Abstracts
Impetigo herpetiformis is a rare dermatosis of pregnancy with typical onset during the last trimester of pregnancy and rapid resolution in the postpartum period. Clinically and histologically, it is consistent with pustular psoriasis. This similarity has led some authors to name the disease "the pustular psoriasis of pregnancy". We report the case of a patient who developed impetigo herpetiformis in two sucessive pregnancies.
Case reports; Impetigo; Pregnancy; Psoriasis
Impetigo herpetiforme é uma dermatose gestacional rara que se inicia tipicamente durante o último trimestre e evolui com rápida resolução no período pós-parto. Clinica e histologicamente é consistente com psoríase pustulosa. Essa similaridade tem levado alguns autores a nomearem a doença como "psoríase pustulosa da gestação". Relatamos o caso de uma paciente que apresentou impetigo herpetiforme em duas gestações subsequentes.
Gravidez; Impetigo; Psoríase; Relatos de casos
INTRODUCTION
Impetigo herpetiformis is a rare gestational dermatosis with typical onset in the last trimester of pregnancy and rapid resolution in the postpartum period11. Roth MM, Feier V, Cristodor P, Moguelet P. Impetigo herpetiformis with postpartum flare-up: a case report. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:77-82.,22. Lotem M, Katzenelson V, Rotem A, Hod M, Sandbank M. Impetigo herpetiformis: a variant of pustular psoriasis or a separate entity? J Am Acad Dermatol. 1989;20:338-41. It is clinically and histologically consistent with pustular psoriasis. This similarity has led authors to name the disease "pustular psoriasis of pregnancy".22. Lotem M, Katzenelson V, Rotem A, Hod M, Sandbank M. Impetigo herpetiformis: a variant of pustular psoriasis or a separate entity? J Am Acad Dermatol. 1989;20:338-41.
The maternal-fetal prognosis is uneven. Maternal deaths are rare but there are risks of stillbirth.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9. We report two successive pregnancies of a patient with two different outcomes: stillbirth in the first pregnancy; and a healthy newborn in the second.
CASE REPORT
Patient, female, white, first pregnancy two years ago, at 17 years of age. First assessment at outpatient dermatology service in December 2010, after 27 weeks of pregnancy, due to the appearance of erythematous plaques in the sternal region in week 19, with rapid spread by skin surface. She denied having a history of psoriasis. Patient and fetus were stable from a gynecological standpoint.
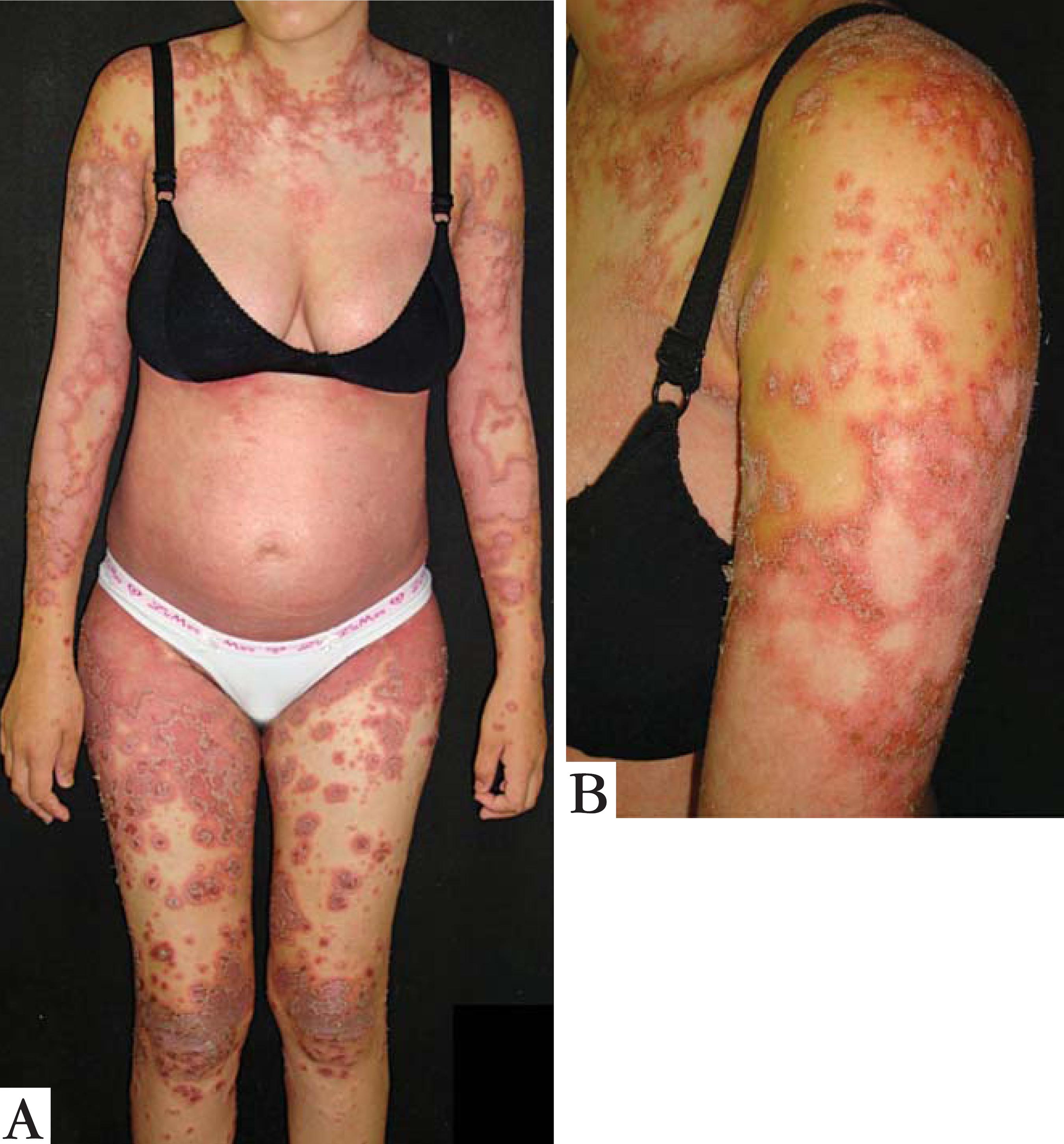
Physical examination showed erythematous, scaly, Figuretive lesions, with pustules on the periphery (Figures 1A and 1B). A biopsy revealed spongiform pustules of Kogoj with neutrophils forming intraepidermal and multilocular microabscesses (Figure 2).
A – 27 weeks into the first pregnancy . B- Detail of lesions on arm. Pustules on the periphery of the lesions.
A – 27 weeks into the first pregnancy . B- Detail of lesions on arm. Pustules on the periphery of the lesions.
Laboratory tests showed leukocytosis of 24.800/mm3, parathormone within reference values (PTH = 45pg/ml) and increased erythrocyte sedimentation rate (ESR = 80mm/h). Serum levels of calcium, sodium and potassium were normal.
Therapy was begun with oral prednisone 60mg per day. Since there was partial improvement, the decision was taken to reduce corticosteroid dose to 40mg per day. At 39 weeks of pregnancy, the patient spontaneously sought gynecological care, worried about decreased fetal movements. Clinical examination and ultrasound proved there was no fetal heartbeat. After finding the stillbirth, labor was induced vaginally. Systemic corticosteroid was reduced gradually during postpartum. However, persistent cutaneous lesions had motivated introduction of oral cyclosporine, with good response. After resolution of cutaneous symptoms, our patient lost dermatological follow.
In June 2012, a woman was referred by the attending physician of her city of origin for obstetric care in our hospital, 37 weeks pregnant and with skin lesions. On that occasion, dermatology was again called. It was found to be the same patient, now aged 19, G2P1 (1 stillborn), with skin lesions that started two weeks before (Figure 3).
In view of poor fetal outcome in the first pregnancy, we instituted supportive treatment with antibiotics and systemic steroids, and suggested delivery resolution to obstetric team. After failure in inducing vaginal delivery, a healthy child was born by cesarean two days after admission. Skin lesions improved progressively and rapidly during postpartum and steroid dosage was gradually reduced.
DISCUSSION
Psoriasis is a chronic disease with a worldwide prevalence of 1-3%.44. Christophers E, Mrowietz U. Psoriasis. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in General Medicine. 6th ed. New York: McGraw Hill; 2003. p.407-27.,55. Martins GA, Arruda L. Systemic treatment of psoriasis - Part I: methotrexate and acitretin. An Bras Dermatol. 2004;79:263-78. Clinical forms can be classified into: vulgaris, guttate, nail, inverted, keratodermic, pustular and erythrodermic. Pustular psoriases can be localized, for instance palmoplantar and continuous acrodermatitis of Hallopeau, or widespread, as in acute forms (von Zumbush), circinate and pregnancy (impetigo herpetiformis).33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.,44. Christophers E, Mrowietz U. Psoriasis. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in General Medicine. 6th ed. New York: McGraw Hill; 2003. p.407-27.,66. Lawley TJ, Yancey KB. Skin changes and diseases in pregnancy. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in general medicine. 6th ed. New York: McGraw Hill; 2003. p.1361-6.
Impetigo herpetiformis (IH) was first described by von Hebra et al, with a report of five pregnant women with pustular grouped lesions, with inflammatory nature and crust evolution, all of which evolved into fetal deaths, in addition to four maternal deaths.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9. Currently, some authors use the term "pustular psoriasis of pregnancy"(PPG), based on the fact that the pustules are sterile and do not present viral etiology.22. Lotem M, Katzenelson V, Rotem A, Hod M, Sandbank M. Impetigo herpetiformis: a variant of pustular psoriasis or a separate entity? J Am Acad Dermatol. 1989;20:338-41.,33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.,77. Hazarika D. Generalized pustular psoriasis of pregnancy successfully treated with cyclosporine. Indian J Dermatol Venereol Leprol. 2009;75:638.,88. Vun YY, Jones B, Al-Mudhaffer M, Egan C. Generalized pustular psoriasis of pregnancy treated with narrowband UVB and topical steroids. J Am Acad Dermatol. 2006;54:S28-30.
Some authors consider the IH/PPG as a variant of pustular psoriasis that occurs during pregnancy, due to clinical and histological similarities.22. Lotem M, Katzenelson V, Rotem A, Hod M, Sandbank M. Impetigo herpetiformis: a variant of pustular psoriasis or a separate entity? J Am Acad Dermatol. 1989;20:338-41. Former PPG criteria included: absence of personal and medical history of psoriasis; self-limited disease development, clearing spontaneously after delivery; and recurrence in subsequent pregnancies.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9. There are, however, reports of personal and familial psoriasis history and non-complete regression of lesions after delivery, as observed by Azulay-Abulafia et al.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9. Hence, PPG is assumed to be a simple variant of generalized pustular psoriasis, representing a pustular stage of the disease, as a result of the hormonal changes of pregnancy or other factors that are not yet understood.22. Lotem M, Katzenelson V, Rotem A, Hod M, Sandbank M. Impetigo herpetiformis: a variant of pustular psoriasis or a separate entity? J Am Acad Dermatol. 1989;20:338-41.,33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.,77. Hazarika D. Generalized pustular psoriasis of pregnancy successfully treated with cyclosporine. Indian J Dermatol Venereol Leprol. 2009;75:638.
Its etiology is still unknown. Association with hypocalcemia and hypoparathyroidism has been suggested, although these findings do not feature in most cases. The role of hormonal contraception, stress, bacterial infection, seasonal variation and certain medications (activated charcoal, potassium iodide and salicylates), is questionable, and more research is needed on this topic.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.
Clinical examination is characterized by lesions initiated in skin folds, with centrifugal spread, in some cases affecting the entire skin surface. There may be poor general condition, fever, diarrhea, dehydration, tachycardia and seizures. The following laboratory findings stand out: leukocytosis, increased ESR and negative bacterial culture of pustules and peripheral blood. Levels of calcium, phosphate and albumin may be reduced. The diagnosis is suggested by PPG clinical and laboratory elements, and is predominantly confirmed by predominantly neutrophilc inflammatory infiltrate, epidermal acanthosis and papillomatosis with focal parakeratosis, upon histological examination. There are neutrophils collections, forming intraepidermal multilocular microabscesses, called spongiform pustules of Kogoj.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.
Differential diagnoses include: pustular psoriasis, dermatitis herpetiformis, erythema multiforme, pustular subcorneal dermatosis and gestational pemphigoid.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.,66. Lawley TJ, Yancey KB. Skin changes and diseases in pregnancy. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in general medicine. 6th ed. New York: McGraw Hill; 2003. p.1361-6.
The treatment of choice during pregnancy is systemic corticosteroids, with 30-60mg of prednisone per day. Cyclosporin may be used in refractory cases.55. Martins GA, Arruda L. Systemic treatment of psoriasis - Part I: methotrexate and acitretin. An Bras Dermatol. 2004;79:263-78. Methotrexate and retinoids are contraindicated during pregnancy.66. Lawley TJ, Yancey KB. Skin changes and diseases in pregnancy. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in general medicine. 6th ed. New York: McGraw Hill; 2003. p.1361-6.,77. Hazarika D. Generalized pustular psoriasis of pregnancy successfully treated with cyclosporine. Indian J Dermatol Venereol Leprol. 2009;75:638. Even if the pustules are sterile, some authors recommend adjuvant treatment with cephalospirin, especially in cases of slight improvement after the introduction of systemic steroids.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9. Replacement of calcium, fluids and electrolytes should be instituted as indicated.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.,66. Lawley TJ, Yancey KB. Skin changes and diseases in pregnancy. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in general medicine. 6th ed. New York: McGraw Hill; 2003. p.1361-6. Although lesions tend to disappear after delivery, there is a risk of recurrence in subsequent pregnancies, presenting earlier, with greater severity and worse maternal-fetal prognosis. This should be made clear to the patient regarding any future reproductive decisions.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.
The current use of steroid and antibiotic therapy has dramatically reduced maternal deaths. However, the risk of stillbirth and perinatal mortality remains high, due to placental insufficiency, premature rupture of membranes, preterm labor and intrauterine growth restriction.33. Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9. Dermatologists and obstetricians must work together to improve the quality of life of the mother and, of course, contribute to a favorable outcome for the fetus.
REFERENCES
-
1Roth MM, Feier V, Cristodor P, Moguelet P. Impetigo herpetiformis with postpartum flare-up: a case report. Acta Dermatovenerol Alp Panonica Adriat. 2009;18:77-82.
-
2Lotem M, Katzenelson V, Rotem A, Hod M, Sandbank M. Impetigo herpetiformis: a variant of pustular psoriasis or a separate entity? J Am Acad Dermatol. 1989;20:338-41.
-
3Azulay-Abulafia L Brotas A, Braga A, Volta AC, Gripp AC. Psoríase pustulosa da gestação (impetigo herpetiforme): relato de dois casos e revisão na literatura. Rev Bras Ginecol Obstet. 2004;26:153-9.
-
4Christophers E, Mrowietz U. Psoriasis. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in General Medicine. 6th ed. New York: McGraw Hill; 2003. p.407-27.
-
5Martins GA, Arruda L. Systemic treatment of psoriasis - Part I: methotrexate and acitretin. An Bras Dermatol. 2004;79:263-78.
-
6Lawley TJ, Yancey KB. Skin changes and diseases in pregnancy. In: Fitzpatrick TB, Eisen AZ, Wolff K, Freedberg IN, Austen KF, editors. Dermatology in general medicine. 6th ed. New York: McGraw Hill; 2003. p.1361-6.
-
7Hazarika D. Generalized pustular psoriasis of pregnancy successfully treated with cyclosporine. Indian J Dermatol Venereol Leprol. 2009;75:638.
-
8Vun YY, Jones B, Al-Mudhaffer M, Egan C. Generalized pustular psoriasis of pregnancy treated with narrowband UVB and topical steroids. J Am Acad Dermatol. 2006;54:S28-30.
-
* Work performed in the dermatology department at the Regional University Hospital of the North of Paraná - State University of Londrina (HURNP-UEL) - Londrina (PR), Brazil.
-
Conflict of interest: None
-
Financial funding: None
Publication Dates
-
Publication in this collection
Nov-Dec 2013
History
-
Received
19 Sept 2012 -
Accepted
19 Oct 2012