SUMMARY
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice and can lead to significant decline in functional status and quality of life among affected patients. The risk of developing AF increases with age and the presence of structural heart disease. Thus, the attendance of patients with high ventricular response to AF is common, which makes knowledge of its management mandatory. In this context, the choice of heart rate and/or rhythm control therapy is fundamental and complex, with multiple possibilities. Thus, this review aims to assist in the management of these patients, systematizing their care.
Keywords
atrial fibrillation; emergency; arrhythmia
RESUMO
A fibrilação atrial (AF) é a arritmia mais comum da prática clínica e pode levar à redução significativa do estado funcional e da qualidade de vida dos pacientes acometidos. O risco de desenvolvimento de AF aumenta com a idade e com a presença de doença cardíaca estrutural. Dessa forma, o comparecimento de paciente com AF de alta resposta ventricular é frequente, o que torna o conhecimento de seu manejo obrigatório. Nesse âmbito, a escolha da terapia de controle de frequência cardíaca e/ou ritmo é fundamental e complexa, com múltiplas possibilidades. Esta revisão tem o objetivo de auxiliar a abordagem desses pacientes, sistematizando o atendimento.
Palavras-chave
fi brilação atrial; emergência; arritmia
INTRODUCTION
Atrial fibrillation (AF) is the most common arrhythmia in clinical practice and is characterized by the absence of P waves and irregular interval between QRS complexes on the electrocardiogram (ECG).11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
AF can lead to a significant reduction in the functional status and quality of life of the affected patients. It increases mortality between 1.5 and 1.9 times on the account of hemodynamic deterioration caused by increased heart rate (HR), loss of atrioventricular (AV) synchrony and progressive dysfunction of the left atrium and ventricle, in addition to increasing the risk of stroke and other embolic events triggered by atrial thrombi.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
3 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
4 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.-55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
The risk of developing AF increases with age and with the presence of structural heart disease. Prevalence increases from 0.1% in adults less than 55 years to 8% in those aged 80 years or older. It is higher among men compared with women (1.1% x 0.8%); and among white compared with black individuals (2.2% x 1.5%).22 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.,44 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.,55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
Arterial hypertension (SAH) and coronary artery disease (CAD) (post acute myocardial infarction or ischemic cardiomyopathy) are the most common comorbidities present in patients with AF in developed countries. Rheumatic heart disease, although currently uncommon in developed countries, has a much greater association with AF. AF is an infrequent form of manifestation of acute myocardial infarction or ischemia in the absence of other signs and symptoms of CAD.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
3 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
4 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.-55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
AF and heart failure (HF) often occur together, and a cause and effect relationship between the two is common. In addition, AF is associated with pulmonary disorders including chronic obstructive pulmonary disease (COPD) and pulmonary embolism. Similarly, both the clinical and subclinical forms of hyperthyroidism are associated with an increased risk of AF. Other risk factors related to AF include chronic renal failure, genetic factors, autonomic dysfunction, hypomagnesemia, alcohol consumption, and drugs such as theophylline, adenosine and digitalis.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
3 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
4 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.-55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
The classification proposed by the ACC/AHA/ESC for AF divides it into five subtypes:11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
-
First detected or diagnosed episode independent of its duration and presence of any symptoms.
-
Paroxysmal: recurrent (more than two episodes) that terminate spontaneously lasting up to 7 days (usually ceases within 24 hours).
-
Persistent: Episodes lasting longer than 7 days that require pharmacological or electrical cardioversion to return to sinus rhythm.
-
Long-lasting persistent: the same as persistent AF, but lasting for one year or longer.
-
Permanent: when it is not possible to maintain sinus rhythm after cardioversion, or when it has been decided not to attempt cardioversion for several factors (e.g. elderly, asymptomatic, AF with low or normal ventricular response and large left atrium).
Thus, the presence of a patient with high ventricular response AF is frequent, and makes the knowledge of its management compulsory. In this context, the choice of heart rate and/or rhythm control therapy is fundamental and complex, with multiple possibilities. This review therefore aims at assisting in the approach of these patients, systematizing their care.
CLINICAL PICTURE
Not all patients with AF are symptomatic and among those who are, there is a wide variety of symptoms. Information such as onset of symptoms, timing of diagnosis, frequency and duration of episodes and severity of symptoms is very important for the therapeutic decision. Episodes can be precipitated by exercise, emotions or acute intake of large amounts of alcohol. In other cases, they may be precipitated during sleep or after a meal.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
3 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
4 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.-55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
The typical symptoms associated with AF are palpitations, tachycardia, fatigue, weakness, dizziness, reduced exercise capacity, increased urinary volume, dyspnea.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47. Follow-up studies of patients with AF have shown that approximately 90% of these individuals have recurrent episodes of AF, although more than 90% of the events are not recognized by them. Nevertheless, asymptomatic episodes lasting more than 48 hours are not uncommon, occurring in 17% of patients.44 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.,55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
More severe symptoms include restless dyspnea, angina, pre-syncope, syncope (infrequent). Some patients may also have thromboembolic events and/or stroke as their first presentation.44 Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.,55 Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
FIVE STEPS FOR THE SYSTEMATIC APPROACH OF AF IN THE EMERGENCY ROOM
1) Recognize/ward off clinical instability related to AF
It is not always easy to recognize whether AF is the main cause of clinical instability presented by the patient. Anamnesis and physical examination should be performed in all patients with AF, seeking signs of hemodynamic instability (hypotension, significant pulmonary congestion, history of syncope, mental confusion, angina/chest pain), adequate use of medications, signs/symptoms of infection, time of onset of symptoms, presence of structural heart changes (systolic HF and/or left ventricular hypertrophy) and coronary artery disease.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
Those presenting signs of hemodynamic instability at baseline (hypotension, significant pulmonary congestion, history of syncope, mental confusion, angina/chest pain – these being attributable to arrhythmia [usually in HR greater than 150 to 160 beats per minute]) should be taken to the emergency room for peripheral venous access, continuous monitoring and oxygen therapy, and promptly submitted to synchronized electrical cardioversion with 100 to 200 J, regardless of the time of onset. A bolus dose of 10,000 units of unfractionated heparin is recommended prior to this emergency cardioversion. In such cases, after the reversal, associated diseases such as CAD, valvopathy and ventricular dysfunction should always be investigated. The same is true for patients with AF and pre-excitation with elevated HR or hemodynamic instability.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
2) Remove secondary causes that induce high ventricular response
The main cause for high ventricular response AF should always be evaluated, especially in those patients with refractory HR control or who already have permanent/persistent AF and presented recent lack of HR control even while correctly using the medications. When drug adherence is appropriate, drug or alcohol use, hyperthyroidism, anemia, hydroelectrolytic disorders (especially hypo or hyperkalemia and hypomagnesemia), infections and pulmonary thromboembolism should always be considered. In these cases, all patients should perform a chest x-ray and, in women, even if asymptomatic, the collection of type I urine and uroculture must be performed.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
A recently published retrospective study evaluated the management of patients with high ventricular response AF in the ER, either according to the rhythm control or reversal strategy or not, when the patient arrives at the site. In about 30% of patients, the cause of high ventricular response AF was sepsis. The rate of adverse events among patients undergoing control/reversal strategies versus uncontrolled strategy was 40.7% x 7.1%, and only about 20% of patients achieved adequate control with therapy when a secondary cause was present. This reinforces the idea of investigating the secondary cause before adopting complementary measures in the initial approach, unless the patient presents with hemodynamic instability.66 Scheuermeyer FX, Pourvali R, Rowe BH, Grafstein E, Heslop C, MacPhee J, et al. Emergency department patients with atrial fibrillation or flutter and an acute underlying medical illness may not benefit from attempts to control rate or rhythm. Ann Emerg Med. 2015; 65(5):511-22.e2.
3) Obtain proper control of HR
There are two main strategies for managing the symptoms of patients with AF: control of HR using AV node blockers, or rhythm control (reversion to sinus rhythm followed by maintenance), either with antiarrhythmic drugs or by catheter ablation.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
The results of two large multicentric studies, AFFIRM and RACE, demonstrated that both rhythm control and ventricular rate control strategies are associated with similar rates of mortality and severe comorbidities. Generally, the choice of one or another strategy takes into account factors such as the age of the patient and the presence of symptoms associated with AF with an impact on the quality of life, and reduction of the left ventricular systolic function attributed to the presence of the arrhythmia.77 Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010; 362(15):1363-73.,88 Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, et al. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002; 347(23):1834-40.
Thus, theoretically, the initial and main objective adopted in the care of patients in the emergency room who do not present clinical instability related to AF is HR control, especially in those with more than 48 hours of symptoms, multiple comorbidities or heart disease (left ventricular dysfunction, left ventricular hypertrophy and left atrium > 50 mm).11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47. When controlling HR, unrestricted control maintenance (HR < 110 bpm) proved to be similar to the restricted control (HR < 80 bpm), and the most flexible measure was also adopted in the emergency sector approach.77 Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010; 362(15):1363-73. Exception is made for patients with left ventricular dysfunction, symptomatic mitral stenosis or coronary stenosis, in whom HR control should be more rigorous due to underlying heart disease.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
A heart rate control strategy generally requires drugs that reduce AV node conduction, such as B-blockers, nondihydropyridine calcium channel blockers or digoxin, either alone or in combination (Table 1).11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
B-blockers and/or calcium channel blockers (diltiazen and verapamil) are generally the drugs of choice for initiation of therapy. It has been proven that drugs such as diltiazen, esmolol, metoprolol and verapamil are superior in the control of HR compared to digitalis and amiodarone.99 Siu CW, Lau CP, Lee WL, Lam KF, Tse HF. Intravenous diltiazem is superior to intravenous amiodarone or digoxin for achieving ventricular rate control in patients with acute uncomplicated atrial fibrillation. Crit Care Med. 2009; 37(7):2174-9.
10 Demircan C, Cikriklar HI, Engindeniz Z, Cebicci H, Atar N, Guler V, et al. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J. 2005; 22(6):411-4.
11 Phillips BG, Gandhi AJ, Sanoski CA, Just VL, Bauman JL. Comparison of intravenous diltiazem and verapamil for the acute treatment of atrial fibrillation and atrial flutter. Pharmacotherapy. 1997; 17(6):1238-45.
12 Ellenbogen KA, Dias VC, Plumb VJ, Heywood JT, Mirvis DM. A placebo-controlled trial of continuous intravenous diltiazem infusion for 24-hour heart rate control during atrial fibrillation and atrial flutter: a multicenter study. J Am Coll Cardiol. 1991; 18(4):891-7.-1313 Platia EV, Michelson EL, Porterfield JK, Das G. Esmolol versus verapamil in the acute treatment of atrial fibrillation or atrial flutter. Am J Cardiol. 1989; 63(13):925-9. In patients without ventricular dysfunction we may use intravenous metoprolol (maximum dose of 15 mg), diltiazen 0.25 mg intravenously (repeat 0.35 mg/ kg if necessary), or verapamil 5 to 10 mg intravenously.99 Siu CW, Lau CP, Lee WL, Lam KF, Tse HF. Intravenous diltiazem is superior to intravenous amiodarone or digoxin for achieving ventricular rate control in patients with acute uncomplicated atrial fibrillation. Crit Care Med. 2009; 37(7):2174-9.
10 Demircan C, Cikriklar HI, Engindeniz Z, Cebicci H, Atar N, Guler V, et al. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J. 2005; 22(6):411-4.
11 Phillips BG, Gandhi AJ, Sanoski CA, Just VL, Bauman JL. Comparison of intravenous diltiazem and verapamil for the acute treatment of atrial fibrillation and atrial flutter. Pharmacotherapy. 1997; 17(6):1238-45.
12 Ellenbogen KA, Dias VC, Plumb VJ, Heywood JT, Mirvis DM. A placebo-controlled trial of continuous intravenous diltiazem infusion for 24-hour heart rate control during atrial fibrillation and atrial flutter: a multicenter study. J Am Coll Cardiol. 1991; 18(4):891-7.-1313 Platia EV, Michelson EL, Porterfield JK, Das G. Esmolol versus verapamil in the acute treatment of atrial fibrillation or atrial flutter. Am J Cardiol. 1989; 63(13):925-9.
Digoxin may also be used, but it is not as effective in controlling HR during physical activity.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.,1414 Jordaens L, Trouerbach J, Calle P, Tavernier R, Derycke E, Vertongen P, et al. Conversion of atrial fibrillation to sinus rhythm and rate control by digoxin in comparison to placebo. Eur Heart J. 1997; 18(4):643-8. In patients with ventricular dysfunction, the use of C-lanatoside, 0.4 mg intravenously (maximum dose of 0.8 mg), or amiodarone, 150 mg intravenously in 10 minutes, is considered as the first option.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47. The fact that amiodarone can lead to the reversal of the rhythm in up to 28% of the patients, predisposing them to the occurrence of embolic events, is highlighted.1515 Hofmann R, Steinwender C, Kammler J, Kypta A, Leisch F. Effects of a high dose intravenous bolus amiodarone in patients with atrial fibrillation and a rapid ventricular rate. Int J Cardiol. 2006; 110(1):27-32.
In patients with hemodynamic shock and AF, heart rate control should be done only when HR exceeds 130 to 150 beats per minute and preferably amiodarone via continuous infusion pump (450 to 1,200 mg daily) depending on the chronotropic response of the patient. In these cases, the HR target is usually around 120 beats per minute, without damaging the compensatory response to shock, and its indication should be reviewed daily and individually.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
4) Consider heart rate control/AF reversal
Although HR control is the main target in the treatment of high ventricular response AF in the emergency room, there are some situations in which the rhythm control strategy should be considered: if the symptoms have clearly started less than 48 hours; persistent symptoms despite adequate HR control; inability to achieve adequate HR control (ruling out secondary causes); young patients with a first episode of AF diagnosed or those in whom arrhythmia had a recent onset and the risk of recurrence appears to be lower; and, in the latter case, according to the patient’s preference.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
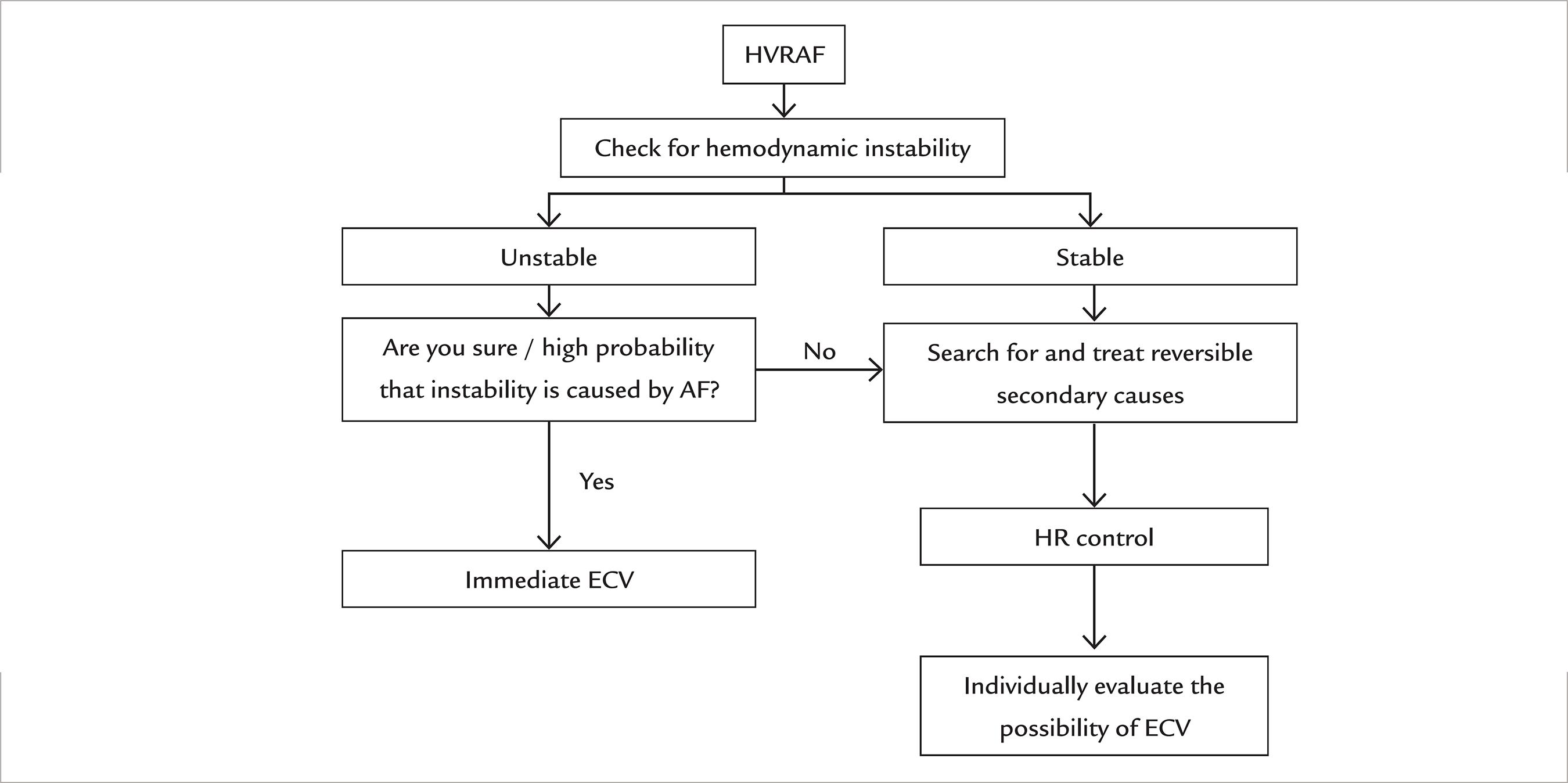
If cardioversion is chosen, it may be chemical (using antiarrhythmic drugs) or electric (Figure 1). In such cases, the patient’s HR should be kept preferably high, since after the reversal the risk of sinus bradycardia associated with clinical instability becomes lower.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
For chemical reversal, the recommended medications are: flecainide, dofetilide, ibutilide, propafenone and amiodarone. The first three are not available in Brazil. Before administering antiarrhythmic medication for cardioversion, a B-blocker or a calcium channel blocker should be given to prevent rapid AV conduction.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
In patients without structural heart disease, the option of choice is propafenone. In the first event, it should be administered in hospital orally at a dose of 450 mg (if the patient’s weight is less than 70 kg) or 600 mg (weight 70 kg or more). If the treatment is well tolerated and effective, the patient can be discharged with the guidance of home use at the same dose, if there is recurrence, in a strategy called pill in the pocket. In these cases, the probability of AF reversion in up to 6 hours is around 94% of cases. This strategy should be done only in cases of AF with few recurrences (up to 2 every 6 months).11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
In patients with structural heart disease [left ventricular hypertrophy (septum and posterior wall thickness > 1.2 cm), ischemia, valvular disease and/or ventricular dysfunction], amiodarone is the best option for chemical cardioversion. Amiodarone should be given at a dose of 150 mg intravenously in 10 minutes, or 5-7 mg/kg in 1 hour (up to a maximum dose of 2.2 g in 24 hours). Amiodarone is associated with higher rates of maintenance of sinus rhythm, but is also associated with a greater number of adverse effects in the long term.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
Sotalol may be beneficial in patients with paroxysmal AF also in sinus rhythm, provided that the patient has minimal structural disease or normal heart, and QTc < 460 ms. It is the antiarrhythmic drug of choice in patients with AF and CAD who do not have left ventricular systolic dysfunction. In this situation, propafenone is contraindicated.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
If electric cardioversion is chosen, it should be done with the administration of shock initially synchronized at 100 to 200 J in a single-phase defibrillator or 100 J in a biphasic defibrillator, after explaining the procedure and adequate sedation to the patient. Administration of amiodarone prior to electrical cardioversion increases the chance of success and may prevent immediate recurrence of AF.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
Finally, radiofrequency ablation (RFA) is also useful in maintaining sinus rhythm mainly in symptomatic patients with paroxysmal AF who have failed an antiarrhythmic, have normal or slightly increased left atrium, and normal or discreetly decreased function of the left ventricle. However, its use should be considered an exception when it comes to patients seen in emergency units.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
If there is structural heart disease, after the reversal, the patient should be discharged with amiodarone prescribed at a dose of 200 mg orally, three times a day for 2 weeks, followed by 200 mg twice daily for another 2 weeks. Thereafter, amiodarone at 200 mg daily. In the absence of evidence of structural heart disease, amiodarone should preferably be replaced with propafenone, 150 to 300 mg every 12 hours.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
In all cases with more than 48 hours of AF or in those with structural heart disease, if reversion is chosen, it is mandatory that the patient be anti-coagulated for at least 3 weeks.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47. In the case of warfarin, the weekly INR control should show values between 2.0 and 3.0. Currently one option is to use one of the new anticoagulants. In a prospective study, rivaroxaban was validated and showed the same level of safety of warfarin related to electrical cardioversion (ECV).1616 Cappato R, Ezekowitz MD, Klein AL, Camm AJ, Ma CS, Le Heuzey JY, et al. Rivaroxaban vs. vitamin Kantagonists for cardioversion in atrial fibrillation. Eur Heart J. 2014; 35(47):3346-55. Apixaban and dabigatran, on the other hand, also showed the same safety profile of warfarin in subanalyses.1717 Nagarakanti R, Ezekowitz MD, Oldgren J, Yang S, Chernick M, Aikens TH, et al. Dabigatran versus warfarin in patients with atrial fibrillation: an analysis of patients undergoing cardioversion. Circulation. 2011; 123(2):131-6.,1818 Flaker G, Lopes RD, Al-Khatib SM, Hermosillo AG, Hohnloser SH, Tinga B, et al.; ARISTOTLE Committees and Investigators. Efficacy and safety of apixaban in patients after cardioversion for atrial fibrillation: insights from the ARISTOTLE Trial (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation). J Am Coll Cardiol. 2014; 63(11):1082-7. Thus, the guidelines release their use when choosing to reverse the patient’s rhythm. After reversion, any of the anticoagulants used should be maintained for a minimum period of 4 weeks, and may be extended indefinitely if the patient presents risk factors for AF recurrence (ventricular dysfunction and/or structural heart disease, atrial dilatation, previous episodes, etc).11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
In those without oral anticoagulant use for at least three continuous weeks, transesophageal echocardiography must be performed. In the absence of thrombi, the patient may be cardioverted with synchronized electrical therapy or chemical therapy.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
If a thrombus is seen, only HR control should be performed and the patient is discharged with oral anti-coagulation prescription to schedule the procedure after at least 3 weeks at an outpatient clinic.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
5) Define the indication for oral anticoagulation
All patients with AF should be evaluated for the need for anticoagulation and this is done by applying the CHADS2 and/or CHA2DS2VASC scores. The latter is a refinement of the former and has been the most used in recent years because it identifies patients with actual “low risk” more accurately. For the evaluation of bleeding risk, the most commonly used criterion is HAS-BLED, which serves as a guideline for the rational and cautious choice of anti-coagulation. However, it should not contraindicate it.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.,1919 Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012; 33(12):1500-10.
There are two indications of anticoagulation in AF. In the short term, in patients with low thromboembolic risk in which the strategy of rhythm control is chosen and cardioversion is performed to the sinus rhythm, and in the long term, patients that meet criteria for chronic anticoagulation.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
Antithrombotic therapy to prevent thromboembolism should be indicated for all patients with AF, except for those with isolated AF without other risk factors, and those with a contraindication to it. Anticoagulation is recommended for patients at high risk of thromboembolic event (two or more risk factors considering the CHA2DS2VASC score). If the CHA2DS2VASC criterion only scores for the female sex, chronic oral anticoagulation is not mandatory.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
The selection of the anticoagulant agent should be based on the absolute risk of stroke and bleeding and the risk/benefit ratio to the patient. In patients with significant heart valve disease, mechanical valvular prostheses and/ or chronic renal insufficiency (CrCl < 30 mL/min), the option is warfarin. The target INR is 2.0 to 3.0, except for mitral and aortic mechanical prostheses, in which case the target varies between 2.5 and 3.5.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
In the remaining patients, warfarin or any of the new anticoagulants (apixaban, rivaroxaban or dabigatran) may be used.11 American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
2 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.-33 Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.,2020 Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al.; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361(12):1139-51.
21 Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al.; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365(10):883-91.-2222 Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al.; ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Eng J Med. 2011; 365(11):981-92.
The association of ASA and clopidogrel to reduce the risk of thromboembolic events may be considered for patients with AF in case of possible inadequate anticoagulation with warfarin, either at the choice of the patient or when the attending physician is not sure of the safety for the patient. In this case, the level of evidence is lower and comes from simple non-multicentre studies.22 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
When the patient with AF remains hospitalized for another reason, the use of warfarin should be routinely withdrawn at least in the initial phase. Although there is limited evidence in hospitalized patients, when INR is below 2.0, anticoagulation should be initiated with subcutaneous enoxaparin, 1 mg/kg every 12 hours, or unfractionated heparin via continuous infusion.22 Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
CONCLUSION
Management of patients with high ventricular response AF in the emergency room is complex. Identifying factors that cause AF is critical to correct treatment. When possible, heart rate control is the priority. At the time of hospital discharge, the patient should be evaluated for indication and possibility of oral anticoagulation. In a simplified manner, the algorithm for conduct is shown in Figure 2.
-
Study conducted at Instituto do Coração (InCor), Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil
REFERENCES
-
1American College of Cardiology Foundation; American Heart Association; European Society of Cardiology; Heart Rhythm Society, Wann LS, Curtis AB, et al. Management of patients with atrial fibrillation (compilation of 2006 ACCF/AHA/ESC and 2011 ACCF/AHA/HRS recommendations): a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. Circulation. 2013; 127(18):1916-26.
-
2Magalhães LP, Figueiredo MJO, Cintra FD, Saad EB, Kuniyoshi RR, Teixeira RA, et al. II Diretrizes Brasileiras de Fibrilação Atrial. Arq Bras Cardiol 2016; 106(4Supl. 2):1-22.
-
3Camm AJ, Lip GY, De Caterina R, Savelieva I, Atar D, Hohnloser SH, et al.; ESC Committee for Practice Guidelines (CPG). 2012 focused update of the ESC Guidelines for the management of atrial fibrillation: an update of the 2010 ESC Guidelines for the management of atrial fibrillation. Developed with the special contribution of the European Heart Rhythm Association. Eur Heart J. 2012; 33(21):2719-47.
-
4Chugh SS, Blackshear JL, Shen WK, Hammill SC, Gersh BJ. Epidemiology and natural history of atrial fibrillation: clinical implications. J Am Coll Cardiol. 2001; 37(2):371-8.
-
5Heeringa J, van der Kuip DA, Hofman A, Kors JA, van Herpen G, Stricker BH, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam study. Eur Heart J 2006; 27(8):949-53.
-
6Scheuermeyer FX, Pourvali R, Rowe BH, Grafstein E, Heslop C, MacPhee J, et al. Emergency department patients with atrial fibrillation or flutter and an acute underlying medical illness may not benefit from attempts to control rate or rhythm. Ann Emerg Med. 2015; 65(5):511-22.e2.
-
7Van Gelder IC, Groenveld HF, Crijns HJ, Tuininga YS, Tijssen JG, Alings AM, et al. Lenient versus strict rate control in patients with atrial fibrillation. N Engl J Med. 2010; 362(15):1363-73.
-
8Van Gelder IC, Hagens VE, Bosker HA, Kingma JH, Kamp O, Kingma T, et al. A comparison of rate control and rhythm control in patients with recurrent persistent atrial fibrillation. N Engl J Med. 2002; 347(23):1834-40.
-
9Siu CW, Lau CP, Lee WL, Lam KF, Tse HF. Intravenous diltiazem is superior to intravenous amiodarone or digoxin for achieving ventricular rate control in patients with acute uncomplicated atrial fibrillation. Crit Care Med. 2009; 37(7):2174-9.
-
10Demircan C, Cikriklar HI, Engindeniz Z, Cebicci H, Atar N, Guler V, et al. Comparison of the effectiveness of intravenous diltiazem and metoprolol in the management of rapid ventricular rate in atrial fibrillation. Emerg Med J. 2005; 22(6):411-4.
-
11Phillips BG, Gandhi AJ, Sanoski CA, Just VL, Bauman JL. Comparison of intravenous diltiazem and verapamil for the acute treatment of atrial fibrillation and atrial flutter. Pharmacotherapy. 1997; 17(6):1238-45.
-
12Ellenbogen KA, Dias VC, Plumb VJ, Heywood JT, Mirvis DM. A placebo-controlled trial of continuous intravenous diltiazem infusion for 24-hour heart rate control during atrial fibrillation and atrial flutter: a multicenter study. J Am Coll Cardiol. 1991; 18(4):891-7.
-
13Platia EV, Michelson EL, Porterfield JK, Das G. Esmolol versus verapamil in the acute treatment of atrial fibrillation or atrial flutter. Am J Cardiol. 1989; 63(13):925-9.
-
14Jordaens L, Trouerbach J, Calle P, Tavernier R, Derycke E, Vertongen P, et al. Conversion of atrial fibrillation to sinus rhythm and rate control by digoxin in comparison to placebo. Eur Heart J. 1997; 18(4):643-8.
-
15Hofmann R, Steinwender C, Kammler J, Kypta A, Leisch F. Effects of a high dose intravenous bolus amiodarone in patients with atrial fibrillation and a rapid ventricular rate. Int J Cardiol. 2006; 110(1):27-32.
-
16Cappato R, Ezekowitz MD, Klein AL, Camm AJ, Ma CS, Le Heuzey JY, et al. Rivaroxaban vs. vitamin Kantagonists for cardioversion in atrial fibrillation. Eur Heart J. 2014; 35(47):3346-55.
-
17Nagarakanti R, Ezekowitz MD, Oldgren J, Yang S, Chernick M, Aikens TH, et al. Dabigatran versus warfarin in patients with atrial fibrillation: an analysis of patients undergoing cardioversion. Circulation. 2011; 123(2):131-6.
-
18Flaker G, Lopes RD, Al-Khatib SM, Hermosillo AG, Hohnloser SH, Tinga B, et al.; ARISTOTLE Committees and Investigators. Efficacy and safety of apixaban in patients after cardioversion for atrial fibrillation: insights from the ARISTOTLE Trial (Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation). J Am Coll Cardiol. 2014; 63(11):1082-7.
-
19Friberg L, Rosenqvist M, Lip GY. Evaluation of risk stratification schemes for ischaemic stroke and bleeding in 182 678 patients with atrial fibrillation: the Swedish Atrial Fibrillation cohort study. Eur Heart J. 2012; 33(12):1500-10.
-
20Connolly SJ, Ezekowitz MD, Yusuf S, Eikelboom J, Oldgren J, Parekh A, et al.; RE-LY Steering Committee and Investigators. Dabigatran versus warfarin in patients with atrial fibrillation. N Engl J Med. 2009; 361(12):1139-51.
-
21Patel MR, Mahaffey KW, Garg J, Pan G, Singer DE, Hacke W, et al.; ROCKET AF Investigators. Rivaroxaban versus warfarin in nonvalvular atrial fibrillation. N Engl J Med. 2011; 365(10):883-91.
-
22Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al.; ARISTOTLE Committees and Investigators. Apixaban versus warfarin in patients with atrial fibrillation. N Eng J Med. 2011; 365(11):981-92.
Publication Dates
-
Publication in this collection
Dec 2016
History
-
Received
30 July 2016 -
Accepted
19 Oct 2016