Abstracts
Management of gingival lesions of vesicobullous autoimmune diseases is one the main challenges to oral medicine, primarily because of their chronic nature. Systemic therapy is required in most severe lesions, however, whenever feasible, topic corticosteroid therapy is preferred. This article describes a technique to provide topical occlusive corticotherapy that has shown to be effective in controlling these lesions, especially in patients exclusively with gingival lesions.
Adrenal cortex hormones; Autoimmune diseases; Gingiva; Oral manifestations; Skin diseases; vesiculobullous
O tratamento das lesões gengivais de doenças vesicobolhosas auto-imunes constitui grande desafio na estomatologia, principalmente pela natureza crônica das lesões. O tratamento sistêmico é necessário no controle das apresentações mais graves; entretanto, quando possível, o tratamento tópico é preferível. Este artigo descreve uma técnica oclusiva para aplicação de corticosteróide tópico que tem demonstrado ser eficaz no controle dessas lesões, sobretudo em pacientes com manifestações exclusivamente gengivais.
Corticosteróides; Dermatopatias vesiculobolhosas; Doenças auto-imunes; Gengiva; Manifestações bucais
COMMUNICATION
Topical occlusive corticosteroid for the treatment of gingival manifestations of vesicobullous autoimmune diseases* * Work done at School of Dentistry of Universidade de São Paulo - USP (Campi São Paulo and Ribeirão Preto); Hospital das Clínicas School of Medicine of Ribeirão Preto - Universidade de São Paulo - USP - São Paulo (SP), Brazil.
Ana Carolina Fragoso MottaI; Marilena Chinali KomesuII; Márcio Fernando de Moraes GrisiIII; Cacilda da Silva SouzaIV; Ana Maria Ferreira RoselinoV; Dante Antonio MigliariVI
IDentist, Ph.D. in Oral Diagnosis, School of Dentistry, Universidade de São Paulo USP - São Paulo (SP), Brazil
IIAssociate Professor, Dept. of Morphology, Stomatology, and Physiology of the School of Dentistry of Ribeirão Preto da Universidade de São Paulo USP - Ribeirão Preto (SP), Brazil
IIIAssociate Professor, Dept. of Orthognatic Surgery, Traumatology, and Periodontics of the School of Dentistry of Ribeirão Preto da Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
IVM.D., Professor, Dept of Clinical Medicine, Division of Dermatology, School of Medicine of Ribeirão Preto da Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
VAssociate Professor, Dept of Clinical Medicine, Division of Dermatology, School of Medicine of Ribeirão Preto da Universidade de São Paulo - USP - Ribeirão Preto (SP), Brazil
VIAssociate Professor, Dept. of Stomatology, School of Dentistry, Universidade de São Paulo - USP - São Paulo (SP), Brazil
Correspondence Correspondence
ABSTRACT
Management of gingival lesions of vesicobullous autoimmune diseases is one the main challenges to oral medicine, primarily because of their chronic nature. Systemic therapy is required in most severe lesions, however, whenever feasible, topic corticosteroid therapy is preferred. This article describes a technique to provide topical occlusive corticotherapy that has shown to be effective in controlling these lesions, especially in patients exclusively with gingival lesions.
Keywords: Adrenal cortex hormones; Autoimmune diseases; Gingiva; Oral manifestations; Skin diseases, vesiculobullous
Management of gingival lesions of vesicobullous autoimmune diseases is one the main challenges to oral medicine, primarily because of their chronic nature.1-3 Treatment of these lesions usually requires topical corticosteroids, or other anti-inflammatory drugs. Systemic therapy is required in most severe lesions, especially in pemphigus. However, whenever feasible, topical corticosteroid is preferred, because of adverse effects of systemic treatment.4-6 Some studies reported good outcomes of patients with oral lesions treated with a topical corticosteroids mouthwash,4 and ointment with or without an adherent vehicle.5-8 However, it can be difficult to apply and maintain the corticosteroid on the entire lesional surface in patients with extensive or deep gingival lesions. In addition, normal mouth movements can rapidly displace the corticosteroid from its initial localization, reducing the contact time between drug and lesions. The use of a tray with ointment provides a solution for this problem, because it secures the corticosteroid, and provides an occlusive therapy.9,10
This article describes a technique of topical occlusive corticotherapy in a 36-year-old woman that was presented to Oral Diagnosis Clinics of Dentistry School of Ribeirão Preto at University of São Paulo for evaluation of painful, ulcerated, desquamative gingival lesions that had developed 12 years before. These had been unresponsive to all forms of treatment. A medical history of the patient was taken and revealed no unusual findings. Upon physical examination, she presented a good aspect, with no evidence of other lesions in her body. Intraoral examination revealed diffuse gingival inflammation with mild edema and evidence of intact bulla, involving mainly the vestibular gingival surfaces (Figure 1).
The patient was referred to University Hospital of Medical School of Ribeirão Preto at University of São Paulo, Division of Dermatology for a baseline evaluation of possible involvement in other sites. There were no ocular, skin or genital lesions and the patient remains free of such involvement to the present day.
A biopsy specimen of gingival lesion was then obtained for light microscopy and direct immunofluorescence analysis. Histopathologic examination showed subepithelial vesicle formation separating the surface epithelium from the underlying connective tissue at the level of the basement membrane. A mild infiltration of chronic inflammatory cells was noticed subjacent to the cleavage sites. Direct immunofluorescence revealed deposition of IgG in the linear band at the level of the basement membrane. After a review of all findings, diagnosis was of mucous membrane pemphigoid.
Firstly, periodontal treatment was carried out because the patient presented gingivitis, and it consisted of plaque control and standard scaling and crown planning. After periodontal treatment, a topical corticosteroid therapy was instituted using soft maxillary and mandibular trays of silicone plates fabricated on study models (Figure 2A, B, C and D ) similar to those described by Aufdemorte et al.10
The patient was instructed to coat all internal surfaces with clobetasol propionate 0.05% ointment Clob x, Galderma Brazil Ltda., São Paulo, SP and to insert the trays three times a day (after breakfast, after lunch and after dinner), 20 minutes each time, after the oral hygiene. The patient was advised to expectorate excess saliva after the application and not to swallow for at least 1 hour.
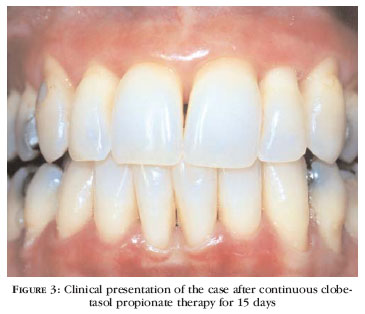
All areas of ulceration were healing after 2 weeks (Figure 3). The corticosteroid was gradually tapered off over the next week and then discontinued. The patient was advised to continue applying the corticosteroid ointment (3-week cycle) whenever necessary.
Close follow-up of the patient was carried out, starting on a monthly basis for three months and every three months, thereafter.
This paper describes an occlusive technique for treatment of gingival lesions of vesicobullous autoimmune diseases. Due to the localized nature of involvement in this patient presented here, topical occlusive corticosteroid therapy was considered the treatment of choice. The use of a tray with a potent topical corticosteroid, as clobetasol propionate that was used in this study, has been promised to improve disease control since it maintains a greater contact time between the ointment and all the gingival lesion.10 Special emphasis should be placed to oral hygiene, because dental plaque often aggravates the symptoms of the lesions. Hence the need for proper oral physiotherapy should constantly be reinforced to the patient and periodontal treatment should be instituted whenever necessary.9,10
In conclusion, we emphasize that patients with gingival lesions of vesicobullous diseases require interdisciplinary care, and that the technique here described can be used for patients exclusively with gingival lesions, and can be an adjunct to systemic treatment in patients with oral and skin lesions.
REFERENCES
Ana Carolina Fragoso Motta
Rua Padre Anchieta, 2050 - Jardim Antártica
14051-220 - Ribeirão Preto - SP
Fax: +55 (16) 3633-6720
E-mail: anacfm@usp.br
Received on May 18, 2004.
Approved by the Consultive Council and accepted for publication on April 03, 2006.
Conflict of interest: None
-
11. Markopoulos AK, Antoniades D, Papanayotou P, Trigonidis G. Desquamative gingivitis: A clinical, histopathologic, and immunologic study. Quintessence Int. 1996;27:763-7.
-
22. Chan JS, Ahmed AR, Anhalt GJ, Bernauer W, Cooper KD, Elder MJ, et al. The first international consensus on mucous membrane pemphigoid. Arch Dermatol. 2002;138:370-9.
-
33. Mignona MD, Lo Muzio L, Bucci E. Clinical features of gingival pemphigus vulgaris. J Clin Periodontol. 2001;28:489-93.
-
44. Gonzalez-Moles MA, Morales P, Rodríguez-Archilla A, Isabel IR-A, Gonzales-Moles S. Treatment of severe chronic oral erosive lesions with clobetasol propionate in aqueous solution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:264-70.
-
55. Lozada-Nur F, Miranda C, Maliksi R. Double-bind clinical trial of 0.05% clobetasol proprionate ointment in orabase and 0.05% fluocinonide ointment in orabase in the treatment of patients with oral vesiculoerosive diseases. Oral Surg Oral Med Oral Pathol. 1994;77:598-604.
-
66. Lozada F, Silverman Jr. S. Topically applied fluocinonide in an adhesive base in the treatment of oral vesiculoerosive diseases. Arch Dermatol. 1980;116:898-900.
-
77. Voute AB, Schulten EA, Langendijk PN, Kostense PJ, van der Waal I. Fluocinonide in an adhesive base for treatment of oral lichen planus. A double-blind, placebo-controlled clinical study. Oral Surg Oral Med Oral Pathol. 1993;75:181-5.
-
88. Lozada-Nur F, Huang MZ. Open preliminary clinical trial of clobetasol propionate in adhesive paste for treatment of chronic oral vesiculoerosive diseases. Oral Surg Oral Med Oral Pathol. 1991;71:283-7.
-
99. Aufdemorte TB, De Villez RL, Parel SM. Modified topical corticosteroid therapy for the treatment of oral mucous membrane pemphigoid. Oral Surg Oral Med Oral Pathol. 1985;59:256-60.
-
1010. Gonzalez-Moles MA, Ruiz-Avila I, Rodriguez-Archilla A, Morales-Garcia P, Mesa-Aguado F, Bascones-Martinez A, et al. Treatment of severe erosive gingival lesions by topical application of clobetasol propionate in custom trays. Oral Surg Oral Pathol Oral Radiol Endod. 2003;95:688-92.
Publication Dates
-
Publication in this collection
24 July 2006 -
Date of issue
June 2006
History
-
Accepted
03 Apr 2006 -
Received
18 May 2004