Abstracts
Pancreatic panniculitis is a rare pathological condition affecting 2-3% of patients with pancreatic disease. In 40% of cases the condition precedes manifestations of pancreatic disease. We report the case of a 71-year-old female who presented with an erythematous tender node which had appeared one month previously, progressing to ulceration and yellowish exudation. No abdominal symptoms. Biopsy revealed fat necrosis and vacuolated macrophages represented by amorphous amphophilic areas. Laboratory examination and CT scan revealed chronic pancreatitis. It is assumed that release of pancreatic enzymes such as trypsin may enhance the permeability of the microcirculation leading to lipase and amylase causing the subcutaneous fat necrosis observed in the lesions. Histology showed "ghost cells" and, firstly, septal panniculitis, followed later by lobular panniculitis. Treatment focused on resolution of the underlying pancreatic disease
Pancreas; Panniculitis; Adipose tissue
A paniculite pancreática, condição patológica rara, acomete 2-3% dos pacientes com doença do pâncreas. Em 40% dos casos, precede manifestações de doença pancreática. Relata-se caso de paciente feminina, 71 anos, surgimento há 1 mês de nódulos eritematosos nas pernas que evoluíram para ulceração e saída de conteúdo amarelado. Sem sintomas abdominais. A biópsia revelou macrófagos vacuolizados e necrose gordurosa representada por áreas anfofílicas, de material amorfo. Exame laboratorial e TAC demonstraram pancreatite crônica. Presume-se que a liberação de enzimas pancreáticas, tais como a tripsina, pode aumentar a permeabilidade da microcirculação e, então, a lípase e a amilase causariam a necrose de gordura subcutânea observada nas lesões. Na histologia, observam-se "células fantasmas" e paniculite septal de início e posteriormente lobular. O tratamento direciona-se a resolução da doença base
Pâncreas; Paniculite; Tecido adiposo
CASE REPORT
Pancreatic panniculitis as the first manifestation of visceral disease - case report*
Fernanda Homem de Mello de SouzaI; Elisa Beatriz Dalledone SiqueiraII; Lismary MesquitaIII; Lincoln Zambaldi FabricioIV; Felipe Francisco TuonV
IResident of the third year of dermatology at the Dermatology Service of the Universidade de Brasília (UnB) - Brasília (DF), Brazil
IIDoctor in dermatology by the Universidade de Brasília - Assistant physician of the Dermatology service of the Universidade de Brasília (UnB) - Brasília (DF), Brazil
IIIMaster in dermatology by the Universidade de Brasília - Assistant physician of the Dermatology service of the Universidade de Brasília (UnB) - Brasília (DF), Brazil
IVMédico dermatologista - Médico chefe do Departamento de Dermatologia do Hospital Universitário Evangélico de Curitiba da Faculdade Evangélica do Paraná (FEPAR) - Curitiba (PR), Brasil
VMédico Infectologista - Médico do departamento de infectologia do Hospital Universitário Evangélico de Curitiba da Faculdade Evangélica do Paraná (FEPAR) - Curitiba (PR), Brasil
Mailing address
ABSTRACT
Pancreatic panniculitis is a rare pathological condition affecting 2-3% of patients with pancreatic disease. In 40% of cases the condition precedes manifestations of pancreatic disease. We report the case of a 71-year-old female who presented with an erythematous tender node which had appeared one month previously, progressing to ulceration and yellowish exudation. No abdominal symptoms. Biopsy revealed fat necrosis and vacuolated macrophages represented by amorphous amphophilic areas. Laboratory examination and CT scan revealed chronic pancreatitis. It is assumed that release of pancreatic enzymes such as trypsin may enhance the permeability of the microcirculation leading to lipase and amylase causing the subcutaneous fat necrosis observed in the lesions. Histology showed "ghost cells" and, firstly, septal panniculitis, followed later by lobular panniculitis. Treatment focused on resolution of the underlying pancreatic disease.
Keywords: Pancreas; Panniculitis; Adipose tissue
INTRODUCTION
Panniculitis is a group of diseases whose hall-Panniculitis are normally durable and in some cases mark is inflammation of the subcutaneous adipose tis-can last for months - a diagnostic challenge for dermasue. May arise due to inflammatory and/or infectious tologists and pathologists. From a clinical viewpoint, mechanisms. 1,2 The clinical picture of panniculitis is many types of panniculitis of different etiologies manifested by deep erythematous plaques or nodules, resemble one another, presenting as erythematous with or without ulceration, on different locations of subcutaneous nodules. Some panniculitis may be a the body, but predominantly affecting the legs. manifestation of a number of different diseases (a classic example is erythema nodosum), and even in cases where the type of panniculitis is correctly identified identification is merely the first step in a series of clinical and laboratory investigations to determine the cause. 3 From an anatopathologic point of view, the subcutaneous fat responds to a variety of insults in a limited number of ways, and histopathological differences between the various forms of panniculitis can therefore be subtle. 4 Clinicopathological correlation is of key importance for distinguishing between the different entities of this spectrum of diseases. A deep incisional biopsy of the lesions needs to be performed to assist diagnosis. 2.5
Several types of panniculitis exist. Our clinical case of pancreatic panniculitis is classified as a predominantly lobular panniculitis without vasculitis, with a predominance of neutrophils in the inflammatory infiltrate, and may be associated with extensive areas of necrosis and saponification of adipocytes. 5
Pancreatic panniculitis is linked to disease of the pancreas. A rare condition, affecting 2-3% of patients with diseases of the pancreas, it tends to predominate in males because of higher rates of alcoholism. It is suspected that it is caused by the release of trypsin, lipase, amylase and phospholipase in the peripheral circulation. 1,2,6
The case report below refers to chronic pancreatitis which, contrary to the normal pattern of progression, at first presented clinically as pancreatic panniculitis.
CASE REPORT
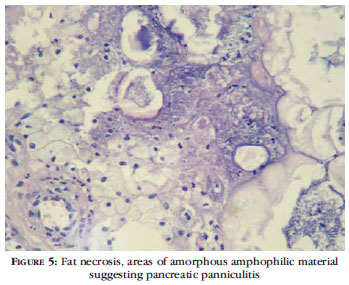
71-year-old female patient complained of emergence, one month previously, of erythematous nodules on the legs which progressed to ulceration and yellowish exudation. Erythema around the nodules and associated pain but good general condition, without associated complaints. Taking Metoprolol for hypertension. Examination revealed erythematous nodules on the legs, predominantly on the anterior, interspersed with ulcerated lesions with ulceration and yellow exudation (figures1, 2 and 3 ). Deep biopsy revealed acute and chronic inflammation with fat necrosis and vacuolated macrophages represented by areas of amorphous amphophilic material, suggesting pancreatic panniculitis (figures 4 and 5). Requested pancreatic enzymes - amylase: 1073 units/liter (Reference value: 22-80U/L-cloronitrofenol method) and lipase: 1871 units/liter (RV: up to 200 U/L - with the ultraviolet kinetic turbidimetric method). Abdominal CT scan showed increased diameter of the pancreas with pseudocyst image, compatible with chronic pancreatitis. The patient remains under surveillance for investigation of the etiology of the pancreatic disease.
DISCUSSION
Acute or chronic pancreatitis and pancreatic carcinoma (usually of acinar cells) are the most common pancreatic diseases associated with pancreatic panniculitis. However, pancreatic pseudocyst, post-traumatic pancreatitis, pancreas divisum and pancreatic vascular fistulas have also been reported. 1,2,6,7 The pathogenesis is unknown, but it is assumed that the release of pancreatic enzymes such as trypsin may increase microcirculation permeability, resulting in lipase and amylase causing the subcutaneous fat necrosis observed in the lesions. 6 Cases of pancreatic panniculitis with normal enzyme levels have been reported. 2,5,6 These reports and the discrepancy between the relative frequency of the disease and the frequency of pancreatic panniculitis suggest the involvement of an additional etiological factor. One hypothesis is that these patients are unable to degrade pancreatic enzymes, probably due to inherited enzyme deficiencies such as alpha 1-antitrypsin (AAT). 1.6
The clinical picture of pancreatic panniculitis consists of soft or violet erythematous plaques and nodules predominantly on the legs (around the ankles and pretibial region), buttocks or trunk, which may resolve spontaneously. The nodules may evolve to fluctuation and produce necrotic sterile abscesses that ulcerate spontaneously, exuding thick oily brownish material due to liquefactive fat necrosis. 1.6 More generalized cases also present with arthritis due to periarticular fat necrosis and pleural effusions, and reports exist of ascites and eosinophilia. 1,5,8
In 40% of cases of pancreatic panniculitis, skin lesions precede the abdominal symptoms of pancreatic disease. In these cases the average interval between the cutaneous findings and the discovery of abdominal disease is 13 weeks.1,2,6,9 A deep skin biopsy is required for diagnosis. 6
Histologically, pancreatic panniculitis is a predominantly lobular panniculitis. Initial lesions are characterized by lymphoplasmacytic infiltration along the fibrous septum around subcutaneous fat lobules and dermal blood vessels. 1,2,7 Coagulative pancreatic fat necrosis is characterized by collections of "ghost cells" which are anucleate adipocytes containing fine basophilic granular intracytoplasmic material arising from saponification of fat by pancreatic enzymes. 1,2,5 These histological characteristics evolve and old lesions show more granulomatous panniculitis containing foamy histiocytes and multinucleated giant cells. 1.7 Vasculitis is not present. 6
Treatment is supportive and targeted at pancreatic disease. The prognosis is poor in cases associated with pancreatic carcinoma. 1.6
REFERENCES
-
1Farrant P, Abu-Nab Z, Hextall J. Tender erythematous nodules on the lower limb. Clin Exp Dermatol. 2009;34:549-51.
-
2Johnson MA, Kannan DG, Balachandar TG, Jeswanth S, Rajendran S, Surendran R. Acute septal panniculitis. A cutaneous marker of a very early stage of pancreatic panniculitis indicating acute pancreatitis. JOP. 2005;06h33min-8.
-
3Balassiano E, Costa MA. Paniculites (hipodermites). An Bras Dermatol. 1981;56:55-60.
-
4Patterson JW. Differential diagnosis of panniculitis. Adv Dermatol. 1991;6:309-29.
-
5Requena L, Yus ES Panniculitis. Part II. Mostly lobular panniculitis. J Am Acad Dermatol. 2001;45:325-61.
-
6Lee WS, Kim MY, Kim SW, Paik CN, Kim HO, Park YM. Fatal pancreatic panniculitis associated with acute pancreatitis: a case report. J Korean Med Sci. 2007;22:914-7.
-
7Shehan JM, Kalaaji AN. Pancreatic panniculitis due to pancreatic carcinoma. Mayo Clin Proc. 2005;80:822.
-
8Rde W, Hagler KT, Carag HR, Flowers FP. Pancreatic panniculitis. Eur J Surg Oncol. 2005;31:1213-5.
-
9Dahl PR, Su WP, Cullimore KC, Dicken CH. Pancreatic panniculitis. J Am Acad Dermatol. 1995;33:413-7.
Publication Dates
-
Publication in this collection
08 Nov 2011 -
Date of issue
Aug 2011
History
-
Received
15 Feb 2011 -
Accepted
26 Apr 2011