Abstracts
The development of a Brazilian National Surveillance System in 1975 led to a compulsory reporting of selected infectious diseases aiming to reduce the burden of these events in the country. However, shifts in the epidemiology of these diseases associated with modern life style, demand constant revision of surveillance activities. In this manuscript we present the epidemiology, trends and differential diagnosis of the following compulsory notifiable diseases in Brazil: Aids, dengue fever, hanseniasis, American tegumentary leishmaniasis, measles, rubella and congenital rubella syndrome and syphilis. Additionally, the current challenges for control and prevention of each disease are presented
Acquired immunodeficiency syndrome; Brazil; Dengue; Epidemiologic surveillance; Leishmaniasis; cutaneous; Leprosy; Measles; Rubella; Rubella syndrome; congenital; Syphilis
A estruturação do Sistema Nacional de Vigilância Epidemiológica do Brasil, em 1975, tornou obrigatória a notificação de algumas doenças transmissíveis com o objetivo de reduzir a carga destes eventos no país. Entretanto, as alterações no perfil epidemiológico destas doenças, associadas a características da sociedade contemporânea, determinam a constante adequação das atividades de vigilância a este cenário. Neste manuscrito, são descritos epidemiologia, tendências e diagnóstico diferencial das seguintes doenças dermatológicas de notificação compulsória no Brasil: aids, dengue, hanseníase, leishmaniose tegumentar americana, sarampo, rubéola e síndrome da rubéola congênita e sífilis. Também são apresentados os principais desafios atuais para o controle e prevenção para cada uma dessas doenças no Brasil
Brasil; Dengue; Hanseníase; Rubéola; Sarampo; Sífilis; Síndrome de imunodeficiência adquirida; Síndrome da rubéola congênita; Vigilância epidemiológica
SPECIAL
Dermatological diseases of compulsory notification in Brazil*
Gerson Oliveira PennaI; Carla M. A. S. DominguesII; João Bosco Siqueira JrII,III; Ana Nilce S. M. ElkhouryII; Michella P. CechinelII; Maria Aparecida de Faria GrossiII; Marcia de Leite S. GomesII; Joana M. SenaII; Gerson Fernando Mendes PereiraII; Francisco Edilson F. Lima JúniorII; Teresa Cristina Vieira SegattoII; Flavia Cardoso de MeloII; Fabiano Marques RosaII; Marcia Mesquita SilvaII; Renata Amadei NicolauIII
IDermatologist, PhD in Tropical Medicine, Research Physician of the Tropical Medicine Unit of the Universidade de Brasília. Health Surveillance Secretary of the Ministry of Health from April 2007/January 2011 - Brasília (DF), Brazil
IIDepartment of Epidemiologic Surveillance of the Health Surveillance Board of the Ministry of Health - Brasília (DF), Brazil
IIIDepartment de Collective Health / Universidade Federal de Goiás - Goiânia (GO), Brazil
Mailing address
ABSTRACT
The development of a Brazilian National Surveillance System in 1975 led to a compulsory reporting of selected infectious diseases aiming to reduce the burden of these events in the country. However, shifts in the epidemiology of these diseases associated with modern life style, demand constant revision of surveillance activities. In this manuscript we present the epidemiology, trends and differential diagnosis of the following compulsory notifiable diseases in Brazil: Aids, dengue fever, hanseniasis, American tegumentary leishmaniasis, measles, rubella and congenital rubella syndrome and syphilis. Additionally, the current challenges for control and prevention of each disease are presented.
Keywords: Acquired immunodeficiency syndrome; Brazil; Dengue; Epidemiologic surveillance; Leishmaniasis, cutaneous; Leprosy; Measles; Rubella; Rubella syndrome, congenital; Syphilis
INTRODUCTION
As defined by the Organic Health Law (Law 8.080/90), the epidemiologic surveillance is "the group of activites that permits the gathering of indispensable information in order to know, at any moment, the behaviour or natural history of the diseases, as well as to detect or foresee alterations of their conditioning factors, aiming at the timely recommendation of adequate and efficient measures for prevention and control of particular diseases."
In Brazil this concept was initially used in programs for control of malaria, yellow fever and, mostly, on the Smallpox Eradication Campaign (SEC) from 1966 to 1973, coordinated by the Ministry of Health. The experience with SEC motivated the application of the principles of epidemiologic surveillance to other diseases preventable by vaccination. In 1969, a weekly disease notification system was organized based on the network of permanent health units, under the coordination of the State Secretariats of Health. The information of interest from this system went on to be released regularly by the Ministry of Health, by ways of a fortnightly epidemiologic bulletin. 1
With the eradication of smallpox the epidemiologic surveillance established itself as a relevant public health tool in the country. The National System of Epidemiologic Surveillance - NSES was established under specific legislation by the Law number 6259 from 30/10/1975 and the Decree number 78.231 from 12/08/1976, making the notification of some transmissible diseases compulsory. This way, the first national list of compulsory notifiable diseases was created, including those preventable by vaccination, transmissible by vectors, tuberculosis, hanseniasis, and, later on, meningococcal disease and human rabies.
With the creation of the National Program of Immunization in 1977, it became necessary to monitor questions related to vaccine coverage, distribution network, storage and conservation of vaccines as well as to organize a national system of information for the epidemiologic surveillance, in order to make possible the evaluation of the results and the impact of the actions. The vaccination and notification of the cases then become a routine activity of the basic health network, structured in programs with actions coordination and execution in a centralized form, under the coordination of the Ministry of Health.
During the eighties, along with the process of building the Unified Health System (UHS), there was also the decentralization of the surveillance actions and the empowering of the municipal systems of epidemiologic surveillance, requiring the capacitating of human resources with techno-managerial capabilities to understand the epidemiologic situation of their designated area, propitiating the development of organized actions based on the needs of their areas.
Within this perspective there was a restructuring of the NSES in order manage the heterogeneity of the many events under surveillance on the municipal sphere, in face of the transformation of the epidemiologic profile of transmissible diseases on Brazil. Diseases like measles, whooping cough, diphtheria, and accidental and neonatal tetanus tend to decline while other diseases like viral hepatitis, leishmaniasis, malaria, tuberculosis and hanseniasis stay at the same level. On the other hand, new diseases considered emergent or emergent offences become a public health problem.
This way, the list of diseases of compulsory notification goes under systematic revisions, aiming to encompass health problems other than diseases preventable by immunization or those caused by vectors. Other criteria are taken into account in order to establish the compulsory notification of the cases:
Magnitude: frequency, incidence/prevalence and lost years of life.
Potential of dissemination: transmissibility of the disease.
Transcendency: clinical and epidemiologic characteristics like: severity (lethality, hospitalizations and sequelae), social relevance (stigmatization and fear) and economic relevance (loss of lives, work absenteeism, cost of the treatment).
Vulnerability: existence of specific instruments for prevention and control.
International commitments: deals agreed between the Brazilian government and member countries of OPAS/WHO.
Epidemics, Outbreaks and Unexpected Offenses.
It is within this context that the dermatological diseases of compulsory notification are monitored, aiming at the formulation and evaluation of health policies, plans and programs, supporting the process of decision making, in order to contribute to the improvement of the health situation of the population.
Nowadays, the diseases and outbreaks follow the rules of the new International Sanitary Regulation (ISR), approved at the World Assembly of Health Ministers in 2005 and ratified by Legislation Decree number 395 in June 2009, from the Brazilian Federal Senate. In order to keep in line with the ISR, the Ministerial Act number 2472 from 31 August 2010, containing 44 events, regulates the compulsory notification of a large list of diseases and offenses in our country, including some dermatological diseases that will be discussed below. The integral text of this act is available at www.saude.gov.br/sinanweb.3
2. DERMATOLOGICAL DISEASES OF COMPULSORY NOTIFICATION
2.1 Aids
The acquired immunodeficiency syndrome is caused by a retrovirus of the Lentiviridae family, HIV1 e HIV-2. Those affected by the human immunodeficiency virus (HIV) progress to a severe dysfunction of the immunologic system, as the CD4+ T lymphocytes, one of the virus target cells, are being destroyed.
The criteria adopted by the Ministry of Health for the case definition of AIDS are specified on the Guide to Epidemiological Surveillance, available at www.aids.gov.br 4
In a nutshell, in any individual aged 13 years or older, for the purpose of epidemiologic surveillance they are: a) Adapted CDC Criteria; b) Rio de Janeiro/Caracas Criteria; and, Exceptional Death Criteria.
For the purpose of epidemiologic surveillance of AIDS in cases in individuals younger than 13 years the Ministry of Health uses two criteria for case definition: a) Adapted CDC Criteria; and, b) Exceptional Death Criteria.
2.1.1 Epidemiology
Aids represents one of the greatest public health problems, due to its pandemic characteristic and its severity. According to the World Health Organization parameters 5, the HIV/aids epidemic in Brazil is concentrated, because of the prevalence rates of HIV infection higher than 5% in populations of added risk, like injectable drug users, men who have sex with men, sex industry professionals, and less than 1% on the general population. In Brazil, the prevalence of HIV infection is 0,61% on the population aged between 15 and 49 years (0,41% for women and 0,82% for men), stable since 2004. 6 It is estimated that 630 thousand people currently live with HIV/Aids. With the introduction of the antiretroviral therapy, in association with early diagnosis and adequate treatment, the WHO included AIDS on the category of chronic and treatable conditions.
In Brazil, since the identification of the first case of AIDS in 1980, up to June 2009, around 544 thousand cases of the disease have been identified, and around 80% of the cases are concentrated on the Southeast and South regions. After a peak in 2002, the AIDS incidence had a drop on the Southeast region, having stabilized on the Center-West region and increased on the other regions over the last few years of 2000 (Table 1).
The sex ratio (M: F) in Brazil dropped considerably from the start of the epidemic to current days: in 1986 the ratio was 15,1:1 and, from 2002, it stabilized at 1,5:1. The analysis of the sex ration in young people from 13 to 19 years stands out. In this age bracket the number of AIDS cases is higher in women, and the ratio observed since 1998 is 0,8:1. Over the last decade an average of 11 thousand deaths per year has being observed in the country, and the mortality coefficient has been around 6, 0 deaths per 100 thousand inhabitants since 2000.
2.1.2 Challenges
After around 30 years of the HIV/Aids epidemic, and despite the advances obtained when fighting it, there are still many challenges to be confronted. Amongst those, the decrease of the vertical transmission that has been acknowledged in all states and districts, the continuous need to recognize the diverse cultural, social and political contexts where AIDS is dealt with and the implementation of prevention and stigma reduction campaigns. The country seeks selfsufficiency on the production of antiretrovirals and improvement for the development of an infrastructure that ensures the assistance and respect to people living with HIV and AIDS. One of the main challenges for the government is to increase the coverage for tests to detect the HIV and encourage the population to test itself. It is estimated that, in Brazil, 250 thousand people are HIV carriers; however they are not aware of their serologic profile.
2.2 Dengue Fever
Dengue fever is an acute febrile disease caused by an RNA genome virus of the Flavivirus genus and transmitted by infected mosquitoes of the Aedes genus, being the Aedes aegypti its principal vector. Four serotypes are known: DENV1-4, with the clinical manifestations of the disease varying from asymptomatic infection to more severe forms with hemorrhagic signs and shock, which can even progress to death. 7
Between 2001 and 2006, more than 3.4 million cases of the disease were notified in the Americas, with 79.664 cases of hemorrhagic dengue fever and 982 deaths. In 2007 more than 890.000 cases were notified in America, from which 26.000 were hemorrhagic dengue fever. 8
A suspect case of Classic Dengue Fever is a patient with an acute febrile disease, lasting for a maximum of 7 days, associated with at least two of the following symptoms: headache, retro orbital pain, myalgia, arthralgia, prostration and exanthema. The cases are confirmed by serology (Elisa-IgM) during non-epidemic periods or by clinical-epidemiologic criteria during outbreaks of the disease. One confirmed case of Hemorrhagic Dengue Fever (HDF) is confirmed by the presence of all of these criteria: 1. Fever lasting up to 7 days; 2. Thrombocytopenia (<= 100.000/mm3); 3. Spontaneous or induced hemorrhagic manifestations; 4. Plasma extravasations, due to increased capillary permeability, manifested as: hematocrit showing increment of 20% from the base value or drop in 20% after treatment; or presence of cavitary effusion; or hypoproteinemia, and 5. Specific laboratory confirmation (serology or isolation). A case of Dengue with Complications (DWC) is any suspect case of dengue fever that progresses to a severe form but do not present ALL the criteria of HDF. The presence of ONE of the following clinical or laboratorial alterations is enough to close the case as DWC: neurologic alterations; cardio-respiratory dysfunction; hepatic insufficiency; important (voluminous) digestive hemorrhage; pleural or pericardic effusion and ascites; plaquetopenia lower than 20.000/mm3; leukometry equal to or below 1.000/mm3; or suspect case of dengue fever that progresses to death.
2.2.1 Epidemiology
In Brazil a seasonal pattern for the occurrence of dengue fever has been observed, which coincides with summer, due to the occurrence of heavier rains and increase of temperature. Between the years of 2000 and 2009, around 4 million cases of dengue fever were notified, in special in the years of 2002 and 2008, when the largest epidemics registered during this decade were observed (Chart 1).
Up to the year of 2005 the occurrence of dengue fever in the country could be classified in two distinct periods: epidemic waves developing in great urban centers (1986-1993) and epidemic/endemic circulation of the virus in all regions of the country (1994-2005). 9,10 The year 2006 marks the beginning of the third period of the occurrence of dengue fever in the country, characterized by the migration of the severity to children, 11 reaching the highest point with the epidemic that occurred in 2008, specially on the state of Rio de Janeiro. A possible explanation for this scenario can be found on the re-emergency of the DENV2 serotype. This serotype circulated in the country during the 90's without a marked predominance throughout those years. On the other hand, a significant part of the population living on the country had contact with the DENV3 during the great epidemics caused by this serotype between the years 2002 to 2006. The occurrence of new epidemics by DENV2 after a great circulation of DENV3 increases the chances of the development of secondary infections and more severe cases of the disease, as observed in other countries.
Currently we have the circulation of the serotypes 1, 2 and 3 of the virus in Brazil, but is has been observed that the circulation of one serotype usually predominates over the others. However, the alternation of predominating serotypes has caused transmission cycles that peaked in 1998 (DENV1), 2002 (DENV3) and 2008 (DENV2) (Chart 1). It should be highlighted that from the second semester of 2009 the DENV1 of the virus began to be isolated again in many states of the country, which represents a new cycle of transmission of this serotype, which has not circulated intensely since 2002.
In August 2010 the DENV4 was re-introduced on the North region of Brazil (state of Roraima). The genomic sequencing showed that the virus came from Venezuela. As there has been no circulation of this serotype in our country for 28 years, all Brazilians, in theory, are susceptible to dengue fever by the DENV4. GRAPH
With this scenario, the map for the risk of epidemics by dengue fever in its seasonality 2010/2011 is shown on figure 1.
2.2.2 Challenges
The main challenge for the prevention and control of dengue fever is in keeping the infestation by the Aedes aegypti in levels sufficiently low in order to avoid the transmission of the disease. In order to do so a joint effort from all the society, not only the health sector is necessary. Improvements on the infrastructure of the urban centers, identification and adoption of sustainable strategies aiming at changing the habits and behavior of the population in relation to mosquito breeders in residences and the effective integration of the components of dengue fever prevention: epidemiology, entomology, laboratory, education and social mobilization, become necessary.
For the epidemiologic surveillance, the challenge resides on the early identification of the occurrence of cases in order to adopt measures to cut short the transmission of the disease. Therefore, it is necessary that the notification of cases is done in a timely fashion by the health units and a rapid exchange of information between surveillance and vector control on the districts with disease transmission.
2.3 Hanseniasis
It is an infectious disease of compulsory notification all over the national territory, with chronic evolution, caused by the Mycobacterium leprae, a bacillus with predilection to the skin and peripheric nerves, characterized by typical clinical manifestations, making its diagnosis simple in most cases. However, it can be mistaken by other neuropathies and dermatosis. 12
Hanseniasis is part of the diseases of compulsory notification group due to its magnitude, transcendence, the risk of causing disability and deformities, and because it is a transmissible disease amenable to treatment and control. The disease has low vulnerability due to the existence of a specific vaccine, developing, mostly, in young adults and causing high economic losses, both direct, in relation to treatment and rehabilitation and indirect, in relation to loss of productive years, as well as the social stigma still attached to the disease. 12, 13
In the article, "Perfil nosológico das consultas dermatológicas no Brasil" ("Nosological profile of dermatologic consultations in Brazil") published by the Brazilian Society of Dermatology, 14 involving 932 dermatologists and 49 services that offered medical residency in dermatology, in a total of 57 thousand dermatological consultations, hanseniasis was the 20th cause of consultation all over the country, and the 4th on the Center-West region. The results reinforce the importance of hanseniasis as a public health problem in Brazil, for which a continuous investment in health education is necessary.
2.3.1 Epidemiology
The World Health Organization registered, in 2009, 244.796 new cases of hanseniasis in 141 countries, 93% of those notified in 16 countries: Bangladesh, Brazil, China, Congo, Ethiopia, India, Indonesia, Madagascar, Mozambique, Myanmar, Nepal, Nigeria, The Philippines, Sri Lanka, Sudan and Tanzania. 15 Brazil was responsible for 37.610 of these new cases, meaning a detection rate of 19, 64 new cases for each 100.000 population. From this total, 7, 1% of the cases were younger than 15 years and 7, 2% were diagnosed in a later stage, already with deformities.
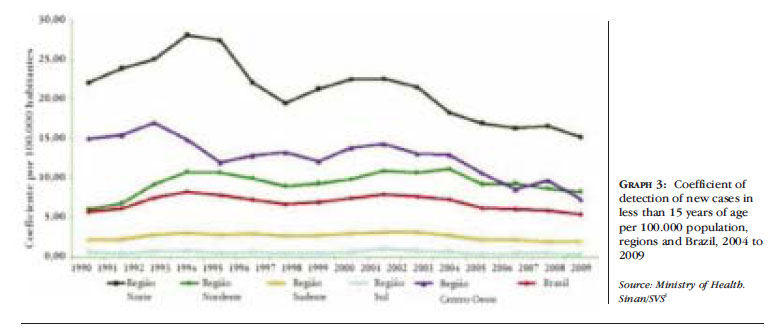
In the period from 2004 to 2009, hanseniasis had a tendency to stabilization of the general detection and in those less than 15 years in Brazil, but still at very high levels on the North, Northeast and Center-West regions (Charts 2 and 3). This scenario strengthens the effort to reach the target of the Ministry of Health, which proposes to reduce hanseniasis in those less than 15 years.
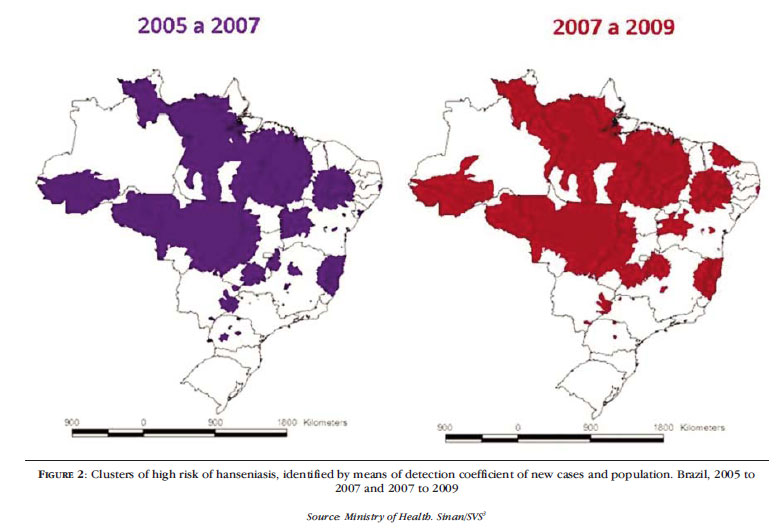
The 10 greatest concentrations of cases with indication of active transmission in the country included 1.173 districts with 53, 5% of the new cases detected on the period from 2005 to 2007 and only 17, 5% of the country population. Historical and social determinants, coupled with the occupation of the Legal Amazon and the maintenance of social inequities on the Northeast region help explain the accumulation of infected people, this being a disease with long incubation period. (Figure 2). 10, 16
2.3.2 Challenges
The principal challenges for the control of hanseniasis in the country are: the intensification of epidemiologic surveillance on the most endemic areas, the maintenance of effective actions on those with stabilization of the endemic, the strengthening of the decentralized administration in states and districts, the guarantee of integral attention to the person with hanseniasis and/or their sequelae, the amplification of control actions within a network of care (including from primary to specialized out-patients and hospital attention), social mobilization and the amplification of partnerships with universities, scientific institutions, professional class entities and nongovernmental organizations, with effective participation of the social control. 17
2.4 American Tegumentary Leishmaniasis
The American Tegumentary Leishmaniasis (ATL) is an infectious disease of the skin and mucosa and the etiologic agent is a protozoa from the genus Leishmania.18, 19 Its transmission happens via the bite of infected female phlebotomies, involving different species in close association with parasites and reservoirs, shaping the links of the diverse transmission cycles that occur on the national territory.20, 21 Since the decade of 1980, a process of geographic expansion of the transmission of the disease have been developing, with occurrence in all of the country federal units nowadays, with a change of the epidemiologic profile of the disease. 18, 22
In Brazil and in other New World countries, its importance resides not only on the high incidence and broad geographic distribution, but also on the possibility of assuming forms that can determine destructive, disfiguring and also disabling lesions, with serious repercussion on the individual's psychosocial profile. 23 Timely and adequate treatments are very important in order to prevent the evolution of the disease to more destructive and severe forms, like the mucosal form. 24
The suspected cases of tegumentary leishmaniasis are defined by the following forms 4:
Clinical cutaneous form: individual with the presence of cutaneous ulcer, with granulose floor and frame-like infiltrated borders;
Clinical mucosa form: individual with the presence of ulcer on the nasal mucosa, with or without perforation or loss of the nasal septum, that can involve lips, palate and nasal pharynx.
The cases are confirmed according to the following criteria:
Residence, origin or travel within/to area of confirmed transmission and finding of the parasite in direct or indirect parasitological exams;
Residence, origin or travel within/to area of confirmed transmission and positive Montenegro intradermal reaction (MIR);
Residence, origin or travel within/to area of confirmed transmission with other positive methods of diagnosis.
Epidemiology
Between 1999 and 2008 269.122 cases of ATL were registered, with an annual average of 26.912 cases. The disease occurs predominantly in adult males, although, recently, a higher occurrence in children, regardless of gender, has been documented. These last findings suggest a change on the pattern of the transmission of the disease, probably due to changes on the behavior of the vector mosquito, reinforcing the importance of peridomicile or intradomicile transmission. 24, 25 The chart 4 presents the total cases of ATL according to the country regions between 2000 and 2009 and the figure 3 the expansion of the disease in Brazil.
2.4.2 Challenges
The tegumentary leishmaniasis is considered a neglected disease, generally occurring in people with low socio-economic status, with weak political strength and not very appealing to the pharmaceutical industry. The medications currently employed on the treatment of this endemic frequently cause adverse effects. After clinical studies the Ministry of Health approved the medication miltefosina for oral use in Brazil which, in order to be implemented on the control program, awaits the regularization of its registration with the ANVISA by the manufacturing laboratory. This medicament has being used by other countries that deal with this endemic.
The actual challenges to ATL are: a) increase the investments on the search of drugs with better efficacy, safety, low cost, easiness of administration and sustainability; b) keep the adverse effects of the medications under surveillance; c) broaden the health network for the early diagnosis and adequate treatment of the cases; d) investigate and evaluate the deaths; e) implement actions of surveillance in territorial units; f) amplify the actions of entomologic surveillance.
2.5 Measles
It is an acute infectious disease, caused by a virus, severe, transmissible and extremely contagious. Amongst the infect-contagious diseases measles is considered one of the principal causes of morbiditymortality in children under five years, above all in those who are malnourished and who live in underdeveloped countries.4 The infection by the measles virus compromises the host's resistance, facilitating the occurrence of other infections (viral or bacterial), that can progress with high lethality pneumonia, diarrhea leading to dehydration and to worsening of malnutrition and to neurologic complications like encephalitis and meningo- encephalitis, with mortality rates that can reach 10%. The sub acute sclerosing panencephalitis (SSPE) develops rarely, in a proportion of 1 case to each million cases of measles, after approximately seven years of the disease, and it is irreversible, leading to death. The complications of measles can also leave sequelae like: decrease of mental capacity, blindness, deafness and mental retardation. 3
A suspect case of measles is any patient that, independently of the age and vaccine status, presents with fever and maculo-papular exanthema, associated with one or more of the following signs and symptoms: cough and/or nasal discharge and/or conjunctivitis. Due to the Certification of elimination of the transmission of the wild-type virus of measles and rubella until 2012, all confirmed cases of the disease must have laboratorial classification. Imported cased of the disease might occur, mostly from countries outside the American continent that still have transmission of the wild type virus or that are still at the stage of reducing the mortality by measles (Africa).
2.5.1 Epidemiology
Since 1992 various efforts have been made for the elimination of the disease in Brazil. From 1999, with the implementation of the Measles Elimination Plan, the launch of follow-up campaigns (2000 and 2004), the intensification of epidemiologic surveillance activities and follow-up of the epidemiologic surveillance quality indicators, the country has confirmed the last case of wild type measles in the state of Mato Grosso do Sul in 2000. Since that date only confirmed cases of imported virus were detected.
Between 2001 and 2009, 67 imported cases were confirmed in the country. The last outbreak occurred in 2006 on the state of Bahia with 57 confirmed cases; the D4 virus, which circulates in European countries, was identified. All cases of measles confirmed in the country were in non-vaccinated people, indicating that the vaccine is still the best and the greatest protection against the disease and continuous efforts from all sectors of the civil and the academic society must be maintained (Chart 5).
All public health state laboratories perform the laboratorial diagnosis of the disease, including measles, rubella and Congenital Rubella Syndrome IgM and IgG antibodies test, as well as the differential diagnosis with dengue fever, Parvovirus B19 and Herpes Virus 6. The elimination of the transmission of the wild type virus is a sustainable reality and should be certified by the Pan American Health Organization until 2012.
2.6 Rubella and Congenital Rubella Syndrome
This is an acute viral exanthematic disease, highly contagious, afflicting mostly children. A suspect case of rubella is any patient who presents with fever and maculo-papular exanthema, associated with retro auricular, occipital and cervical lymphadenopathy, independently of age and vaccine status. A confirmed case of rubella can be defined by the laboratory, epidemiologic and clinical aspects. 4
The Congenital Rubella Syndrome (CRS) develops when the pregnant woman is sick with rubella and the virus is transmitted though the placenta, with infection of the placenta and the fetus soon after the maternal viremia. The infection can result in various types of malformation depending on the stage the viremia occurred. By infecting the fetus the virus produces a chronic infection that can represent an important source of dissemination of the virus for a period of over one year. A suspect case of CRS is any newborn whose mother was a confirmed case of rubella or had contact with a confirmed case of rubella during gestation and/or any child up to 12 months of age who presents with clinical signs compatible with congenital infection by the rubella virus independently of the maternal history. The clinical signs are represented by congenital cardiopathy (persistence of the arterial canal, aortic and pulmonary stenosis), congenital glaucoma/cataract and deafness. The confirmation of the CRS must be laboratorial and clinical specimens (nasal pharynx and urine swab) must be collected for viral identification.
2.6.1 Epidemiology
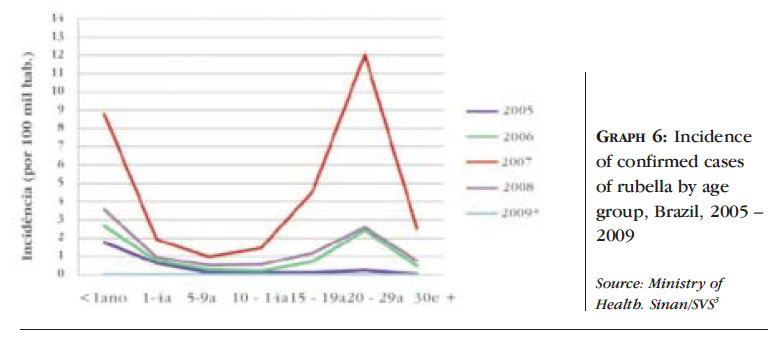
In order to eliminate rubella and the CRS, Brazil launched the National Vaccination Campaign against Rubella in 2008, when around 70 million people were vaccinated. Between 2007 and 2008 10.654 cases of rubella were confirmed and in 2009 no case of the disease was confirmed, an indication that the vaccination campaign had an impact in relation to the transmission of the pos-natal rubella virus. During that period 50 cases of CRS and 25 of ICR were confirmed. In 2009 12 cases of CRS and 7 of ICR were confirmed, which indicates for the surveillance system an alert call for new cases of rubella due to the existence of children eliminating the virus for at least 18 months after their birth. This way, the intensification of the epidemiologic surveillance of rubella must remain active till the end of 2011. The cases of CRS and ICR in 2009 were those in mothers who got sick in 2008 during the outbreaks of rubella in the country. Cases of rubella occurred on the age bracket of adolescents and young adults (14 to 39 years of age) in both sexes. (Chart 6).
2.6.2 Challenges
The challenges faced by the epidemiologic surveillance of exanthematic diseases are to maintain the elimination of the circulation of the measles virus, to break the endemic transmission of the rubella virus and to reach the target of elimination of rubella and congenital rubella syndrome in the country.
2.7 Syphilis
Syphilis is an infectious disease of chronic evolution, sexually (acquired syphilis ) or vertically (congenital syphilis) transmitted by the Treponema pallidum.4 Cases in pregnant women and congenital syphilis are a serious public health problem in the country, due to the high rates of prevalence, the vertical transmission and the high mortality. Acquired syphilis became a disease of compulsory notification in 2010. However, the notification of cases of congenital syphilis has been compulsory since 1986 and that of syphilis in pregnant women since 2005.
In terms of epidemiologic surveillance a case will be considered according to the criteria as:
(i) Congenital syphilis
First criteria - any child, abortion or stillborn from a mother with clinical evidence of syphilis and/or non-treponemal serology reactive to syphilis in any titre, in the absence of treponemal confirmatory test, performed during the antenatal period or during labor or curettage, that has not been treated or received inadequate treatment.
Second criteria - any individual under 13 years of age with the following serologic evidence: ascending titration (non treponemal tests); and/or non treponemal tests reactive after six months of age (except in situations of therapeutic follow-up); and/or reactive treponemal tests after 18 months of age; and/or non-treponemal tests higher that those of the mother.
Third criteria - any individual younger that 13 years with reactive non- treponemal test and clinical, liquoric or radiologic evidence of congenital syphilis.
Fourth criteria - any situation of evidence of infection by the T. pallidum on the placenta or umbilical cord and/or sample of the lesion, biopsy or necropsy of child, abortion of stillborn.
(ii) Syphilis in pregnant women
Pregnant woman that during the antenatal period presents with clinical evidence of syphilis and/or reactive non-treponemal serology, when the treponemal test is positive or was not performed.
(iii) Acquired syphilis: (suspicion):
Individual with clinic evidence of syphilis and/or reactive non-treponemal serology.
(iv) Acquired syphilis (confirmation): individual with reactive treponemal test.
2.7.1 Epidemiology
The World Health Organization estimated, in 1999, the annual global incidence of the four sexually transmitted diseases considered curable (syphilis, gonorrhea, Chlamydia and trichomoniasis) to be around 340 million cases. 4 12 million of those estimated cases occurred in Brazil, from which acquired syphilis would represent approximately 937 mil of the total number of cases.
A study of national representation performed with pregnant women in 2004 estimated a prevalence of 1,6% of syphilis infection, which would represent around 49 thousand pregnant women carrying the infection and an estimate of 12 thousand live-born with syphilis (vertical transmission rate of 25%). It is important to stress that the prevalence of syphilis in pregnant women is around four times higher than the prevalence of HIV infection.
Since the inclusion of syphilis in pregnant women on the compulsory notification list in 2005, until June 2009, 19.608 cases were detected in the country (Table 2). The case detection is still very low, considering the estimative of expected cases, which is also true for congenital syphilis. From 1998 to June 2009, a total of 55.124 cases were notified to SINAN, with an incidence rate, in 2007, of 1, 8 per 1.000 liveborn. In terms of mortality by congenital syphilis in the country, between 2004 and 2008 348 deaths were declared, representing around 28, 3% of the total of deaths registered since 1996. As far as sub notification is concerned, the data above indicate the high magnitude of the problem.
2.7.2 Challenges
In 1995 Brazil, together with other countries from Latin America and the Caribbean, assumed the compromise for the elaboration of the Action Plan, with the objective to eliminate congenital syphilis from the Americas. In 2007 The Operational Plan for the Reduction of the Vertical Transmission of HIV and Syphilis was officially launched, that ally estates and districts aiming at gradual and regionalized reduction of mother-child transmission rates of HIV and syphilis until 2011. The aim of this plan is to increase the coverage of HIV and syphilis testing on the antenatal period, increase the coverage of syphilis treatment to pregnant women and their partners, and amplify the prevention actions in order to, finally, reach the target of elimination considered by the Ministry of Health: the registration of up to one case of congenital syphilis per 1.000 live-born/year.
REFERENCES
- 1. Silva LJ. Vigilância epidemiológica: a perspectiva de quem é responsável. ComCiência. 2005;66.
- 2. Paim JS, Teixeira MGLC. Reorganização do sistema de vigilância epidemiológica na perspectiva do Sistema Único de Saúde (SUS). Scripta Nova. 1992;5:27-57.
- 3. Ministério da Saúde [Internet]. Secretaria de Vigilância em Saúde. Sistema de Informação de Agravos de Notificação - Sinan. [acesso 03 Nov 2010]. Available from: http://dtr2004.saude.gov.br/sinanweb/
- 4. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância Epidemiológica. Guia de vigilância epidemiológica. 7 ed. Brasília: Ministério da Saúde, 2009.
- 5. World Health Organization [Internet]. Global Program on AIDS. Global prevalence and incidence of selected curable sexually transmitted diseases: overview and esti mates. [cited 2009 Nov 03]. Available from: www.who.int/hiv/pub/sti/who_hiv_aids_2001.02.pdf
- 6. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Programa Nacional de DST e Aids. Prevalências e frequências relativas de Doenças Sexualmente Transmissíveis (DST) em populações selecionadas de seis capitais brasileiras, 2005. Brasília: Ministério da Saúde; 2008.
- 7. World Health Organization. Dengue: guidelines for diagnosis, treatment, prevention and control - New edition. Genebra: World Health Organization; 2009. p. 3-29.
-
8Pan American Health Organization. 2008:Number of reported cases of dengue and dengue hemorrhagic fever (DHF) - Region of the Americas (by country and subregion). Estados Unidos da América: Pan American HealthOrganization, 2009 [cited 2009 Dec. 10]. Available from: www.paho.org/English/AD/DPC/CD/dengue-cases-2008.htm
- 9. Siqueira JB, Martelli CMT, Coelho GE, Simplício ACR, Hatch DL. Dengue and Dengue Hemorrhagic Fever, Brazil, 1981-2002. Emerg Infect Dis. 2005;11:48-53.
- 10. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Análise de Situação de Saúde. Saúde Brasil 2009: uma análise da situação de saúde e da agenda nacional e internacional de prioridades em saúde. Brasília: Ministério da Saúde, 2010.
- 11. Teixeira MG, Costa MC, Coelho G, Barreto ML. Recent shift in age pattern of dengue hemorrhagic fever, Brazil. Emerg Infect Dis. 2008;14:1663.
- 12. Brasil. Ministério da Saúde. Cadernos de Atenção Básica. Hanseníase. In: Vigilância em Saúde. 2 ed rev. Brasília: Ministério da Saúde; 2008. n. 21. p.66-100.
- 13. Talhari S, Neves RG, Penna GO, Oliveira MLW. Hanseníase. 4 ed. Manaus: Gráfica Tropical; 2006.
- 14. Sociedade Brasileira de Dermatologia. Perfil nosológico das consultas dermatológicas no Brasil. An Bras Dermatol. 2006;81:549-58.
-
15World Health Organization [Internet]. Weekly Epidemiological Record.Genebra: World Health Organization, 2009c;84:333-40. [cited 2009 Ago 22]. Available from: http://www.who.int/wer
» link - 16. Penna MLF, Oliveira MLV, PennaGO. The Epidemiological Behaviour of Leprosy in Brazil. Lepr Rev. 2009;80:332-44.
-
17Brasil. Ministério da Saúde. Secretaria de vigilância em Saúde. Portaria conjunta nº 125 de 26 de março de 2009. Define ações de controle de hanseníase. Brasília: Ministério da Saúde, 2009b. [acesso 20 Jun 2011]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/svs/2009/poc0125_26_03_2009.html
- 18. Gontijo B, Carvalho MLR. Leishmaniose tegumentar americana. Rev Soc Bras Med Trop. 2003;36:71-80.
- 19. Lima EB, Motta JOC, Porto C, Sampaio RN. Tratamento da leishmaniose tegumentar americana. An Bras Dermatol. 2007;82:111-24.
- 20. Killick-Kendrick R. Phlebotomine vectors of the leishmaniases: a review. Med Vet Entomol. 1990;4:1-24.
- 21. Rangel EF, Laison R. Ecologia das leishmanioses. In: Flebotomíneos do Brasil. Rio de Janeiro: Fiocruz; 2003.
- 22. Guedes ACM, Carvalho MLR, Melo MN. Leishmaniose tegumentar: apresentação pouco comum. An Bras Dermatol. 2008;83:445-9.
- 23. Lessa MM, Lessa HA, Castro TWN, Oliveira A, Scherifer A, Machado P, et al. Leishmaniose mucosa: aspectos clínicos e epidemiológicos. Rev Bras Otorrinolaringol. 2007;73:843-7.
- 24. Carvalho ML, de Fontes CJR, Hueb MGF, Afonso AM, Melo LCC. Leishmaniose tegumentar no estado do Mato Grosso (Brasil): estudo clínico, laboratorial e terapêutico. An Bras Dermatol. 2002;77:45-56.
- 25. Passos VMA, Barreto SM, Romanha AJ, Krettli AU, Volpin AC, Gontijo SMF, et al. Leishmaniose tegumentar na região metropolitana de Belo Horizonte: aspectos clínicos, laboratoriais, terapêuticos e evolutivos (1989-1995). Rev Soc Bras Med Trop. 2001;34:5-12.
Publication Dates
-
Publication in this collection
01 Dec 2011 -
Date of issue
Oct 2011
History
-
Received
10 Aug 2010 -
Accepted
30 Nov 2010