Dear Editor,
Psoriasis is a chronic skin condition that affects 0.5 to 5% of the population. It is characterized by erythematous, scaly plaques, typically affecting the extensor surfaces of the knees and elbows, scalp, intergluteal cleft and sacrum.11 Christophers E. Psoriasis-epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314-20. Around 40% of psoriasis patients have psoriatic arthritis, which leads to physical limitations, decreased quality of life, and increase in patient mortality.22 Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-41.,33 Herrera E, Habicheyn S. Infliximab. Actas Dermosifiliogr. 2008;99:7-13.
Erythrodermic psoriasis is a rare form of psoriasis, characterized by generalized erythema with variable scaling. It is associated with severe morbidity and even mortality, since it can cause hyper or hypothermia leading to decreased cardiac output and affecting liver and renal functions. Erythrodermic psoriasis results from worsening of a previous case of psoriasis or it can develop as the initial presentation of psoriasis. Its treatment is still a challenge and is not yet standardized due to lack of scientific evidence regarding therapeutic recommendations. Traditional systemic therapies include methotrexate, cyclosporine and oral retinoid.44 Belda Junior W, Di Chiacchio N, Criado PR. Tratado de dermatologia. 2. ed. São Paulo: Editora Atheneu; 2014.,55 Lee WK, Kim GW, Cho HH, Kim WJ, Mun JH, Song M, et al .Erythrodermic Psoriasis Treated with Golimumab: A Case report. Ann Dermatol. 2015;27:446-9.,66 Rosenbach M, Hsu S, Korman NJ, Lebwohl MG, Young M, Bebo BF Jr, Van Voorhees AS; National Psoriasis Foundation Medical Board. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:655-62.
Tumor necrosis factor alpha (TNF-alfa) is a key mediator in the pathogenesis of psoriasis, because it is involved in keratinocyte proliferation, endothelial cell regulation and T lymphocyte recruitment.33 Herrera E, Habicheyn S. Infliximab. Actas Dermosifiliogr. 2008;99:7-13. Based on the important role of TNF-alpha in the pathogenesis of psoriasis, the first biologic drugs emerged, which changed radically the treatment for patients with moderate to severe psoriasis.22 Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-41. Infliximab was the first biologic drug used for treatment of psoriasis, approved by the Food and Drug Administration (FDA) in 2006.77 Geller M, Scheinberg MA. Diagnóstico e Tratamento das Doenças Imunológicas. 2. ed. - Rio de Janeiro: Elsevier, 2015. p.195-197.
Erythrodermic psoriasis treatment with traditional systemic medications (methotrexate, cyclosporine and oral retinoid), although effective, is frequently associated with therapeutic failure or intolerance, with the need of alternative strategies. Recently, TNF inhibitor biologic drugs have been used in the treatment of erythrodermic psoriasis with good results.44 Belda Junior W, Di Chiacchio N, Criado PR. Tratado de dermatologia. 2. ed. São Paulo: Editora Atheneu; 2014. We report a case of a patient with erythrodermic psoriasis and psoriatic arthritis that had excellent results using infliximab after 11-year follow up.
Male, 55-year-old patient developed moderate to severe plaque psoriasis 30 years ago. His PASI (Psoriasis Area and Severity Index) was above 10 and he progressed with joint involvement about two months after the appearance of the lesions.
The patient was treated for 18 years at another medical service with topical medications and oral corticosteroids, with periods of remission and exacerbation of the lesions, but with progression of his psoriatic arthritis leading to deformities of the small joints and affecting the hip and knee joints.
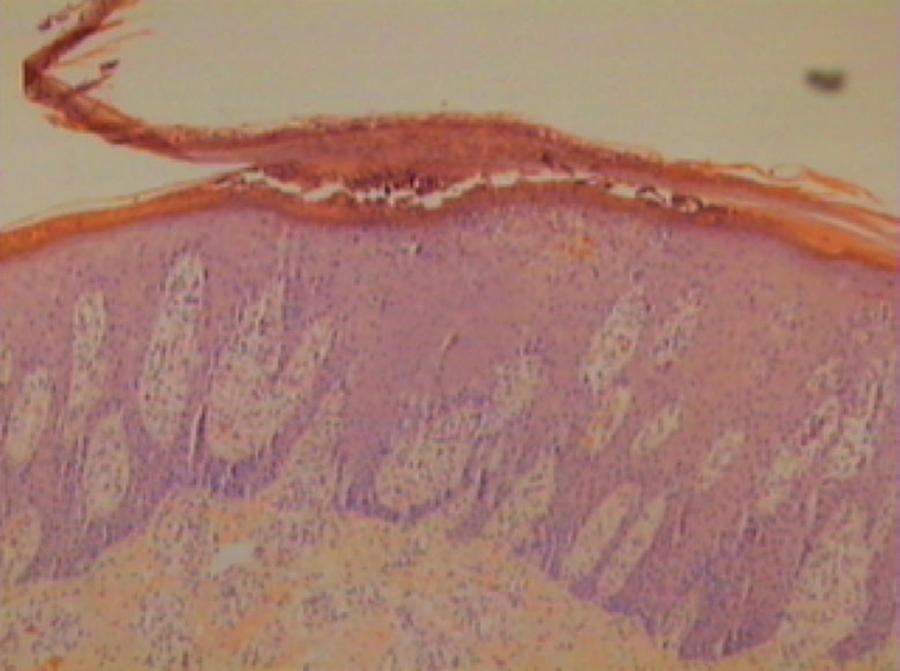
Twelve years ago, the patient was referred to our service with psoriatic exfoliative erythroderma and intense arthralgia (Figure 1). He was admitted and treatment was started with methotrexate 12.5 mg/week for one week and then 25 mg/every week. Biopsy of the lesions confirmed the diagnosis of psoriasis (Figure 2). After three months of treatment, the patient had improvement of the erythroderma and joint pain, but his lesions remained widespread.
Skin biopsy showing parakeratosis and pustule in the stratum corneum, regular acanthosis and suprapapillary thinning. Hematoxylin & eosin, X100
We opted to start infliximab 5 mg/kg/day in three loading doses (weeks 0, 2 and 6) and maintenance doses every eight weeks thereafter. After the second dose, the patient's lesions improved significantly. Methotrexate was discontinued after the seventh dose of infliximab and the patient had variable PASI between 0 and 4 after methotrexate discontinuation (Figure 3).
Since then, infliximab was maintained at 5 mg/kg/day every eight weeks until now, completing 11 years using the medication. His PASI is zero for four years, the patient went back to walking normally soon after the introduction of infliximab and has no joint pain (he only remains with the bone resorption sequelae in the distal phalanges of his hands).
Throughout 11 years of treatment with infliximab, there was no complication or side effect. There are limited data about the efficacy of infliximab in Dermatology. In the available studies, infliximab is well tolerated, with no increase in side effects over time. 88 Castelo-Soccio L, Van Voorhees AS. Long-term efficacy of biologics in dermatology. Dermatol Ther. 2009;22:22-33.
In the reported case, we observed the long-term effectiveness of the medication, for there was no reduction in the therapeutic potential in 11 years.
-
*
Study conducted at Faculdade de Medicina de São José do Rio Preto (FAMERP) - São José do Rio Preto (SP), Brazil.
-
Financial support: None.
REFERENCES
-
1Christophers E. Psoriasis-epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314-20.
-
2Mease PJ, Armstrong AW. Managing patients with psoriatic disease: the diagnosis and pharmacologic treatment of psoriatic arthritis in patients with psoriasis. Drugs. 2014;74:423-41.
-
3Herrera E, Habicheyn S. Infliximab. Actas Dermosifiliogr. 2008;99:7-13.
-
4Belda Junior W, Di Chiacchio N, Criado PR. Tratado de dermatologia. 2. ed. São Paulo: Editora Atheneu; 2014.
-
5Lee WK, Kim GW, Cho HH, Kim WJ, Mun JH, Song M, et al .Erythrodermic Psoriasis Treated with Golimumab: A Case report. Ann Dermatol. 2015;27:446-9.
-
6Rosenbach M, Hsu S, Korman NJ, Lebwohl MG, Young M, Bebo BF Jr, Van Voorhees AS; National Psoriasis Foundation Medical Board. Treatment of erythrodermic psoriasis: from the medical board of the National Psoriasis Foundation. J Am Acad Dermatol. 2010;62:655-62.
-
7Geller M, Scheinberg MA. Diagnóstico e Tratamento das Doenças Imunológicas. 2. ed. - Rio de Janeiro: Elsevier, 2015. p.195-197.
-
8Castelo-Soccio L, Van Voorhees AS. Long-term efficacy of biologics in dermatology. Dermatol Ther. 2009;22:22-33.
Publication Dates
-
Publication in this collection
Sep-Oct 2017
History
-
Received
05 Oct 2016 -
Accepted
16 Mar 2017