Abstract:
We report a case of a 76-year-old patient with a history of recent weight loss and ulcerated umbilical nodular lesion. Initially, we considered the diagnostic hypothesis of Sister Mary Joseph's nodule. However, histopathological evaluation revealed that it was an ulcerated intradermal nevus. We perform a brief review of umbilical nodules.
Keywords:
Abdominal neoplasms; Digestive system neoplasms; Nevus; Nevus, intradermal
CASE REPORT
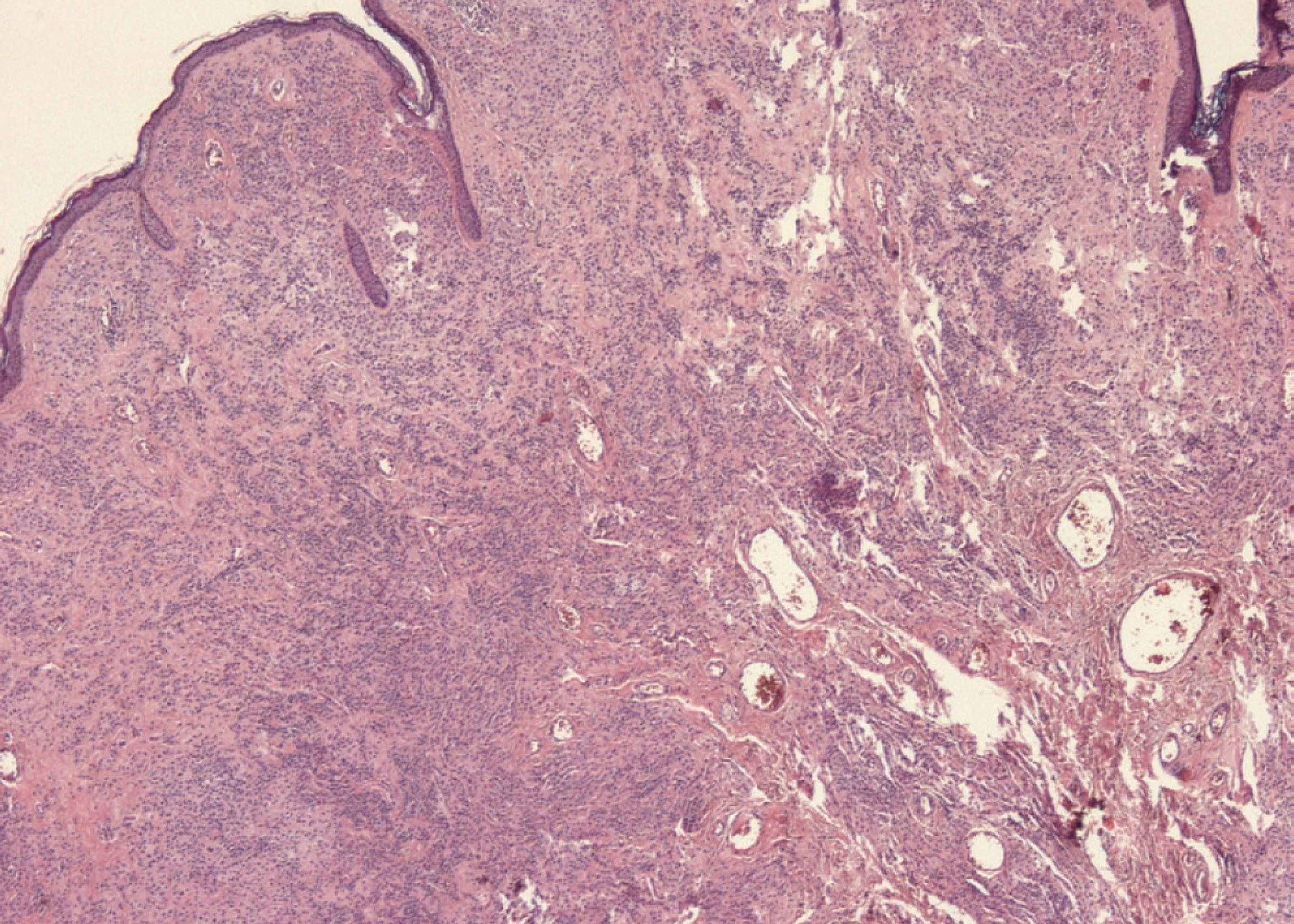
Male patient, 76 years old, with a history of hypertension, smoking, former alcohol consumption, gout, and stroke, admitted to Neurology two months previously with a new stroke and recent weight loss. Physical examination showed a brownish cerebriform umbilical nodule 2cm in diameter surrounded by serous-hematic crust (Figure 1). Patient reported that the lesion was asymptomatic, present for one year, with no recent growth. On dermoscopy, the cerebriform area showed comma-shaped and irregular vessels on a light pink background (Figure 2). The location and dermoscopic clinical features raised the diagnostic hypothesis of Sister Mary Joseph's nodule, and an excisional biopsy was performed. Histopathology showed epidermal atrophy, nevus cells without atypia in the dermis, and preserved deep maturation, interspersed with congested blood vessels (Figures 3 and 4).
Brownish cerebriform umbilical nodule 2cm in diameter with surrounding serous and hematic crust
Dermoscopy of the cerebriform area shows comma-shaped and irregular linear vessels on light pink background
Atrophic epidermis, nevus cells without atypia in the dermis, and preserved deep maturation and interspersed congested blood vessels (Hematoxylin & eosin, x40)
DISCUSSION
Sister Mary Joseph's nodule is a metastasis located in the umbilicus, originating from advanced intraabdominal tumors and with a somber prognosis. Clinically, it presents as a firm, painful, irregular nodule 0.5-2cm in diameter. The surface may also present ulceration, necrosis, and purulent or serous secretion.11 Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D. Umbilical metastasis or Sister Mary Joseph's nodule. Int J Dermatol. 1998;37:7-13. In dermoscopic examination of this nodule, Mun JH et al. described vascular polymorphism with serpentine linear and curved linear vessels with whitish and milky-red unstructured areas. Differential diagnosis should include umbilical hernia, malignant or benign primary tumors on the umbilical region, omphalitis, keloids, pyogenic granuloma, melanocytic nevus, cutaneous endometriosis, and seborrheic keratosis.11 Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D. Umbilical metastasis or Sister Mary Joseph's nodule. Int J Dermatol. 1998;37:7-13.,22 Aich RK, Karim R, Chakraborty B, Dasgupta S, Deb AR. Sister Mary Joseph's nodule. Indian J Med Paediatr Oncol. 2008;2:40-3. Intradermal nevi present as raised lesions, either pigmented or not, which may have a cerebriform appearance. Their most common location is on the face, but they may be found anywhere on the skin surface, although they are uncommon on the palms and soles. On dermoscopy, they present with absence of pigment network and presence of dots and globules. They may also present fine or comma-shaped linear vessels, as in the case described here.33 Mun JH, Kim JM, Ko HC, Kim BS, Kim MB. Dermoscopy of a Sister Mary Joseph nodule. J Am Acad Dermatol. 2013;68:e190-2.,44 Rezze GG, Soares de Sá BC, Neves RI. Dermoscopy: the pattern analysis. An Bras Dermatol. 2006;81:261-8. Thus, Sister Mary Joseph's nodule presents similar dermoscopic alterations to those of intradermal nevus. There are comma-shaped or curved linear vessels in both. In addition, there is no description of a specific lesion in Sister Mary Joseph's nodule, which contributed to the difficulty in the differential diagnosis. In these cases, one should suspect metastatic umbilical nodule, and histopathological examination is essential, considering the prognostic importance of this diagnosis, as performed in the case reported here.
-
*
Work conducted at Hospital do Servidor Público Estadual, São Paulo (SP), Brazil.
-
Financial support: None.
REFERENCES
-
1Dubreuil A, Dompmartin A, Barjot P, Louvet S, Leroy D. Umbilical metastasis or Sister Mary Joseph's nodule. Int J Dermatol. 1998;37:7-13.
-
2Aich RK, Karim R, Chakraborty B, Dasgupta S, Deb AR. Sister Mary Joseph's nodule. Indian J Med Paediatr Oncol. 2008;2:40-3.
-
3Mun JH, Kim JM, Ko HC, Kim BS, Kim MB. Dermoscopy of a Sister Mary Joseph nodule. J Am Acad Dermatol. 2013;68:e190-2.
-
4Rezze GG, Soares de Sá BC, Neves RI. Dermoscopy: the pattern analysis. An Bras Dermatol. 2006;81:261-8.
Publication Dates
-
Publication in this collection
Nov/Dec 2018
History
-
Received
06 July 2017 -
Accepted
07 Jan 2018