Abstracts
The yellow nail syndrome is a rare disease, in which there is a triad of lymphedema, pleural effusion and slow-growing dystrophic yellow nails. Many associations have already been described; among them, chronic respiratory tract diseases, autoimmune disorders, malignancies and immunodeficiency conditions. Only one third of cases in the literature show all findings. The case reported next is an example of the classical triad.
Lymphedema; Nail diseases; Pleural effusion
A síndrome da unha amarela é uma doença rara, caracterizada pela tríade de linfedema, derrame pleural e unhas Distróficas de crescimento lento e coloração amarelada. Várias associações já foram descritas, entre elas, afecções crônicas do aparelho respiratório, doenças autoimunes, malignidades e estados de imunodeficiência. Entre os casos citados na literatura, apenas cerca de um terço se apresenta com todos os achados e o caso relatado a seguir é um exemplo da tríade clássica.
Derrame pleural; Doenças da unha; Linfedema
CASE REPORT
Yellow nail syndrome - Case report
IResident physician of Dermatology at Universidade Federal de Juiz de Fora (UFJF) - Juiz de Fora (MG), Brazil
IIResident physician of Dermatology at Universidade Federal de Juiz de Fora (UFJF) - Juiz de Fora (MG), Brazil
IIIResident physician of Clinical Medicine at Universidade Federal de Juiz de Fora (UFJF) - Juiz de Fora (MG), Brazil
IVDermatologist. Preceptor of Dermatology at Universidade Federal de Juiz de Fora (UFJF) - Juiz de Fora (MG), Brazil
VDouctor of dermatology. Head of Dermatology at Universidade Federal de Juiz de Fora (UFJF) - Juiz de Fora (MG), Brazil
Mailing Address
ABSTRACT
The yellow nail syndrome is a rare disease, in which there is a triad of lymphedema, pleural effusion and slow-growing dystrophic yellow nails. Many associations have already been described; among them, chronic respiratory tract diseases, autoimmune disorders, malignancies and immunodeficiency conditions. Only one third of cases in the literature show all findings. The case reported next is an example of the classical triad.
Keywords: pleural effusion; nail diseases; lymphedema
INTRODUTION
Described for the first time in 1964 by Samman and White,1 the yellow nail syndrome (YNS) is a rare condition that is characterized by the triad of lymphedema, pleural effusion and slow-growth yellowish dystrophic nails. Its main causal factor is deficiency in lymphatic drainage and it predominates in middle age with a female:male ratio of 1.6:1.2
Many associations have been described including chronic symptoms of the respiratory tract,3 autoimmune diseases like lupus erythematosus, thyroiditis, and rheumatoid arthritis,4 malignancies5, and immunodeficiencies.6
About only one third of the cases described in the literature present all symptoms, and Gupta7 observed it in 27% of the 62 cases he revised. The following report is one example of the classical triad described by Emerson.8
CASE REPORT
A 61-year-old white woman reported alterations in finger and toe nails that had started at 19 years of age characterized by slow growth and yellowish color.
Referred by the Department of Pneumology, she was under investigation for wet cough with mucous discharge present for more than 40 years, dyspnea after moderate effort in the past five years, which recently was present even during rest. She also had bilateral pleural effusion and edema in the lower limbs which did not disappear in spite of the use of diuretics.
Ex-smoker for 20 years (20 years/pack) she reported a prior diagnosis of bronchial ectasia, three previous unsuccessful systemic treatments for onychomycosis. She denied similar conditions in her family.
Relevant information provided by the physical examination revealed nail dystrophy in both hands and feet, characterized by thickening, opacity, yellow color, increased lateral and anteroposterior curvatures, onycholysis, and absence lunula and cuticle (Figure 1).
Upon examination of the respiratory tract, she presented absence of vesicular murmur and reduced thoracic-vocal thrill on the bases. In lower limbs, there was hard pitting edema (Figure 2).
Additional examination did not show any alteration in the CBC, blood biochemistry, thyroid function test, neither in auto-antibodies or inflammatory activity tests, with a poorly reactive PPD and negative for HIV.
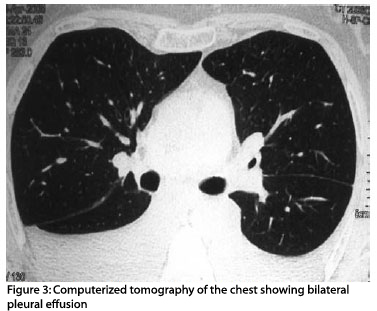
The analysis of pleural fluid was compatible with exudate, without underlying infectious or neoplastic processes, which the pleural biopsy confirmed. Chest x-ray and CT scan showed abundant bilateral pleural effusion (Figure 3).
The results of three direct mycology tests and fungi cultures of nail scraping were negative.
DISCUSSION
YNS was initially described in 1964, in a study with thirteen patients with yellow nails and lymphedema.1 It affects more frequently women (1.6:1) and occurs especially in middle age, although it has been described from birth to the eight decade of life.2 Family history is rare.
The case presented here is a typical yellow nail syndrome where it was possible to see a yellowish color ranging from pale yellow to greenish yellow, thick opaque slow-growing nails (less than 0.25mm per week) with an increase in lateral and anteroposterior curvatures. All 20 nails may be affected and in most cases few are spared; exclusive nail affection occurs in about 10% of the patients. Nail alterations are an early and constant sign, and their absence will lead to doubt as to the diagnosis that may made clinically upon the presence of at least two of the elements of triad. The cuticle and lunula are absent and onycholysis is frequent. These alterations seem to be due to deficiency in lymphatic drainage in finger extremities as suggested by lymphographic and histopathology studies of the nail matrix, which were not done in this case, but which when done will show dense fibrous tissue replacing stroma with intense vessel ectasia.1,2,8 The pigment affected by the yellowish color is probably lipofucsin, resulting from the oxidation of fat due to excess free radicals.9
It is important to emphasize that yellow nails are not specific to YNS and may occur after the use of tetracyclines or certain nail varnishes, as well as the consequence of onychomycosis and lichen planus.
Lymphedema, present in 80% of cases, prevails on lower limbs, like in the patient herein; it is frequently asymmetric, sometimes very mild, but it may also affect the hands and face and occasionally is widespread.2
Each manifestation may emerge at different times and pleural effusion seems to be a late manifestation of the syndrome, as in the case reported. Characterized by a unilateral or bilateral exudate with lymphocyte predominance, it generally affects both sides. There is a tendency to persistency and fluid deposition may return after relief drainage and, when there is an early relapse, pleurodesis might be necessary.10
D'Alessandro et al defend the theory that lymphatic block alone is not enough to explain all clinical manifestations like, for example, the high protein levels found in the pleural fluid and they suggest the presence of microangiopathy with increased microvascular patency as the most likely physiopathological mechanism.11
In addition to the classical triad, other manifestations may accompany the syndrome, for example chronic rhinosinusitis, bronchial ectasies3, pericardial effusion, and chylous ascitis.12 It may also be associated to autoimmune diseases and a immunodeficiencies like rheumatoid arthritis,4 lupus erythematosus, thyroidis, and AIDS.6 There are reports of association with malignancies including breast, lung, larynx, endometrium, Gall bladder, melanoma, and metastatic sarcomas, Hodgkin's disease, and T-cell skin lymphoma.
The spontaneous improvement of the nail symptoms may occur in 7 to 30% of patients, and in some cases, when associated diseases are treated, nails also improve. The treatments proposed include especially the topical use (5%) and oral use (600 a 1200UI) of vitamin E13 for long periods, 6 to 18 months, but there are also reports on the use of intralesional steroids, oral zinc sulfate, and antifungal drugs such as itraconazole 400mg/day for one week every month for 4 to 6 months and fluconazole 300mg weekly because they stimulate nail growth.14,15
Yellow nail syndrome is a rare disease and its diagnosis should always consider the possibility of malignancy or other associated diseases, and its treatment still remains a challenge to dermatologists.
REFERENCES
- 1. Samman PD, White WF. The "yellow nail" syndrome. Br J Dermatol. 1964;76:153-7.
- 2. Nordkild P, Kromann-Andersen H, Struve-Christensen E. Yellow nail syndrome: the triad of yellow nails, lymphedema and pleural effusions. A review of the literature and a case report. Acta Med Scand. 1986;219:221-7.
- 3. Kaminsky S, Castro LGM. SÍndrome das unhas amarelas: relato de um caso. An Bras Dermatol. 1994;69:115-7.
- 4. Mattingly PC, Bossingham DH. Yellow nail syndrome in rheumatoid arthritis: a report of three cases. Ann Rheum Dis. 1979;38:475-8.
- 5. Guin JD, Elleman JH. Yellow nail syndrome: possible association with malignancy. Arch Dermatol. 1979;115:734-5.
- 6. Scher RK. Acquired immunodeficiency syndrome and yellow nails. J Am Acad Dermatol. 1988;18:758-9.
- 7. Gupta AK, Davies GM, Haberman HF. Yellow nail syndrome. Cutis. 1986;37:371-4.
- 8. Emerson PA. Yellow nail, lymphedema and pleural effusions. Thorax. 1966;21:247-53.
- 9. Siakatos AN, Munkers KD. Recent developments in the isolation and properties of autofluorescent lipopigments. In: Armstrong A, Koppang N, Rider JA. Ceroid lipofuscinosis (Batten's disease). Amsterdan: Elsevier; 1982. p.165-87.
- 10. Glazer M, Berkman N, Lafair JS, Kramer MR. Successful talc slurry pleurodesis in patients with nonmalignant pleural effusion. Chest. 2000;117:1404-9.
- 11. D'Alessandro A, Muzi G, Monaco A, Filiberto S, Barboni A, Abbritti G. Yellow nail syndrome: does protein leakage play a role? Eur Respir J. 2001;17:149-52.
- 12. Desramé J, Béchade D, Patte J H, Jean R, Karsenti D, Coutant G, et al. Syndrome des ongles jaunes associé à des lymphangiectasies intestinales. Gastroenterol Clin Biol. 2000;24:837-40.
- 13. Williams HC, Buffham R, du Vivier A. Successful use of topical vitamin E solution in the treatment of nail changes in yellow nail syndrome. Arch Dermatol. 1991;127:1023-8.
- 14. Luyten C, André J, Walraevens C, De Doncker P. Yellow nail syndrome and onychomycosis. Experience with itraconazole pulse therapy combined with vitamin E. Dermatol. 1996;192:406-8.
- 15. Baran R. The new oral antifungal drugs in the treatment of the yellow nail syndrome. Br J Dermatol. 2002;147:189-91.
Publication Dates
-
Publication in this collection
25 Feb 2010 -
Date of issue
Dec 2009
History
-
Accepted
31 July 2009 -
Received
21 Jan 2009