Abstracts
Cutaneous endometriosis is a rare manifestation of endometriosis, representing 0.5% to 1% of all endometriosis cases. It can be divided into primary and secondary, when appearing spontaneously or after a surgical procedure, when it is mostly found on surgical scar tissue. Some etiologies were proposed, but none of them could entirely explain the appearance of the tumor. Differential diagnosis includes melanoma, metastatic nodule, keloid and pyogenic granuloma. Dermoscopic features are not yet well established, but there are some characteristics that suggest the diagnosis. Treatment is surgical in larger sized lesions. Malignization can occur. The screening for endometriosis is mandatory by means of gynecologic, imaging and marked-tumor evaluation. We report a case of primary umbilical endometriosis and discuss its dermoscopic aspects.
Dermoscopy; Endometriosis; Keloid; Melanoma
A endometriose cutânea é forma rara de endometriose, representando de 0,5% a 1% de todos os casos da doença. Pode ser dividida em forma primária, de surgimento espontâneo, ou secundária, após procedimentos cirúrgicos aonde geralmente encontra-se sobre a cicatriz cirúrgica. Diversas etiologias foram propostas, porém, nenhuma capaz de explicar inteiramente seu aparecimento. Diagnósticos diferenciais incluem melanoma, nódulos metastáticos, quelóide e granuloma piogênico. A dermatoscopia da lesão ainda não foi bem estabelecida, mas existem alguns achados que podem sugerir o diagnóstico. O tratamento é cirúrgico nos casos de lesões maiores e o screening para endometriose é mandatório através de avaliação ginecológica, de imagem e marcador tumoral. Relatamos um caso de endometriose cutânea primária e discutimos seus aspectos dermatoscópicos.
Dermoscopia; Endometriose; Melanoma; Quelóide
INTRODUCTION
The term endometriosis refers to the presence of endometrial tissue outside the uterine cavity.11. Pereira Júnior AC, Silva ACL, Marques AC. Endometriose Cutânea. An Bras Dermatol. 1970;45:371-6.
2. Castro MCR, Costa APF, Salles R, Maya TC, Ramos e Silva M. Endometriose umbilical. An Bras Dermatol. 1997;72:255-8.
3. Giorgi VD, Massi D, Mannone F, Stante M, Carli P. Cutaneous endometriosis: noninvasive analysis by epiluminescence microscopy. Clin Exp Dermatol. 2003;28:315-7.
4. Valencio MCS, Rossoe EWT, Pegas JRP, Tebcherani A, Santos CP, Santos MR, et al. Endometriose cutânea primária- relato de caso. Diagn Tratamento. 2006;11:144-6.
5. Carvalho BR, Rosa e Silva JC, Rosa e Silva ACJS, Barbosa HF, Poli Neto OB, Reis FJC, et al. Endometriose umbilical sem cirurgia pélvica prévia. Rev Bras Ginecol Obstet. 2008;30:167-70.
6. Agarwal A, Fong Y F. Spontaneous endometriosis. Singapore Med J. 2008;49:704-9.
7. Chatzikokkinou P, Thorfinn J, Angelidis K, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:126-30.
8. Attia L, Ben Temime R, Sidhom J, Sahli A, Makhlouf T, Chachia A, et al. A case of cutaneous endometriosis development on an abdominal scar. Tunis Med. 2010;88:841-3.
9. Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9-1010. Nácul AP, Spritzer PM. Aspectos atuais do diagnóstico e tratamento da endometriose. Rev Bras Ginecol Obstet. 2010;32:298-307. It is considered a common disease prevalent in approximately 12% of women of reproductive age. Its etiopathogeny, however, is not yet well established. The most accepted theory is that of "implantation", described in 1927 by Sampson, which is based on the retrograde menstrual flow where endometrial tissue implants would travel during menstruation and settle in other places such as the ovary and peritoneum. However, it is known that up to 90% of women have this type of bleeding and only a minority will develop the disease.88. Attia L, Ben Temime R, Sidhom J, Sahli A, Makhlouf T, Chachia A, et al. A case of cutaneous endometriosis development on an abdominal scar. Tunis Med. 2010;88:841-3.Another form derived from this same theory, would be the iatrogenic implantation during surgical procedures such as a cesarean section, where the growth of this tissue would normally be found on the surgical scar.
Umbilical endometriosis is rare, representing 0.5% to 1% of all endometriosis cases. Antonio Carlos Pereira Junior et al was the first Brazilian to describe the disease, in these annals, in 1970. This kind of endometriosis can be classified as primary, when it comes "de novo" or secondary, when it comes after surgical procedures. The umbilicus, considered a physiologic scar, could have tropism for endometrial cells, as seen in other scar tissues.88. Attia L, Ben Temime R, Sidhom J, Sahli A, Makhlouf T, Chachia A, et al. A case of cutaneous endometriosis development on an abdominal scar. Tunis Med. 2010;88:841-3.
The designation secondary endometriosis can be used even when it is not located on surgical scars, such as on the umbilicus, but only if its onset occurs within 2 years after the procedure.88. Attia L, Ben Temime R, Sidhom J, Sahli A, Makhlouf T, Chachia A, et al. A case of cutaneous endometriosis development on an abdominal scar. Tunis Med. 2010;88:841-3. , 99. Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9 Clinically it presents as a reddish-brown nodule, commonly painful, with cyclic variations in size, with or without bleeding, that may coincide or not with the patient's menstrual cycle.44. Valencio MCS, Rossoe EWT, Pegas JRP, Tebcherani A, Santos CP, Santos MR, et al. Endometriose cutânea primária- relato de caso. Diagn Tratamento. 2006;11:144-6.
As for the differential diagnosis, mainly melanoma, umbilical metastasis (Mary Sister Joseph nodule), keloid and pyogenic granuloma should be considered.11. Pereira Júnior AC, Silva ACL, Marques AC. Endometriose Cutânea. An Bras Dermatol. 1970;45:371-6.
2. Castro MCR, Costa APF, Salles R, Maya TC, Ramos e Silva M. Endometriose umbilical. An Bras Dermatol. 1997;72:255-8.
3. Giorgi VD, Massi D, Mannone F, Stante M, Carli P. Cutaneous endometriosis: noninvasive analysis by epiluminescence microscopy. Clin Exp Dermatol. 2003;28:315-7.
4. Valencio MCS, Rossoe EWT, Pegas JRP, Tebcherani A, Santos CP, Santos MR, et al. Endometriose cutânea primária- relato de caso. Diagn Tratamento. 2006;11:144-6.
5. Carvalho BR, Rosa e Silva JC, Rosa e Silva ACJS, Barbosa HF, Poli Neto OB, Reis FJC, et al. Endometriose umbilical sem cirurgia pélvica prévia. Rev Bras Ginecol Obstet. 2008;30:167-70.
6. Agarwal A, Fong Y F. Spontaneous endometriosis. Singapore Med J. 2008;49:704-9.
7. Chatzikokkinou P, Thorfinn J, Angelidis K, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:126-30.
8. Attia L, Ben Temime R, Sidhom J, Sahli A, Makhlouf T, Chachia A, et al. A case of cutaneous endometriosis development on an abdominal scar. Tunis Med. 2010;88:841-3.
9. Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9-1010. Nácul AP, Spritzer PM. Aspectos atuais do diagnóstico e tratamento da endometriose. Rev Bras Ginecol Obstet. 2010;32:298-307.
The histopathology is also changeable depending on the endometrial phase biopsied. The general feature is the absence of or discrete epidermal findings; in the dermis, fibroblast proliferation, seen as spindle cells.11. Pereira Júnior AC, Silva ACL, Marques AC. Endometriose Cutânea. An Bras Dermatol. 1970;45:371-6.
2. Castro MCR, Costa APF, Salles R, Maya TC, Ramos e Silva M. Endometriose umbilical. An Bras Dermatol. 1997;72:255-8.
3. Giorgi VD, Massi D, Mannone F, Stante M, Carli P. Cutaneous endometriosis: noninvasive analysis by epiluminescence microscopy. Clin Exp Dermatol. 2003;28:315-7.
4. Valencio MCS, Rossoe EWT, Pegas JRP, Tebcherani A, Santos CP, Santos MR, et al. Endometriose cutânea primária- relato de caso. Diagn Tratamento. 2006;11:144-6.
5. Carvalho BR, Rosa e Silva JC, Rosa e Silva ACJS, Barbosa HF, Poli Neto OB, Reis FJC, et al. Endometriose umbilical sem cirurgia pélvica prévia. Rev Bras Ginecol Obstet. 2008;30:167-70.
6. Agarwal A, Fong Y F. Spontaneous endometriosis. Singapore Med J. 2008;49:704-9.-77. Chatzikokkinou P, Thorfinn J, Angelidis K, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:126-30., 99. Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9 The endometrial tissue, better seen when stained by anti CD10, is present in the dermis and can demonstrate the proliferative phase, when it will be possible to identify endometrial glands with intense mitotic activity or the secretory phase, in which glands with decapitation secretion will be present.99. Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9Findings of hemosiderin in the dermis may be present, representing prior bleeding, better evidenced when stained by Pearls.55. Carvalho BR, Rosa e Silva JC, Rosa e Silva ACJS, Barbosa HF, Poli Neto OB, Reis FJC, et al. Endometriose umbilical sem cirurgia pélvica prévia. Rev Bras Ginecol Obstet. 2008;30:167-70.
A screening for pelvic endometriosis is mandatory. An elevated Ca-125 (cancer antigen 125) dosage can alert to this concomitance. This antigen is best known as a blood marker for ovarian cancer but it may also be elevated in other cancers and benign conditions, such as endometriosis. Images, initially with USG and later with NMR (nuclear magnetic resonance) can detect that presence more accurately. However, video laparoscopy is still the "golden key" to diagnose pelvic endometriosis.1010. Nácul AP, Spritzer PM. Aspectos atuais do diagnóstico e tratamento da endometriose. Rev Bras Ginecol Obstet. 2010;32:298-307.
Dermoscopy is found to assist in the diagnosis of this rare entity. In the literature, there was only one case reported by Di Giorgi et al in 2003, where the author proposes dermoscopic findings in the diagnosis of a presented case. It describes homogeneous red coloration, regularly distributed, fading to the periphery. Within this usual pigmentation some small red globular structures are described, that he refers to as "red atolls". After a dermoscopic-histopathologic correlation the authors show that these "red atolls" would correspond to irregular glands containing erythrocytes embedded in a cellular stroma and the red homogeneous aspect would correspond to vascular stroma with myxoid appearance containing extravasated erythrocytes.33. Giorgi VD, Massi D, Mannone F, Stante M, Carli P. Cutaneous endometriosis: noninvasive analysis by epiluminescence microscopy. Clin Exp Dermatol. 2003;28:315-7., 77. Chatzikokkinou P, Thorfinn J, Angelidis K, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:126-30.
The first line treatment is surgical, due to high incidence of recurrence and also the possibility of malignant transformation. Pretreatment with hormones is also an option especially in larger tumors, providing a reduction in size before surgery.99. Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9,1010. Nácul AP, Spritzer PM. Aspectos atuais do diagnóstico e tratamento da endometriose. Rev Bras Ginecol Obstet. 2010;32:298-307.
CASE REPORT
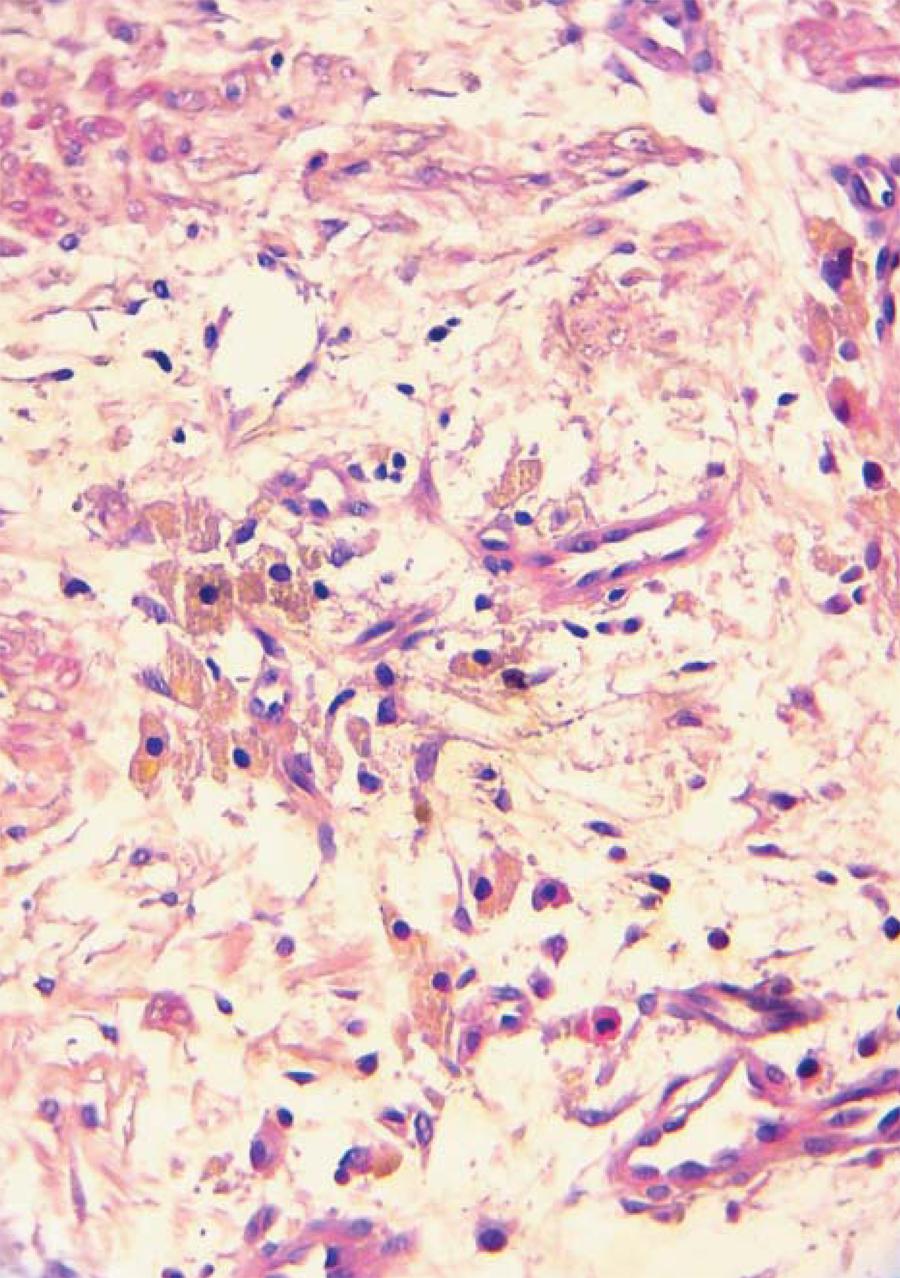
Female, 32 years old, came to our service complaining about a 3-month growth in the umbilical area. The lesion was a shiny reddish-brown nodule, measuring 3cmx3cm, painful to the touch and that alternated in size since its onset (Figure 1). The patient referred one episode of spontaneous bleeding that did not follow her menstrual cycle. She had had a cesarean delivery 6 years ago and no gynecologic complaints. After clinical examination, dermoscopic observation was performed, using a polarized light dermatoscope (DermLite II Pro HR). It showed homogeneous reddish localized pigmentation, with no differentiated structures. In addition, an amorphous brown area was present, where normal skin network was more evident in some parts (Figure 2). The biopsy revealed fibroblastic proliferation in the dermis and endometrial glandular tissue, of the decapitation secretion type (Figures 3 and 4). It also revealed deposit of hemosiderin in the dermis as an evidence of previous bleeding (Figure 5). The diagnosis of primary umbilical endometriosis was established. All the imaging exams as well as the Ca-125 dosage were normal.
Umbilical endometriosis. Clinical aspect. A shiny reddish-brown tumor, with well defined limits, located on the umbilicus scar. The patient referred one episode of spontaneous bleeding
Umbilical endometriosis. Dermoscopic aspect by epiluminescence microscopy. 10x magnification. Number 1: a regular pigmented network is noticed in its central area. Number 2: an amorphous brown area with white scar tissue in the center, caused by a biopsy procedure. Number 3: a homogeneous reddish pigmentation is regularly distributed
Umbilical endometriosis. Histopathological aspect. Stained by Hematoxylin and Eosin (HE). On left lower portion, epidermis with discrete acanthosis. In the dermis, a myxoid stroma aspect with fibroblastic proliferation, evidenced by the spinde-shaped cells. On the upper right portion, glandular type cells, characteristic of endometriosis
Umbilical endometriosis. Histopathological aspect, stained by Hematoxylin and Eosin (HE). The upper right portion of the first histopathological picture shows a higher approach to the decapitation secretion of the glandular cells. These features belong to the secretory phase of the glandular epithelium
Umbilical Endometriosis. Histopathological aspect. Stained by Hematoxylin and Eosin (HE). In the dermis, hemosiderin deposit located mostly around vessels is evidence of previous bleeding
DISCUSSION
Cutaneous umbilical endometriosis is a rare entity, representing 0.5% to 1% of all endometriosis cases. As described before, its primary form can arise spontaneously with or without associated symptoms, such as in the presented case where the absence of symptoms made the diagnosis more difficult. The presence of spontaneous bleeding, as well as the color of the lesion should alert the clinician to the possibility of melanoma diagnosis.
A biopsy is mandatory in all cases, especially when melanoma cannot be ruled out. Therefore, we suggest dermoscopy as an auxiliary tool in the physical examination of these patients.
Our dermoscopic findings were only in part similar to the previous reported cases. The presence of the reddish homogeneous pigmentation was observed only in one part of the lesion and there was no evidence of the "red atolls" described before. We considered that such differences could come from the different phases when the evaluation was performed. Our hypothesis, however, can only be proven with other evaluations in different phases of endometriosis. Therefore, this case report has as the objective of providing contributions to describe and clearly establish the dermoscopic features of cutaneous endometriosis.
REFERENCES
-
1Pereira Júnior AC, Silva ACL, Marques AC. Endometriose Cutânea. An Bras Dermatol. 1970;45:371-6.
-
2Castro MCR, Costa APF, Salles R, Maya TC, Ramos e Silva M. Endometriose umbilical. An Bras Dermatol. 1997;72:255-8.
-
3Giorgi VD, Massi D, Mannone F, Stante M, Carli P. Cutaneous endometriosis: noninvasive analysis by epiluminescence microscopy. Clin Exp Dermatol. 2003;28:315-7.
-
4Valencio MCS, Rossoe EWT, Pegas JRP, Tebcherani A, Santos CP, Santos MR, et al. Endometriose cutânea primária- relato de caso. Diagn Tratamento. 2006;11:144-6.
-
5Carvalho BR, Rosa e Silva JC, Rosa e Silva ACJS, Barbosa HF, Poli Neto OB, Reis FJC, et al. Endometriose umbilical sem cirurgia pélvica prévia. Rev Bras Ginecol Obstet. 2008;30:167-70.
-
6Agarwal A, Fong Y F. Spontaneous endometriosis. Singapore Med J. 2008;49:704-9.
-
7Chatzikokkinou P, Thorfinn J, Angelidis K, Papa G, Trevisan G. Spontaneous endometriosis in an umbilical skin lesion. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:126-30.
-
8Attia L, Ben Temime R, Sidhom J, Sahli A, Makhlouf T, Chachia A, et al. A case of cutaneous endometriosis development on an abdominal scar. Tunis Med. 2010;88:841-3.
-
9Esteves T, Cabrita J R, Coelho Vale E. Endometriose cutânea- a propósito de um caso clínico. Dermatol On Line J. 2010;16:9
-
10Nácul AP, Spritzer PM. Aspectos atuais do diagnóstico e tratamento da endometriose. Rev Bras Ginecol Obstet. 2010;32:298-307.
-
* Study carried out at the Naval Hospital Marcílio Dias (HNMD) - Rio de Janeiro (RJ), Brazil.
Publication Dates
-
Publication in this collection
Feb 2013
History
-
Received
18 Aug 2011 -
Accepted
16 Jan 2012