Abstracts
We describe a clinical case involving a 62-year-old white male, diagnosed with lymphocytoma cutis (Spiegler-Fendt sarcoid) in the cephalic segment. The diagnosis was carried out by pathological study and confirmed by immunohistochemical panel: evidence of polyclonality. Phototherapy sessions were suggested as treatment (13 PUVA sessions, with an accumulated dose of 58.65 J/cm2 ). The improvement was partial. Thus, infiltration of triamcinolone was opted for (one intralesional infiltration every 3 weeks). After 5 sessions, satisfactory improvement was observed: regression of nearly all the lesions.
Immunohistochemistry; Lymphoma; Pseudolymphoma; Triamcinolone acetonide
Relatamos um caso de um paciente de 62 anos, branco e com diagnóstico de linfocitoma cutis (Sarcoide de Spigler-Fendt) em segmento cefálico. O diagnóstico foi confirmado pelo histopatológico e reafirmado pelo painel imuno-histoquímico: evidência de policlonalidade. Sessões de fototerapia foram propostas como tratamento: 13 sessões de PUVA cuja dose acumulada foi de 58.65 J/cm2); a melhora foi parcial. Optado, então, por infiltrações de triancinolona (uma infiltração intralesional a cada 3 semanas). Na quinta sessão, satisfatória melhora já podia ser evidenciada: regressão de quase todas as lesões.
Imunoistoquímica; Linfoma; Pseudolinfoma; Triancinolona acetonida
INTRODUCTION
Lymphocytoma cutis, or Spiegler-Fendt sarcoid, is classed as one of the
pseudolymphonas,11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1. referring to inflammatory
disorders in which the accumulation of lymphocytes on the skin resemble, clinically and
histopathologically, cutaneous lymphomas.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.
2. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso.
Rev Cent Dermatol Pascua. 2003;12:75-8.-33. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial
histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas
(linfocitoma): Estudo de três casos. An Bras Dermatol.
1995;70:319-21.
In order to obtain an accurate diagnosis, careful clinical evaluation is needed, as well
as histopathological and immunohistochemical exams.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.
2. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso.
Rev Cent Dermatol Pascua. 2003;12:75-8.-33. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial
histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas
(linfocitoma): Estudo de três casos. An Bras Dermatol.
1995;70:319-21.
Here, we describe a case involving a patient over 60, with lesions distributed across upper parts of the head, whose final diagnosis was lymphocytoma cutis.
Despite the improvement in the lesions following corticoid infiltrations, the patient remains under clinical observation, since, in some cases, the condition can evolve into cutaneous lymphoma.
CASE REPORT
White male, 62, suffering for a year from lesions in the skin in the frontal, zygomatic lateral and temporal anterior (both bilaterally), regions. There was no itching but he experienced occasional pain to local palpation. He sought help from doctors, who prescribed ketoconazole shampoo and antihistamines, among other medications, but to no avail.
The patient denied being a smoker or a heavy drinker, and was taking omeprazole to control the reflux disease.
The physical exam revealed macules, papules, nodules and plaques. The lesions presented in an erythematous-violaceous color, and others in erythema-tous-pink. There was no scaling (Figures 1 and 2).
Macules, papules and plaques. Some are erythematous-violaceous and others are erythematous-pink. There are no scaly lesions
Further diagnoses included sarcoidosis, pseudolymphoma and cutaneous lymphoma. Other more unlikely hypotheses were: luminal eruption, rosacea and erythematous lupus, borreliosis.
Serum exams revealed no alterations. The serum calcium dosage was applied, as a hypercalcemia suggested the diagnosis of sarcoidosis.
The ANF was non-reactive, suggesting, in principle, that the condition was not autoimmune.
There were non-reactive IgM and IgG antiborrelia antibodies, eliminating the possibility of borreliosis.
A chest x-ray revealed no pulmonary alterations (which thus reduced the chances of sarcoidosis). An ultrasound of the abdomen showed the presence of light hepatic steatosis.
The skin biopsy revealed hydropic degeneration of the basal layer. In the dermis, there was chronic and nonspecific inflammatory infiltrate, with a predominance of lymphocytes in the reticular dermis and the formation of lymphoid follicles: germinative centers (Figure 3).
Skin fragment showing inflammatory infiltrate in the dermis. Predominance of lymphocytes in the reticular dermis. Formation of lymphoid follicles: germinative centers. (HE, 100x)
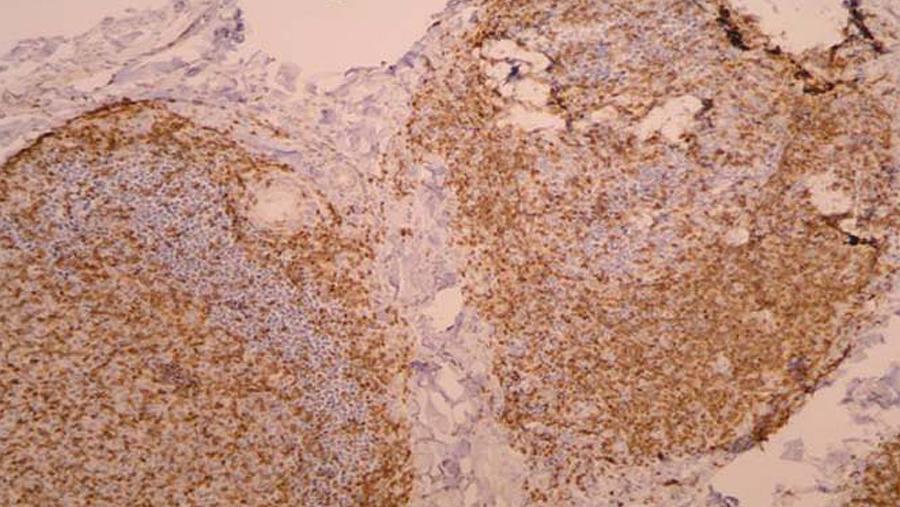
The immunohistocemistry confirmed polyclonal lymphoid infiltrate: lymphocytes B-CD20 and lymphocytes T-CD3 (Figures 4 and 5).
The immunohistochemical analysis was also complemented by the BCL2, CD4, CD7 and CD8, markers: thus reaffirming the polyclonality.
The initial treatment suggested was phototherapy: 13 PUVA sessions were carried out in a period of 2 months, with a total accumulated dose of 58.65 J/cm2 (8-MOP administered twice a week with a dose of 0.65mg/kg). There was some improvement, though the patient could not continue with this treatment.
Hence, the chosen treatment was infiltrations of triamcinolone acetonide 40mg/ml, every 10-15 days. Clinical improvement was noted during the 5th session.(Figure 6)
DISCUSSION
Lymphocytoma cutis, or Spiegler-Fendt sarcoid, can be understood as a lymphoreticular and hyperplasic reaction occurring in the dermis.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas; 2007. p.1270-1.-22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.,44. du Vivier A. Micose fungoide e quadros correlatos. Atlas de Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18. It is a pseudolymphoma of the B cells.44. du Vivier A. Micose fungoide e quadros correlatos. Atlas de Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.-55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
Many possible triggering factors have been identified: acupuncture, earrings, piercings, tattoos, phenytoin, vaccinations, infections from the herpes simplex virus and zoster, insect bites, and infection by the bacterium Borrelia burgdorferi.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas; 2007. p.1270-1.-22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012. However, in most cases, the trigger seems to be idiopathic.22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
It is a rare disease, generally affecting young adults (under the age of 40), with a
predilection for females (3:1).22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso.
Rev Cent Dermatol Pascua. 2003;12:75-8.,44. du Vivier A. Micose fungoide e quadros correlatos. Atlas de
Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.
5. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
6. Arai E, Shimizu M, Hirose T. A review of 55 cases of cutaneous
lymphoid hyperplasia: reassessment of the histopathologic findings leading to
reclassification of 4 lesions as cutaneous marginal zone lymphoma and 19 as
pseudolymphomatous folliculitis. Hum Pathol. 2005;36:505-11.-77. Leinweber B, Colli C, Chott A, Kerl H, Cerroni L. Differential
diagnosis of cutaneous infiltrates of B Lymphocytes with follicular growth pattern.
Am J Dermatopathol. 2004;26:4-13. However, cases involving different age groups have been reported.33. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial
histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas
(linfocitoma): Estudo de três casos. An Bras Dermatol.
1995;70:319-21. It affects predominantly caucasians.55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
Clinically, lesions present as papules and/or nodules that can be shiny.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.
2. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso.
Rev Cent Dermatol Pascua. 2003;12:75-8.
3. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial
histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas
(linfocitoma): Estudo de três casos. An Bras Dermatol.
1995;70:319-21.
4. du Vivier A. Micose fungoide e quadros correlatos. Atlas de
Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.-55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.,88. van Vloten WA, Willemze R. The many faces of lymphocytoma cutis. J
Eur Acad Dermatol Venereol. 2003;17:3-6. They are not scaly and
can be skin-colored, erythematous, brownish or violaceous.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.,44. du Vivier A. Micose fungoide e quadros correlatos. Atlas de
Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012. Itching can occur. In
the literature, it is common to find descriptions of lesions with softened
consistency.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012. In the case under discussion, the consistency of the lesions was
similar to that of non-affected skin.
The localized form accounts for 70% of cases, occurring predominantly on the face or upper limbs. The disseminated form is rarer, found mostly in elderly people, affecting the midsection and extremities, in addition to the face.55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.-66. Arai E, Shimizu M, Hirose T. A review of 55 cases of cutaneous lymphoid hyperplasia: reassessment of the histopathologic findings leading to reclassification of 4 lesions as cutaneous marginal zone lymphoma and 19 as pseudolymphomatous folliculitis. Hum Pathol. 2005;36:505-11.,88. van Vloten WA, Willemze R. The many faces of lymphocytoma cutis. J Eur Acad Dermatol Venereol. 2003;17:3-6. The clinical condition in which there is dissemination of lesions is termed miliary lymphocytoma cutis.22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
Differential diagnoses include: cutaneous lymphoma, sarcoidosis, erythematous lupus,
angiolymphoid hyperplasia, luminal eruption and rosacea.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.
2. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso.
Rev Cent Dermatol Pascua. 2003;12:75-8.-33. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial
histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas
(linfocitoma): Estudo de três casos. An Bras Dermatol.
1995;70:319-21.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
Histopathologically, it is characterized by foci of lymphocytes in the dermis, permeated by histiocytes, bringing about a follicular arrangement that is translated by B cells bordered by T cells, that is to say, the germinative centers. With lymphomas, there are no germinative centers, except in cases of malignant lymphomas of the giant follicular type.33. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas (linfocitoma): Estudo de três casos. An Bras Dermatol. 1995;70:319-21.
The dermis can be separated from the epidermis by a thin area of collagen.22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
Immunohistochemistry reveals the polyclonality (presence of B lymphocytes and T lymphocytes).33. Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas (linfocitoma): Estudo de três casos. An Bras Dermatol. 1995;70:319-21.,55. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
Therapeutics options include systemic corticoids, corticoid infiltrations, superficial
radiotherapy, PUVA, cryosurgery, hydroxychloroquine, surgery, photodynamic therapy.11. Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas;
2007. p.1270-1.,22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso.
Rev Cent Dermatol Pascua. 2003;12:75-8.,44. du Vivier A. Micose fungoide e quadros correlatos. Atlas de
Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.
5. Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz.
PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro,
Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
6. Arai E, Shimizu M, Hirose T. A review of 55 cases of cutaneous
lymphoid hyperplasia: reassessment of the histopathologic findings leading to
reclassification of 4 lesions as cutaneous marginal zone lymphoma and 19 as
pseudolymphomatous folliculitis. Hum Pathol. 2005;36:505-11.-77. Leinweber B, Colli C, Chott A, Kerl H, Cerroni L. Differential
diagnosis of cutaneous infiltrates of B Lymphocytes with follicular growth pattern.
Am J Dermatopathol. 2004;26:4-13.,99. Stoll DM. Treatment of cutaneous pseudolymphoma with
hydroxychloroquine. J Am Acad Dermatol. 1983;8:696-9.,1010. O'Neill J, Fien S, Zeitouni NC. ALA-PDT for treatment of cutaneous
psudolymphoma: a case repor. J Drugs Dermatol. 2010;9:688-9. When the lymphocytoma
cutis is associated with borreliosis, treatment is tailored to this condition.
Follow-up of patients is crucial, as the condition can evolve into cutaneous lymphoma.22. Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.,44. du Vivier A. Micose fungoide e quadros correlatos. Atlas de Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.
ACKNOWLEDGEMENTS
The authors are grateful for the valuable contributions of: Dr. Daniela Chaves Tarquínio, who conducted the phototherapy sessions; and Dr. Mariângela Esther Alencar Marques, who helped in the histopathological study.
REFERENCES
-
1Sampaio SAP, Rivitti EA. Dermatologia 3 ed. São Paulo: Artes Médicas; 2007. p.1270-1.
-
2Lemus SMV, Alarcón H, Ruiz SM. Linfocitoma Cutis. Reporte de un caso. Rev Cent Dermatol Pascua. 2003;12:75-8.
-
3Peçanha PLVB, Pereira Jr AC, Castro O. Diagnóstico diferencial histopatológico e imuno-histoquímico entre linfoma maligno e pseudolinfomas (linfocitoma): Estudo de três casos. An Bras Dermatol. 1995;70:319-21.
-
4du Vivier A. Micose fungoide e quadros correlatos. Atlas de Dermatologia Clínica. 3. ed. São Paulo: Manole; 2000. p.10.17-18.
-
5Nasser N, Nasser Filho N, Rosa TSC. Linfocitoma cutis no nariz. PE-338. In: 67. Congresso Brasileiro de Dermatologia; 2012 set 1-4; Rio de Janeiro, Brasil. Rio de Janeiro: Sociedade Brasileira de Dermatologia; 2012.
-
6Arai E, Shimizu M, Hirose T. A review of 55 cases of cutaneous lymphoid hyperplasia: reassessment of the histopathologic findings leading to reclassification of 4 lesions as cutaneous marginal zone lymphoma and 19 as pseudolymphomatous folliculitis. Hum Pathol. 2005;36:505-11.
-
7Leinweber B, Colli C, Chott A, Kerl H, Cerroni L. Differential diagnosis of cutaneous infiltrates of B Lymphocytes with follicular growth pattern. Am J Dermatopathol. 2004;26:4-13.
-
8van Vloten WA, Willemze R. The many faces of lymphocytoma cutis. J Eur Acad Dermatol Venereol. 2003;17:3-6.
-
9Stoll DM. Treatment of cutaneous pseudolymphoma with hydroxychloroquine. J Am Acad Dermatol. 1983;8:696-9.
-
10O'Neill J, Fien S, Zeitouni NC. ALA-PDT for treatment of cutaneous psudolymphoma: a case repor. J Drugs Dermatol. 2010;9:688-9.
-
* Study carried out at the Clínica Endoderm - Ribeirão Preto (SP), Brazil.
-
Conflict of interest: None
-
Financial funding: None
Publication Dates
-
Publication in this collection
Nov-Dec 2013
History
-
Received
28 Nov 2012 -
Accepted
17 Jan 2013