Abstract:
Immunosuppressive drugs and biological agents may represent a potential risk of lymphoma development in patients with rheumatoid arthritis. But most cases are diffuse, large B-cell lymphomas. Primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma, a provisional entity in the 2005 WHO-EORTC classification of cutaneous lymphomas, is only described in a limited number of reports. To our knowledge, our case is a rare instance of primary cutaneous CD4+ small/medium-sized pleomorphic T-cell lymphoma, after associated treatment with methotrexate and etanercept, in a patient with moderate rheumatoid arthritis who had undergone an orchidectomy incorrectly.
Keywords:
Biological agents; Lymphoma, T-Cell, peripheral; Lymphoma, T-Cell, cutaneous; Lymphoma, primary cutaneous anaplastic large cell; Methotrexate
INTRODUCTION
Duration of exposure to immunosuppressive drugs may represent a potential risk of lymphoma development in patients with rheumatoid arthritis (RA). Biologic response modifiers have also been associated with a possible risk of lymphoproliferative disease.11 MacKenzie P, Kamili QU, Menter A, Cooper B. Lymphoma and immunosuppression: a report of a case associated with efalizumab Therapy. Clin Lymphoma Myeloma Leuk. 2010;10:E14-6. We describe a rare case of primary cutaneous CD4 positive small/medium-sized pleomorphic T-cell lymphoma (PCSM-TCL), after the associated treatment with methotrexate and etanercept in a patient with RA.
CASE REPORT
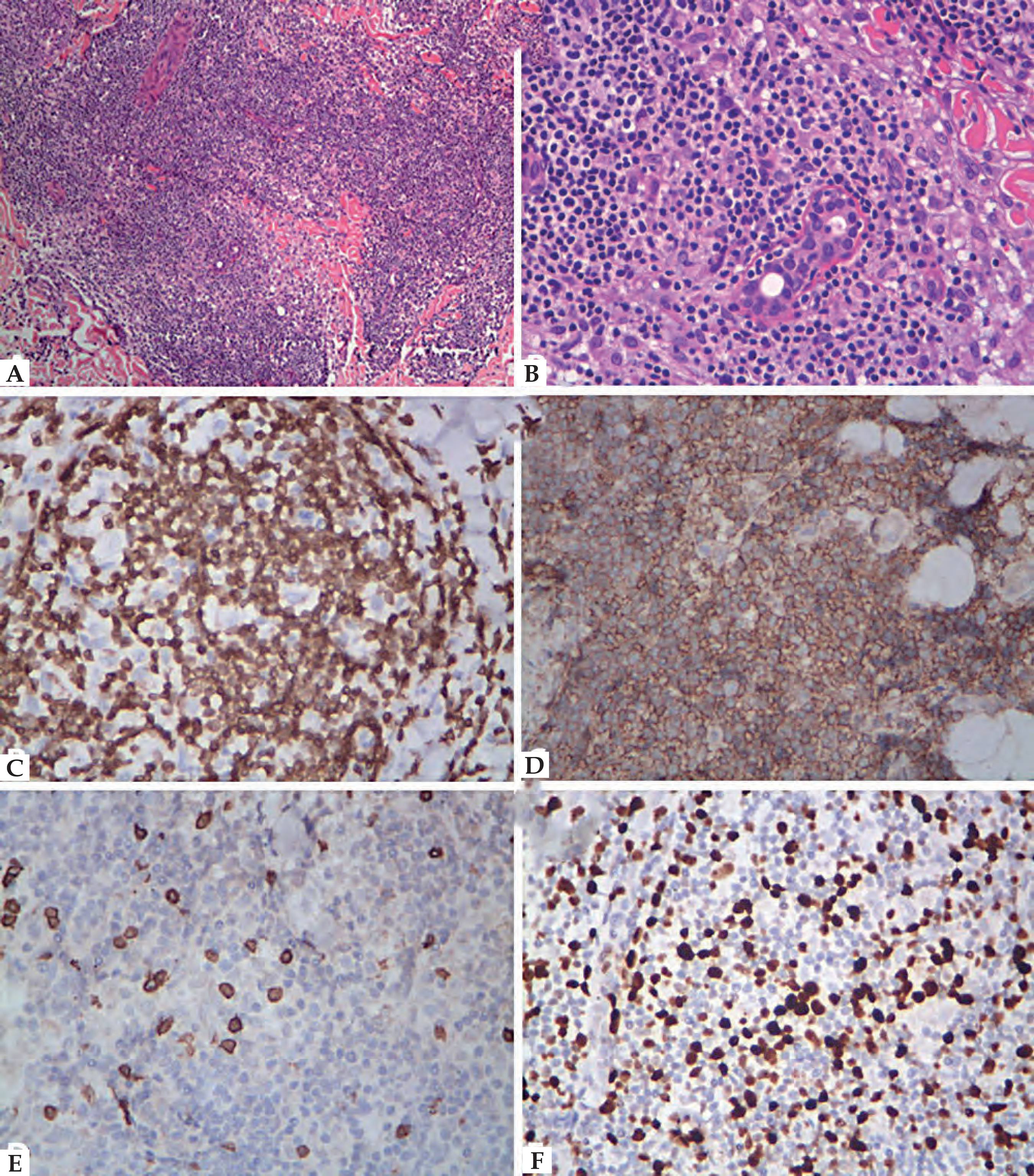
A 62-year-old man had had dark purple nodules and plaques on the face, trunk and bilateral extremities for 8 months (Figure 1). He received a definite diagnosis of RA with moderate disease activity 2 years ago, and responded unsatisfactorily to a 3-month course of methotrexate at 10 mg/wk. Therapeutic regimens were then converted to associated treatment with etanercept 25mg biweekly for the next 3 months. Over the third month only, the patient developed non-tender, bilateral cervical and groin lymphadenopathy and felt gradual nasal obstruction. Microscopic examination of the enlarged lymph node revealed diffuse effacement of the normal nodal architecture by an infiltrate composed of small lymphocytes and macrophages. Nasal mucosa biopsy also revealed numerous lymphoid cells, infiltrated in the dermis. However, the immunohistochemistry showed a polyclonal mixture of lymphocytes. The disorder was therefore thought to represent non-specific inflammation. Because of improvement in joint symptoms, etanercept was continued singly and the dosage was reduced to once weekly for the next 3 months. Due to swelling and gradual bilateral testicular pain, the treatment finally ended. But the groin lymphadenopathy and swollen testes did not resolve following drug withdrawal. Thus, the patient underwent an orchiectomy at the local hospital for presumed testicular neoplasm. Histopathologic examination of the testes tissue revealed folliculus lymphaticus formation and many lymphocytes infiltrated around the epididymis duct. Immunophenotyping indicated positive reactions for: CD3, CD43, CD4, CD8 (partly), CD20 (partly), CD79a (partly), CD38 (partly) and Ki-67 (<1%). Clonal TCR gene rearrangements were negative. Lymphoma was not yet definite at that time. One month later, after the orchiectomy, rufous papules emerged firstly on his face; dark purple nodules and plaques then broke out, spreading to the trunk and bilateral extremities. Physical examination revealed numerous, enlarged, superficial lymph nodes in the groin region. A complete blood count and immunoglobulin levels were normal. A bone marrow biopsy and whole body computed tomography scan resulted negative. Histopathologic examination of the skin nodule on the back revealed an uninvolved epidermis and sheets of small to medium-sized lymphocytes with mild atypia, infiltrated in nodular or diffuse distribution in the dermis, affecting part of the eccrine glands (Figure 2). Immunohistochemistry showed the infiltrative lymphocytes to be strongly positive for CD2, CD3, CD4, CD5, CD7 and CD45RO (Figure 2). Furthermore, staining was focally positive for CD68, CD20, CD79a, CD8, but negative for CD30, CD56, TIA-1, CD23 and Granzyme B (Figure 2). The proliferation rate was 50%, based on Ki-67 expression (Figure 2). Epstein-Barr virus-encoded RNA (EBER-1) in situ hybridization demonstrated negative reactivity. Analysis of the T-cell receptor gamma (TCR-γ) gene rearrangement, using PCR, showed monoclonal rearrangement. A diagnosis of PCSM-TCL was advanced, drawing on the immunophenotype characterization of the infiltrative tumor cells (monomorphic sheets of CD4+ T cells, CD8+ T and B cells were both rare) and the result of clonal TCR-γ gene rearrangement. Since the patient presented persistent waxing and waning of cutaneous nodules but no evidence of systemic involvement, we continued to follow him up without administering any systemic cytotoxic drugs, only low-dose corticosteroids. At the time of writing, the patient was still alive and most of the lesions had disappeared spontaneously.
Histopathological and immunopathological features of the skin lesion. A. HE: small to medium-sized lymphocytes infiltrate in nodular distribution in the dermis; B. HE: mild atypical lymphoid cells affecting part of the eccrine glands. Immunohistochemical staining. C. CD3; D. CD4; E. CD8; F. Ki-67
DISCUSSION
PCSM-TCL is a provisional entity in the 2005 WHO-EORTC classification of cutaneous lymphomas, defined by a predominance of small to medium-sized pleomorphic CD4-positive T cells, infiltrated in the dermis, without the typical clinicopathologic features of mycosis fungoides. Clinically, it is characterized by single or multiple solitary skin plaque(s) and/or nodule(s) on the face, neck and upper trunk. Histopathologic features include dense dermal infiltrates, consisting primarily of small/medium-sized pleomorphic T cells and less than 30% large pleomorphic cells. Epidermotropism is rare, but the infiltrate may extend into the subcutis. Immunohistochemical staining demonstrates, by definition, a CD3+, CD4+, CD30-, CD8- phenotype, and monoclonal T-cell expansion is often exhibited by TCR gene rearrangement studies.22 Baum CL, Link BK, Neppalli VT, Swick BL, Liu V. Reappraisal of the provisional entity primary cutaneous CD41 small/medium pleomorphic T-cell lymphoma: A series of 10 adult and pediatric patients and review of the literature. J Am Acad Dermatol. 2011;65:739-48.
Grogg et al. reported that compared to 20% for unspecified primary cutaneous peripheral T-cell lymphoma, PCSM-TCL had an indolent clinical behavior with a relatively favorable 5-year survival rate of 60-80%.33 Grogg KL, Jung S, Erickson LA, McClure RF, Dogan A. Primary cutaneous CD4-positive small/medium-sized pleomorphic T-cell lymphoma: a clonal T-cell lymphoproliferative disorder with indolent behavior. Mod Pathol. 2008;21:708-15. Similarly, Baum et al. suggested that PCSM-TCL entailed clinically indolent behavior whilst lacking the systemic findings documented in the recent literature.22 Baum CL, Link BK, Neppalli VT, Swick BL, Liu V. Reappraisal of the provisional entity primary cutaneous CD41 small/medium pleomorphic T-cell lymphoma: A series of 10 adult and pediatric patients and review of the literature. J Am Acad Dermatol. 2011;65:739-48.Thus, it is necessary to distinguish PCSM-TCL from other lymphoma types through careful clinicopathologic correlation, and avoid unnecessary treatment for these patients. Cetinözman et al. reported that programmed death-1 (PD-1) could serve as a useful diagnostic marker to differentiate between PCSM-TCL and cutaneous pseudo-T-cell lymphomas on the one hand, and other types of cutaneous T-cell lymphomas (CTCLs) on the other.44 Cetinözman F, Jansen PM, Willemze R.. Expression of programmed death-1 in primary cutaneous CD4-positive small/medium-sized pleomorphic T-cell lymphoma, cutaneous pseudo-T-cell lymphoma, and other types of cutaneous T-cell lymphoma. Am J Surg Pathol. 2012;36:109-16.
The mechanism that accounts for increased incidence of lymphoma in RA patients is not well established and there is an ongoing debate in the field of rheumatology about whether the potentially toxic medications used to treat RA are responsible for the increased risk of lymphoma, or whether the chronic inflammation itself (especially with long-standing and severe disease) is still responsible.55 Kaiser R. Incidence of lymphoma in patients with rheumatoid arthritis: a systematic review of the literature. Clin Lymphoma Myeloma. 2008;8:87-93. In this case, the disease grade for RA was only moderate, while the inchoate lymphoma symptoms, including cervical/groin lymphadenopathy and nasal obstruction, occurred immediately after the employment of immunosuppressive and biological agents. Hence, the medicines may have been the most likely cause of PCSM-TCL in this case. Dermatologists should be aware of the potential adverse reactions when treating severe psoriasis - as well as other inflammatory dermatologic diseases - with immunosuppressive drugs or biologic response modifiers.
-
Financial Support: None.
-
*
Work perfprmed at the Third Affiliated Hospital, Sun Yat-sen University - Guangdong, China.
REFERENCES
-
1MacKenzie P, Kamili QU, Menter A, Cooper B. Lymphoma and immunosuppression: a report of a case associated with efalizumab Therapy. Clin Lymphoma Myeloma Leuk. 2010;10:E14-6.
-
2Baum CL, Link BK, Neppalli VT, Swick BL, Liu V. Reappraisal of the provisional entity primary cutaneous CD41 small/medium pleomorphic T-cell lymphoma: A series of 10 adult and pediatric patients and review of the literature. J Am Acad Dermatol. 2011;65:739-48.
-
3Grogg KL, Jung S, Erickson LA, McClure RF, Dogan A. Primary cutaneous CD4-positive small/medium-sized pleomorphic T-cell lymphoma: a clonal T-cell lymphoproliferative disorder with indolent behavior. Mod Pathol. 2008;21:708-15.
-
4Cetinözman F, Jansen PM, Willemze R.. Expression of programmed death-1 in primary cutaneous CD4-positive small/medium-sized pleomorphic T-cell lymphoma, cutaneous pseudo-T-cell lymphoma, and other types of cutaneous T-cell lymphoma. Am J Surg Pathol. 2012;36:109-16.
-
5Kaiser R. Incidence of lymphoma in patients with rheumatoid arthritis: a systematic review of the literature. Clin Lymphoma Myeloma. 2008;8:87-93.
Publication Dates
-
Publication in this collection
May-Jun 2016
History
-
Received
24 July 2014 -
Accepted
21 Nov 2014