Abstracts
Elaioconiosis is a work-related acneiform dermatosis which affects the exposed skin of individuals working with oils or greases. Its incidence has decreased with the introduction of personal protective equipment, personal hygiene measures and the cleaning of work clothes. Although not a rare disease, elaioconiosis is seldom reported in the literature, particularly in Brazil. Sufferers need to take time off work to proceed with the prolonged treatment to resolve the lesions caused by this condition
Occupational dermatitis; Acneiform eruptions; Occupational medicine; Industrial oils; Lubricating Oils
Elaioconiose é uma dermatose ocupacional do tipo acneiforme que afeta as áreas expostas de trabalhadores que lidam com óleos ou graxas. Atualmente, com o uso dos equipamentos de proteção individual, medidas de higiene pessoal e lavagem dos uniformes de trabalho, sua incidência diminuiu. Apesar de não ser uma doença rara, é pouco relatada na literatura, principalmente na nacional. Seu tratamento é lento e para a resolução das lesões, requer o afastamento do trabalhador de suas atividades laborativas
Dermatite ocupacional; Erupções acneiformes; Medicina do trabalho; Óleos industriais; Óleos Lubrificantes
CASE REPORT
Elaioconiosis - case report*
Nanashara ValgasI; Cristina Paula SalaroII; Eduardo Bornhausen-DemarchIII; Clarice Jordão BonoraIV; Ariane Aimee Abrego BroceI
IMD, Postgraduate student in dermatology at the Prof. Rubem David Azulay Institute of Dermatology, Santa Casa da Misericordia do Rio de Janeiro (IDPRDA-SCMRJ), Post-Graduate Medical School, Catholic University of Rio de Janeiro (PUC-RIO), Brazil
IIFellow in Dermatology, Harvard University, USA
IIIMD, Postgraduate student in dermatology at the Prof. Rubem David Azulay Institute of Dermatology, Santa Casa da Misericordia do Rio de Janeiro (IDPRDA-SCMRJ), Post-Graduate Medical School, Catholic University of Rio de Janeiro (PUC-RIO), Brazil
IVMD, Postgraduate student in dermatology, Federal University of Rio de Janeiro (UFRJ), Brazil
VMD, Postgraduate student in dermatology at the Prof. Rubem David Azulay Institute of Dermatology, Santa Casa da Misericordia do Rio de Janeiro (IDPRDA-SCMRJ), Brazil
Mailing address
ABSTRACT
Elaioconiosis is a work-related acneiform dermatosis which affects the exposed skin of individuals working with oils or greases. Its incidence has decreased with the introduction of personal protective equipment, personal hygiene measures and the cleaning of work clothes. Although not a rare disease, elaioconiosis is seldom reported in the literature, particularly in Brazil. Sufferers need to take time off work to proceed with the prolonged treatment to resolve the lesions caused by this condition.
Keywords: Occupational dermatitis; Acneiform eruptions; Occupational medicine; Industrial oils, Lubricating Oils
INTRODUCTION
Elaioconiosis is an acneiform eruption which affects metal-industry workers and vehicle mechanics exposed to cutting oils. 1 Also known as follicular dermatitis or oil acne, this disorder is caused by exposure to heavy oils extracted from petroleum. Its incidence has however been reduced due to exposed workers adopting better hygiene, cleaning their clothes after work and using personal protective equipment. Treatment is difficult and prolonged, requiring sufferers to spend long periods away from work until remission of the lesions. Diagnosis of elaioconiosis is based on morphology, location of the lesions and the patient's history of exposure to oils and greases at work.
CASE REPORT
51-year-old mechanic, black, married, born in Rio de Janeiro, living in São Gonçalo, presented himself at the general dermatology clinic complaining of itchy black spots on the upper limbs which began to appear about four months previously (Figure 1). He said that he had been a mechanic for over ten years, had never used gloves or any other protective equipment and claimed that he had not suffered before from the condition.
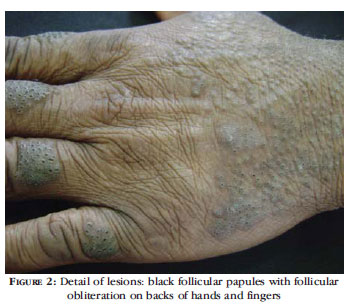
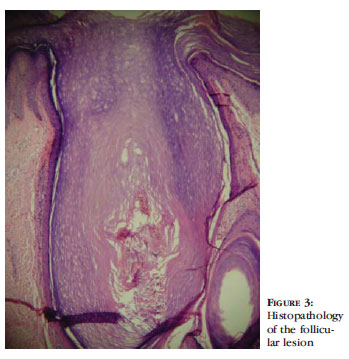
Dermatological examination revealed follicular papules with blackened central points located on the back of the patient's hands, fingers, arms and forearms, sparing the palmar region (Figure 2). We performed punch biopsy of a lesion on the dorsum of the third finger of the left hand. Histopathological examination detected infundibular hyperkeratosis, atrophy and obstruction of the ostium of the follicle wall, with mild inflammatory infiltrate. The adjacent epidermis was observed with acanthosis, hyperkeratosis hypergranulosis, without inflammatory infiltrate (Figure 3).
15% urea cream was initially prescribed to be applied twice daily, with 0.05% retinoic acid to be used at night. The patient was also instructed to use a loofer (natural vegetable sponge) when showering. No improvement was observed after one month. Although advised of the importance of staying away from work, the patient failed to do so and only slight clinical improvement was noted after three months of treatment. The prescription was then changed to 20% urea lotion combined with 3% salicylic acid twice daily, betamethasone cream twice daily for seven days (due to patient's complaining of severe itching) and bathing the affected parts in warm water with the use of a loofer. At this stage the patient succeeded in getting approval for leave of absence from work through the National Social Security Institute (INSS), and was therefore able to avoid contact with oils and greases.
Shortly after beginning this therapy at home the patient began to show clinical improvement. We observed via dermoscopy clear follicular ostia with no blackened central points (Figure 4).
DISCUSSION
The first reference to this occupational dermatosis was made by Purdon in 1867, who observed its occurrence among workers responsible for cleaning and lubricating the loom-coils used in the textile industry. In 1889 Leloir reported cases among female cotton spinners. 2 Paul Blum subsequently posited the term "follicular elaioconiosis" to describe this disorder. 3 Osvaldo Costa published in 1943 his report of a case of elaioconiosis, one of the first cases to appear in the Brazilian literature. Our research in Medline using the terms "elaioconiosis", "elaiokoniosis", "oil acne" and "occupational acne," revealed few studies on the subject and no specific study published over the last ten years.
Although elaioconiosis represents a significant proportion of occupational skin disorders, it is rarely seen in dermatology clinics. Its prevalence is unclear, since most cases are not statistically recorded and generally fail to attract the attention of dermatologists. Many cases are self-medicated, while other patients are treated by medical staff at work. The disorder mainly affects mechanics and can occur at any stage of life. Elaioconiosis was known as a common occupational skin disease 30 years ago. However its occurrence has declined significantly over recent years due to the advent of automated technology in industry, the better quality of soluble oils, the adoption by workers of proper hygiene, the use of personal protective equipment, cleaner workplaces and the wearing of industrial clothing.
The pathogenesis of elaioconiosis is not yet established. Some authors believe that it is linked to the obliteration of the follicular ostia by grease and metal particles contained therein, with secondary production of acne, comedones and subsequent infection of the follicle. Others are of the opinion that the oil itself has little influence in its genesis and that follicular lesions are caused by the acidity of the oils and the ability of hydrocarbons contained in the oils to cause follicular damage. 4 In the case described above, histopathology showed no inflammatory infiltrate in the hair follicle, suggesting that its initial cause is directly related to mechanical obstruction of the follicle ostium.
Peixoto Perilo Galvao (1948) divided elaioconiosis into three phases, 2 with which we concur:
1) The obliterans phase, involving obstruction of the follicular ostium by oil or the particles contained therein, which may lead to mild perifollicular inflammation accompanied by the appearance of short hairs, black spots and small crusty pimples.
2) The papular peripilar phase, exhibiting flat or tapered comedones and papules and follicular hyperkeratosis.
3) The infectious phase: formation of follicular papular pustules.
The clinical presentation shows comedoniform black spots in the follicular ostia and papules and pustules which can cause pain and itching. These may develop scarring and appear only infrequently as suppurative or furunculoid lesions. Clovis Bopp and Ralph Müller's 1979 study found that the forearms were the most affected areas, 3 although the hands and arms are also often affected. Our patient's lesions were consistent, clinically and pathologically, with the first and second stages (see above).
It is essential that patients take time off work to proceed with the prolonged treatment of elaioconiosis aimed at improving the clinical manifestations of this disorder. Keratolytics, and using a loofer in the shower, can help to unblock the affected follicles. Treatment with systemic antibiotics, such as tetracycline, and topical and systemic retinoids has been reported, with moderate success. 5,6 Preventive measures are also recommended such the application of silicone creams, frequent hand/clothes washing and using personal protective equipment. 7
Elaioconiosis is an occupational dermatosis that needs to be identified and treated as such by a dermatologist. Early diagnosis is crucial, since appropriate treatment together with personal hygiene and other prevention measures (including time away from work) are essential for controlling the symptoms.
REFERENCES
-
1Ministério da Saúde. [Internet]. Secretaria de Atenção à Saúde. Departamento de Ações programáticas Estratégicas. Dermatoses ocupacionais. Brasília: Ministério da Saúde; 2006. 92 p. [Acesso 28 abr. 2011]. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/protocolo_dermatoses.pdf
-
2Peixoto PG. Elaioconiose folicular. An Bras Dermatol. 1948;23:1-15.
-
3Bopp C, Muller R. Elaioconiose folicular. An Bras Dermatol. 1979;54:123-36.
-
4Costa OG. Elaioconiose folicular (Paul Blum). An Bras Dermatol. 1943;18:167-9.
-
5Czernielewski A, Skwarczyƒska-BanyÊ E. Oral treatment of acne vulgaris and oil acne with tetracycline. Dermatologica.1982;165:62-5.
-
6Finkelstein E, Lazarov A, Cagnano M, Halevy S. Oil acne: sucessful treatment with isotretnoin. J Am Acad Dermatol. 1994;30:491-2.
-
7Svendsen K, Hilt B. Skin disorders in ship's engineers exposed to oils and solvents. Contact Dermatitis. 1997;36:216-20.
Publication Dates
-
Publication in this collection
08 Nov 2011 -
Date of issue
Aug 2011
History
-
Accepted
17 Feb 2011 -
Received
11 Dec 2010