Abstract:
Morbihan disease is a rare condition characterized by chronic and persistent erythematous solid edema localized on the face. It is believed to be a complication of rosacea and may occur at any stage of the disease. Features of this condition include variable therapeutic response and great refractoriness. We report a case of a 61-year-old man with rosacea history diagnosed with Morbihan disease, who showed excellent therapeutic response with the combination of deflazacort and oral isotretinoin but developed recurrence after corticosteroid discontinuation. We believe that in severe cases of lymphedema of the face this combination is effective and corticosteroid suspension should be done slowly and gradually.
Keywords:
Glucocorticoids; Isotretinoin; Lymphedema; Rosacea
INTRODUCTION
Morbihan disease is a rare entity with only a few cases reported in the literature. It is characterized by a chronic and recurrent pattern of erythema and symmetrical facial edema, mainly located in the middle and upper thirds of the face (malar regions, nose, glabella, eyelids, and forehead). The evolution of the condition results in deformity of facial contours and even in visual changes.11 Veraldi S, Persico MC, Francia C. Morbihan syndrome. Indian Dermatol Online J. 2013;4:122-4.
CASE REPORT
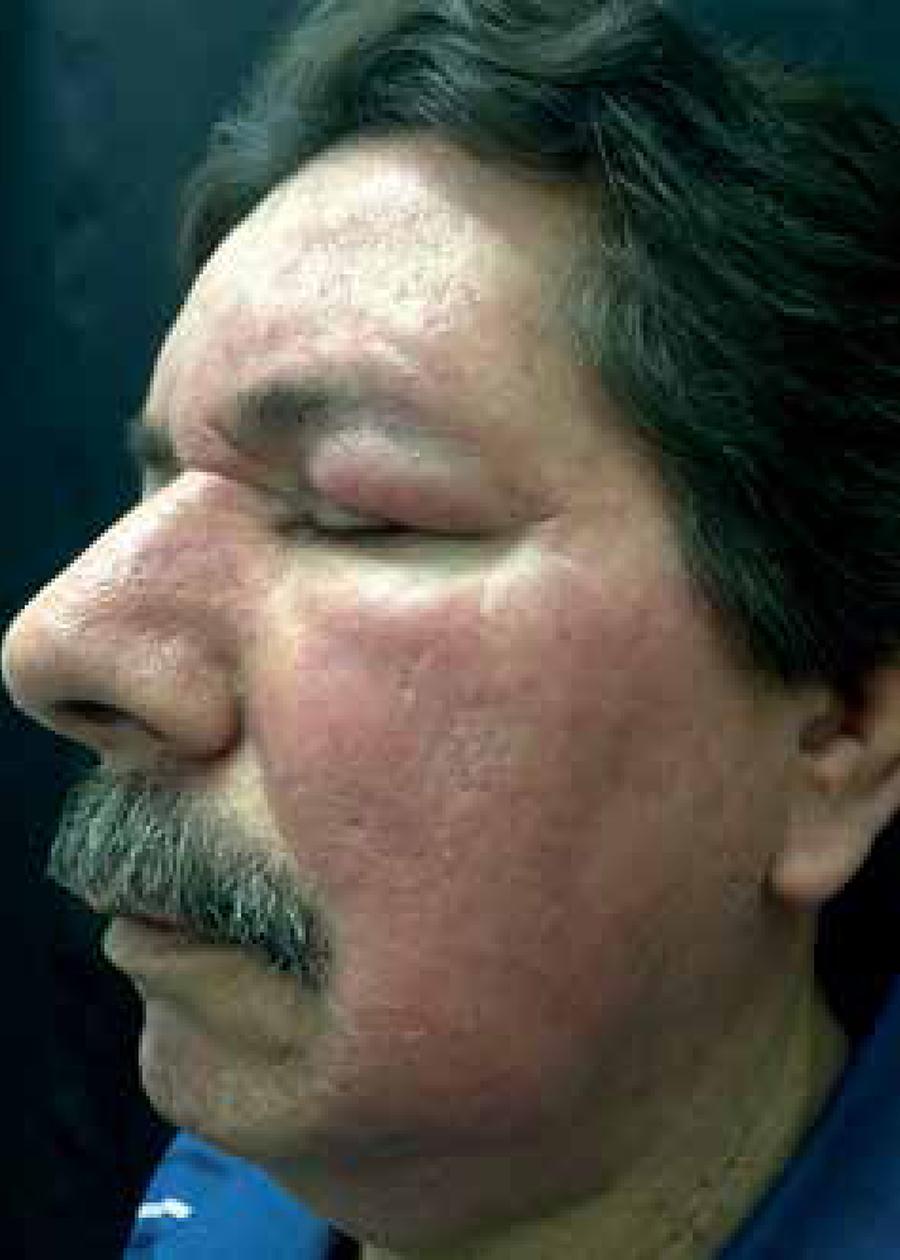
A 61-year-old Caucasian man reported a 20-year history of rosacea, which evolved over the past two years to erythematous, with painless and persistent edema on the face (Figure 1). He complained of a hot sensation on his face and was unhappy with the cosmetic aspect. He reported no visual complaints. He had previously been treated with oral isotretinoin for six months (he was not able to inform the dose he used), with partial response during use and relapse after drug suspension. Laboratory tests were normal. Histopathological examination is shown in Figure 2. The patient started on isotretinoin (20mg - 0.3mg/kg) and deflazacort (30mg) with excellent therapeutic response after one month (Figure 3). Isotretinoin was maintained, and the corticosteroid was discontinued after one month of use, with recurrence occurring within a few days. Topical metronidazole and later oral metronidazole were then associated, but we observed no improvement. We increased the dose of isotretinoin to 40mg (0.5mg/kg), but with no improvement either. Finally, we reintroduced the systemic corticosteroid (deflazacort 30mg/ daily) and maintained isotretinoin (20mg/daily), with significant improvement of the erythema and lymphedema of the face, recommending that a slow and gradual withdrawal of the medication should be done.
Facial fixed erythema and edema, altering facial contours, and telagiectasias, before starting treatment
Figure 1B
Side view of the face before starting treatment
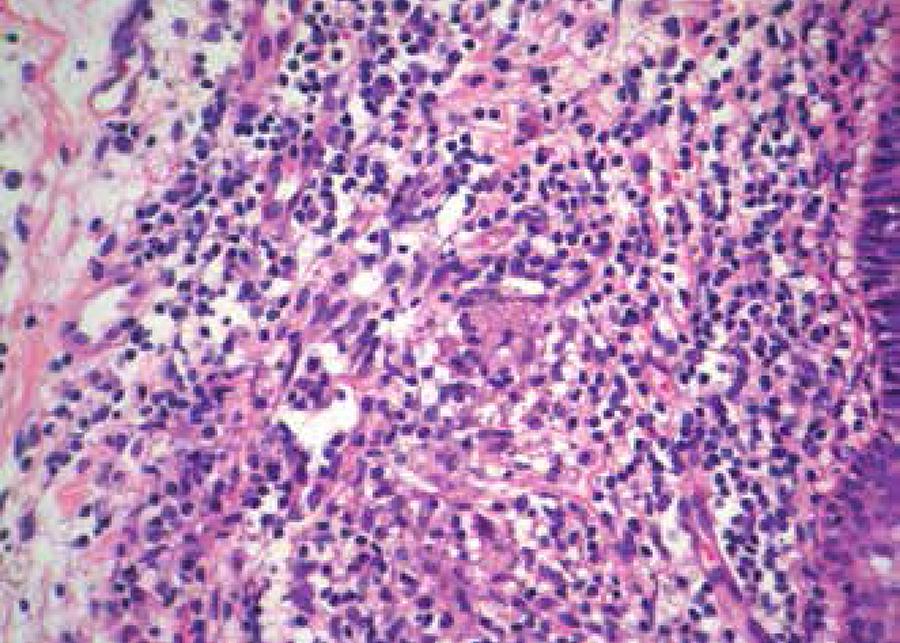
Preserved epidermis; dermis with edema between collagen fibers, dilated vessels with telangiectasias and lymphocytic infiltrate (Hematoxylin & eosin, X40)
Figure 2B
Lymphocytic infiltrate in the dermis with few plasma cells, mast cells and granulomas, as well as Langhans giant cells (Hematoxylin & eosin, X400)
Excellent improvement of erythema and lymphedema after a month of treatment with isotretinoin and deflazacort
Figure 3B
Side view of the face after the first month of treatment
DISCUSSION
Morbihan disease affects Caucasian adults of both genders and is considered by most authors as a clinical variety or complication of acne or rosacea. However, it is unclear whether it is a distinct disease and may occur in patients without clinical manifestations of rosacea.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,33 Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): Evidence of hidden immunologic contact urticária and impaired lymphatic drainage. J Am Acad Dermatol. 2005;52:595-602. The term "Morbihan" refers to a district of France where the first French patient was observed by Robert Degos in 1957.11 Veraldi S, Persico MC, Francia C. Morbihan syndrome. Indian Dermatol Online J. 2013;4:122-4.
Other nomenclatures include rosacea lymphoedema, solid persistent facial edema, and morbus Morbihan.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,44 Chen DM, Crosby DL. Periorbital edema as an initial presentation of rosacea. J Am Acad Dermatol. 1997;37:346-8. The typical finding of Morbihan's disease is non-depressive edema of the upper two thirds of the face, with no tendency for spontaneous regression.55 Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7. However, pitting edema may be evident in its early stages and the typical solid edema appears after fibrotic induration that occurs due to recurrent inflammation.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,66 Morales-Burgos A, Alvarez Del Manzano G, Sánchez JL, Cruz CL. Persistent Eyelid Swelling in a Patient with Rosácea. P R Health Sci J. 2009;28:80-2. The facial erythema is described as poorly defined or as discrete patches or isolated plaques.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8. Its evolution is initially fluctuating but becomes permanent with time, leading to disfigurement of facial contours.77 Romiti N. Morbus Morbihan: edema e eritema sólido e persistente da face. An Bras Dermatol. 2000;75:599-603 Eye involvement with rosacea is common, especially in the form of blepharitis and conjunctivitis. Al-though reported, lymphedema of the eyelids is a rare complication.88 Lai TF, Leibovitch I, James C, Huilgol SC, Selva D. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand. 2004;82:765-7.
The etiology of Morbihan disease is uncertain. Clinical manifestations are presumably caused by derangement of local cutaneous vascularization and disbalance between lymphatic production and drainage.33 Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): Evidence of hidden immunologic contact urticária and impaired lymphatic drainage. J Am Acad Dermatol. 2005;52:595-602.,99 Ranu H, Lee J, Hee TH. Successful treatment of Morbihan's disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23:682-5. There are indications of the association between Morbihan disease and rosacea. Vasodilation and chronic inflammation accompanying rosacea can lead to the destruction of collagen and elastic fibers around the blood vessels in the dermis, resulting in increased vessel permeability and fluid transudation. With chronic evolution, permanent obstruction of lymphatic vessels or fibrosis in the dermis induced by mast cells leads to lymphedema of the underlying tissue.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,55 Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7.,66 Morales-Burgos A, Alvarez Del Manzano G, Sánchez JL, Cruz CL. Persistent Eyelid Swelling in a Patient with Rosácea. P R Health Sci J. 2009;28:80-2.,88 Lai TF, Leibovitch I, James C, Huilgol SC, Selva D. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand. 2004;82:765-7.
9 Ranu H, Lee J, Hee TH. Successful treatment of Morbihan's disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23:682-5.-1010 Erbagci Z. Rosacea lymphoedema responding to prednisolone, metronidazole and ketotifen therapy in a patient with alopecia universalis. Gazi Medical Journal. 2000;11:47-9. Histochemical and immunohistochemical studies show that more than one-third of dilated vessels in lymphedematous skin are lymphatic vessels. Recently, findings such as the increase in D2-40 expression in the lymphatic endothelium of the skin affected by rosacea suggest that the lymphangiogenesis process is early involved in the pathogenesis of rosacea.66 Morales-Burgos A, Alvarez Del Manzano G, Sánchez JL, Cruz CL. Persistent Eyelid Swelling in a Patient with Rosácea. P R Health Sci J. 2009;28:80-2.
Histopathological findings are non-specific and poorly described in the literature. They include edema in the dermis, dilated blood vessels, presence of lymphocytes, neutrophils, and perivascular and perifollicular histiocytes, perifollicular fibrosis, and, rarely, an increase in the number of mast cells.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,55 Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7.,77 Romiti N. Morbus Morbihan: edema e eritema sólido e persistente da face. An Bras Dermatol. 2000;75:599-603,99 Ranu H, Lee J, Hee TH. Successful treatment of Morbihan's disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23:682-5. Nagasaka et al. also reported the formation of granulomas around dilated lymphatic vessels and luminal obstruction by histiocytic infiltration.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,99 Ranu H, Lee J, Hee TH. Successful treatment of Morbihan's disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23:682-5. However, only a few reports reveal granuloma in the dermis. What could explain the absence of granuloma formation in the dermis in previous investigations is the lack of biopsies deep enough to confirm lymphatic involvement and the possibility of Morbihan disease occurring at any stage of rosacea.55 Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7.
Another feature of Morbihan disease is the absence of systemic manifestations and laboratory abnormalities. Clinical history and complete physical examination are important in order to exclude differential diagnoses, which include systemic lupus erythematosus, angioedema, chronic actinic dermatitis, chronic contact dermatitis, dermatomyositis, sarcoidosis, and Melkersson-Rosenthal syndrome.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.,33 Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): Evidence of hidden immunologic contact urticária and impaired lymphatic drainage. J Am Acad Dermatol. 2005;52:595-602.
Treatment options for Morbihan disease reported in the literature are isotretinoin, systemic antibiotics (tetracyclines, metronidazole), antihistamines (ketotifen), and systemic corticosteroids (prednisone, prednisolone). Clofazimine and thalidomide are also reported.11 Veraldi S, Persico MC, Francia C. Morbihan syndrome. Indian Dermatol Online J. 2013;4:122-4. Although about 20% of patients may not respond to oral isotretinoin, it is considered the first-line of therapy.11 Veraldi S, Persico MC, Francia C. Morbihan syndrome. Indian Dermatol Online J. 2013;4:122-4. In 2014 Smith and Cohen showed good results with isotretinoin alone (40mg-80mg/day) for a prolonged period (9-24 months), with no documented recurrence in the five patients reported.22 Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8. Our patient showed no significant improvement with isotretinoin alone. Other studies report the association of isotretinoin with ketotifen or clofazimine, prednisolone with metronidazole and ketotifen, and doxycycline with prednisolone, with variable outcomes.55 Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7.,77 Romiti N. Morbus Morbihan: edema e eritema sólido e persistente da face. An Bras Dermatol. 2000;75:599-603,99 Ranu H, Lee J, Hee TH. Successful treatment of Morbihan's disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23:682-5.,1010 Erbagci Z. Rosacea lymphoedema responding to prednisolone, metronidazole and ketotifen therapy in a patient with alopecia universalis. Gazi Medical Journal. 2000;11:47-9. The association of deflazacort with oral isotretinoin, a regimen used in our study, was not found in the literature. Despite the excellent therapeutic response, we observed a relapse after corticosteroid suspension after one month of use. We believe that in severe cases, with significant lymphedema of the face, like that of our patient, corticosteroid withdrawal should be slow and gradual. Surgical procedures, such as blepharoplasty, may be useful in refractive cases.55 Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7.
The pathogenesis of Morbihan disease is still unclear. Only a few therapeutic options are reported with uncertain results and a high index of refractory cases. However, we believe that early diagnosis and treatment are essential to avoid irreversible lymphatic damage. The association of deflazacort with isotretinoin showed to be effective in our patient, but we should monitor him longer to observe possible relapse after the suspension of treatment.
-
*
Work performed at Hospital Universitário Pedro Ernesto, Universidade do Estado do Rio de Janeiro (HUPE-UERJ) - Rio de Janeiro (RJ), Brazil
-
Financial support: None.
REFERENCES
-
1Veraldi S, Persico MC, Francia C. Morbihan syndrome. Indian Dermatol Online J. 2013;4:122-4.
-
2Smith LA, Cohen DE. Successful Long-term Use of Oral Isotretinoin for the Management of Morbihan Disease. Arch Dermatol. 2012;148:1395-8.
-
3Wohlrab J, Lueftl M, Marsch WC. Persistent erythema and edema of the midthird and upper aspect of the face (morbus morbihan): Evidence of hidden immunologic contact urticária and impaired lymphatic drainage. J Am Acad Dermatol. 2005;52:595-602.
-
4Chen DM, Crosby DL. Periorbital edema as an initial presentation of rosacea. J Am Acad Dermatol. 1997;37:346-8.
-
5Nagasaka T, Koyama T, Matsumura K, Chen KR. Persistent lymphoedema in Morbihan disease: formation of perilymphatic epithelioid cell granulomas as a possible pathogenesis. Clin Exp Dermatol. 2008;33:764-7.
-
6Morales-Burgos A, Alvarez Del Manzano G, Sánchez JL, Cruz CL. Persistent Eyelid Swelling in a Patient with Rosácea. P R Health Sci J. 2009;28:80-2.
-
7Romiti N. Morbus Morbihan: edema e eritema sólido e persistente da face. An Bras Dermatol. 2000;75:599-603
-
8Lai TF, Leibovitch I, James C, Huilgol SC, Selva D. Rosacea lymphoedema of the eyelid. Acta Ophthalmol Scand. 2004;82:765-7.
-
9Ranu H, Lee J, Hee TH. Successful treatment of Morbihan's disease with oral prednisolone and doxycycline. Dermatol Ther. 2010;23:682-5.
-
10Erbagci Z. Rosacea lymphoedema responding to prednisolone, metronidazole and ketotifen therapy in a patient with alopecia universalis. Gazi Medical Journal. 2000;11:47-9.
Publication Dates
-
Publication in this collection
Nov-Dec 2017
History
-
Received
21 Feb 2015 -
Accepted
10 June 2015