Abstracts
Two adolescent females and a girl, all with clinically diagnosed vitiligo, were treated with 0.2% 8-methoxypsoralen cream followed by exposure to solar ultraviolet light. One year later, they developed hypopigmented and achromic spots on the areas affected by the vitiligo. Biopsy of skin tissue taken from one of these cases showed a marked reduction in melanin. Clinical and histological findings point to a diagnosis of leukoderma punctata.
Hypopigmentation; Psoralens; Vitiligo
Duas adolescentes e uma menina com vitiligo clinicamente diagnosticado foram tratadas com 8-metoxipsoraleno a 0,2% em creme Lanette com subsequente exposição solar. Um ano após, apresentaram máculas acrômicas na área do vitiligo. A biópsia de pele em um dos casos revelou melanócitos com escassa pigmentação melânica. Os achados clínicos e histológicos sugerem o diagnóstico de leucodermia punctata.
Hipopigmentação; Psoralenos; Vitiligo
COMMUNICATION
IAssociate Professor, School of Medicine, Clementino Fraga Filho Teaching Hospital, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
IISpecialization Course in Dermatology, School of Medicine, Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
Mailing address
ABSTRACT
Two adolescent females and a girl, all with clinically diagnosed vitiligo, were treated with 0.2% 8-methoxypsoralen cream followed by exposure to solar ultraviolet light. One year later, they developed hypopigmented and achromic spots on the areas affected by the vitiligo. Biopsy of skin tissue taken from one of these cases showed a marked reduction in melanin. Clinical and histological findings point to a diagnosis of leukoderma punctata.
Keywords: Hypopigmentation; Psoralens; Vitiligo
Leukoderma punctata (guttata) was first described by Falabella et al. in 1988 1 as multiple hypopigmented, achromic, punctate macules that appeared during and after vitiligo treatment with oral PUVAsol. The thirteen patients described in that report, the majority of whom were female, ranged from 7 to 38 years of age. The numerous rounded or oval macules with well-defined margins and a diameter of 0.5 to 1.5 mm were distributed on the extremities, trunk and occasionally on the face. DOPA and Fontana Masson staining showed a reduced quantity but not an absence of functional melanocytes. Ultrastructural studies showed cell damage inside keratinocytes and also inside melanocytes. These authors hypothesized that the probable causes of leukoderma punctata in their patients were psoralen and the natural phototoxicity of UVA-UVB.
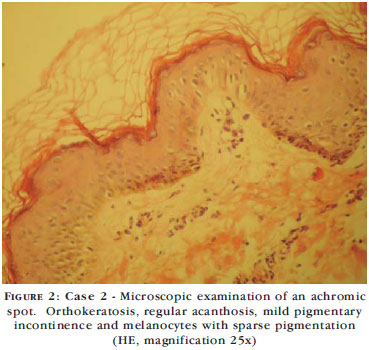
In the period between 1994 and 2008, a condition compatible with leukoderma punctata was found in three cases of vitiligo treated with topical PUVAsol. A 12-year old adolescent girl with segmental vitiligo on her left upper limb and scapular region was treated with 0.2% 8-methoxypsoralen in the form of Lanette cream together with progressively longer sun exposure until reaching a maximum duration of ten minutes. One year later, she presented multiple achromic macules of 1-3 mm on the area affected by the vitiligo. A nine-year old girl with segmental vitiligo on the right thoracolumbar region, who was submitted to the same therapeutic regimen, developed a condition similar to that previously described one year following treatment. Biopsy of the lesion revealed orthokeratosis, regular acanthosis, preserved appendages and vessels, mild pigmentary incontinence and foci of suprapapillary melanocytes with sparse melanin pigmentation (Figures 1 and 2). An eleven-year old girl with generalized vitiligo was treated using the same regimen and developed hypochromic macules on her lower limbs. The therapeutic regimen was discontinued in the three patients and they remained under observation and in use of a low-potency topical corticoid. No treatment has thus far been proposed in the literature.
Photochemotherapy (PUVA) is recognized as a treatment for vitiligo. It consists of the use of topical or systemic psoralen and exposure to ultraviolet light using lamps that emit wavelengths between 320 and 400 nm or natural sun exposure.
Leukoderma punctata has been described as an adverse effect of phototherapy in psoriasis treated with UVB phototherapy 2, in vitiligo treated with PUVA in a PUVA cabin 3, in vitiligo treated with topical PUVAsol 4 and in mycosis fungoides treated with UVB 5.
Idiopathic guttate hypomelanosis is the principal differential diagnosis. This is an acquired condition that affects principally individuals of African descent. It affects males and females equally. It presents well-circumscribed, porcelain-like, rounded or stellate macules measuring 1 mm, 5 mm or 2 cm in diameter. Macules may be few or multiple, increasing in number and size with the age of the patient. They are more common in exposed areas of the extremities, particularly on the front of the lower limbs. They are asymptomatic and irreversible. Histologically, they present flattening of the dermoepidermal junction, a moderate or accentuated reduction in melanin granules in the basal layer and epidermal cristae, epidermal atrophy and hyperkeratosis. There is a moderate reduction in melanocytes. The familial, nonactinic type is located on the trunk, particularly in the case of skin phototype VI.
REFERENCES
- 1. Falabella R, Escobar CE, Carrascal E, Arroyave JA. Leukoderma punctata. J Am Acad Dermatol. 1998;18:485-94.
- 2. Park YK, Hann SK, Hong KT, Kim YC. Generalized punctata leukoderma following UVB phototherapy in the psoriasis patients. Ann Dermatol. 1990;2:93-5.
- 3. Dogra S, Jain R, Parsad D, Handa S. Leukoderma punctatum following systemic PUVA therapy. Int J Dermatol. 2002;41:922-3.
- 4. Park JH, Lee MH. Case of leukoderma punctata after topical PUVA treatment. Int J Dermatol. 2004;43:138-9.
- 5. Kaya TI, Yazici AC, Tursen U, Ikizoglu G. Idiopathic guttate hypomelanosis: idiopathic or ultraviolet induced? Photodermatol Photoimmunol Photomed. 2005;2:270-1.
Leukoderma punctata following topical PUVAsol treatment
Publication Dates
-
Publication in this collection
01 Oct 2010 -
Date of issue
Aug 2010
History
-
Accepted
27 Nov 2009 -
Received
26 Jan 2009