Abstracts
BACKGROUNDS: Although easily diagnosed, molluscum contagiosum may present as a single lesion or as several small, inflamed lesions of difficult diagnosis. OBJECTIVE: To describe the dermoscopic characteristics of molluscum contagiosum and to compare the findings from clinical examination and dermoscopy. METHODS: Histopathologically confirmed lesions were evaluated clinically and dermoscopically in 57 patients. RESULTS: At clinical examination and dermoscopy of 211 lesions, orifices were visualized in 50.24% and 96.68% of the lesions, and vessels in 6.16% and 89.10%, respectively. The vascular patterns found in the 188 lesions in which vessels were found at dermoscopy were the crown (72.34%), radial (54.25%) and punctiform patterns (20.21%). Half of the 188 lesions had a combination of vascular patterns, with the flower pattern (a new vascular pattern) being found in 19.68% of cases. More orifices and vessels were identified at dermoscopy than at clinical examination, including cases with inflammation or perilesional eczema and small lesions. Punctiform vessels were associated with inflammation, excoriation and perilesional eczema. CONCLUSIONS: Dermoscopy performed on molluscum contagiosum lesions proved superior to dermatological examination even in cases in which clinical diagnosis was difficult. The presence of orifices, vessels and specific vascular patterns aids diagnosis, including differential diagnosis with other types of skin lesion.
Dermatology; Diagnostic equipment; Microscopy; Molluscum contagiosum
FUNDAMENTOS: Embora de fácil diagnóstico, o molusco contagioso pode apresentar-se como lesões inflamadas, únicas ou pequenas de difícil diagnóstico. OBJETIVO: Descrever características dermatoscópicas do molusco contagioso e comparar achados do exame clínico e dermatoscópico. MÉTODOS: Avaliou-se clínica e dermatoscopicamente lesões confirmadas pela histopatologia em 57 pacientes. RESULTADOS: Nos exames clínico e dermatoscópico de 211 lesões, foram visualizados orifícios em 50,24% e 96,68% das lesões e vasos em 6,16% e 89,10% delas, respectivamente. Os padrões vasculares encontrados em 188 lesões que apresentaram vasos à dermatoscopia foram coroa (72,34%), radial (54,25%) e puntiforme (20,21%). Metade das 188 lesões apresentou padrão vascular combinado, sendo o padrão em flor (novo padrão vascular) responsável por 19,68%. Foram identificados mais orifícios e vasos no exame dermatoscópico que no clínico, inclusive naquelas com inflamação, eczema perilesional e de tamanho pequeno. Vasos puntiformes relacionaram-se com inflamação, escoriação e eczema perilesional. CONCLUSÕES: A dermatoscopia das lesões de molusco mostrou-se superior ao exame dermatológico mesmo quando seu diagnóstico clínico torna-se difícil. A presença de orifícios, vasos e padrões vasculares específicos auxilia no seu diagnóstico e na diferenciação de outras lesões de pele.
Dermatologia; Equipamentos para diagnóstico; Molusco contagioso
INVESTIGATION
Dermoscopic patterns of molluscum contagiosum: a study of 211 lesions confirmed by histopathology*
Mayra IanhezI; Silmara da Costa P. CestariII; Mauro Yoshiaki EnokiharaIII; Maria Bandeira de Paiva Melo SeizeIV
IMédica colaboradora do Ambulatório de Dermatologia da Universidade Federal de Goiás - Goiânia (GO), Brasil
IIDoutora em Dermatologia - Professora Adjunta do Departamento de Dermatologia da Universidade Federal de São Paulo / Escola Paulista de Medicina (UNIFESP/EPM) - São Paulo (SP), Brasil
IIIDoutor em Dermatologia - Médico colaborador do Ambulatório de Dermatologia da Universidade Federal de São Paulo (UNIFESP/EPM) - São Paulo (SP), Brasil
IVMestre em Dermatologia
Mailing address
ABSTRACT
BACKGROUNDS: Although easily diagnosed, molluscum contagiosum may present as a single lesion or as several small, inflamed lesions of difficult diagnosis.
OBJECTIVE: To describe the dermoscopic characteristics of molluscum contagiosum and to compare the findings from clinical examination and dermoscopy.
METHODS: Histopathologically confirmed lesions were evaluated clinically and dermoscopically in 57 patients.
RESULTS: At clinical examination and dermoscopy of 211 lesions, orifices were visualized in 50.24% and 96.68% of the lesions, and vessels in 6.16% and 89.10%, respectively. The vascular patterns found in the 188 lesions in which vessels were found at dermoscopy were the crown (72.34%), radial (54.25%) and punctiform patterns (20.21%). Half of the 188 lesions had a combination of vascular patterns, with the flower pattern (a new vascular pattern) being found in 19.68% of cases. More orifices and vessels were identified at dermoscopy than at clinical examination, including cases with inflammation or perilesional eczema and small lesions. Punctiform vessels were associated with inflammation, excoriation and perilesional eczema.
CONCLUSIONS: Dermoscopy performed on molluscum contagiosum lesions proved superior to dermatological examination even in cases in which clinical diagnosis was difficult. The presence of orifices, vessels and specific vascular patterns aids diagnosis, including differential diagnosis with other types of skin lesion.
Keywords: Dermatology; Diagnostic equipment; Microscopy; Molluscum contagiosum
INTRODUCTION
Molluscum contagiosum is a viral infection of the epidermal keratinocytes that results in a skin lesion with characteristic intracytoplasmic inclusions. Lesions are generally numerous, characteristically 2-4 mm umbilicated skin-colored papules, with a translucent, glossy appearance, located at various sites on the skin surface. 1
Other factors may hamper diagnosis of molluscum contagiosum, such as: lack of central umbilication, 2 associations with other types of dermatological lesions, 3 atypical lesions, 4 small, single, initial lesions, 5 inflammatory lesions and lesions with perilesional eczema. 6 This difficulty in diagnosing the condition may be present at the initial evaluation, during treatment or in the follow-up of the patient.
Various diagnostic methods may facilitate the clinical diagnosis of lesions resulting from this infection, including dermoscopy. This is a noninvasive technique whose principal application was initially directed towards the early diagnosis of skin melanoma and differentiation with melanocytic lesions; however, it has also been used to describe the characteristics of other dermatoses visible using this technique, including molluscum contagiosum. 7
The dermoscopy pattern described in cases of molluscum contagiosum reported in four publications included the presence of a central yellowishwhite structure and vessels around the lesion (vessels in a crown pattern). 5, 7-9
The objective of the present study was to identify the dermoscopic patterns of molluscum contagiosum and to compare them with the patterns that have already been described.
MATERIAL AND METHODS
A total of 211 lesions found in 57 patients receiving care at a dermatology outpatient clinic for molluscum contagiosum, diagnosed by clinical examination and dermoscopy and confirmed by histopathology between July 2006 and December 2007 were included in the study. Exclusion criteria consisted of curetted lesions with any other histopathological diagnosis.
The study was approved by the institution's Internal Review Board. All the patients or their parents or guardians signed an informed consent form agreeing to participate in the study, permitting photographic documentation to be obtained, dermoscopy to be performed on the lesions and the curetted material to be sent for histopathology, as well as giving their consent to undergo the proposed treatment.
Preferentially, at least one small lesion, two lesions with inflammation or perilesional eczema and two of characteristic size and appearance were selected in each patient with five or more lesions. The presence of inflammation or perilesional eczema was included to permit observation of whether the clinical alterations affect the dermoscopic appearance of molluscum contagiosum or its size.
During clinical examination, data such as the gender and age of the patient, the size of the lesions, the presence or absence of an orifice, vessels, inflammation and/or excoriation and perilesional eczema were recorded. At dermoscopy, the following characteristics were registered: the size of the lesions (in mm), the presence or absence of an orifice and vessels and, if vessels were present, the vascular pattern.
The size of the lesions was determined by a dermoscope and classified according to the following scale: a) small: < 1.5 mm; b) medium-sized: > 1.5 mm and < 3 mm; or c) large: > 3 mm.
The vascular patterns were classified in accordance with the study conducted by Vásquez-López et al. 9 in which the vascular patterns of nontumoral dermatoses visualized at dermoscopy are described.
At least two experienced dermatologists familiar with dermoscopy in molluscum contagiosum made the clinical and dermoscopic diagnoses and performed curettage.
All the lesions selected for the study were photographed twice, clinically and dermoscopically, and the data were recorded and stored. All poor quality digital images were excluded from the study. Sony Cybershot P93 and Canon SD800 digital cameras were used, as well as a Heine Delta 20 dermatoscope attached directly to the aforementioned cameras. Alcohol gel was used at the interface between the skin and the dermatoscope.
Following clinical examination and dermoscopy, curettage of the lesions was performed in all the patients, who were then given written and verbal instructions to be followed in the post-operative period. A return follow-up visit was scheduled during which the histopathology results of the treated lesions were given to the patients. The lesions were analyzed by pathologists from the Pathology Department of the institution.
To avoid bias caused by vasoconstriction induced by the topical anesthesia used at curettage, dermoscopy was performed before the product was administered.
The chi-square test was used to associate clinical changes with vascular patterns. Probability (p) < 0.05 was considered indicative of statistical significance and all tests were two-tailed. All the analyses were calculated using the SPSS (Statistical Package for the Social Sciences) software program, version 11.5.1 for Windows.
RESULTS
Of the 57 patients analyzed, 52.63% were female. Age ranged from 1 to 30 years, with 49.12% of patients being in the 1-5 year age group.
Of the 211 lesions selected, perilesional eczema was found in 33 lesions (15.64%) and inflammation and/or excoriation in 34 (16.12%). With respect to size, of the 211 lesions analyzed by dermoscopy, 108 (51.18%) were considered small, 78 (36.97%) medium-sized and 25 (11.85%) large.
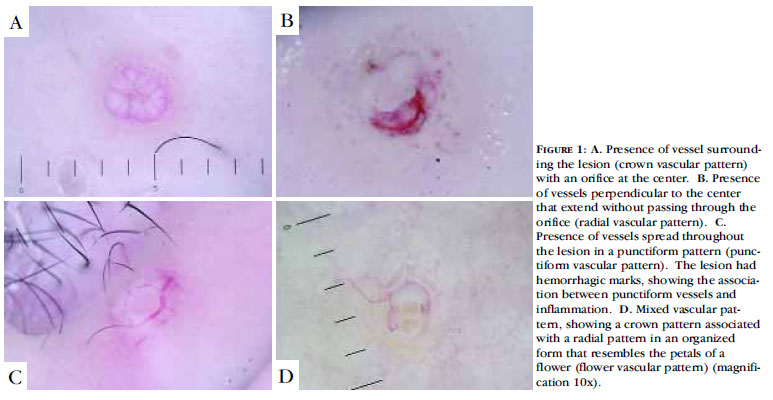
Clinical examination identified the presence of an orifice in 106 lesions (50.24%), while dermoscopy was able to identify this feature in 204 lesions (96.68%). At clinical examination, the presence of vessels was identified in 13 lesions (6.16%), while dermoscopy visualized vessels in 188 lesions (89.10%). The vascular patterns found at dermoscopy in this study are shown in Table 1 and Figure 1.
The presence of an orifice was not associated with the presence of vessels in the lesions analyzed. Comparing those lesions in which an orifice was found with those in which it was not, the proportion of vascular patterns associated with the presence of an orifice was found to be approximately 10-50 times greater than when no orifice was present (Table 2).
In addition to the vascular patterns previously described, combinations of vascular patterns were found that are referred to as mixed vascular patterns. Simple (or single) vascular patterns were found in 102 molluscum contagiosum lesions with vessels (54.26%), while mixed patterns were detected in 86 lesions (45.74%) (Table 3).
Of the 83 lesions with a mixed crown and radial vascular pattern, 37 (19.68% of all the 188 lesions with vessels) had an appearance that resembled the petals of a flower and are therefore described here as having a flower pattern. Table 4 shows the possible combinations of vascular patterns in relation to the presence of vessels and orifices, while Figure 2 shows the patterns of all the lesions included in the study and classified at dermoscopy.
When the vascular patterns were associated with clinical alterations such as inflammation and/or excoriation and perilesional eczema, the proportion of lesions with a punctiform vascular pattern that had inflammation or excoriation was found to be significantly higher compared to those with no inflammation or excoriation (79% versus 8%; c2(1) = 85.1; p<0.001). The proportion of lesions with a punctiform vascular pattern in which eczema was present was significantly higher compared to those without eczema (50% versus 15%; c2(1) = 19.6; p<0.001).
The occurrence of inflammation and/or excoriation was found to be 16 times greater in lesions with a punctiform vascular pattern compared to those with other patterns. Likewise, perilesional eczema was 4.4 times more common in the lesions with a punctiform vascular pattern.
DISCUSSION
Although the clinical diagnosis of molluscum contagiosum is considered simple, up to the present moment more than 40 types of lesions have been described as differential diagnoses (Chart 1). 2,10 Dermoscopy is a diagnostic method that is simple to perform, fast and relatively inexpensive; furthermore, it can be used routinely in the doctor's office.
Dermoscopy for molluscum contagiosum was first described by Vásquez-López et al. in 2004. 9 Since then, only three more papers 5,7,8 have described the use of dermoscopy in this condition, with a total of 20 lesions having been classified in all. In these studies, the only vascular pattern described in molluscum contagiosum lesions was the crown pattern (15/20 lesions; 75%). The vascular patterns found in the present study were classified in accordance with the study published by Vásquez-López et al. 9 on vascular patterns in nontumoral dermatoses. In addition to the crown vascular pattern, two other patterns, the radial and punctiform patterns, were detected in the present analysis.
Zaballos et al. 5 and Morales et al. 8 reported a total of five molluscum contagiosum lesions with vessels in a crown pattern and stated that this pattern was accompanied by vessels that extended through the amorphous structure of the lesions towards their core, without crossing it. These authors may have been referring to the vascular pattern known as radial, although they did not use this term.
Punctiform vessels, presented as small reddish dots inside the lesion, have been described in numerous diseases such as melanoma and clear cell acanthoma, 11 in 80% of lichen planus lesions 12 and also in eccrine poroma 13, but have not yet been reported in molluscum contagiosum lesions. In the present study, 20.21% of the lesions had this type of vascular pattern. Although common in this study, this pattern may never have been described in molluscum contagiosum lesions simply because few studies on dermoscopy in molluscum contagiosum have been reported in the literature up to the present moment. Furthermore, the selection of the lesions in the present study included those with inflammation and perilesional eczema, clinical alterations that were found to be associated with the punctiform pattern.
In their study on the dermoscopic evaluation of the vascular patterns of nontumoral dermatoses, Vásquez-López et al. 9 referred to single or mixed vascular patterns. Nevertheless, only Zaballos et al. 5 and Morales et al. 8 referred to mixed vascular patterns when they described five molluscum contagiosum lesions with vessels that surrounded the lesion and others that extended towards its core. In the present study, 45.74% of the lesions had mixed vascular patterns of which the most common was the crown + radial pattern, as described but not named by Zaballos et al. 5 and Morales et al. 8 The mixed vascular pattern described here as a flower pattern has not been described in any other study and is probably specific to molluscum contagiosum lesions.
In the previous studies carried out using dermoscopy in molluscum contagiosum, no clinical description was ever made of an orifice; however, at dermoscopy, this structure was presumed to represent the central area of the lesion, composed of yellowish or yellowish-white material. In the present study, orifices were not always found in the molluscum contagiosum lesions at dermoscopy; indeed this type of structure was absent in 3.32% of the lesions examined. When present, the orifice showed two types of morphology: the type already described, with yellowish-white material at its center, and another type with a homogenous orifice and no structures visible at its core, consisting only of a rounded area of uniform color. Since the presence of the orifice is an important characteristic in identifying molluscum contagiosum lesions and considering that the orifice is undetectable clinically in many cases, dermoscopy becomes fundamental in those cases in which the orifice is not perceptible at clinical examination.
Vessels were found in 15 of the 20 previously reported molluscum contagiosum lesions evaluated by dermoscopy (75%). Contrary to the orifice, the presence of vessels was rarely identified when only clinical examination was performed, being detected in only 13 of the 211 lesions in the present study (6.16%). No reference was made to the detection of vessels using the naked eye in any of the studies on molluscum contagiosum, even the epidemiological studies. The best-known and most frequently used reference for the diagnosis of molluscum contagiosum refers only to the central orifice. However, in the present study, dermoscopy permitted identification of the presence of vessels in 188 of the 211 lesions evaluated (89.10%), showing that the principal advantage of this diagnostic technique lies in its ability to identify vessels, since the orifice is more often visible at clinical examination and consequently, at dermoscopy.
The majority of molluscum contagiosum lesions with inflammation and/or excoriation and perilesional eczema were found to have a punctiform vascular pattern, and the difference between these and the lesions with no clinical alterations was statistically significant.
Vessels with a punctiform pattern are known to be more common in inflammatory lesions such as lichen planus. 12 However, since they had not been reported previously in molluscum contagiosum, it was impossible to compare the results of the present study with data from the literature. Although inflammation and excoriation were found in this study to be more commonly associated with punctiform vessels, this vascular pattern was also found in lesions without these characteristics.
Even though no direct evidence exists that inflammation is associated with immunity, there is a theory that the papules disappear after becoming inflamed. 14 Two patients in the present study presented this phenomenon of regression, their lesions having become inflammatory with a punctiform vascular pattern. Kipping 6 also reported the disappearance of molluscum contagiosum lesions following the onset of eczema and inflammation. One hypothesis is that punctiform vessels may also precede regression of molluscum contagiosum lesions, just as inflammation and perilesional eczema do. Nevertheless, with the data obtained up to the present moment, it is unknown whether regression may also occur in the case of lesions with no inflammation or eczema but with punctiform vessels.
CONCLUSION
The vascular patterns of molluscum contagiosum identified in this study are: crown, punctiform and radial patterns in addition to the mixed flower pattern, recognized for the first time and named in the present study. The punctiform pattern was principally associated with lesions with alterations such as inflammation and/or excoriation and perilesional eczema.
The presence of vessels and orifices detected at dermoscopy increases suspicion that the lesions analyzed consist of molluscum contagiosum. An association of the presence of vessels with the vascular patterns most often found in molluscum contagiosum may assist the examiner in reaching the correct diagnosis. Therefore, dermoscopy is becoming more and more indispensable as a tool for the identification of molluscum contagiosum lesions that are difficult to diagnose.
REFERENCES
-
1Brown J, Janniger CK, Schwartz RA, Silverberg NB. Childhood molluscum contagiosum. Int J Dermatol. 2006;45:93-9.
-
2Hanson D, Diven DG. Molluscum contagiosum. Dermatol Online J. 2003;9:2.
-
3Duarte AA, Cucé LC. Molusco contagioso ocorrendo em cisto epidérmico. An Bras Dermatol. 1990;65: 145-6.
-
4Lewis EJ, Lam M, Crutchfield CE 3rd. An update on molluscum contagiosum. Cutis. 1997;60:29-34.
-
5Zaballos P, Ara M, Puig S, Malvehy J. Dermoscopy of molluscum contagiosum: a useful tool for clinical diagnosis in adulthood. J Eur Acad Dermatol Venereol. 2006;20:482-3.
-
6Kipping HF. Molluscum dermatitis. Arch Dermatol. 1971;103:106-7.
-
7Zalaudek I, Giacomel J, Cabo H, Di Stefani A, Ferrara G, Hofmann-Wellenhof R, et al. Entodermoscopy: a new tool for diagnosing skin infections and infestations. Dermatology. 2008;216:14-23.
-
8Morales A, Puig S, Malvehy J, Zaballos P. Dermoscopy of molluscum contagiosum. Arch Dermatol. 2005;141:1644.
-
9Vázquez-López F, Kreusch J, Marghoob AA. Dermoscopic semiology: further insights into vascular features by screening a large spectrum of nontumoral skin lesions. Br J Dermatol. 2004;150:226-31.
-
10Gottlieb SL, Myskowski PL. Molluscum contagiosum. Int J Dermatol. 1994;33:453-61.
-
11Blum A, Metzler G, Bauer J, Rassner G, Garbe C. The dermatoscopic pattern of clear-cell acanthoma resembles psoriasis vulgaris. Dermatology. 2001;203:50-2.
-
12Vázquez-López F, Manjón-Haces JA, Maldonado-Seral C, Raya-Aguado C, Pérez-Oliva N, Marghoob AA. Dermoscopic features of plaque psoriasis and lichen planus: new observations. Dermatology. 2003;207:151-6.
-
13Altamura D, Piccolo D, Lozzi GP, Peris K. Eccrine poroma in an unusual site: a clinical and dermoscopic simulator of amelanotic melanoma. J Am Acad Dermatol. 2005;53:539-41.
-
14Steffen C, Markman JA. Spontaneous disappearance of molluscum contagiosum. Report of a case. Arch Dermatol. 1980;116:923-4.
Publication Dates
-
Publication in this collection
21 Mar 2011 -
Date of issue
Feb 2011
History
-
Received
20 Nov 2009 -
Accepted
11 Dec 2010