Abstracts
Acne fulminans (AF) is a rare disorder, the most severe form of the entire clinical spectrum of acne. It is characterized by emergence of painful inflammatory nodules that turn into ulcers, concomitant with systemic manifestations. It can be induced by isotretinoin and some authors believe that the occurrence of this condition is dose dependent. The treatment is controversial and there is no consensus up to this time. A case of this rare disease, developed during use of isotretinoin in low doses, is presented.
Acne vulgaris; Retinoids; Therapeutics
A acne fulminans é afecção rara e a forma mais grave de todo o espectro clínico da acne. Caracterizase pelo aparecimento súbito de nódulos inflamatórios dolorosos que ulceram, concomitantemente, a manifestações sistêmicas. Pode ser induzida pela isotretinoína e alguns autores acreditam que a ocorrência do quadro seja dose dependente. O tratamento é controverso, não havendo padronização até o momento. Apresenta-se caso desta rara doença, desenvolvida durante o uso de isotretinoína em baixas doses.
Acne vulgar; Retinóides; Terapêutica
CASE REPORT
Acne fulminans and isotretinoin - case report*
Mayra Falcao PereiraI; Eduardo Mendes RoncadaI; Cláudia Macedo de OliveiraI; Rodrigo MonteiroI; Marilda Aparecida Milanez Morgado de AbreuII; Luciena Cegato OrtigosaIII
IGraduate student - resident physician of the Dermatology Service in Presidente Prudente (HRPP) - São Paulo (SP), Brazil
IIDoctoral program student - Coordinator of the Dermatology Service in Presidente Prudente (HRPP) - São Paulo (SP), Brazil
IIIDoctoral program student - Professor of the Dermatology Service in Presidente Prudente (HRPP) - São Paulo (SP), Brazil
Mailing address
ABSTRACT
Acne fulminans (AF) is a rare disorder, the most severe form of the entire clinical spectrum of acne. It is characterized by emergence of painful inflammatory nodules that turn into ulcers, concomitant with systemic manifestations. It can be induced by isotretinoin and some authors believe that the occurrence of this condition is dose dependent. The treatment is controversial and there is no consensus up to this time. A case of this rare disease, developed during use of isotretinoin in low doses, is presented.
Keywords: Acne vulgaris; Retinoids; Therapeutics
INTRODUCTION
First described in 1959 by Burns & Colville, acne fulminans (AF) is a rare affection and the most severe form of cystic acne.1-4 It mainly affects young male adults between 13 and 22 years of age, with history of acne vulgaris.3 It is estimated that it occurs in less than 1% of total acne cases.5 It is characterized by the onset of painful inflammatory nodules in the habitual areas of acne infection, which become ulcerated and covered by hemorrhagic crusts.3 Concomitantly, systemic manifestations such as fever, arthralgia, myalgia, asthenia, weight loss and, eventually, nodulous erythema, arthritis, myositis and bone alterations may be found. Laboratory exams may point out to the existence of anemia, leukocytosis with neutrophilia, increased hemosedimentation speed and microscopic hematuria.3,4 The treatment is controversial, there is no standardization up to the moment. Depending on the severity of the symptom complex, topical intralesional or oral glucocorticoids and oral isotretinoin may be utilized.3,6 Antibiotics do not alter the evolution of the disease and do not prevent the occurrence of new crises.3 Here a case of this rare disease, developed eight weeks after isotretinoin 0.3 mg/kg/day began to be used is presented, with 12 weeks of symptom evolution.
CASE REPORT
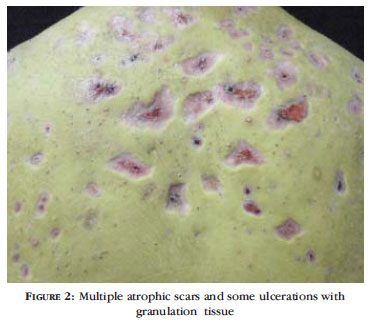
A 15-year-old male patient, weighing 73 kg (initial weight), student, born and domiciled in Presidente Prudente - SP, had presented acne vulgaris from the time he was 11 years of age, having undergone several topical and systemic treatments that showed little effectiveness. He had started treatment with 20 mg/day oral isotretinoin (Roacutam®), in another service, five months before. He mentioned that after the 2nd month of treatment inflamed and painful lesions appeared on the thorax and on the back. There were no family antecedents of severe acne nor of isotretinoin use by other family members. The dermatological exam at the beginning of the study revealed numerous erythematous nodules with 0.5 to 2 cm in diameter, painful on palpation, with pus and blood discharge and ulcerations covered by crusts on the back and thorax (Figure 1). There was also 10 kg weight loss in a five-month period, arthralgia, cervical and axillary lymph node enlargement. Laboratory exams performed during hospitalization revealed leukocytosis, increased hemosedimentation speed, important microscopic hematuria, proteinuria and S. aureus e S. pyogenes growth in the culture of secretion collected from the back. The treatment was done with oxacilin 2g/day, prednisone 30mg/day, and oral isotretinoin was maintained at the same dose of 20 mg/day. The patient evolved with decrease of cutaneous lesions, on which granulation tissue was formed and covered by hemorrhagic crusts, with no abscesses. There was also improvement in the systemic signs and general symptoms. Trichloroacetic acid at 50% was applied on the granulation tissue, with a satisfactory outcome (Figure 2). The patient demonstrated good psychological-emotional balance from the first appointment until this time, cooperating with the treatment. A scar correction procedure was scheduled to take place one year after the end of the isotretinoin treatment.
DISCUSSION
The etiopathogenesis of AF remains obscure, with probable inflammatory and immunologic mechanisms involved in the onset of the symptom complex.5,6 These mechanisms are detected by hypergammaglobulinemia, depletion of the complement system and presence of circulating immune complexes. Delayed cellular hypersensitivity reactions to Propionibacterium acnes are increased during the course of severe inflammatory acne and may also be involved in its pathogenesis. High testosterone levels during puberty may be an important cause of the disease and explains why it affects male adolescents almost exclusively, as in the reported case.6,7
AF can also be induced by isotretinoin.5 The doses and the intervals between the medication and the acute manifestations vary, but the lesions usually appear between the fourth and the eighth week counted from the beginning of the treatment, which is in accordance with the present case, where the onset occurred in the eighth week.6,8
AF, in association with the use of isotretinoin, should be differentiated from acne tetrad and pseudoacne fulminans. 1,3,6 Acne tetrad or follicular occlusion tetrad is composed of acne conglobata, hidradenitis suppurativa, pilonidal cysts and folliculitis abscedens. 9 In pseudo-acne fulminans there are skin ulcerations with hemorrhagic crusts in seborrheic areas, without systemic involvement. This is due to the drug ability to determine alterations in the desmosomes, in the collagen and in vascular proliferation. 3 Nevertheless, the latter is a rare adverse effect of the treatment with isotretinoin; there are few reports on the subject, which needs to be clarified.6
Some authors believe that the occurrence of this condition is dose dependent, while others disagree. 10,11,12 Although there is no consensus, it became evident from the existing reports of patients that developed AF during treatment with oral isotretinoin that they were using full and even high doses (more than 1mg/kg/day), while in the present case a subdose was being used by the patient, but he developed the disease anyway.8
The hemocultures of AF patients usually do not reveal bacterial growth, thus eliminating the possibility of septicemia.3 In skin cultures predominate the isolation of Staphylococcus epidermidis and Propionibacterium acnes, and, more rarely, of Pseudomonas, Staphylococcus aureus and Streptococcus pyogenes; the two last ones were the agents isolated in this patient. Nevertheless, it seems that there is little probability of a direct relationship between these agents and the cutaneous eruption. 5
The acne fulminans treatment is still a challenge, as an effective drug to control it and prevent crises is still unknown. The medications currently used are only effective with prolonged use, triggering several side effects.3 Oral antibiotics produce discreet response in the cutaneous condition and in the systemic symptoms.13 The available therapies are glucocorticoids, isotretinoin and levamisole. 1,3
Systemic glucocorticoids quickly improve skin lesions and systemic symptoms, although they tend to relapse when the dosage is decreased. Therefore, they should be maintained at a higher dose for a period that varies from two to four months, and be subsequently gradually reduced.6 It has been observed that the association with dapsone allows a better control of relapses.3 Another medication that has been intensively studied in AF management is isotretinoin, but it probably is not the treatment of choice and should be started after the use of corticoids. 5 It acts as a powerful anti inflammatory, in addition to its known sebostatic function and effect on the follicular keratinization pattern.6 However, the treatment with oral isotretinoin may induce multiple hyperproliferative lesions, with granulation tissue similar to pyogenic granuloma.5,8 In the presence of this type of lesion, a reduction in the isotretinoin dose, intralesional corticosteroid infiltrations, cauterization with trichloroacetic acid (ATA) or even laser are recommended.5 In this case, the combination of glucocorticoids and oral isotretinoin and topical application of ATA 50% was beneficial, with fast and noticeable improvement of the general and cutaneous symptom complex, without relapses for an eight-month period and without the onset of hypergranulation, which corroborates the findings of some authors that affirm that the most effective therapy is the association of corticoids and oral isotretinoin.5
Although the after-treatment prognosis is satisfactory, the cutaneous lesions usually leave scars and milia.6 As it is a disease of fast onset and evolution, the importance of early diagnosis and treatment should be emphasized, which can significantly decrease. 
REFERENCES
- 1. Hartmann RR, Plewig G. Acne fulminans: Tratamento de 11 pacientes com o ácido 13-cis-retinóico. An Bras Dermatol. 1983;58:3-10.
- 2. Jansen T, Grabbe S, Plewig G. Clinical variants of acne. Hautarzt. 2005;56:1018-26.
- 3. Neves CRS, Lacet IG, Santos JB, Cunha MMS, Silva VB. Acne fulminans: relato de um caso. An Bras Dermatol. 1990;66:15-7.
- 4. Sampaio SAP, Rivitti EA. Foliculoses. In: Sampaio SAP, Rivitti EA. Dermatologia. São Paulo: Artes Médicas; 2008. p. 383-92.
- 5. Romiti R, Jansen T, Plewig G. Acne fulminans. An Bras Dermatol. 2000;75:611-7.
- 6. Sousa AES, Lócio LMVM, Palma SLL, França ER, Azevedo CMC, Cavalcanti SMM. Acne fulminans: relato de dois casos clínicos. An Bras Dermatol. 2001;76:291-5.
- 7. Traupe H, Von Muhlendhal KE, Bramswig J, Happle R. Acne of the fulminans type following testosterone therapy in three excessively tall boys. Arch Dermatol. 1988;124:414-7.
- 8. Azulay DR, Abulafia LA, Costa JAN, Sodre CT. Tecido de granulação exuberante. Efeito colateral da terapêutica com isotretinoína. An Bras Dermatol. 1985;60:179-82.
- 9. Obadia DL, Daxbacher ELR, Jeunon T, Gripp AC. Hidroadenite supurativa tratada com infliximabe. An Bras Dermatol. 2009;84:695-7.
- 10. Spear KL, Muller SA. Nonhealing erosions with granulation tissue in the treatment of acne lesions during isotretinoin therapy. Arch Dermatol. 1984;120:1142.
- 11. Orfanos CE, Falco OB, Farber EM, Grupper CH, Polano MK. Retinoids. 1st ed. Berlin: Verlag Springer; 1981. p. 151.
- 12. Campbell JP, Grekin RC, Ellis CN, Matsuda-John SS, Swanson NA, Voorhees JJ. Retinoid therapy is associated with excess granulation tissue responses. J Am Acad Dermatol. 1983;9:708-13.
- 13. Seukeran DC, Cunliffe WJ. The treatment of acne fulminans: a review of 25 cases. Br J Dermatol. 1999;141:307-9.
Publication Dates
-
Publication in this collection
01 Dec 2011 -
Date of issue
Oct 2011
History
-
Received
19 June 2010 -
Accepted
05 Aug 2010