Abstracts
Cutaneous mucinosis is a group of conditions involving an accumulation of mucin or glycosaminoglycan in the skin and its annexes. It is described in some connective tissue diseases but never in association with mixed connective tissue disease. This report concerns two cases of cutaneous mucinosis in patients with mixed connective tissue disease in remission; one patient presented the papular form, and the other reticular erythematous mucinosis. These are the first cases of mucinosis described in mixed connective tissue disease. Both cases had skin lesions with no other clinical or laboratorial manifestations, with clinical response to azathioprine in one, and to an association of chloroquine and prednisone in the other.
Autoimmune diseases; Lupus erythematosus, cutaneous; Mixed connective tissue disease; Mucinoses
A mucinose cutânea é um grupo de condições em que há um acúmulo de mucina ou glicosaminoglicanos na pele e seus anexos. É descrita em algumas doenças do tecido conjuntivo, porem nunca em associação com doença mista do tecido conjuntivo. Relatamos dois casos de mucinose cutânea em pacientes com doença mista do tecido conjuntivo em remissão, um apresentava-se sob a forma papular e outro sob a forma reticular eritematosa de mucinose. Estes são os primeiros casos de mucinose descritos na doença mista do tecido conjuntivo. Ambos os casos apresentaram o quadro cutâneo de modo isolado, sem nenhuma outra manifestação clínico-laboratorial, havendo resposta à azatioprina em um e à cloroquina associada a prednisona no outro.
Doença mista do tecido conjuntivo; Doenças auto-imunes; Lupus eritematoso cutâneo; Mucinoses
INTRODUCTION
Cutaneous mucinosis is a group of conditions involving an accumulation of mucin or glycosaminoglycan (GAG) in the skin and its annexes. It can occur in some diffuse connective tissue diseases (DCTD) such as lupus erythematosus, but to the best of our knowledge it has never before been reported in association with mixed connective tissue disease (MCTD).
CASE REPORTS
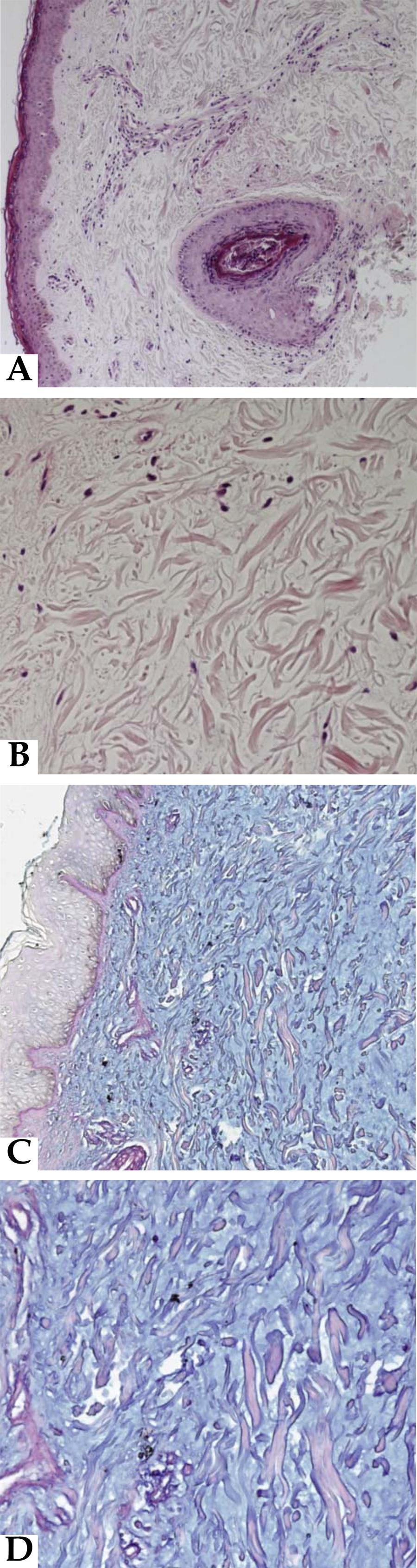
CASE 1: A female patient, 44-years-old, diagnosed with MCTD (Kasukawa's classification criteria) for eight years. She had Raynaud's phenomenon, swollen hands, polyarthritis, photosensitivity, esophageal ectasia, leukopenia, lymphopenia, predominantly axonal peripheral sensorimotor polyneuropathy, sensorineural hearing loss and anterior uveitis. Anti-RNP antibodies titers were 1/1200 (haemaglutination). The patient remained stable for over one year taking azathioprine (1.5 mg/ kg / day) and when joint activity initiated was treated with prednisone 10 mg/ day and leflunomida, with improvement (Figure 1). A month later she noticed papules on the neck, back and face, which were biopsied. The histopathology analysis revealed a mild lymphocytic infiltrate in lymphocytic perivascular and periadnexal areas in the superficial dermis, with some melanophages and collagen fibers dissociation (Figure 2). The PAS showed focal increase of the basal layer of the epidermis. The deposition of mucin was confirmed by Alcian-Blue staining. The epidermis was normal. Immunofluorescence showed no deposition of C3, anti-IgM, anti-IgG or anti-IgA antibodies. Histopathological findings were therefore consistent with cutaneous papular mucinosis. The appearance of this skin condition occurred independently of other manifestations of MCTD. The dose of azathioprine was increased to 2mg/kg/day. This led to an improvement of the lesions.
A and C: Histopathology analysis: mild lymphocytic infiltrate in superficial dermis, and collagen fibers dissociation, with normal epidermis. B and D: The deposition of mucin was confirmed by Alcian-Blue staining. A (100X); B (200X); C and D(400X)
CASE 2: A 42-year-old male, diagnosed with MCTD (Kasukawa's classification criteria) for eight years. He had Raynaud's phenomenon, hand swelling, pleurisy, lymphadenopathy, arthritis, myopathy and anti-RNP antibodies titers 1/6400 (haemaglutination. The patient remained clinically stable for more than seven months with prednisone 15mg/day and azathioprine 2.0 mg/ kg / day when he presented erythematous-violaceous indurated mildly pruritic and painless lesions in the face, trunk and upper limbs (Figure 3). As there were no other signs of MCTD disease activity, the dose of prednisone was reduced to 7.5 mg/ day and azathioprine was discontinued. Histopathological analysis of papules of the trunk showed epidermal parakeratosis and hyperorthokeratosis. Perivascular, interstitial and periadnexal lymphocytic inflammatory infiltrate appeared in the dermis (predominantly the former). The alcian-blue and the PAS staining revealed interstitial mucinosis in the reticular dermis. Chloroquine diphosphate was introduced (250 mg/ day) and the prednisone dose was increased to 20 mg/ day, with improvement of the lesions.
DISCUSSION
Cutaneous mucinosis covers a heterogeneous group of diseases involving a diffuse and/ or focal mucin accumulation in the skin and its annexes.11. Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol. 1992;27:312-5.,22. Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.The diseases can be classified in two groups: primary cutaneous mucinoses that manifest with clinical dermatologic applications (e.g. lichen myxedema, reticular erythematous mucinosis and scleromixedema), and mucinosis associated with other diseases,22. Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.including certain endocrinopathies, especially thyroid diseases, toxic diseases (toxic oil syndrome), Eosinophilia-Myalgia Syndrome, nephrogenic fibrosing dermopathy, DCTD and cancer.11. Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol. 1992;27:312-5.,22. Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.,33. Edward M, Fitzgerald L, Thind C, Leman J, Burden AD. Cutaneous mucinosis associated with dermatomyositis and nephrogenic fibrosing dermopathy: fibroblast hyaluronan synthesis and the effect on patient serum. Br J Dermatol. 2007;156:473-9.
Lupus erythematosus (LE) is a rheumatic disease most often associated with secondary mucinosis (cutaneous mucinosis can occur in up to 1.5% of LE cases).22. Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.Mucin deposits have also been reported in other DCTD such as Sjögren syndrome, systemic sclerosis, rheumatoid arthritis, vasculitis and dermatomyositis.33. Edward M, Fitzgerald L, Thind C, Leman J, Burden AD. Cutaneous mucinosis associated with dermatomyositis and nephrogenic fibrosing dermopathy: fibroblast hyaluronan synthesis and the effect on patient serum. Br J Dermatol. 2007;156:473-9.,44. del Pozo J, Almagro M, Martínez W, YebraPimentel MT, GarcíaSilva J, Peña Penabad C, et al. Dermatomyositis and mucinosis. Int J Dermatol. 2001;40:120-4.
The characteristics of the primary and secondary mucinosis overlap, but the underlying cause of the abnormal deposition of mucin is unknown.22. Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.It is suggested that in rheumatic diseases the mucinosis could be related to circulating antibodies stimulating the synthesis of glycosaminoglycans by skin fibroblasts.
The release of cytokines is an important factor in regulating the production of mucina.33. Edward M, Fitzgerald L, Thind C, Leman J, Burden AD. Cutaneous mucinosis associated with dermatomyositis and nephrogenic fibrosing dermopathy: fibroblast hyaluronan synthesis and the effect on patient serum. Br J Dermatol. 2007;156:473-9.
Hyaluran and chondroitin sulfate are able to activate and attract inflammatory cells, with a resulting local increase in cytokines in vitro. Glycosaminoglycan (GAGs) are increased in dermatomyositis and lupus skin lesions. Their involvement in the pathophysiology of these lesions is therefore suggested.55. Chang LM, Maheshwari P, Werth S, Schaffer L, Head SR, Kovarik C, et al. Identification and Molecular Analysis of Glycosaminoglycans in Cutaneous Lupus Erythematosus and Dermatomyositis. J Histochem Cytochem. 2011;59:336-45.
In LE, the mucin deposits may occur with or without other systemic manifestations.11. Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol. 1992;27:312-5.The LE chronic plaque featuring mucin is classically known as lupus tumidus. The lesions appear as reticular erythematous macules, papules and plaques, located symmetrically in the center of the chest and back, and quite similar to reticular erythematosus mucinosis (REM). However, in this form of mucinosis, the typical LE changes in epidermis and basement membrane are absent and immunofluorescence is negative.11. Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol. 1992;27:312-5.In the first case we found the typical histological findings of papular mucinosis. In the second case, although the histology had shown mild epidermal involvement, there were no other changes typical of LE; mucin deposition was found only in the reticular dermis, while in LE it would have been found throughout it. These findings point to the diagnosis of reticular mucinosis.
No specific treatment exists for cutaneous mucinosis related to DCTD. Therapy is usually directed towards the underlying disease. In idiopathic forms, numerous treatments have already been reported, especially for the generalized forms. In Case 1 a significant improvement was noted after increasing the azathioprine dose, and in Case 2 the response occurred using an association of chloroquine diphosphate and prednisone. The response to antimalarial drugs has already been mentioned in various reports and series of cases.11. Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol. 1992;27:312-5.,22. Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.,66. Dias ED, Schetinne AP, Lima IC, Souza MAS, Souza IS. REM syndrome associated with systemic lupus erythematosus and hypotiroidism. An Bras Dermatol. 2005;80:S376-9.,77. Clarke JT. Recognizing and managing reticular erythematous mucinosis: comment on "Clinical features and efficacy of antimalarial treatment for reticular erythematous mucinosis". Arch Dermatol. 2011;147:715.In refractory cases the use of intralesional or systemic corticosteroids could be effective, with the good response due to suppression of T cells, keratinocytes and fibroblasts, with a consequent reduction of the proliferation of the extracelular matrix.88. s1dLan C, Li C, Yang M, Mei X, He Z, Chen W, et al. Pretibial myxoedema with autoimmunity and hyperplasia treated with glucocorticoids and surgery. Br J Dermatol. 2012;166:457-9.Partial regression of nodular lesions has been reported with intralesional injection of hyaluronidase. In generalized forms thalidomide was effective in some cases and isotretinoin has been used with good response.99. Sansbury JC, Cocuroccia B, Jorizzo JL, Gubinelli E, Gisondi P, Girolomoni G. Treatment of recalcitrant scleromyxedema with thalidomide in 3 patients. Am Acad Dermatol. 2004;51:126-31.,1010. Singh S, Kanwar AJ, Saikia UN. Scleromyxoedema with disseminated subcutaneous nodules: rare presentation of an uncommon dermatosis. Clin Exp Dermatol. 2013;38:36-9.Several other immunosuppressant agents such as cyclophosphamide, melphalan and azathioprine have been used with variable responses to severe forms, but there are no reports in localized forms.
These are the first reports of mucinosis in MCTD. In both cases, the appearance of skin lesions occurred during good control of other underlying disease. There was a clinical response to azathioprine in one case and to chloroquine plus prednisone in the other.
REFERENCES
-
1Lowe L, Rapini RP, Golitz LE, Johnson TM. Papulonodular dermal mucinosis in lupus erythematosus. J Am Acad Dermatol. 1992;27:312-5.
-
2Rongioletti F, Rebora A. The new cutaneous mucinosis: A review with an up-to- date classification of cutaneous mucinosis. J Am Acad Dermatol. 1991;24:265-70.
-
3Edward M, Fitzgerald L, Thind C, Leman J, Burden AD. Cutaneous mucinosis associated with dermatomyositis and nephrogenic fibrosing dermopathy: fibroblast hyaluronan synthesis and the effect on patient serum. Br J Dermatol. 2007;156:473-9.
-
4del Pozo J, Almagro M, Martínez W, YebraPimentel MT, GarcíaSilva J, Peña Penabad C, et al. Dermatomyositis and mucinosis. Int J Dermatol. 2001;40:120-4.
-
5Chang LM, Maheshwari P, Werth S, Schaffer L, Head SR, Kovarik C, et al. Identification and Molecular Analysis of Glycosaminoglycans in Cutaneous Lupus Erythematosus and Dermatomyositis. J Histochem Cytochem. 2011;59:336-45.
-
6Dias ED, Schetinne AP, Lima IC, Souza MAS, Souza IS. REM syndrome associated with systemic lupus erythematosus and hypotiroidism. An Bras Dermatol. 2005;80:S376-9.
-
7Clarke JT. Recognizing and managing reticular erythematous mucinosis: comment on "Clinical features and efficacy of antimalarial treatment for reticular erythematous mucinosis". Arch Dermatol. 2011;147:715.
-
8s1dLan C, Li C, Yang M, Mei X, He Z, Chen W, et al. Pretibial myxoedema with autoimmunity and hyperplasia treated with glucocorticoids and surgery. Br J Dermatol. 2012;166:457-9.
-
9Sansbury JC, Cocuroccia B, Jorizzo JL, Gubinelli E, Gisondi P, Girolomoni G. Treatment of recalcitrant scleromyxedema with thalidomide in 3 patients. Am Acad Dermatol. 2004;51:126-31.
-
10Singh S, Kanwar AJ, Saikia UN. Scleromyxoedema with disseminated subcutaneous nodules: rare presentation of an uncommon dermatosis. Clin Exp Dermatol. 2013;38:36-9.
-
*
Study conducted at the Rheumatology and Dermatology Department of the Hospital das Clínicas of the Faculty of Medicine, University of São Paulo (HC-FMUSP) - São Paulo (SP), Brazil.
Publication Dates
-
Publication in this collection
Aug 2013
History
-
Received
17 June 2012 -
Accepted
19 Sept 2012