Abstracts
We report a patient suffering from dimorphic Hansen's disease who has self medicated his neuropathy with oral corticosteroid for a long time. A yellowish, nodular-cystic lesion partially topped with crusting, surrounded by a brownish red halo, was noted on the inner aspect of his left leg. Direct mycological examination confirmed the hypothesis of pheohyphomycosis.
Cladosporium; Exophiala; Iatrogenic disease; Mycoses
Descreve-se caso clínico de paciente tratado de hanseníase dimorfa, que utilizou automedicação, com doses variadas de corticosteróide oral, por longo período, devido à neuropatia hansênica. Desenvolveu lesão nódulo-cística, amarelada, com algumas crostas, envolta por halo eritêmato-acastanhado, na face interna da perna esquerda. O exame micológico direto confirmou a hipótese diagnóstica de feo-hifomicose.
Cladosporium; Doença iatrogênica; Exophiala; Micoses
WHICH IS YOUR DIAGNOSIS?
Case for diagnosis* * Work done at Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória EMESCAM - Vitória (ES), Brazil.
Leonardo Mello FerreiraI; Rodrigo Negri PereiraII; Lucia Martins DinizIII; João Basilio de Souza FilhoIV
IPost-Graduate student at the Department of Dermatology of EMESCAM - Vitória (ES), Brazil
IIPost-Graduate student at the Department of Dermatology of EMESCAM - Vitória (ES), Brazil
IIIAssistant Professor of Graduate Studies in Dermatology at EMESCAM - Vitória (ES), Brazil. Especialista em dermatologia pela Sociedade Brasileira de Dermatologia
IVTitular Professor of Dermatology at EMESCAM - Vitória (ES), Brazil. Dermatologist of the Brazilian Society of Dermatology
Correspondence Correspondence Leonardo Mello Ferreira Av. Nossa Senhora da Penha, 2432 - apto. 1406 Edifício Angra dos Reis - Bairro Praia do Canto 29045-402 Vitória - ES Telephone: +55 (27) 3225-8904 E-mail: llsmf@globo.com
ABSTRACT
We report a patient suffering from dimorphic Hansen's disease who has self medicated his neuropathy with oral corticosteroid for a long time. A yellowish, nodular-cystic lesion partially topped with crusting, surrounded by a brownish red halo, was noted on the inner aspect of his left leg. Direct mycological examination confirmed the hypothesis of pheohyphomycosis.
Keywords: Cladosporium; Exophiala; Iatrogenic disease; Mycoses
HISTORY OF THE DISEASE
Forty-year-old male patient, rural worker, living in the rural area of Afonso Cláudio, ES.
Sought the dermatology department due to joint pain and parestesias in extremities, besides a lesion in the left lower limb, with four months of evolution, and a few inflammatory episodes. In his past medical history there was a multibacillary multidrug therapy for dimorphic Hansen's disease during 12 months, having been discharged in 2001. Since then, he had episodes of types I and II hansenic reaction. In order to treat them, he made continuous use of thalidomide and prednisone, with or without medical follow-up, and, currently, of 20 mg oral prednisone.
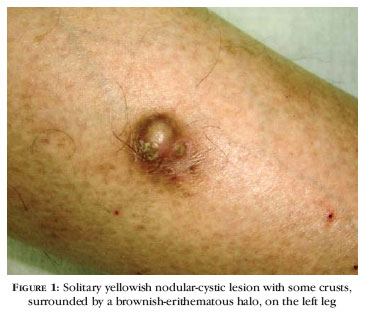
Upon dermatological examination, a yellowish nodular-cystic lesion with some crusts was found, surrounded by a brownish-erithematous halo, on the inner surface of the left leg (Figure 1).
An aspiration of the lesion content was carried out, with a yellowish secretion that underwent direct mycological examination with 20% KOH, in which dematiaceous and septated hyphae were observed (Figure 2).
Surgical exeresis with grafting was programmed, and a steroid withdrawal scheme was initiated, with control of hansenic neuropathy.
COMMENTS
Initial clinical hypotheses were those of infected epidermal cyst and subcutaneous pheohyphomycosis. The latter was confirmed by means of direct mycological examination of lesion secretion. Colony macromorphology, obtained under room temperature in agar Sabouraud culture medium, exhibited a black leaven-like aspect, with a white cottonous area on the surface. Micromorphology of the colony identified the fungus Exophiala jeanselmei.
Pheohyphomycosis is the term used to designate cutaneous and systemic diseases caused by dematiaceous fungi, which present in tissues as leaven cells, pseudohyphae and dematiaceous hyphae.1
Incidence of this disease has been increasing importantly over the last few years. It is suspected that one of the reasons for such increase is iatrogenic immunosuppresion.2
Mycosis is often an opportunistic infection, occurring in weakened patients, bearing chronic diseases, diabetes, leukemia, and other immunosuppressed, even though in many reported cases there is no evidence for an immunodeppression.1,3
Over 100 species have been identified as causing the disease.2 Among the most common etiological factors, are Exophiala jeanselmei and Wangiella dermatitidis.1
Clinical forms are twofold: subcutaneous and systemic. Subcutaneous form happens in consequence of a traumatic inoculation, and presents as cysts, abscesses or verrucous lesions, of slow evolution.1E. jeanselmei is a typical agent in this form,1 which has a difficult differential diagnosis with epidermal cyst.3 In the disseminated form, infection pathway is usually inhalation, and develops with compromising of several internal organs, in particular the central nervous system, and the most frequently identified etiological factor is Cladosporium bantianum.1,4
Diagnosis of the cystic form of the mycosis is usually obtained by means of histopathological examination. Abscesses situated in cellular subcutaneous tissue or deep dermis are surrounded by a thick fibrous capsule. Fungi are found mainly in the inner layer of the cyst wall, although they can be seen in the core of the abscess, under the form of septated hyphae of brownish color.3
First treatment choice for pheohyphomycosis is itraconazol in a prolonged schedule. Located lesions must be treated surgically or with local infiltration of amphoterecin B. For the disseminated cases, an association of amphoterecin B and 5-flyorocytosine is used.1,3
In the present report, even more important than the rarity of the disease and the way it was diagnosed, is the warning for the consequences of prolonged steroid therapy without proper follow-up, which can be far more severe than those hereby presented.
REFERENCES
Received on December 30, 2005.
Approved by the Consultive Council and accepted for publication on April 17, 2006.
Conflict of interest: None
- 1. Lacaz CS, Porto E, Martins JEC, Heins-Vaccari EM, Melo NT. Tratado de Micologia Médica Lacaz. 9 ed. São Paulo: Sarvier; 2002. p.519-61.
- 2. Revancar SG, Patterson JE, Sutton DA, Pullen R, Rinaldi MG. Disseminated phaeohyphomycosis: review of an emerging mycosis. Clin Infect Dis. 2002;35:1022-3.
- 3. Fonseca APM, Fonseca WSM, Silva JG, Bona SH, Araújo RCA, Silva JF. Feohifomicose subcutânea: relato de três casos. An Bras Dermatol. 1990;6:303-7.
- 4. Revancar SG, Sutton DA, Rinaldi MG. Primary central nervous system phaeohyphomycosis: a review of 101 cases. Clin Infect Dis. 2004;38:206-16.
Publication Dates
-
Publication in this collection
24 July 2006 -
Date of issue
June 2006
History
-
Accepted
17 Apr 2006 -
Received
30 Dec 2005