Abstract
Background:
Alopecia areata is a highly frequent disease with an impact on quality of life and several treatment options with little clinical confirmatory evidence.
Objective:
To disseminate the recommendations of Brazilian dermatologists with expertise in the treatment of alopecia areata.
Methods:
Eight specialists with expertise in alopecia areata from different university centers were appointed by the Brazilian Society of Dermatology to reach a consensus on its treatment. Based on the adapted DELPHI methodology, the relevant elements were considered; then, an analysis of recent literature was carried out and the consensus was written down. Consensus on the management of alopecia areata was defined with the approval of at least 70% of the panel.
Results/Conclusions:
Intralesional injectable corticotherapy was considered the first option for localized disease in adults. In extensive cases with signs of activity, systemic corticosteroid therapy should be considered and can be used together with immunosuppressants (corticosteroid-sparing agents). The use of an immunosensitizer (diphencyprone) is an option for stable long-term cases. Evaluation of side effects is as important as the rate of hair regrowth.
Keywords
Adrenal cortex hormones; Alopecia areata; Consensus; Methotrexate; Therapeutics
Introduction
Alopecia areata (AA) is an autoimmune disease that targets hair follicles in the anagen phase and causes non-scarring alopecia. AA usually manifests before the age of 40 years, with no predilection for sex or race. The lifetime risk of developing AA is estimated at 2%.11 Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1% by Rochester Epidemiology Project, 1990-2009. J Invest Dermatol. 2014;134:1141-2. In a survey conducted by the Brazilian Society of Dermatology, AA accounted for 1.2% of all dermatological consultations. Among the causes of hair loss, it was only less frequent than androgenetic alopecia and telogen effluvium.22 Sociedade Brasileira de Dermatologia, Miot HA, Penna GO,Ramos AMC, Penna ML, Schmidt SM, et al. Profile of dermatological consultations in Brazil (2018). An Bras Dermatol. 2018;93:916-28.
Most studies on AA treatment do not present a high level of scientific evidence.33 Hordinsky M, Donati A. Alopecia areata: an evidence-based treatment update. Am J Clin Dermatol. 2014;15:231-46. This study aims to guide the treatment and follow-up of patients with AA based on the recommendations of a group of Brazilian specialists.
Methods
Eight specialists with expertise in AA from different university centers were appointed by the Brazilian Society of Dermatology to reach a consensus on its treatment. The adapted DELPHI methodology was used.
The first step was to define the structure of the text and the topics to be addressed. Then, the themes were divided among the participants, who carried out a bibliographic review and drafted the text. Subsequently, all sections and recommendations on the treatment of AA were reviewed and discussed among all members. Consensus was defined as approval by at least 70% of the panel.
Pre-treatment considerations
The pre-treatment considerations are summarized in Table 1.
Clinical presentation
According to the extent and topography of involvement, AA is clinically classified into different patterns, as shown in Table 2.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.–66 Sato-Kawamura M, Aiba S, Tagami H. Acute diffuse and total alopecia of the female scalp. A new subtype of diffuse alopecia areata that has a favorable prognosis. Dermatology. 2002;205:367-73.
In order to determine the different types of treatment for each patient, this consensus considered AA as severe when it affected more than 50% of the scalp or when it affected over 25% of the scalp and presented a rapid evolution or had high impact on patient's quality of life.
Prognosis
AA is a chronic disease of unpredictable course. One may face spontaneous remission or progress to extensive hair loss not responding to any treatment.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23. About 50% of patients with AA experience spontaneous repilation in the first six months and 70% present repilation in the first year, although AA may recur months or years after remission.77 Ikeda T. A new classification of alopecia areata. Dermatologica. 1965;131:421-45.
Extensive forms of the disease generally do not respond well to treatment. Approximately 7% of the patients evolve to the subtypes of total alopecia (TA) or universal alopecia (UA).77 Ikeda T. A new classification of alopecia areata. Dermatologica. 1965;131:421-45. The long-term recovery rates of TA and UA are less than 10%.77 Ikeda T. A new classification of alopecia areata. Dermatologica. 1965;131:421-45. Patients with the “diffuse acute and total” subtype have a favorable prognosis, regardless of treatment.66 Sato-Kawamura M, Aiba S, Tagami H. Acute diffuse and total alopecia of the female scalp. A new subtype of diffuse alopecia areata that has a favorable prognosis. Dermatology. 2002;205:367-73. The factors associated with a worse prognosis are summarized in Table 3.77 Ikeda T. A new classification of alopecia areata. Dermatologica. 1965;131:421-45.–99 Burroway B, Griggs J, Tosti A. Alopecia totalis and universalis long-term outcomes: a review. J Eur Acad Dermatol Venereol. 2020;34:709-15.
In this consensus, an acute episode was considered to be one that lasted up to six months and a chronic episode, one lasting more than six months. It is not known whether rapid treatment of the acute episode decreases the chance of developing chronic disease.88 Cranwell WC, Lai VW, Photiou L, Meah N, Wall D, Rathnayake D, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60:163-70. The presence of signs of activity (Table 4) helps in the therapeutic decision. The time interval between episodes is unpredictable, and they may not even happen again. Permanent maintenance treatment is not recommended to prevent relapse.88 Cranwell WC, Lai VW, Photiou L, Meah N, Wall D, Rathnayake D, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60:163-70.
Complementary exams
The diagnosis of AA is made based on clinical and dermoscopic evaluation, and anatomopathological examination can be performed in doubtful cases. Complementary exams are not mandatory. Depending on the clinical suspicion, blood count, fasting blood glucose, FAN, VDRL, TSH, free T4, anti-TPO, antithyroglobulin, 25-OH vitamin D, vitamin B12, zinc, ferritin, and C-reactive protein may be requested.
Psychosomatic aspects
A proper conversation with the patient with AA starts by discussing their emotional aspects, including triggering factors and chances of hair regrowth. The psychological and social impact of hair goes beyond its biological significance. The negative effects of AA on the social and emotional well-being and on mental health were evidenced by quality of life indexes. To consider AA as mere hair loss does not take into account the negative impact that the disease can have on the patient's life.
A patient’s self-image, interpersonal relationships, and work or school activity can be affected by AA, even in cases with localized disease. More than half of the patients believe that the disease has major consequences in their lives.1010 Firooz A, Firoozabadi MR, Ghazisaidi B, Dowlati Y. Concepts of patients with alopecia areata about their disease. BMC Dermatol. 2005;5:1. Acknowledging the emotional aspects of this “cosmetic” disorder allows comprehensive patient care.1111 Mulinari-Brenner F. Psychosomatic aspects of alopecia areata. Clin Dermatol. 2018;36:709-13.
Psychiatric diagnoses such as depression, anxiety disorder, adjustment disorders, and paranoid disorders have been reported in up to 78% of patients.1212 Schmitt JV, Ribeiro CF, Souza FH, Siqueira EB, Bebber FR. Hair loss perception and symptoms of depression in female outpatients attending a general dermatology clinic. An Bras Dermatol. 2012;87:412-7.,1313 Baghestani S, Zare S, Seddigh SH. Severity of depression and anxiety in patients with Alopecia Areata in Bandar Abbas. Iran. Dermatol Reports. 2015;7:6063. AA is the second leading cause of psychiatric referral by dermatologists, second only to psoriasis.1414 Ocek T, Kani AS, Bas A, Yalcin M, Turan S, Emul M, et al. Psychodermatology: knowledge, awareness, practicing patterns, and attitudes of dermatologists in Turkey. Prim Care Companion CNS Disord. 2015;17, eCollection 2015.
The isolated effectiveness of antidepressants, psychotherapy, relaxation techniques, and individual or group therapy in the treatment of AA has not been evaluated by clinical trials.1111 Mulinari-Brenner F. Psychosomatic aspects of alopecia areata. Clin Dermatol. 2018;36:709-13. Hypnotherapy has demonstrated improvement in hair growth and in the quality of life index in dermatology, with varied responses and high recurrence.1515 Willemsen R, Vanderlinden J, Deconinck A, Roseeuw D. Hypnotherapeutic management of alopecia areata. J Am Acad Dermatol. 2006;55:233-7. More than half of patients with AA believe that their behavior could determine the improvement or worsening of the disease.1010 Firooz A, Firoozabadi MR, Ghazisaidi B, Dowlati Y. Concepts of patients with alopecia areata about their disease. BMC Dermatol. 2005;5:1. To understand and respond to the difficulties that chronic AA can present, patients create their own models of their condition. Information received from various sources, including doctors, family, friends, the internet, and existing social and cultural notions about health and illness shape this model. These beliefs motivate treatment. If the belief system is inadequate, low compliance and treatment abandonment are frequent.1111 Mulinari-Brenner F. Psychosomatic aspects of alopecia areata. Clin Dermatol. 2018;36:709-13.
Support groups can play a crucial role in coping with AA. Group partners help patients find their own identity. Sharing experiences with others with the same disease can be a fundamental link for treatment. Parents should always be the focus of pediatric AA. They can send their children the message that they are not “normal” or “beautiful”. Support groups help parents learn to communicate to their children that they are special and equal to them, with or without hair. Regular meetings of AA patients and family members can be an invaluable resource. In these groups, positive strategies for coping with daily difficulties such as the application of prostheses and uncomfortable situations are shared, in addition to updates on research with a view to the future of the disease. The psychosomatic aspects are summarized in Table 5.
Treatment
One of the essential steps in the treatment of AA is explaining to the patient the nature and course of the disease, as well as the available therapies, to realistically discuss the patient’s expectations.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23. Due to the variable efficacy of treatments and their respective side effects, clinicians play an important role, making the patient more aware of the positive and negative aspects of each option. It should be clear to the patient that none of the therapies has been proven to change the course of the disease in the long term.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23. AA treatment is not mandatory; therefore, the decision must be shared with the patient.11 Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1% by Rochester Epidemiology Project, 1990-2009. J Invest Dermatol. 2014;134:1141-2. Going untreated is a legitimate option for many patients.88 Cranwell WC, Lai VW, Photiou L, Meah N, Wall D, Rathnayake D, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60:163-70. Table 6 summarizes the therapeutic considerations.
Intralesional corticosteroid therapy
This route of administration overcomes the epidermal barrier, making the drug available directly in the inflamed area.1616 MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-9.–1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2. Thus, it minimizes the possible adverse effects of systemic corticosteroid (CT) therapy, with greater drug penetration when compared with the topical route.1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2. Patients with isolated alopecia patches, of small size (<3 cm), short duration, or occupying less than 25% of the scalp are the best candidates for intralesional infiltration.55 Cervantes J, Fertig RM, Maddy A, Tosti A. Alopecia Areata of the Beard: a review of the literature. Am J Clin Dermatol. 2017;18:789-96.,1616 MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-9.,1919 Dainichi T, Kabashima K. Alopecia areata: what’s new in epidemiology, pathogenesis, diagnosis, and therapeutic options?. J Dermatol Sci. 2017;86:3-12. To date, no randomized clinical studies attested the effectiveness of this therapeutic modality.2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202.
Approximately 60%–75% of patients with AA in patches who undergo CT infiltration present hair growth, a rate that varies with the severity of the disease; the perception of the clinical response generally occurs six weeks after the beginning of the treatment.1919 Dainichi T, Kabashima K. Alopecia areata: what’s new in epidemiology, pathogenesis, diagnosis, and therapeutic options?. J Dermatol Sci. 2017;86:3-12.,2121 Kuldeep C, Singhal H, Khare AK, Mittal A, Gupta LK, Garg A. Randomized comparison of topical betamethasone valerate foam, intralesional triamcinolone acetonide and tacrolimus ointment in management of localized alopecia areata. Int J Trichol. 2011;3:20-4.,2222 Spano F, Donovan JC. Alopecia areata: part 2: treatment. Can Fam Physician. 2015;61:757-61. Intralesional corticotherapy can be applied on the scalp, eyebrows, beard, and other affected body areas.55 Cervantes J, Fertig RM, Maddy A, Tosti A. Alopecia Areata of the Beard: a review of the literature. Am J Clin Dermatol. 2017;18:789-96.,1616 MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-9. Although it is an important pillar of AA treatment, there is still no consensus regarding the ideal concentration and total dose of the drug.2323 Hordinsky M, Junqueira AL. Alopecia areata update. Semin Cutan Med Surg. 2015;34:72-5.
Triamcinolone acetonide (TAc) is the most widely used injectable synthetic CT worldwide.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.,2424 Ito T. Advances in the management of alopecia areata. J Dermatol. 2012;39:11-7. In Brazil, TAc is restricted to intraocular use and, therefore, the most widespread form has become triamcinolone hexacetonide (TH), its less soluble derivative and with a higher risk of cutaneous atrophy.1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2. Classically, the concentration of 2.5–10 mg/mL of triamcinolone is used for the scalp and 2.5–5 mg/mL for the face and other body areas.33 Hordinsky M, Donati A. Alopecia areata: an evidence-based treatment update. Am J Clin Dermatol. 2014;15:231-46.,2525 Yee BE, Tong Y, Goldenberg A, Hata T. Efficacy of different concentrations of intralesional triamcinolone acetonide for alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82:1018-21. A pilot study showed that lower concentrations, such as 2.5 mg/mL, were as effective as higher concentrations and with a lower risk of atrophy.2626 Chu TW, AlJasser M, Alharbi A, Abahussein O, McElwee K, Shapiro J. Benefit of different concentrations of intralesional triamcinolone acetonide in alopecia areata: An intrasubject pilot study. J Am Acad Dermatol. 2015;73:338-40. An alternative option to TH for the intralesional treatment of AA is betamethasone (betamethasone dipropionate 5 mg/mL + disodium phosphate betamethasone 2 mg/mL).1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2. A good response has also been reported with hydrocortisone acetate 25 mg/mL.1616 MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-9.
The technique consists on infiltration of 0.05−0.1 mL per puncture into the dermis or upper part of the subcutaneous tissue, with a spacing of 0.5–1 cm between the punctures and an interval of four to six weeks between sessions.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.,88 Cranwell WC, Lai VW, Photiou L, Meah N, Wall D, Rathnayake D, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60:163-70.,2121 Kuldeep C, Singhal H, Khare AK, Mittal A, Gupta LK, Garg A. Randomized comparison of topical betamethasone valerate foam, intralesional triamcinolone acetonide and tacrolimus ointment in management of localized alopecia areata. Int J Trichol. 2011;3:20-4. Dilution with saline or glycoside is recommended, and it may or may not be mixed with lidocaine.1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2. If the anesthetic has methylparaben, propylparaben, or phenol as components of its vehicle, the addition of lidocaine can increase the risk of flocculation of the drug, which can increase the chance of atrophy.1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2.
Pain is a limiting factor, especially in children or patients with extensive forms of AA.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.,2222 Spano F, Donovan JC. Alopecia areata: part 2: treatment. Can Fam Physician. 2015;61:757-61. The use of topical anesthetics, vibration, or local cooling before application can be useful to minimize the discomfort of the procedure.1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2.,2727 Spano F, Donovan JC. Alopecia areata: part 1: pathogenesis, diagnosis, and prognosis. Can Fam Physician. 2015;61:751-5. Needle-free devices are also an option; the device must be sterilized before use.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23. These complementary measures may enable infiltration in children and even in adults who, at first, reject intralesional therapy. Treatment should be suspended if no improvement is observed six months after the beginning of the infiltrations.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.,2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202. Patients who do not respond to glucocorticoids may show resistance due to the low expression of thioredoxin reductase 1 in the external root sheath of the hair follicle.2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202.,2424 Ito T. Advances in the management of alopecia areata. J Dermatol. 2012;39:11-7.
Adverse effects include pain and hemorrhage at puncture sites, headache, reversible local cutaneous atrophy, dyschromia, systemic absorption and, much more rarely, anaphylaxis.88 Cranwell WC, Lai VW, Photiou L, Meah N, Wall D, Rathnayake D, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60:163-70.,1717 Sardesai VR, Prasad S, Agarwal TD. A study to evaluate the efficacy of various topical treatment modalities for alopecia areata. Int J Trichol. 2012;4:265-70. Atrophy is common and can be minimized by applying small volumes of the drug, using more diluted concentrations, increasing the spacing between punctures, and avoiding superficial injections outside the correct drug administration plane.2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202. Increased intraocular pressure and cataracts have already been reported in patients undergoing multiple sessions of intralesional CT therapy for AA in the eyebrow.1616 MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-9. The considerations about intralesional CT therapy are summarized in Table 7.
Topical corticosteroid therapy
Topical CT therapy is widely used in the treatment of all forms of AA, although its clinical efficacy is controversial, due to limited evidence.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23. It is usually used isolated only in limited AA, since its effectiveness is apparently lower in more advanced forms of the disease.1919 Dainichi T, Kabashima K. Alopecia areata: what’s new in epidemiology, pathogenesis, diagnosis, and therapeutic options?. J Dermatol Sci. 2017;86:3-12. However, its use and possible benefits encompass all subtypes of AA, including in association with systemic therapy in extensive cases.
Different topical CTs have already been used in AA, with variable responses.2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202. Comparative studies, however, have shown that very high-potency CTs, such as clobetasol, are significantly more effective than others of lesser potency, such as hydrocortisone.2222 Spano F, Donovan JC. Alopecia areata: part 2: treatment. Can Fam Physician. 2015;61:757-61.,2828 Tosti A, Piraccini BM, Pazzaglia M, Vincenzi C. Clobetasol propionate 0.05% under occlusion in the treatment of alopecia totalis/universalis. J Am Acad Dermatol. 2003;49:96-8. The advantages of this therapeutic modality include the lesser side effects in relation to the systemic route, greater patient compliance, and the possibility of use in several vehicles.33 Hordinsky M, Donati A. Alopecia areata: an evidence-based treatment update. Am J Clin Dermatol. 2014;15:231-46. Clobetasol has already shown a positive result when used as foam, cream, or ointment.33 Hordinsky M, Donati A. Alopecia areata: an evidence-based treatment update. Am J Clin Dermatol. 2014;15:231-46.,2121 Kuldeep C, Singhal H, Khare AK, Mittal A, Gupta LK, Garg A. Randomized comparison of topical betamethasone valerate foam, intralesional triamcinolone acetonide and tacrolimus ointment in management of localized alopecia areata. Int J Trichol. 2011;3:20-4. Its effectiveness appears to increase when applied under occlusion, with promising results even in severe forms of the disease, such as TA and UA, although it can increase the chance of side effects.2121 Kuldeep C, Singhal H, Khare AK, Mittal A, Gupta LK, Garg A. Randomized comparison of topical betamethasone valerate foam, intralesional triamcinolone acetonide and tacrolimus ointment in management of localized alopecia areata. Int J Trichol. 2011;3:20-4.,2424 Ito T. Advances in the management of alopecia areata. J Dermatol. 2012;39:11-7.
The most common adverse effects are folliculitis, local skin atrophy, striae, acneiform rash, telangiectasias, dyschromia, and rarely adrenal suppression.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.,2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202. Washing the site after 12 h of application is recommended to reduce the incidence of folliculitis and fractionizing the dose up to five times a week appears to prevent the onset of atrophy.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23. The recommendations for topical corticotherapy are summarized in Table 8.
Topical calcineurin inhibitors
Preliminary studies in animal models have suggested that tacrolimus may be a promising drug for the treatment of AA in humans. However, tacrolimus 0.1% ointment twice daily for six months was shown to be ineffective in inducing repilation in AA patients.44 Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.,2929 Peloquin L, Castelo-Soccio L. Alopecia Areata: an update on treatment options for children. Paediatr Drugs. 2017;19:411-22. Despite the lack of literature data proving its effectiveness, topical tacrolimus is used almost as often as minoxidil for the treatment of AA, especially in the face region and in children.2929 Peloquin L, Castelo-Soccio L. Alopecia Areata: an update on treatment options for children. Paediatr Drugs. 2017;19:411-22.
Superiority in the efficacy of pimecrolimus cream 1% when compared with placebo was not demonstrated.3030 Rigopoulos D, Gregoriou S, Korfitis C, Gintzou C, Vergou T, Katrinaki A, et al. Lack of response of alopecia areata to pimecrolimus cream. Clin Exp Dermatol. 2007;32:456-7. Similarly to tacrolimus, pimecrolimus does not appear to be a good therapeutic option for AA, especially in patients who are unresponsive to previous therapies. The recommendations on topical immunomodulators are summarized in Table 9.
Topical minoxidil
The mechanism of action through which minoxidil stimulates the hair follicle has not been fully clarified. Vasodilation, angiogenesis, opening of potassium channels, and stimulation of the proliferation of follicular dermal papilla cells are some of the proposed mechanisms.3131 Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol. 2004;150:186-94.,3232 Rossi A, Cantisani C, Melis L, Iorio A, Scali E, Calvieri S. Minoxidil use in dermatology, side effects and recent patents. Recent Pat Inflamm Allergy Drug Discov. 2012;6:130-6. Based on the premise that it can increase the duration of the anagen phase of the hair cycle, the application of minoxidil appears reasonable as soon as the repilation starts, in order to increase the thickness and length of the new hair.
A recent meta-analysis considered minoxidil 5% to be superior to placebo when used in AA in patches. This evidence was classified as having moderate quality.3333 Freire PC, Riera R, Martimbianco AL, Petri V, Atallah AN. Minoxidil for patchy alopecia areata: systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33:1792-9. Concomitant use with topical anthralin or intralesional corticotherapy appears to provide superior results when compared with isolated treatments.2929 Peloquin L, Castelo-Soccio L. Alopecia Areata: an update on treatment options for children. Paediatr Drugs. 2017;19:411-22. Expected side effects are hypertrichosis, contact dermatitis, and pruritus.2020 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202.
Albeit controversial, topical minoxidil has been widely applied in clinical practice as adjuvant therapy in AA. The usual concentration of use in adults is 5%, ranging from one to two daily applications. The recommendations on topical minoxidil are summarized in Table 10.
Topical immunotherapy
Topical immunotherapy (TIT) is performed with agents that trigger allergic contact dermatitis. They are used in the treatment of AA in order to decrease lymphocytic inflammation of the anagen follicle. The mechanism is not well understood, but it is believed to be related to deviation of the inflammatory process from the bulb to the place where the new inflammatory process is being induced by the medication. In this way, the follicle is able to recover.3434 Strazzulla LC, Wang EH, Avila L, Lo Sicco K, Brinster N, Christiano AM, et al. Alopecia areata: an appraisal of new treatment approaches and overview of current therapies. J Am Acad Dermatol. 2018;78:15-24.,3535 Tang L, Sundberg JP, Lui H, Shapiro J. Old wine in new bottles: reviving old therapies for alopecia areata using rodent models. J Investig Dermatol Symp Proc. 2003;8:212-6.
Upon contact with the patient's skin, the sensitizer triggers a delayed hypersensitivity reaction (type IV), originating memory lymphocytes. Thus, after new exposure, the immune system will produce an inflammatory response mediated by T cells.
In Brazil, the sensitizing agent most commonly used is diphencyprone (DPCP), available only at compounding pharmacies. It must be formulated in acetone (highly volatile) and kept in containers protected from light (amber bottle).
After initial exposure to DPCP, the entire immune cascade takes between two to three weeks to elicit memory. Only after this period, the substance will be recognized as an allergen, causing dermatitis.
DPCP is indicated mainly in extensive cases. The rate of satisfactory clinical response can vary between 30%–48%; the rate of any type of response can reach up to 72.2%.3434 Strazzulla LC, Wang EH, Avila L, Lo Sicco K, Brinster N, Christiano AM, et al. Alopecia areata: an appraisal of new treatment approaches and overview of current therapies. J Am Acad Dermatol. 2018;78:15-24.,3636 Kuin RA, Spuls PI, Limpens J, van Zuuren EJ. Diphenylcyclopropenone in patients with alopecia areata. A critically appraised topic. Br J Dermatol. 2015;173:896-909.,3737 Chiang KS, Mesinkovska NA, Piliang MP, Bergfeld WF. Clinical efficacy of Diphenylcyclopropenone in Alopecia Areata: retrospective data analysis of 50 patients. J Investig Dermatol Symp Proc. 2015;17:50-5. The use of this substance is divided into three phases: initial, follow-up, and maintenance. Each phase has its peculiarities, which will be discussed below:
Phase I (initial or sensitizing)
In this phase, 2% DPCP diluted in acetone is used. A small amount is applied with a soaked cotton swab, in an area of 2 × 2 cm. The sensitization process can cause local hypo- or hyperchromia, which is why it is suggested that the application be done in a barely visible area, such as the scalp behind the ear. It is recommended not to expose the area to the sun or wash it for 48 h.
Phase II (follow-up)
Two to three weeks after Phase I, Phase II can begin. In this step, DPCP is applied weekly at low concentration, which is gradually increased. This is the most delicate moment of TIT, since it is necessary to establish the lowest concentration of DPCP that causes an inflammatory process on the skin. The application should not be started with the same concentration as the initial phase, as there is a great chance of an exacerbated inflammation, leading to complications such as blisters.
The medication should be applied to half of the scalp enough to slightly moisten the skin. One end of a soaked cotton swab is enough to spread the medication over one half of the scalp.
Thus, it is suggested to start with low concentrations, to be progressively increased every two weeks: 0.01%, 0.02%, 0.05%, 0.1%, 0.2%, 0.5%, 1%, and 2%. The speed of progression is at the physician's discretion; it can be even slower, using intermediate concentrations between those recommended. The ideal concentration should induce mild to moderate erythema, scaling, itching, and discomfort in the first 48 h after application; meaning that it was strong enough to trigger an inflammatory process. Thus, if the patient does not report any signs/symptoms in two applications, it is possible to increase the concentration in the third session.
After reaching the ideal concentration, treatment should be continued weekly. In cases of lack of response for six months, another treatment can be attempted. However, some authors report the need to persist with treatment up to 12–24 months to observe hair regrowth.3737 Chiang KS, Mesinkovska NA, Piliang MP, Bergfeld WF. Clinical efficacy of Diphenylcyclopropenone in Alopecia Areata: retrospective data analysis of 50 patients. J Investig Dermatol Symp Proc. 2015;17:50-5. In case of hair regrowth, treatment must be maintained until acceptable cosmetic coverage is reached and no signs of activity are observed.
Phase III (weaning/maintenance)
After cosmetic hair regrowth, it is suggested to reduce the frequency of applications to biweekly, followed by monthly and, finally, suspension. In cases of disease recurrence after the medication is discontinued, fortnightly or monthly treatment maintenance should be considered.
The most frequent complications are hyperpigmentation, hypopigmentation, intense eczema, blisters, lymph node enlargement, folliculitis, and flu-like symptoms.3636 Kuin RA, Spuls PI, Limpens J, van Zuuren EJ. Diphenylcyclopropenone in patients with alopecia areata. A critically appraised topic. Br J Dermatol. 2015;173:896-909. TIT recommendations are summarized in Table 11.
Anthralin
The use of anthralin also aims to divert the inflammatory process away from the bulb, but it causes irritative contact dermatitis, rather than the allergic form. In Brazil, anthralin is only available in compounding pharmacies. Its concentration can vary from 0.5% to 2.0% in lanette cream or solution.
Its use in children is justified by the lack of systemic side effects. Hair regrowth is observed in 71% of the cases of alopecia in patches.3838 Wu SZ, Wang S, Ratnaparkhi R, Bergfeld WF. Treatment of pediatric alopecia areata with anthralin: a retrospective study of 37 patients. Pediatr Dermatol. 2018;35:817-20. The mean time to initial response is three months, and a complete response is observed in 15 months.3838 Wu SZ, Wang S, Ratnaparkhi R, Bergfeld WF. Treatment of pediatric alopecia areata with anthralin: a retrospective study of 37 patients. Pediatr Dermatol. 2018;35:817-20.
The drug is applied to the affected area, extending up to 1 cm into the apparently healthy area. The patient is instructed to wash the area and thoroughly remove the product after 30 min. The procedure is repeated daily. Every three days, the time of contact with the skin is increased by 15 min. That is, the initial time is 30 min, then increased to 45 min, 60 min, 75 min, and so on until the maximum time of two hours is reached. The goal is to cause mild eczema. When there is no reaction after two hours, the contact time can be extended, in some cases, to overnight.
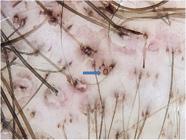
Anthralin is a dark brown substance with a characteristic odor. With frequent applications, it ends up pigmenting the follicular ostia, simulating black dots. However, on dermoscopy, the difference between a black dot in the center of the ostium and the regularly distributed brown pigmentation on the edge of the follicular ostium by anthralin is clear (Fig. 1). One of the signs of therapeutic failure is evidenced by the lack of pigmentation of the ostia, which can have three main causes: irregular application, short contact time with the scalp, or low quality medication.
Brown pigmentation at the edge of the follicular ostium by anthralin (blue arrow); differentiate from the black dots that are in the center of the ostium.
This is a safe therapy, but care must be taken to avoid complications. As the goal is to cause local irritation, the increase in the time of contact of the medication with the skin must be systematic, avoiding an exacerbated irritation.
The use of anthralin leads to hyperpigmentation of the treated area, but the color will return to normal after treatment discontinuation. The recommendations on anthralin are summarized in Table 12.
Systemic corticosteroids
Several forms of systemic administration of CTs have been described for the treatment of AA. A 200 mg oral prednisolone pulse once a week for three months presented a response rate of 40% in patients with more than 40% of the affected scalp or more than ten patches on the scalp or body.3939 Kar BR, Handa S, Dogra S, Kumar B. Placebo-controlled oral pulse prednisolone therapy in alopecia areata. J Am Acad Dermatol. 2005;52:287-90. Other regimens include prednisolone 80 mg/day for three consecutive days every three months and for patients resistant to other therapeutic modalities, a megapulse of 15 mg/kg for two days every three weeks.4040 Kurosawa M, Nakagawa S, Mizuashi M, Sasaki Y, Kawamura M, Saito M, et al. A comparison of the efficacy, relapse rate and side effects among three modalities of systemic corticosteroid therapy for alopecia areata. Dermatology. 2006;212:361-5.,4141 Bin Saif GA, Al-Khawajah MM, Al-Otaibi HM, Al-Roujayee AS, Alzolibani AA, Kalantan HA, et al. Efficacy and safety of oral mega pulse methylprednisolone for severe therapy resistant Alopecia areata. Saudi Med J. 2012;33:284-91.
There is no consensus in the literature on the dose and duration of daily oral corticotherapy use in AA. Prednisone can be used in doses ranging from 0.1 to 1 mg/kg/day. It is suggested to start with higher doses (0.5–1 mg/kg/day), with a gradual reduction (over 6–12 weeks) after hair regrowth is achieved.
Although not described in guidelines for AA and presenting a higher cost, this consensus considers deflazacort to be the best option for oral CT, due to its more favorable safety profile. The drug has a high therapeutic index, with potency ranging between 70%−90% of prednisone, with a lower impact on calcium metabolism when compared with any other synthetic CT. In addition, it has comparatively little effect on carbohydrate metabolism, water retention, and hypokalemia.4242 Parente L. Deflazacort: therapeutic index, relative potency and equivalent doses versus other corticosteroids. BMC Pharmacol Toxicol. 2017;18:1. It is suggested to start with a daily dose of 0.5 mg/kg for both adults and children, with a slow reduction after hair regrowth.
Long-term CTs can be administered intramuscularly or intravenously as an alternative to oral use. In a comparative randomized clinical trial, the application of 40 mg of intramuscular TAc once a month for six months was superior to pulsed prednisolone (80 mg for three consecutive days every three months) and to dexamethasone (0.5 mg/day for six months).4040 Kurosawa M, Nakagawa S, Mizuashi M, Sasaki Y, Kawamura M, Saito M, et al. A comparison of the efficacy, relapse rate and side effects among three modalities of systemic corticosteroid therapy for alopecia areata. Dermatology. 2006;212:361-5.
Similarly to the intralesional use, TAc is recommended over TH for intramuscular use, due to the greater risk of developing atrophy and telangiectasias in the long term.4343 Pirmez R, Abraham LS, Duque-Estrada B, Damasco P, Farias DC, Kelly Y, et al. Trichoscopy of steroid-induced atrophy. Skin Appendage Disord. 2017;3:171-4. The authors suggest, as a second option, the substitution by the combination of betamethasone dipropionate 5 mg/mL (fast action) with disodium phosphate betamethasone 2 mg/mL (prolonged action).1818 Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2. Table 13 presents the dose equivalence of the different CTs.4444 Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: a review of glucocorticoid pharmacology and bone health. J Am Acad Dermatol. 2017;76:1-9.
The response rates with systemic CT are high, but many patients experience relapses with dose reduction or shortly after medication withdrawal. For patients who respond to CT, but who become steroid dependent, the combination of another systemic medication can be useful to spare the use of CT.
For all types of long-term CT therapy, it is important to classify and monitor the patient for the risk of side effects, in addition to providing information about interactions and vaccination.4444 Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: a review of glucocorticoid pharmacology and bone health. J Am Acad Dermatol. 2017;76:1-9.–4747 Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoidinduced side effects: a comprehensive review: ocular, cardiovascular, muscular, and psychiatric side effects and issues unique to pediatric patients. J Am Acad Dermatol. 2017;76:201-7. The recommendations on systemic CT are summarized in Table 14.
Immunosuppressants
Methotrexate (MTX)
MTX is a competitive chemotherapeutic inhibitor of dihydrofolate reductase. Its use in low doses in inflammatory diseases such as AA requires folic acid supplementation. Among the independent pathways, suppression of the JAK/STAT signaling pathway appears to be the main mechanism of action.4848 Thomas S, Fisher KH, Snowden JA, Danson SJ, Brown S, Zeidler MP. Methotrexate is a JAK/STAT pathway inhibitor. PLoS One. 2015;10:e0130078.
Initial doses of 5–10 mg/week are progressively increased over four to six weeks, reaching up to 20–25 mg. As oral MTX in doses above 15 mg may present erratic absorption, the injectable option should be considered in these cases. Combination with oral and intralesional CT have been reported. In most cases, a minimum dose of MTX, ranging from 7.5 to 12.5 mg/week, is required for maintenance.4949 Anuset D, Perceau G, Bernard P, Reguiai Z. Efficacy and safety of methotrexate combined with low-to moderate-dose corticosteroids for severe Alopecia Areata. Dermatology. 2016;232:242-8.,5050 Hammerschmidt M, Mulinari Brenner F. Efficacy and safety of methotrexate in alopecia areata. An Bras Dermatol. 2014;89:729-34.
Better responses are observed in men, patients over 40 years old, those with less than five years of illness, those who reached cumulative doses of 1000−1500 mg, and those who received CT in addition to MTX.5050 Hammerschmidt M, Mulinari Brenner F. Efficacy and safety of methotrexate in alopecia areata. An Bras Dermatol. 2014;89:729-34.,5151 Phan K, Ramachandran V, Sebaratnam DF. Methotrexate for alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80, 120-7.e2. Recurrence can happen during treatment and after discontinuation of medication. Prolonged use is necessary.
MTX in conjunction with low doses of prednisone showed hair regrowth of terminal hairs in up to 96% of patients with AA.4949 Anuset D, Perceau G, Bernard P, Reguiai Z. Efficacy and safety of methotrexate combined with low-to moderate-dose corticosteroids for severe Alopecia Areata. Dermatology. 2016;232:242-8. Total hair regrowth has been demonstrated in 15%–64% of patients.5151 Phan K, Ramachandran V, Sebaratnam DF. Methotrexate for alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80, 120-7.e2.
Pancytopenia is the most common toxicity when using low-dose MTX. Patients with renal failure, hypoalbuminemia, those who use erroneously high doses, and those who use other drugs that interact with MTX (e.g., anti-inflammatory drugs) are at increased risk.5252 Kivity S, Zafrir Y, Loebstein R, Pauzner R, Mouallem M, Mayan H. Clinical characteristics and risk factors for low dose methotrexate toxicity: a cohort of 28 patients. Autoimmun Rev. 2014;13:1109-13.,5353 Shen S, O’Brien T, Yap LM, Prince HM, McCormack CJ. The use of methotrexate in dermatology: a review. Australas J Dermatol. 2012;53:1-18. Interstitial pneumonitis and abnormal liver function have been reported.5151 Phan K, Ramachandran V, Sebaratnam DF. Methotrexate for alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80, 120-7.e2. Folic acid supplementation reduces the side effects of MTX, especially gastrointestinal ones. Various doses and frequencies of administration have been described, ranging from 5 mg per week to 1–5 mg/day. Even in daily doses, folic acid does not interfere with the effectiveness of MTX.5454 Cline A, Jorizzo JL. Does daily folic acid supplementation reduce methotrexate efficacy?. Dermatol Online J. 2017;23,13030/qt4hf5v2vk. Folinic acid supplementation is reserved for cases of toxicity by the drug.5454 Cline A, Jorizzo JL. Does daily folic acid supplementation reduce methotrexate efficacy?. Dermatol Online J. 2017;23,13030/qt4hf5v2vk.
Cyclosporine
Cyclosporine is an immunosuppressive agent capable of inhibiting the activation of auxiliary T cell and suppressing the production of gamma interferon, reducing the perifollicular inflammatory infiltrate. The high recurrence and high incidence of long-term side effects limit its use. This is the only immunosuppressant for which a controlled, double-blinded, randomized study demonstrated a response in AA.5555 Lai VWY, Chen G, Gin D, Sinclair R. Cyclosporine for moderate-to-severe alopecia areata: a double-blind, randomized, placebo-controlled clinical trial of efficacy and safety. J Am Acad Dermatol. 2019;81:694-701.
A daily dose of 2 mg/kg/day, divided into three intakes, is used initially, with a progressive increase of up to 5 mg/kg/day.5656 Jang YH, Kim SL, Lee KC, Kim MJ, Park KH, Lee WJ, et al. A Comparative study of oral cyclosporine and betamethasone minipulse therapy in the treatment of Alopecia Areata. Ann Dermatol. 2016;28:569-74. Regrowth ranges from 25% to 76.6% when associated with systemic and intralesional CT.5656 Jang YH, Kim SL, Lee KC, Kim MJ, Park KH, Lee WJ, et al. A Comparative study of oral cyclosporine and betamethasone minipulse therapy in the treatment of Alopecia Areata. Ann Dermatol. 2016;28:569-74.,5757 Miteva M, Tosti A. Treatment options for alopecia: an update, looking to the future. Expert Opin Pharmacother. 2012;13:1271-81.
Its use is limited by the high recurrence rates after withdrawal and by its side effects, especially nephrotoxicity, immunosuppression, and arterial hypertension. The reported nephrotoxicity, usually due to prerenal vasoconstriction, was reversible in patients with AA.5656 Jang YH, Kim SL, Lee KC, Kim MJ, Park KH, Lee WJ, et al. A Comparative study of oral cyclosporine and betamethasone minipulse therapy in the treatment of Alopecia Areata. Ann Dermatol. 2016;28:569-74.,5757 Miteva M, Tosti A. Treatment options for alopecia: an update, looking to the future. Expert Opin Pharmacother. 2012;13:1271-81.
Azathioprine
Azathioprine is an antimetabolite with few reports of use in AA. Initial doses of 0.5–1 mg/kg/day can be increased up to 2–3 mg/kg/day, according to the patient's tolerance.5858 Vañó-Galván S, Hermosa-Gelbard Á, Sánchez-Neila N, Miguel-Gómez L, Saceda-Corralo D, Rodrigues-Barata R, et al. Treatment of recalcitrant adult alopecia areata universalis with oral azathioprine. J Am Acad Dermatol. 2016;74:1007-8. A dose of 2.5 mg/kg/day can be considered for recalcitrant AA. In 43% of patients, some hair regrowth was observed after four to six months.5858 Vañó-Galván S, Hermosa-Gelbard Á, Sánchez-Neila N, Miguel-Gómez L, Saceda-Corralo D, Rodrigues-Barata R, et al. Treatment of recalcitrant adult alopecia areata universalis with oral azathioprine. J Am Acad Dermatol. 2016;74:1007-8. Gastrointestinal symptoms, elevated liver enzymes, pancreatitis, and bone marrow suppression are the most common side effects.
Better responses can be observed in association with systemic/injectable CT or even MTX. The association with MTX should be carried out carefully, considering the increase in side effects.5959 Mascia P, Milpied B, Darrigade AS, Seneschal J, Eyraud A, Bonamonte D, et al. Azathioprine in combination with methotrexate: a therapeutic alternative in severe and recalcitrant forms of alopecia areata?. J Eur Acad Dermatol Venereol. 2019;33, e494-e5. The recommendations on immunosuppressants are summarized in Table 15.
Janus kinase (JAK) inhibitors
Currently, the pathophysiology of AA is considered to be based on CD8+ cytotoxic T cells that express NKG2D. These lymphocytes are responsible for initiating and maintaining the autoimmune inflammation process against the hair follicle and are activated and perpetuated by IFN-γ and IL-15, which in turn use the JAK-STAT signaling pathway.6060 Xing L, Dai Z, Jabbari A, Cerise JE, Higgins CA, Gong W, et al. Alopecia areata is driven by cytotoxic Tlymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20:1043-9.
JAK inhibitors are small molecule drugs approved for use in myelofibrosis, polycythemia vera, essential thrombocytosis, and rheumatoid and psoriatic arthritis, and have been studied in patients with AA refractory to other treatments.
Ruxolitinib, a JAK1 and JAK2 inhibitor, was investigated in 12 patients with moderate to severe AA (mean SALT: 65.6) at a dose of 20 mg twice daily for three to six months of treatment, and followed-up for three months after drug withdrawal. Nine of the 12 patients (75%) showed improvement, with an average hair regrowth of 92%, without serious adverse effects. Three months after the end of treatment, all patients had recurrence of hair loss.6161 Mackay-Wiggan J, Jabbari A, Nguyen N, Cerise JE, Clark C, Ulerio G, et al. Oral ruxolitinib induces hair regrowth in patients with moderate-to-severe alopecia areata. JCI Insight. 2016;1:e89790. Other case reports have also been published.6262 de Oliveira AB, Alpalhão M, Filipe P, Maia-Silva J. The role of Janus kinase inhibitors in the treatment of alopecia areata: a systematic review. Dermatol Ther. 2019;32:e13053.
Tofacitinib inhibits JAK1/2 and more intensily, JAK3. It is the JAK inhibitor with the most cases published in the literature in various treatment regimens, such as 5 mg twice a day, increasing the dose to 10 mg twice a day and, if there is no response, association with prednisone 300 mg once a month.6363 Liu LY, Craiglow BG, Dai F, King BA. Tofacitinib for the treatment of severe alopecia areata and variants: a study of 90 patients. J Am Acad Dermatol. 2017;76:22-8.–6565 Jabbari A, Sansaricq F, Cerise J, Chen JC, Bitterman A, Ulerio G, et al. An Open-label pilot study to evaluate the efficacy of tofacitinib in moderate to severe patch-type Alopecia Areata, Totalis, and Universalis. J Invest Dermatol. 2018;138:1539-45. A recent meta-analysis included 14 studies, six clinical trials, and eight observational studies, with 275 patients. The rate of acceptable or complete repilation was 54% (95% CI: 46.3%−61.5%), and the partial response rate was 26.1% (95% CI: 20.7%−32.2%). During follow-up, approximately one-quarter of the patients presented recurrence after discontinuation.6666 Guo L, Feng S, Sun B, Jiang X, Liu Y. Benefit and risk profile of tofacitinib for the treatment of alopecia areata: a systemic review and meta-analysis. J Eur Acad Dermatol Venereol. 2020;34:192-201.
In general, the response to treatment with JAK inhibitors did not correlate with demographic characteristics, disease severity, and duration of AA, and there are no predictors of response to date.6767 Phan K, Sebaratnam DF. JAK inhibitors for alopecia areata: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33:850-6. The most common complications are mild infections, mainly of the upper respiratory tract and urinary tract. Dyslipidemia, leukopenia, increased liver enzymes, headache, gastrointestinal complaints, fatigue, acne, and weight gain have also been reported. To date, there are no reports of neoplasms, reactivation of tuberculosis, or hospitalization due to adverse events. Long-term safety data is still limited.6767 Phan K, Sebaratnam DF. JAK inhibitors for alopecia areata: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33:850-6.
Topical JAK inhibitors are not yet available in standard formulations; the reports in the literature are based on compounded presentations, with variable results, and are currently not recommended.6767 Phan K, Sebaratnam DF. JAK inhibitors for alopecia areata: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33:850-6.
Treatment with JAK inhibitors is still based on low-quality evidence, predominantly case reports, retrospective studies, and non-blinded and non-placebo-controlled clinical trials. The development of potentially more selective JAK inhibitors and the optimization of topical formulations are promising. Recommendations regarding the use of JAK inhibitors are summarized in Table 16; Table 17 lists the pre-treatment evaluation.
Other treatments
The treatments mentioned below have little evidence of results and should only be considered in the absence of response to standard therapies.
Hydroxychloroquine
An antimalarial with anti-inflammatory action and immunomodulatory effect. Studies on hydroxychloroquine in AA are controversial.6868 Nissen CV, Wulf HC. Hydroxychloroquine is ineffective in treatment of alopecia totalis and extensive alopecia areata: a case series of 8 patients. JAAD Case Rep. 2016;2:117-8.,6969 Yun D, Silverberg NB, Stein SL. Alopecia areata treated with hydroxychloroquine: a retrospective study of nine pediatric cases. Pediatr Dermatol. 2018;35:361-5. When used, the recommended dose is 5 mg/kg/day; in case of prolonged use of the drug, special attention should be paid to ocular toxicity. Gastrointestinal intolerance and headache are the most commonly reported side effects. Hydroxychloroquine is not recommended for the treatment of AA.
Zinc
A randomized study including patients with AA in patches, double-blinded with cross-over of patients using zinc sulfate at a dose of 5 mg/kg/day, divided into three doses, demonstrated the superiority of zinc over placebo.7070 Sharquie KE, Noaimi AA, Shwail ER. Oral zinc sulphate in treatment of alopecia areata (double blind; crossover study). J Clin Exp Dermatol Res. 2012;3:2-5. In another placebo-controlled study, including patients with TA and UA, no improvement was observed when comparing the treatment group with the control group.7171 Ead RD. Oral zinc sulphate in alopacia areata—a double blind trial. Br J Dermatol. 1981;104:483-4. The authors consider that zinc sulfate could be used in less severe cases and, preferably, associated with other therapies. It can be used even if the patient presents normal serum zinc levels.
Sulfasalazine/mesalazine
Sulfasalazine is a prodrug composed of 5-aminosalicylic acid (5-ASA) associated with sulfapyridine. While 5-ASA is responsible for the efficacy of sulfasalazine, sulfapyridine accounts for most of the side effects: headache, anorexia, nausea, and vomiting, which occur in 10%−45% of patients. Mesalazine contains only slow-release 5-ASA; for this reason, it is usually better tolerated than sulfasalazine. 5-ASA works both as an immunomodulator and immunosuppressant and is used in several autoimmune conditions such as ulcerative colitis, Crohn’s disease, and psoriasis. An uncontrolled open study demonstrated rates of hair regrowth with sulfasalazine (1.5 g 2 ×/day) between 25% and 68% in patients with refractory AA, alone or in combination with CT therapy, acting as a CT-sparing agent. However, the side effect profile remains a limiting factor.7272 Bakar O, Gurbuz O. Is there a role for sulfasalazine in the treatment of alopecia areata?. J Am Acad Dermatol. 2007;57:703-6. Recently, hair regrowth was reported with the use of mesalazine (15−30 mg/kg/day in two daily doses) associated or unassociated with topical oral CT or minoxidil/betamethasone in the treatment of five children and adolescents (2–17 years) with refractory and severe AA.7373 Kiszewski AE, Bevilaqua M, De Abreu LB. Mesalazine in the treatment of extensive alopecia areata: a new therapeutic option?. Int J Trichology. 2018;10:99-102. Follow-up with G6PD, blood count, biochemistry, and hepatogram assessment are essential to monitor possible adverse effects.
Simvastatin/ezetimibe
Data on the efficacy of the combination of simvastatin 40 mg/ezetimibe 10 mg, 1 ×/day in the treatment of AA are limited and controversial.7474 Lattouf C, Jimenez JJ, Tosti A, Miteva M, Wikramanayake TC, Kittles C, et al. Treatment of alopecia areata with simvastatin/ezetimibe. J Am Acad Dermatol. 2015;72:359-61.–7777 Cervantes J, Jimenez JJ, DelCanto GM, Tosti A. Treatment of Alopecia Areata with Simvastatin/Ezetimibe. J Investig Dermatol Symp Proc. 2018;19:S25-31. Positive reports show hair regrowth rates and lower relapse in patients with recent onset and good prognosis for AA.7474 Lattouf C, Jimenez JJ, Tosti A, Miteva M, Wikramanayake TC, Kittles C, et al. Treatment of alopecia areata with simvastatin/ezetimibe. J Am Acad Dermatol. 2015;72:359-61.,7575 Choi JW, Suh DW, Lew BL, Sim WY. Simvastatin/ezetimibe therapy for recalcitrant alopecia areata: an open prospective study of 14 patients. Ann Dermatol. 2017;29:755-60.
Oral minoxidil
The first report of the use of oral minoxidil in AA was in 1987, in monotherapy at a dose of 5 mg, twice a day, in 65 patients, including men and women. Satisfactory repilation was observed in 18% of patients.7878 Fiedler-Weiss VC, Rumsfield J, Buys CM, West DP, Wendrow A. Evaluation of oral minoxidil in the treatment of alopecia areata. Arch Dermatol. 1987;123:1488-90. Despite the high dose, facial hypertrichosis was observed in only 17% of patients. Recently, the combination of minoxidil (2.5 mg/day for women and 2.5 mg twice a day for men) and tofacitinib (5 mg twice a day) has been shown to be positive, with a low incidence of side effects.7979 Wambier CG, Craiglow BG, King BA. Combination tofacitinib and oral minoxidil treatment for severe alopecia areata. J Am Acad Dermatol. 2019, pii: S0190-9622(19)32688-X.
Excimer laser/light
The most studied light-based therapies in AA are the excimer laser and excimer light at 308 nm, which have immunosuppressive properties, possibly by inducing T-cell apoptosis. A recent review included eight clinical studies and case reports, with a total of 94 treated individuals, with an efficiency of 36.9%−100%, and hair regrowth equal to or greater than 50%.8080 Darwin E, Arora H, Hirt PA, Wikramanayake TC, Jimenez JJ. A review of monochromatic light devices for the treatment of alopecia areata. Lasers Med Sci. 2018;33:435-44. A meta-analysis that included only four controlled studies, using excimer laser on AA patches not previously treated, confirmed the effectiveness of the treatment.8181 Gupta AK, Carviel JL. Meta-analysis of 308-nm excimer laser therapy for alopecia areata. J Dermatolog Treat. 2019;:1-4. The main side effects of the therapy are mild erythema, pain during application, hyperpigmentation, blistering, pruritus, and peeling.8282 Mlacker S, Aldahan AS, Simmons BJ, Shah V, McNamara CA, Samarkandy S, et al. A review on laser and light-based therapies for alopecia areata. J Cosmet Laser Ther. 2017;19:93-9. The high cost is the main disadvantage of the treatment. Excimer laser and excimer light can be alternatives for refractory cases, especially when there is CT-induced atrophy or contact dermatitis by other therapies.
PUVA
Photochemotherapy with psoralen and ultraviolet A radiation (PUVA) has been investigated in several therapeutic schemes in studies from the 1980s to 1990s, with different efficacy rates. Due to the chronic and recurrent nature of AA, this therapeutic modality is not recommended due to the risk of large cumulative doses of UVA in the long term, with the possibility of cutaneous malignancy as an adverse effect. More recently, there has been interest in treatment with UVA-1, which has greater penetration into the skin and possibly greater effectiveness and may be an alternative in the treatment of AA.8383 Herz-Ruelas ME, Gomez-Flores M, Miranda-Maldonado I, Welsh E, Ocampo-Candiani J, Welsh O. Escalating dosimetry of UVA-1 in the treatment of alopecia areata. Int J Dermatol. 2017;56:653-9.
Dapsone
Due to its low efficacy and its side effect profile, there is no justification for the use of dapsone in AA.8484 van Baar HM, van der Vleuten CJ, van de Kerkhof PC. Dapsone versus topical immunotherapy in alopecia areata. Br J Dermatol. 1995;133:270-4.,8585 Friedmann PS. Unsuccessful treatment of alopecia areata with dapsone. Br J Dermatol. 1981;104:597-8.
Platelet-rich plasma (PRP) and microneedling
Small clinical trials have suggested a potential benefit of PRP and microneedling in AA, but the real benefit of these techniques has not yet been established.8686 Hesseler MJ, Shyam N. Platelet-rich plasma and its utilities in alopecia: a systematic review. Dermatol Surg. 2020;46:93-102.,8787 Strazzulla LC, Avila L, Lo Sicco K, Shapiro J. An overview of the biology of platelet-rich plasma and microneedling as potential treatments for alopecia areata. J Investg Dermatol. 2018;19.S21-S4. The use of these modalities for the treatment of AA is not recommended. To date, the use of PRP for dermatological purposes is prohibited by the Brazilian Federal Council of Medicine.
Prostheses and camouflages
Cosmetic disguise options should be encouraged. Although few studies have quantified the benefit in the patients' quality of life, the suggestion of these resources is considered good practice.8888 Park J, Kim DW, Park SK, Yun SK, Kim HU. Role of hair prostheses (wigs) in patients with severe alopecia areata. Ann Dermatol. 2018;30:505-7.,8989 Inui S, Inoue T, Itami S. Psychosocial impact of wigs or hairpieces on perceived quality of life level in female patients with alopecia areata. J Dermatol. 2013;40:225-6. There are numerous options for partial or total hair prostheses, and removable or fixed extensions. Camouflages can take the form of hair fibers, sprays, waxes, and pigmented powders. Trichopigmentation can be performed on the scalp and eyebrow area. Eyelashes, false nails, and eyebrow prostheses can also be used.
Treatment in special situations
AA in children
The management of AA cases in children could even be considered an ordinary situation, as it is a common cause of hair loss in childhood and adolescence—up to 60% of cases start in the first two decades of life.9090 Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part I. Clinical picture, histopathology, and pathogenesis. J Am Acad Dermatol. 2010;62:177-88.
In children, topical CT is used as the first therapeutic option, preferably of medium to high potency (mometasone 1% to clobetasol 0.05%). When there is contraindication or lack of response to topical CT, anthralin, DPCP, or minoxidil may be used, or an expectant treatment may be chosen.3838 Wu SZ, Wang S, Ratnaparkhi R, Bergfeld WF. Treatment of pediatric alopecia areata with anthralin: a retrospective study of 37 patients. Pediatr Dermatol. 2018;35:817-20.,9191 Salsberg JM, Donovan J. The safety and efficacy of diphencyprone for the treatment of alopecia areata in children. Arch Dermatol. 2012;148:1084-5.
The administration of systemic drugs can be considered in extensive cases or in cases with extensive disease activity. One should always take into account the child's life stage and degree of development. It is important to pay attention to possible adverse effects, especially changes in growth, and in metabolic and immune competence. Among the options available, there is a preference for systemic CT and MTX. Table 18 presents the main recommendations for the treatment of AA in children.
AA in the beard area
The beard is the second most frequently affected area by AA, second only to the scalp.55 Cervantes J, Fertig RM, Maddy A, Tosti A. Alopecia Areata of the Beard: a review of the literature. Am J Clin Dermatol. 2017;18:789-96. There are no controlled and randomized clinical trials evaluating treatment in this region. The most frequent approach is the use of local therapies, starting with topical CT followed by intralesional CT, or starting directly with the use of intralesional CT, a treatment that has the greatest evidence of efficacy for localized and short-term AA.9292 Saceda-Corralo D, Grimalt R, Fernández-Crehuet P, Clemente A, Bernárdez C, Garcia-Hernandez MJ, et al. Beard alopecia areata: a multicentre review of 55 patients. J Eur Acad Dermatol Venereol. 2017;31:187-92.,9393 Kassim JM, Shipman AR, Szczecinska W, Siah TW, Lam M, Chalmers J, et al. How effective is intralesional injection of triamcinolone acetonide compared with topical treatments in inducing and maintaining hair growth in patients with alopecia areata? A critically appraised topic. Br J Dermatol. 2014;170:766-71. Triamcinolone concentration of 2.5 mg/mL is the most suitable for the treatment of the face. Other treatments described for the region include topical minoxidil, immunotherapy, photodynamic therapy, 1550 nm fractional erbium glass laser, PUVA, or narrow-band UVB phototherapy. Recommendations for treating the beard area are summarized in Table 19.
AA on eyebrows and eyelashes
The involvement of the eyebrows and eyelashes has a great impact on the quality of life, as it directly interferes with the facial appearance. The only agents indicated for hypotrichosis or alopecia in the eyelash region, regardless of their etiology, are prostaglandin analogues, especially the 0.03% bimatoprost solution.9494 Barrón-Hernández YL, Tosti A. Bimatoprost for the treatment of eyelash, eyebrow and scalp alopecia. Expert Opin Investig Drugs. 2017;26:515-22.,9595 Vila TO, Camacho Martinez FM. Bimatoprost in the treatment of eyelash universalis alopecia areata. Int J Trichology. 2010;2:86-8. Some studies have assessed the drug in adult and pediatric patients, with variable results, which is probably due to conditions with different severities and, therefore, different AA prognoses.9696 Borchert M, Bruce S, Wirta D, Yoelin SG, Lee S, Mao C, et al. An evaluation of the safety and efficacy of bimatoprost for eyelash growth in pediatric subjects. Clin Ophthalmol. 2016;10:419-29. It appears to be a safe and potentially effective agent for treating the region. It is important to note the risk of eyelid hyperpigmentation and darkening of the iris.
In the eyebrows, in addition to the possibility of using 0.03% bimatoprost, there is the option of topical and intralesional CT.9494 Barrón-Hernández YL, Tosti A. Bimatoprost for the treatment of eyelash, eyebrow and scalp alopecia. Expert Opin Investig Drugs. 2017;26:515-22. Preferably, a medium-potency CT should be used, and care should be taken to prevent the drug from running into the eyelids and eyes (cream vehicle, instead of solution). Intralesional infiltration of triamcinolone should be done at a dose of 2.5 mg/mL to minimize the risk of cutaneous atrophy. Topical minoxidil is also an option, similarly to the scalp. Recommendations for the treatment of eyelashes and eyebrows are summarized in Table 20.
Follow-up
The interval between follow-up appointments will depend on the treatment regimen chosen for each patient. Those treated with DPCP will require weekly or fortnightly visits; those submitted to intralesional infiltrations should be followed-up every four to six weeks. Patients undergoing topical home treatment can be assessed every two to three months, whereas those receiving systemic treatments will have intervals depending on the chosen drug and on the patient's health conditions. At the initial consultation and at least quarterly, standardized clinical photos documenting different regions of the scalp (top, sides, occipital region) should be taken. Dermoscopic photos of the areas of alopecia are recommended. The classification in one of the methods described for estimation of extension (SALT score, SALT II, ALODEX, Alopecia Areata Progressive Index) and assessment of nail involvement and the involvement of body hair must be included in the patient's medical record. Other instruments, such as quality of life questionnaires, can be adapted for use in AA.9797 Olsen EA, Roberts J, Sperling L, Tosti A, Shapiro J, McMichael A, et al. Objective outcome measures: collecting meaningful data on alopecia areata. J Am Acad Dermatol. 2018;79, 470-8.e3.
Final considerations
The treatment of AA is complex, and few comparative studies show confirmatory evidence. This consensus aimed to provide basic guidance for the management of AA in daily practice with a focus on the Brazilian reality. The recommendations presented herein are summarized in Fig. 2.
-
☆
How to cite this article: Ramos PM, Anzai A, Duque-Estrada B, Melo DF, Sternberg F, Santos LDN, et al. Consensus on the treatment of alopecia areata – Brazilian Society of Dermatology. An Bras Dermatol. 2020;95(S1):39–52.
-
☆☆
Study conducted at the Brazilian Society of Dermatology, Rio de Janeiro, RJ, Brazil.
-
Financial supportNone declared.
References
-
1Mirzoyev SA, Schrum AG, Davis MDP, Torgerson RR. Lifetime incidence risk of alopecia areata estimated at 2.1% by Rochester Epidemiology Project, 1990-2009. J Invest Dermatol. 2014;134:1141-2.
-
2Sociedade Brasileira de Dermatologia, Miot HA, Penna GO,Ramos AMC, Penna ML, Schmidt SM, et al. Profile of dermatological consultations in Brazil (2018). An Bras Dermatol. 2018;93:916-28.
-
3Hordinsky M, Donati A. Alopecia areata: an evidence-based treatment update. Am J Clin Dermatol. 2014;15:231-46.
-
4Rossi A, Muscianese M, Piraccini BM, Starace M, Carlesimo M, Mandel VD, et al. Italian Guidelines in diagnosis and treatment of alopecia areata. G Ital Dermatol Venereol. 2019;154:609-23.
-
5Cervantes J, Fertig RM, Maddy A, Tosti A. Alopecia Areata of the Beard: a review of the literature. Am J Clin Dermatol. 2017;18:789-96.
-
6Sato-Kawamura M, Aiba S, Tagami H. Acute diffuse and total alopecia of the female scalp. A new subtype of diffuse alopecia areata that has a favorable prognosis. Dermatology. 2002;205:367-73.
-
7Ikeda T. A new classification of alopecia areata. Dermatologica. 1965;131:421-45.
-
8Cranwell WC, Lai VW, Photiou L, Meah N, Wall D, Rathnayake D, et al. Treatment of alopecia areata: an Australian expert consensus statement. Australas J Dermatol. 2019;60:163-70.
-
9Burroway B, Griggs J, Tosti A. Alopecia totalis and universalis long-term outcomes: a review. J Eur Acad Dermatol Venereol. 2020;34:709-15.
-
10Firooz A, Firoozabadi MR, Ghazisaidi B, Dowlati Y. Concepts of patients with alopecia areata about their disease. BMC Dermatol. 2005;5:1.
-
11Mulinari-Brenner F. Psychosomatic aspects of alopecia areata. Clin Dermatol. 2018;36:709-13.
-
12Schmitt JV, Ribeiro CF, Souza FH, Siqueira EB, Bebber FR. Hair loss perception and symptoms of depression in female outpatients attending a general dermatology clinic. An Bras Dermatol. 2012;87:412-7.
-
13Baghestani S, Zare S, Seddigh SH. Severity of depression and anxiety in patients with Alopecia Areata in Bandar Abbas. Iran. Dermatol Reports. 2015;7:6063.
-
14Ocek T, Kani AS, Bas A, Yalcin M, Turan S, Emul M, et al. Psychodermatology: knowledge, awareness, practicing patterns, and attitudes of dermatologists in Turkey. Prim Care Companion CNS Disord. 2015;17, eCollection 2015.
-
15Willemsen R, Vanderlinden J, Deconinck A, Roseeuw D. Hypnotherapeutic management of alopecia areata. J Am Acad Dermatol. 2006;55:233-7.
-
16MacDonald Hull SP, Wood ML, Hutchinson PE, Sladden M, Messenger AG. Guidelines for the management of alopecia areata. Br J Dermatol. 2003;149:692-9.
-
17Sardesai VR, Prasad S, Agarwal TD. A study to evaluate the efficacy of various topical treatment modalities for alopecia areata. Int J Trichol. 2012;4:265-70.
-
18Melo DF, Dutra TBS, Baggieri VMAC, Tortelly VD. Intralesional betamethasone as a therapeutic option for alopecia areata. An Bras Dermatol. 2018;93:311-2.
-
19Dainichi T, Kabashima K. Alopecia areata: what’s new in epidemiology, pathogenesis, diagnosis, and therapeutic options?. J Dermatol Sci. 2017;86:3-12.
-
20Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part II. Treatment. J Am Acad Dermatol. 2010;62:191-202.
-
21Kuldeep C, Singhal H, Khare AK, Mittal A, Gupta LK, Garg A. Randomized comparison of topical betamethasone valerate foam, intralesional triamcinolone acetonide and tacrolimus ointment in management of localized alopecia areata. Int J Trichol. 2011;3:20-4.
-
22Spano F, Donovan JC. Alopecia areata: part 2: treatment. Can Fam Physician. 2015;61:757-61.
-
23Hordinsky M, Junqueira AL. Alopecia areata update. Semin Cutan Med Surg. 2015;34:72-5.
-
24Ito T. Advances in the management of alopecia areata. J Dermatol. 2012;39:11-7.
-
25Yee BE, Tong Y, Goldenberg A, Hata T. Efficacy of different concentrations of intralesional triamcinolone acetonide for alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2020;82:1018-21.
-
26Chu TW, AlJasser M, Alharbi A, Abahussein O, McElwee K, Shapiro J. Benefit of different concentrations of intralesional triamcinolone acetonide in alopecia areata: An intrasubject pilot study. J Am Acad Dermatol. 2015;73:338-40.
-
27Spano F, Donovan JC. Alopecia areata: part 1: pathogenesis, diagnosis, and prognosis. Can Fam Physician. 2015;61:751-5.
-
28Tosti A, Piraccini BM, Pazzaglia M, Vincenzi C. Clobetasol propionate 0.05% under occlusion in the treatment of alopecia totalis/universalis. J Am Acad Dermatol. 2003;49:96-8.
-
29Peloquin L, Castelo-Soccio L. Alopecia Areata: an update on treatment options for children. Paediatr Drugs. 2017;19:411-22.
-
30Rigopoulos D, Gregoriou S, Korfitis C, Gintzou C, Vergou T, Katrinaki A, et al. Lack of response of alopecia areata to pimecrolimus cream. Clin Exp Dermatol. 2007;32:456-7.
-
31Messenger AG, Rundegren J. Minoxidil: mechanisms of action on hair growth. Br J Dermatol. 2004;150:186-94.
-
32Rossi A, Cantisani C, Melis L, Iorio A, Scali E, Calvieri S. Minoxidil use in dermatology, side effects and recent patents. Recent Pat Inflamm Allergy Drug Discov. 2012;6:130-6.
-
33Freire PC, Riera R, Martimbianco AL, Petri V, Atallah AN. Minoxidil for patchy alopecia areata: systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33:1792-9.
-
34Strazzulla LC, Wang EH, Avila L, Lo Sicco K, Brinster N, Christiano AM, et al. Alopecia areata: an appraisal of new treatment approaches and overview of current therapies. J Am Acad Dermatol. 2018;78:15-24.
-
35Tang L, Sundberg JP, Lui H, Shapiro J. Old wine in new bottles: reviving old therapies for alopecia areata using rodent models. J Investig Dermatol Symp Proc. 2003;8:212-6.
-
36Kuin RA, Spuls PI, Limpens J, van Zuuren EJ. Diphenylcyclopropenone in patients with alopecia areata. A critically appraised topic. Br J Dermatol. 2015;173:896-909.
-
37Chiang KS, Mesinkovska NA, Piliang MP, Bergfeld WF. Clinical efficacy of Diphenylcyclopropenone in Alopecia Areata: retrospective data analysis of 50 patients. J Investig Dermatol Symp Proc. 2015;17:50-5.
-
38Wu SZ, Wang S, Ratnaparkhi R, Bergfeld WF. Treatment of pediatric alopecia areata with anthralin: a retrospective study of 37 patients. Pediatr Dermatol. 2018;35:817-20.
-
39Kar BR, Handa S, Dogra S, Kumar B. Placebo-controlled oral pulse prednisolone therapy in alopecia areata. J Am Acad Dermatol. 2005;52:287-90.
-
40Kurosawa M, Nakagawa S, Mizuashi M, Sasaki Y, Kawamura M, Saito M, et al. A comparison of the efficacy, relapse rate and side effects among three modalities of systemic corticosteroid therapy for alopecia areata. Dermatology. 2006;212:361-5.
-
41Bin Saif GA, Al-Khawajah MM, Al-Otaibi HM, Al-Roujayee AS, Alzolibani AA, Kalantan HA, et al. Efficacy and safety of oral mega pulse methylprednisolone for severe therapy resistant Alopecia areata. Saudi Med J. 2012;33:284-91.
-
42Parente L. Deflazacort: therapeutic index, relative potency and equivalent doses versus other corticosteroids. BMC Pharmacol Toxicol. 2017;18:1.
-
43Pirmez R, Abraham LS, Duque-Estrada B, Damasco P, Farias DC, Kelly Y, et al. Trichoscopy of steroid-induced atrophy. Skin Appendage Disord. 2017;3:171-4.
-
44Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoid-induced side effects: a comprehensive review: a review of glucocorticoid pharmacology and bone health. J Am Acad Dermatol. 2017;76:1-9.
-
45Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoidinduced side effects: a comprehensive review: Gastrointestinal and endocrinologic side effects. J Am Acad Dermatol. 2017;76:11-6.
-
46Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoidinduced side effects: a comprehensive review: infectious complications and vaccination recommendations. J Am Acad Dermatol. 2017;76:191-8.
-
47Caplan A, Fett N, Rosenbach M, Werth VP, Micheletti RG. Prevention and management of glucocorticoidinduced side effects: a comprehensive review: ocular, cardiovascular, muscular, and psychiatric side effects and issues unique to pediatric patients. J Am Acad Dermatol. 2017;76:201-7.
-
48Thomas S, Fisher KH, Snowden JA, Danson SJ, Brown S, Zeidler MP. Methotrexate is a JAK/STAT pathway inhibitor. PLoS One. 2015;10:e0130078.
-
49Anuset D, Perceau G, Bernard P, Reguiai Z. Efficacy and safety of methotrexate combined with low-to moderate-dose corticosteroids for severe Alopecia Areata. Dermatology. 2016;232:242-8.
-
50Hammerschmidt M, Mulinari Brenner F. Efficacy and safety of methotrexate in alopecia areata. An Bras Dermatol. 2014;89:729-34.
-
51Phan K, Ramachandran V, Sebaratnam DF. Methotrexate for alopecia areata: a systematic review and meta-analysis. J Am Acad Dermatol. 2019;80, 120-7.e2.
-
52Kivity S, Zafrir Y, Loebstein R, Pauzner R, Mouallem M, Mayan H. Clinical characteristics and risk factors for low dose methotrexate toxicity: a cohort of 28 patients. Autoimmun Rev. 2014;13:1109-13.
-
53Shen S, O’Brien T, Yap LM, Prince HM, McCormack CJ. The use of methotrexate in dermatology: a review. Australas J Dermatol. 2012;53:1-18.
-
54Cline A, Jorizzo JL. Does daily folic acid supplementation reduce methotrexate efficacy?. Dermatol Online J. 2017;23,13030/qt4hf5v2vk.
-
55Lai VWY, Chen G, Gin D, Sinclair R. Cyclosporine for moderate-to-severe alopecia areata: a double-blind, randomized, placebo-controlled clinical trial of efficacy and safety. J Am Acad Dermatol. 2019;81:694-701.
-
56Jang YH, Kim SL, Lee KC, Kim MJ, Park KH, Lee WJ, et al. A Comparative study of oral cyclosporine and betamethasone minipulse therapy in the treatment of Alopecia Areata. Ann Dermatol. 2016;28:569-74.
-
57Miteva M, Tosti A. Treatment options for alopecia: an update, looking to the future. Expert Opin Pharmacother. 2012;13:1271-81.
-
58Vañó-Galván S, Hermosa-Gelbard Á, Sánchez-Neila N, Miguel-Gómez L, Saceda-Corralo D, Rodrigues-Barata R, et al. Treatment of recalcitrant adult alopecia areata universalis with oral azathioprine. J Am Acad Dermatol. 2016;74:1007-8.
-
59Mascia P, Milpied B, Darrigade AS, Seneschal J, Eyraud A, Bonamonte D, et al. Azathioprine in combination with methotrexate: a therapeutic alternative in severe and recalcitrant forms of alopecia areata?. J Eur Acad Dermatol Venereol. 2019;33, e494-e5.
-
60Xing L, Dai Z, Jabbari A, Cerise JE, Higgins CA, Gong W, et al. Alopecia areata is driven by cytotoxic Tlymphocytes and is reversed by JAK inhibition. Nat Med. 2014;20:1043-9.
-
61Mackay-Wiggan J, Jabbari A, Nguyen N, Cerise JE, Clark C, Ulerio G, et al. Oral ruxolitinib induces hair regrowth in patients with moderate-to-severe alopecia areata. JCI Insight. 2016;1:e89790.
-
62de Oliveira AB, Alpalhão M, Filipe P, Maia-Silva J. The role of Janus kinase inhibitors in the treatment of alopecia areata: a systematic review. Dermatol Ther. 2019;32:e13053.
-
63Liu LY, Craiglow BG, Dai F, King BA. Tofacitinib for the treatment of severe alopecia areata and variants: a study of 90 patients. J Am Acad Dermatol. 2017;76:22-8.
-
64Kennedy Crispin M, Ko JM, Craiglow BG, Li S, Shankar G, Urban JR, et al. Safety and efficacy of the JAK inhibitor tofacitinib citrate in patients with alopecia areata. JCI Insight. 2016;1:e89776.
-
65Jabbari A, Sansaricq F, Cerise J, Chen JC, Bitterman A, Ulerio G, et al. An Open-label pilot study to evaluate the efficacy of tofacitinib in moderate to severe patch-type Alopecia Areata, Totalis, and Universalis. J Invest Dermatol. 2018;138:1539-45.
-
66Guo L, Feng S, Sun B, Jiang X, Liu Y. Benefit and risk profile of tofacitinib for the treatment of alopecia areata: a systemic review and meta-analysis. J Eur Acad Dermatol Venereol. 2020;34:192-201.
-
67Phan K, Sebaratnam DF. JAK inhibitors for alopecia areata: a systematic review and meta-analysis. J Eur Acad Dermatol Venereol. 2019;33:850-6.
-
68Nissen CV, Wulf HC. Hydroxychloroquine is ineffective in treatment of alopecia totalis and extensive alopecia areata: a case series of 8 patients. JAAD Case Rep. 2016;2:117-8.
-
69Yun D, Silverberg NB, Stein SL. Alopecia areata treated with hydroxychloroquine: a retrospective study of nine pediatric cases. Pediatr Dermatol. 2018;35:361-5.
-
70Sharquie KE, Noaimi AA, Shwail ER. Oral zinc sulphate in treatment of alopecia areata (double blind; crossover study). J Clin Exp Dermatol Res. 2012;3:2-5.
-
71Ead RD. Oral zinc sulphate in alopacia areata—a double blind trial. Br J Dermatol. 1981;104:483-4.
-
72Bakar O, Gurbuz O. Is there a role for sulfasalazine in the treatment of alopecia areata?. J Am Acad Dermatol. 2007;57:703-6.
-
73Kiszewski AE, Bevilaqua M, De Abreu LB. Mesalazine in the treatment of extensive alopecia areata: a new therapeutic option?. Int J Trichology. 2018;10:99-102.
-
74Lattouf C, Jimenez JJ, Tosti A, Miteva M, Wikramanayake TC, Kittles C, et al. Treatment of alopecia areata with simvastatin/ezetimibe. J Am Acad Dermatol. 2015;72:359-61.
-
75Choi JW, Suh DW, Lew BL, Sim WY. Simvastatin/ezetimibe therapy for recalcitrant alopecia areata: an open prospective study of 14 patients. Ann Dermatol. 2017;29:755-60.
-
76Loi C, Starace M, Piraccini BM. Alopecia areata (AA) and treatment with simvastatin/ezetimibe: experience of 20 patients. J Am Acad Dermatol. 2016;74:e99-100.
-
77Cervantes J, Jimenez JJ, DelCanto GM, Tosti A. Treatment of Alopecia Areata with Simvastatin/Ezetimibe. J Investig Dermatol Symp Proc. 2018;19:S25-31.
-
78Fiedler-Weiss VC, Rumsfield J, Buys CM, West DP, Wendrow A. Evaluation of oral minoxidil in the treatment of alopecia areata. Arch Dermatol. 1987;123:1488-90.
-
79Wambier CG, Craiglow BG, King BA. Combination tofacitinib and oral minoxidil treatment for severe alopecia areata. J Am Acad Dermatol. 2019, pii: S0190-9622(19)32688-X.
-
80Darwin E, Arora H, Hirt PA, Wikramanayake TC, Jimenez JJ. A review of monochromatic light devices for the treatment of alopecia areata. Lasers Med Sci. 2018;33:435-44.
-
81Gupta AK, Carviel JL. Meta-analysis of 308-nm excimer laser therapy for alopecia areata. J Dermatolog Treat. 2019;:1-4.
-
82Mlacker S, Aldahan AS, Simmons BJ, Shah V, McNamara CA, Samarkandy S, et al. A review on laser and light-based therapies for alopecia areata. J Cosmet Laser Ther. 2017;19:93-9.
-
83Herz-Ruelas ME, Gomez-Flores M, Miranda-Maldonado I, Welsh E, Ocampo-Candiani J, Welsh O. Escalating dosimetry of UVA-1 in the treatment of alopecia areata. Int J Dermatol. 2017;56:653-9.
-
84van Baar HM, van der Vleuten CJ, van de Kerkhof PC. Dapsone versus topical immunotherapy in alopecia areata. Br J Dermatol. 1995;133:270-4.
-
85Friedmann PS. Unsuccessful treatment of alopecia areata with dapsone. Br J Dermatol. 1981;104:597-8.
-
86Hesseler MJ, Shyam N. Platelet-rich plasma and its utilities in alopecia: a systematic review. Dermatol Surg. 2020;46:93-102.
-
87Strazzulla LC, Avila L, Lo Sicco K, Shapiro J. An overview of the biology of platelet-rich plasma and microneedling as potential treatments for alopecia areata. J Investg Dermatol. 2018;19.S21-S4.
-
88Park J, Kim DW, Park SK, Yun SK, Kim HU. Role of hair prostheses (wigs) in patients with severe alopecia areata. Ann Dermatol. 2018;30:505-7.
-
89Inui S, Inoue T, Itami S. Psychosocial impact of wigs or hairpieces on perceived quality of life level in female patients with alopecia areata. J Dermatol. 2013;40:225-6.
-
90Alkhalifah A, Alsantali A, Wang E, McElwee KJ, Shapiro J. Alopecia areata update: part I. Clinical picture, histopathology, and pathogenesis. J Am Acad Dermatol. 2010;62:177-88.
-
91Salsberg JM, Donovan J. The safety and efficacy of diphencyprone for the treatment of alopecia areata in children. Arch Dermatol. 2012;148:1084-5.
-
92Saceda-Corralo D, Grimalt R, Fernández-Crehuet P, Clemente A, Bernárdez C, Garcia-Hernandez MJ, et al. Beard alopecia areata: a multicentre review of 55 patients. J Eur Acad Dermatol Venereol. 2017;31:187-92.
-
93Kassim JM, Shipman AR, Szczecinska W, Siah TW, Lam M, Chalmers J, et al. How effective is intralesional injection of triamcinolone acetonide compared with topical treatments in inducing and maintaining hair growth in patients with alopecia areata? A critically appraised topic. Br J Dermatol. 2014;170:766-71.
-
94Barrón-Hernández YL, Tosti A. Bimatoprost for the treatment of eyelash, eyebrow and scalp alopecia. Expert Opin Investig Drugs. 2017;26:515-22.
-
95Vila TO, Camacho Martinez FM. Bimatoprost in the treatment of eyelash universalis alopecia areata. Int J Trichology. 2010;2:86-8.
-
96Borchert M, Bruce S, Wirta D, Yoelin SG, Lee S, Mao C, et al. An evaluation of the safety and efficacy of bimatoprost for eyelash growth in pediatric subjects. Clin Ophthalmol. 2016;10:419-29.
-
97Olsen EA, Roberts J, Sperling L, Tosti A, Shapiro J, McMichael A, et al. Objective outcome measures: collecting meaningful data on alopecia areata. J Am Acad Dermatol. 2018;79, 470-8.e3.
Publication Dates
-
Publication in this collection
24 Mar 2021 -
Date of issue
Nov-Dec 2020
History
-
Received
2 Mar 2020 -
Accepted
15 May 2020