enough to recommend it as a way to determine the application of specific therapies for ACS or for secondary prevention of coronary events, which makes its request questionable in such cases.23
The situations in which CRP measurement may be useful in an ER context are indicated in Fig. 1. Much has been published regarding CRP in ERs; however, there are few evidences of its value in this environment.24-27 This analysis will be assessed in the specific situations in which it was studied:
Non-traumatic abdominal pain: in 2007, Bundy et al.28 published a literature review regarding diagnostic methods for acute appendicitis in children. The CRP value was classified as inconsistent. Retrospective studies, such as those by Chen and Wang29 and by Wu et al.,30 analyzed CRP cutoff values versus surgical findings, showing a good correlation; however, these publications did not addressed CRP as a variable for surgical indication. In adults, other diagnoses in addition to appendicitis may be the cause of inflammatory acute abdomen, such as uncomplicated diverticulitis without surgical indication. It can be concluded that medical history, physical examination, and imaging methods are more relevant diagnostic procedures in this clinical condition. If CRP measurement is chosen, the daily curve evolution must also be interpreted.
As a predictor of mortality: for patients presenting apparent severity criteria, initial CRP followed by daily curve represents an additional index among others already studied. We note that, in this work, CRP is not studied as a discriminative factor for hospitalization, but as a prognostic factor in populations where the hospitalization decision has already been taken; nevertheless, the study by Lee et al.8 shows that CRP underperforms the clinical score.
Pneumonia: although included in guidelines for evaluation of patients with community-acquired pneumonia, CRP value as a discriminative factor of essential specific decisions, e.g., hospitalization versus home care, was not satisfactorily studied. It is worth noting that this criterion still contemplates a clinical score. Gonzales et al.9 evaluate the use of CRP regarding the physician's decision to prescribe antibiotics for patients complaining about acute cough; their finding was that the use of CRP did not affect this decision. Once again, the suggestion of this study is that CRP should be requested for patients with pneumonia that will be hospitalized pursuant to traditional decision criteria. It is worth mentioning that the diagnosis of pneumonia requires imaging tests.
Patient with fever, with no defined focus: Lee et al.31,32 pointed out the need to understand the dynamics of CRP when evaluating its results; hence, patients with early fever symptoms for less than 12 hours may present low CRP values; this does not mean a non-severe condition. In these circumstances, the overestimation of laboratory results may result in error. As already mentioned, the clinical score provides better performance when evaluating severity, in comparison with CRP value alone.
Finally, it is suggested that the use of CRP measurement in ERs is reserved for acute infectious syndromes showing clinical indication for hospitalization.
For inpatients in medical wards (Fig. 2), especially in the stage of diagnostic investigation of a systemic inflammatory disease or unidentified acute infection (e.g., fever of unknown origin), with or without identifiable risk factors (e.g., risk for aspiration through airways or central vascular catheter), daily repetition of the measurement may be useful, especially while the clinical condition is undefined or unstable. In cases of definition of a diagnosis or when the patient is stable, repetition should either be suppressed or its frequency reduced at the assistant physician's discretion. In the situations mentioned above, HS-CRP measurement method is not justified.
The admission, in medical wards, of patients with a previously known condition of stable coronary disease also does not justify, by itself, the indication of HS-measurement.23
Finally, Fig. 2 summarizes the clinical situations in which CRP measurement is indicated as part of a diagnostic investigation or long-term follow-up of a known disease in an outpatient clinic. In cases of strong suspicion of a systemic inflammatory disease or acute or chronic infection, high CRP is an unspecific complementary indicator of the disease; however, based on current knowledge, it is not possible to define standards capable of specifically differentiating between inflammatory and infectious diseases, nor between bacterial and viral diseases5 (Box 1). In cases of inflammatory or chronic infectious disease already diagnosed, periodic repetition of CRP (e.g., at each visit for an outpatient appointment) may help to indicate the presence of the disease or the impact of the treatment.
Recently, the association of coronary disease with high CRP serum levels measured through HS (normal cutoff: 3.0 mg/L) and its potential role as an additional indicator in the stratification of cardiovascular risk provided by predictive models (e.g., Framingham score) induced an increase in test requests at outpatient clinics. However, due to the lack of sufficient scientific evidence showing that the reduction in CRP serum concentrations prevents secondary coronary events, its request is questionable, even for patients with well-diagnosed cardiovascular disease (CVD). There are also no conclusive evidences that HS-CRP measurement in a primary screening for cardiovascular disease can modify the morbidity or mortality trend of the general population.33,34
Discussion
The recent diversification of the repertoire of complementary diagnostic and clinical follow-up tests, with state-of-the art and sophisticated techniques, is certainly contributing to improve medical care. Conversely, in several situations, the excessive request for laboratory tests may result in additional health problems, and in the spending of financial resources that could be better applied. The main causes of the growing demand for laboratory tests are:
1. Overestimation of the laboratory test rather than physical examination or medical history;
2. Defensive medical posture;
3. Failure to comply with a basic principle: before requesting a test, the physician must evaluate whether it will bring additional information;
4. Professional insecurity or inexperience;
5. Reduced time of medical appointments;
6. Standardization of "medical check-ups" (tests requested as part of a standard "routine" and not on a selective basis, case by case);
7. Aging of the world's population, with the resulting increase in comorbidities;
8. Emergence of new tests for early detection of high morbidity and chronic diseases in asymptomatic individuals (screening or check-up);
9. Influence of the media and conflicts of interest;
10. Lack of guidelines in educational institutions;
11. Lack of knowledge of procedure costs.
CRP measurement in university hospitals and in exclusively healthcare-only hospitals is showing a strong trend of increase in requests, but the process had not been critically evaluated until now. In this regard, it is possible that the availability of the HS method, which enables the detection of considerably lower CRP serum levels, may be providing physicians with a false feeling of having a more accurate method than the former, thus encouraging its general request, even in situations where it is not indicated, as in cases of diagnosis or monitoring of acute or chronic inflammatory or infectious diseases.
Having been recently introduced into the clinical practice, HS-CRP measurement still requires a set of evidences that conclusively supports recommendations or guidelines for its use, especially when addressing cases of coronary artery disease, which appears to be its main clinical use, although still vaguely defined.
The presentation of these decision flowcharts for CRP requests in the ICU, ER, ward, and outpatient clinic contexts may be the first initiative to contribute to the establishment of guidelines for these requests. They intend to guide physicians, medical students, and residents as to the main test indications and their frequency, encouraging a healthy reflection on the actual need to request them and the impact on the medical conduct to be adopted. As a general rule, if there is a high probability that the conduct will not take into account the test result, its request should be avoided, thereby preventing errors in clinical reasoning.
The guided indication of CRP measurement may have a determining effect on health and progress of clinical cases, as it helps to avoid interpretation errors and improper interventions, such as in the case of CRP requests at intervals shorter than 24 h for ICU or ER patients with inflammatory or infectious diseases, or even in the use of HS-measurement to screen CVD in the general population. It is important to remember that examinations erroneously interpreted as normal (false negative) provide the physician and the patient a false feeling of safety, while examinations erroneously interpreted as abnormal (false positive) may generate a "snowball" of other diagnostic procedures, many of them invasive, with potential risk of health hazards. The same may occur when treatment is changed without clinical justifications, based only on non-significant alterations in the indicators of inflammatory activity.
Finally, flowcharts may be useful to healthcare providers focused on maintaining the good quality of the health care provided to clients covered by the service, while conserving financial resources. Calculated in a simple way, HS-CRP measurement costs on average five times more than regular CRP measurement. Therefore, if improperly requested at a high frequency, its impact on the clinic's total expenses may be significant, and may grow exponentially over the hospitalization or outpatient follow-up period. Add to this the unnecessary costs of other diagnostic or therapeutic procedures indicated by false positives, or the costs of complications or sequelae of erroneously applied examinations or treatments, and the expenses can reach extremely high levels.
This study was a preliminary attempt to promote the rational use of CRP laboratory measurements, based on available scientific evidence and on the clinical experience of a multidisciplinary group of physicians who are familiar with the topic.
The possible limitations of the current stage of the decision flowcharts presented in this work are as follows: 1) lack of a systematic and complete review of the literature that, although desirable, could excessively delayed disclosure of the study, due to its complexity, without ensuring added value to the guided review performed; 2) impossibility, until now, to test the proposed flowcharts in the clinical practice of ICU, ER, medical wards, hospital outpatient clinics, and other exclusive public and private healthcare, university, or assistance services, which may represent a barrier for its implementation.
Conversely, the disclosure of the flowcharts in their current stage of development may enable medical professionals to test them in their specific professional contexts and to improve them based on their own experiences.
REFERENCES
- 1. Pierrakos C, Vincent JL. Sepsis biomarkers: a review. Critical Care. 2010,14:R15.
- 2. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999;340:448-54.
- 3. Wallach J. Interpretação de testes laboratoriais. 7Ş ed. Rio de Janeiro: Guanabara Koogan; 2000.
- 4. Mitaka C. Clinical laboratory differentiation of infectious versus non-infectious systemic inflammatory response syndrome. Clin Chim Acta. 2005;351:17-29.
- 5. Ho KM. An update on C-reactive protein for intensivists. Anaesth Intensive Care. 2009;37:234-41.
- 6. Clyne B, Olsaker JS. The C-reactive protein. J Emerg Med. 1999;17:1019-25.
- 7. Póvoa P.C-reactive protein: a valuable marker of sepsis Intensive Care Med. 2002;28:235-43.
- 8. Borg EJT, Horst G, Limburg PC, van Rijswijk MH, Kallenberg CG. C-reactive protein levels during disease exacerbations and infections in systemic lupus erythematosus: a prospective longitudinal study. J Rheumatol. 1990;17:1642-8.
- 9. Moutsopoulos HM, Mavridis AK, Acritidis NC, Avgerinos PC. High C-reactive protein response in lupus polyarthritis. Clin Exp Rheumatol. 1983;1:53-5.
- 10. Ridker PM, Danielson E, Fonseca FAH, Genest F, Gotto AM Jr, Kastelein JJP et al., for the JUPITER Study Group. Rosuvastatin to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein. N Engl J Med. 2008;359:2195-207.
- 11. Kuller LH, Tracy RP, Shaten J, Meilahn EN, for the MRFIT Research Group. Relation of C-reactive protein and coronary heart disease in the MRFIT nested case-control study. Am J Epidemiol. 1996;144:537-47.
- 12. Koenig W, Sund M, Frohlich M, Fischer HG, Lowel H, Doring A et al. C-reactive protein, a sensitive marker of inflammation, predicts future risk of coronary heart disease in initially healthy middle-aged men results from the MONICA (Monitoring Trends and Determinants in Cardiovascular Disease). Augsburg Cohort Study, 1984 to 1992. Circulation. 1999;99:237-42.
- 13. Haverkatea E, Thompsonb SG, Pykeb SDM, Gallimorec JR, Pepys MB. Production of C-reactive protein and risk of coronary events in stable and unstable angina. Lancet.1997;349:462-66.
- 14. Haverkate F, Thompson SG, Pyke SDM, Gallimore JR, Pepys MB, for the European Concerted Action on Thrombosis and Disabilities Angina Pectoris Study Group. Production of C-reactive protein and risk of coronary events in stable and unstable angina. Lancet. 1997;349:462-6.
- 15. Liuzzo G, Biasucci LM, Gallimore JR, Grillo Rl, Rebuzzi AG, Pepys MB et al. Prognostic value of C-reactive protein and plasma amyloid A protein in severe unstable angina. N Engl J Med. 1994;331:417-24.
- 16. Buckley DI, Fu R, Freeman M, Rogers K, Mark Helfand M. C-Reactive Protein as a Risk Factor for Coronary Heart Disease: a systematic review and meta-analyses for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;151:483-95.
- 17. Danesh J, Collins R; Appleby P, Peto R. Association of fibrinogen, C-reactive protein, albumin, or leukocyte count with coronary heart disease meta-analyses of prospective studies. JAMA. 1998;279:1477-82.
- 18. Casas JP, Shah T, Hingorani AD, Danesh J, Pepys MB. C-reactive protein and coronary heart disease: a critical review. J Intern Med. 2008;264:295-314.
- 19. Hemingway H, Philipson P, Chen R, Fitzpatrick NK, Damant J, Shipley M et al. Evaluating the quality of research into a single prognostic biomarker: a systematic review and meta-analysis of 83 studies of C-reactive protein in stable coronary artery disease. PLoS Medicine. 2010;7(6):e1000286.
- 20. Santos IS, Bensenor IM, Machado JB, Fedeli LM, Lotufo PA. Intervention to reduce C-reactive protein determination request for acute infections at an emergency department. Emerg Med J. 2012;29(12):965-8.
- 21. Ward PCJ, Harris IB, Burke MD, Horwitz C. Systematic instruction in interpretive aspects of laboratory medicine. J Med Educ. 1976;51:648-56.
- 22. Prat G, Lefreve M, Nowak E, Tonnelier JM, Renault A, L'Her E et al. Impact of clinical guidelines to improve appropriateness of laboratory tests and chest radiographs. Intensive Care Med. 2009;35:1047-53.
- 23. Pearson TA, Mensah GA, Alexander RW, Anderson JL, Cannon RO III, Criqui M et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499-511.
- 24. Adams NG. Diagnostic use of C-reactive protein in bacteraemic emergency department patients. Emerg Med Austral. 2005;17:371-5.
- 25. Antonescu-Turcu AL, Tomic R. C-reactive protein and copeptin: prognostic predictors in chronic obstructive pulmonary disease exacerbations. Curr Opin Pulmon Med. 2009;15:120-5.
- 26. Stolz D, Christ-Crain M, Morgenthaler NG, Leuppi J, Miedinger D, Bingisser R et al. Copeptin, C-reactive protein and procalcitonin as prognostic biomarkers in acute exacerbation of COPD. Chest 2007;131:1058-67.
- 27. Flanders SA, Stein J, Shochat G et al. Performance of a bedside C-reactive protein test in the diagnosis of community-acquired pneumonia in adults with acute cough. Am J Med. 2004;116:529-35.
- 28. Bundy DG, Byerley JS, Liles EA, Perrin EM, Katznelson J, Rice HE. Does this child have appendicitis? JAMA. 2007;298:438-51.
- 29. Chen SC, Wang SM. C-Reactive protein in the diagnosis of acute appendicitis. Am J Emerg Med. 1996;14:101-3.
- 30. Wu HP, Lin CY, Chang CF, Changc YJ, Huang CY. Predictive value of C-reactive protein at different cutoff levels in acute appendicitis. Am J Emerg Med. 2005;23:449-53.
- 31. Lee CC, Hong MY, Lee NY, Chen PL, Chang CM, Ko WC. Pitfalls in using serum C-reactive protein to predict bacteremia in febrile adults in the ED. Am J Emerg Med. 2012;30:562-9.
- 32. Gonzales AEM, Camargo CA, Ma J, Plautz M, Maselli JH, McCulloch CE et al. C-Reactive protein testing does not decrease antibiotic use for acute cough illness when compared to a clinical algorithm. J Emerg Med. 2011;41:1-7.
- 33. Buckley DI, Fu R, Freeman M, Rogers K, Helfand M. C-Reactive protein as a risk factor for coronary heart disease. A Systematic Review and Meta-analyses for the US Preventive Services Task Force. Ann Intern Med. 2009;151:483-95.
- 34. Michael E. A persistently elevated C-reactive protein level in pneumonia may indicate empyema. Critical Care. 2008;12:409.
Publication Dates
-
Publication in this collection
21 Feb 2013 -
Date of issue
Feb 2013
History
-
Received
02 May 2012 -
Accepted
10 July 2012