Abstracts
Psoriasis is a relatively frequent inflammatory dermatosis. Scarring alopecia due to scalp psoriasis was first reported in 1972, but few reports have been written since then, showing that this is a very rare complication of a common disorder. We report a young Brazilian woman with longstanding scalp psoriasis, which progressed to scaring alopecia.
Alopecia; Psoriasis; Scalp
A psoríase é uma dermatose inflamatória que atinge com relativa frequência o couro cabeludo. Alopecia cicatricial devido à psoríase do couro cabeludo foi publicada pela primeira vez em 1972, mas poucos relatos foram escritos desde então. Aqui nós relatamos uma jovem brasileira com psoríase do couro cabeludo de longa data, que evoluiu para alopecia cicatricial.
Alopecia; Couro cabeludo; Psoríase
INTRODUCTION
Psoriasis is a chronic, recurrent and relatively frequent inflammatory dermatosis. Between 50% and 80% of patients present scalp involvement alone or in conjunction with lesions on other parts of the body. Typical scalp psoriasis shows well-demarcated erythematous plaques covered by silver-colored scales affecting various percentages of the scalp.11. Arruda LHF, Campbell GAM, Takahashi MDF. Psoriasis. An Bras Dermatol. 2001;76:141-67.,22. Sola-Ortigosa J, Sánchez-Regaña M, Umbert-Millet P. An update on scalp psoriasis. Actas Dermosifiliogr. 2009;100:536-43.
Hair loss is a common complaint in psoriatic patients with scalp involvement, but telogen effluvium due to the inflammatory process and trauma, caused by scratching of itchy lesions, are believed to be the cause in most of these cases.33. Runne U, Kroneisen-Wiersma P. Psoriatic alopecia: acute and chronic hair loss in 47 patients with scalp psoriasis. Dermatology. 1992;185:82-7. Few reports of scarring alopecia due to psoriasis have been published.
Here we report a young Brazilian woman with longstanding scalp psoriasis which evolved to scaring alopecia.
CASE REPORT
A 42-year-old Caucasian woman with a 22-year history of severe scalp psoriasis presented to our outpatient clinic complaining of itchy scalp and diffuse hair loss for the last five years. Increased hair shedding was associated with episodes of greater inflammation and pruritus. Nail and articular psoriasis were absent. Psoriatic lesions had always been confined to her scalp. Topical clobetasol, oral cyclosporine, methotrexate, UVB-NB phototherapy and antibiotics had been used as treatment with only temporary relief.
On physical examination, diffuse erythema, infiltration, scales and crusts were present all over the scalp. Decreased hair density in the fronto-parietal area was observed. The right parietal side was the most severely affected, so both dermoscopy and skin biopsies were performed in this area (Figures 1 and 2). Fungal assessment, from both scalp scales and hair shafts, were negative.
Dermoscopy showed interfollicular twisted red loops characteristic of scalp psoriasis and lack of follicular openings (Figure 3). No pustules or tufted hairs were observed.
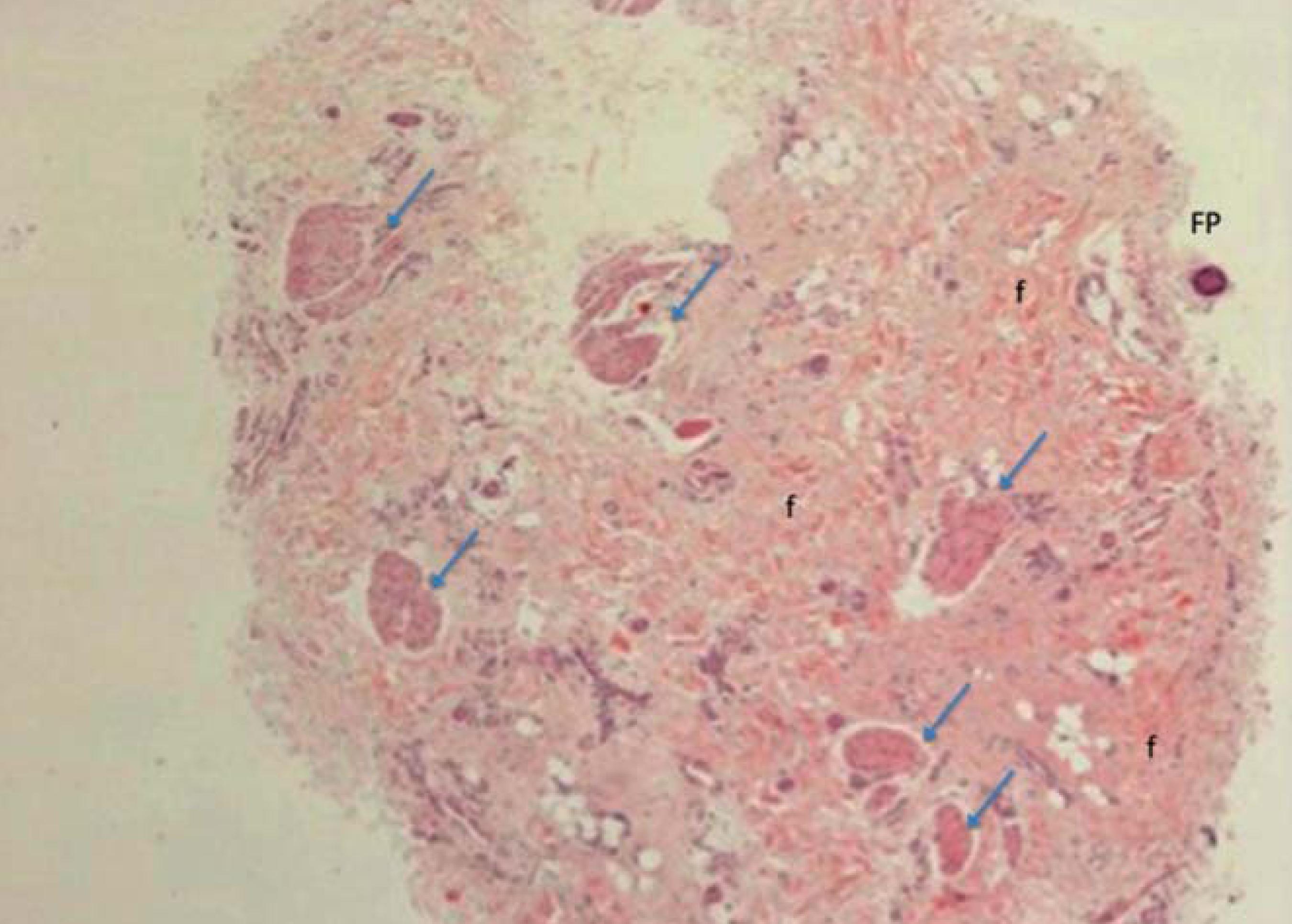
Horizontal sectioning of the biopsy specimen showed follicular drop-out with only one follicle at the subcutaneous level and 3 vellus follicles at the dermis level (Figures 4 and 5). Sebaceous glands were not visualized at all, but isolated pili erector muscles were present and fibrosis could also be observed (Figure 4). No signs of androgenic alopecia were detected.
Horizontal section. Follicular drop-out with only one follicle (FP) at subcutaneous level, fibrosis (f) and isolated pili erector muscles (arrows). HE 40X
Vertical analysis showed epidermal changes compatible with psoriasis and a moderate chronic inflammatory infiltrate around vessels and eccrine glands, associated with fibrous tracts (Figure 6). No interface changes were observed at the dermal-epidermal level or affecting the follicular epithelium.
Vertical section. Hiperkeratosis, regular acathosis, fusion of epidermal cones (psoriatic changes) associated with chronic inflammatory infiltrate around vessels and eccrine glands and fibrosis (arrows). HE 40X
Direct immunofluorescence was negative for IgG, IgM, IgA and complement.
Findings were consistent with scarring alopecia associated with psoriasiform epidermal changes.
DISCUSSION
Scalp involvement in patients with psoriasis is one of the most frequent manifestations over the course of the disease.44. Shuster S. Psoriatic alopecia. Br J Dermatol. 1972;87:73-7.,55. van de Kerkhof PC, Franssen ME. Psoriasis of the scalp. Diagnosis and management. Am J Clin Dermatol. 2001;2:159-65. Hair loss due to scalp psoriasis is common, but alopecia is almost always non-cicatricial and complete regrowth is observed after inflammation ceases.33. Runne U, Kroneisen-Wiersma P. Psoriatic alopecia: acute and chronic hair loss in 47 patients with scalp psoriasis. Dermatology. 1992;185:82-7.,66. van de Kerkhof PC, Chang A. Scarring alopecia and psoriasis. Br J Dermatol. 1992;126: 524-5.,77. Wright AL, Messenger AG. Scarring alopecia in psoriasis. Acta Derm Venereol. 1990;70:156-9.
Scarring alopecia due to psoriasis was described for the first time in 1972, when Shuster44. Shuster S. Psoriatic alopecia. Br J Dermatol. 1972;87:73-7. described "destructive alopecia" as the least frequent type of hair loss complications associated with psoriasis.
Years later, Wright and Messenger described 3 cases of psoriatic scarring alopecia and for the first time the histopathology was studied and showed adnexotropic lymphohistiocytic infiltrate which destroyed the follicular epithelium.77. Wright AL, Messenger AG. Scarring alopecia in psoriasis. Acta Derm Venereol. 1990;70:156-9. Complete destruction of the follicular epithelium would free keratinized hair shafts directly into the dermis, leading to a granulomatous reaction. Atrophic or absent sebaceous glands were observed.
Van de Kerkhof and Chang described an 18year-old female with a 6-year history of hair loss and a well-demarcated area of scarring alopecia on the scalp.66. van de Kerkhof PC, Chang A. Scarring alopecia and psoriasis. Br J Dermatol. 1992;126: 524-5. The biopsy showed characteristics of scarring alopecia and psoriasis in the interfollicular epidermis.
The largest series of cases was described by Runne and Kroneisen-Wiersma, who studied 47 patients with acute and chronic hair loss in scalp psoriasis.33. Runne U, Kroneisen-Wiersma P. Psoriatic alopecia: acute and chronic hair loss in 47 patients with scalp psoriasis. Dermatology. 1992;185:82-7. Most cases presented complete hair regrowth after local antipsoriatic therapy, but 5 patients presented with scar formation, which showed similar histological findings as the previously described cases.
Four patients with scarring alopecia in scalp psoriasis were reported by Bardazzi et al, where pathology revealed typical aspects of psoriasis in the interfollicular epidermis and reduction in the number of follicular units, which were replaced by fibrous tracts.88. Bardazzi F, Fanti PA, Orlandi C, Chieregato C, Misciali C. Psoriatic scarring alopecia: observations in four patients. Int J Dermatol. 1999;38:765-76.
It is a common observation that long duration and higher severity of scalp psoriasis are the factors most frequently associated with psoriatic scarring alopecia.66. van de Kerkhof PC, Chang A. Scarring alopecia and psoriasis. Br J Dermatol. 1992;126: 524-5.,77. Wright AL, Messenger AG. Scarring alopecia in psoriasis. Acta Derm Venereol. 1990;70:156-9. One exception was published by Schön et al in 2000 in which a HIV-positive 35-year-old patient developed scalp psoriasis with scarring alopecia within only five weeks of overt inflammation.99. Schön MP, Reifenberger J, Gantke B, Megahed M, Lehmann P. Progressive scarring psoriatic alopecia in AIDS. Hautarzt. 2000;51:935-8.
Our patient presented with a long history of severe scalp psoriasis. Scratching and secondary infections are supposed to present the main drivers of the cicatricial process. Scalp pathology showed concomitant findings of psoriasis and cicatricial alopecia, as described in psoriatic scarring alopecia. Other causes of primary and secondary alopecias, such as lichen planus pilaris, lupus erythematosus, folliculitis decal-vans and infectious disorders, were excluded.
Psoriasis can be a cause of secondary cicatricial alopecia. The true incidence of this complication is not known, but appropriate control of psoriasis inflammation is important in order to avoid progression to scarring alopecia.
REFERENCES
-
1Arruda LHF, Campbell GAM, Takahashi MDF. Psoriasis. An Bras Dermatol. 2001;76:141-67.
-
2Sola-Ortigosa J, Sánchez-Regaña M, Umbert-Millet P. An update on scalp psoriasis. Actas Dermosifiliogr. 2009;100:536-43.
-
3Runne U, Kroneisen-Wiersma P. Psoriatic alopecia: acute and chronic hair loss in 47 patients with scalp psoriasis. Dermatology. 1992;185:82-7.
-
4Shuster S. Psoriatic alopecia. Br J Dermatol. 1972;87:73-7.
-
5van de Kerkhof PC, Franssen ME. Psoriasis of the scalp. Diagnosis and management. Am J Clin Dermatol. 2001;2:159-65.
-
6van de Kerkhof PC, Chang A. Scarring alopecia and psoriasis. Br J Dermatol. 1992;126: 524-5.
-
7Wright AL, Messenger AG. Scarring alopecia in psoriasis. Acta Derm Venereol. 1990;70:156-9.
-
8Bardazzi F, Fanti PA, Orlandi C, Chieregato C, Misciali C. Psoriatic scarring alopecia: observations in four patients. Int J Dermatol. 1999;38:765-76.
-
9Schön MP, Reifenberger J, Gantke B, Megahed M, Lehmann P. Progressive scarring psoriatic alopecia in AIDS. Hautarzt. 2000;51:935-8.
-
* Work performed at the Trichology Outpatient Clinic of the Hospital das Clinicas, Faculty of Medicine, University of São Paulo (HC-FMUSP) - São Paulo (SP), Brazil.
-
Conflict of interest: None
-
Financial funding: None
Publication Dates
-
Publication in this collection
Nov-Dec 2013
History
-
Received
01 Nov 2012 -
Accepted
22 Mar 2012