Abstracts
Pyomyositis is a primary infection of the skeletal muscle, occurring most commonly in tropical countries. Adults who develop the disease have, in most cases, associated comorbidities that compromise the immune system, including diabetes mellitus and liver cirrhosis
pyomyositis; diabetes mellitus; liver cirrhosis
A piomiosite é uma infecção primária do músculo esquelético mais comum nos países tropicais. Adultos que desenvolvem a doença apresentam, na maioria dos casos, comorbidades associadas que comprometem o sistema imunológico, entre elas diabetes mellitus e cirrose hepática
piomiosite; diabetes mellitus; cirrose hepática
CASE REPORT
IFirst year resident at Rheumatology Sector da Fundação Faculdade Regional de Medicina - FAMERP
IIFirst year resident at General Surgery Sector of FAMERP
IVAssistant Physician at Rheumatology Sector of FAMERP
VProfessor at Rheumatology Sector of FAMERR
Correspondence to
ABSTRACT
Pyomyositis is a primary infection of the skeletal muscle, occurring most commonly in tropical countries. Adults who develop the disease have, in most cases, associated comorbidities that compromise the immune system, including diabetes mellitus and liver cirrhosis.
Keywords: pyomyositis, diabetes mellitus, liver cirrhosis.
INTRODUCTION
Pyomyositis is a disease of skeletal muscle. It can affect any muscle group by contiguity or hematogenous spread from a distant focus. Apredilection for muscle groups of the trunk and lower limbs is observed. Staphylococcus aureus is usually the etiologic agent found in cases described in literature.1.2
A delay regarding the diagnosis of pyomyositis is usually observed due to the nonspecific clinical signs at onset. Pyomyositis can possibly be mistaken for bone or joint infectious processes, thrombophlebitis, panniculitis, or systemic diseases.3
CASE REPORT
Female, 42 years old, with a history of hepatitis C virus cirrhosis and type 2 diabetes mellitus was admitted to the Rheumatology Service reporting pain in lateral face of right thigh for 20 days. Initially, the pain was sudden and of high intensity, progressively worsening, and irradiating to entire right leg, getting worse with walking. The patient also reported measured fever of 38ºC and asthenia. On physical examination, she was prostrated, pale, jaundiced; blood pressure 100 x 70 mmHg; heart rate of 100 beats per minute; axillary temperature of 38.6ºC; pain on palpation of lateral face of right thigh; and pain on rotation of internal and external right hip joint, without signs of inflammation or joint blockage.
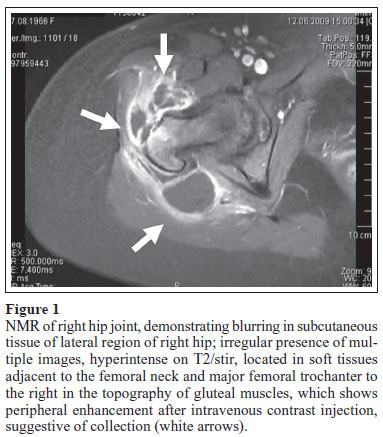
The patient underwent additional tests: complete blood count showed hemoglobin 9.8 mg/dL, hematocrit 29%, WBC 2500/mm3 with neutrophils 72%, eosinophils 2%, lymphocytes 10%, monocytes 16%, and platelets 23.000/mm3; C-reactive protein (CRP) 20.07 mg/dL; erythrocyte sedimentation rate (ESR) 52mm; C3 and C4 decreased; absent cryoglobulins; creatine phosphokinase (CPK) 40UI / L; creatinine 0.8 m/ dL; IgE 64 ng/mL; albumin 2, 4 g/dL; prothrombin time activation 17.1 s; INR 1.6; activated partial thromboplastin time 31.4 s; prothrombin activity 43%; serum glucose 187mg/ dL; total bilirubin 3.2 mg/dL; direct bilirubin 1,3 mg/dL; indirect bilirubin 1.9 mg/dL; blood culture positive for group B beta-hemolytic Streptococcus. Radiography of right hip joint showed no change; ultrasonography showed presence of edema in thigh muscle and absence of collections suggestive of abscess; nuclear magnetic resonance (NMR) showed collection areas within gluteus muscle and peritrochanteric region (Figure 1). Muscle biopsy showed debridement product of gluteus region with acute and partly exudative inflammatory process in fibrous connective and fat tissues.
Given the results found on NMR, pyomyositis was diagnosed, with indication for open surgical drainage (Figure 2), biopsy, and collection of material for culture.
In our case, we chose to start oxacillin (2 g intravenously every 6 hours) and antibiotic therapy, taking into account the high prevalence of Staphylococcus aureus as the main agent, which is consistent with reports in literature. However, we observe growth of group B beta-hemolytic Streptococcus in both blood culture and secretions collected during surgery and, therefore, after the outcome of the new antibiogram, antibiotic therapy was changed to cefepime (1 g every 12 hours).
On the ninth day of treatment with cefepime, the patient developed fever and, even showing no signs of inflammation or formation of new collection on surgical site, we decided to change the antibiotic. As a result of the antibiogram, the patient was treated with sulbactam (1 g intravenously every 6 hours) and ampicillin (2 g intravenously every 6 hours) for 21 days. Patient's general condition was improved, there was a decrease in CRP value reaching 2.76 mg/dL and ESR decreased to 38 mm. However, the pancytopenia persisted, probably attributed to hypersplenism secondary to cirrhosis unrelated to the infection condition. During the course of evolution, CPK levels remained within normal limits.
DISCUSSION
According to Marques et al., Scriba was the first to report pyomyositis in 1985. It is a disease that preferentially affects individuals in the first and second decades of life, with prevalence in men.4 Adults above 30 years of age who develop the disease, in 50% of the time, have an associated comorbidity.1 Associations reported in literature include patients with the human immunodeficiency virus, diabetes mellitus, cancer, liver cirrhosis, kidney failure, transplant recipients and users of immunosuppressive agents.5,6
The pathogenesis of primary pyomyositis remains unclear, although the role of trauma and immune impairment are questioned as predisposing factors.7,8
In our case, the patient had comorbidities such as hepatitis C virus and diabetes mellitus, both involved in reducing the immune response.
Laboratory findings are nonspecific, but blood count can reveal everything from leukopenia to leukocytosis with left shift, depending on the etiologic agent and the individual immune response. Eosinophilia may be found in patients with concomitant parasitic infection.9 There may be increased inflammatory evidence, and CPK usually does not change.1,5 NMR is the gold standard for pyomyositis diagnosis, since it is possible to detect early findings of muscles diffuse inflammation.1
The etiology of pyomyositis is attributed mainly to Staphylococcus aureus (85% to 95%), followed by Streptococcus sp. (1% to 5%) and, rarely, by enterobacteriaceae.10 Blood cultures are positive in less than 40% of patients and secretion cultures are positive in only 21-41% of cases.1 Pyomyositis usually affect only one muscle, but 11% to 43% of patients may have widespread outbreaks in various muscles. The primary muscle involved is the quadriceps, followed by gluteal and iliopsoas muscles.11
According to literature, the infection whose etiologic agent is Streptococcus sp. can be very aggressive, causing extensive muscle necrosis and septicemia, while infections whose etiologic agent is Staphylococcus aureus tend to present better evolution.10 Our objective in reporting this case is to alert about the need for early diagnosis and prompt introduction of therapy for patient to obtain a better clinical outcome.
REFERENCES
-
1Bickels J, Ben-Sira L, Kessler A, Wientroub S. Primary pyomyositis. J Bone Joint Surg Am 2002; 84A(12):2277-86.
-
2Saissy JM, Ducourau JP, Tchoua R, Diatta B. Tropical myositis. Med Trop 1998; 58(3):297-306.
-
3Mangueira CLP. Piomiosite tropical em jovem imunocompetente: relato de caso e revisão da literatura. J Bras Patol Med Lab 2000; 36(4):247-50.
-
4Marques GC, Mauro Filho GL, Valiatti M et al Piomiosite tropical: estudo retrospectivo de 27 casos. Rev Bras Reumatol 1995; 35(4):193-200.
-
5Crum NF. Bacterial pyomiositis in the United States. Am J Med 2004; 117(6):420-8.
-
6Belsky DS, Teates CD, Hartman ML. Case Report: Diabetes mellitus as a predisposing factor in the development of pyomyositis. Am J Med Sci 1994; 308(4):251-4.
-
7Verab RM, Marquésa AF, Maestreb MM. Piomiositis lumbar por Finegoldia magna (Peptostreptococcus magnus) en paciente con hepatitis. C Med Clin (Barc) 2008; 130(9):357-9.
-
8Patel SR, Olenginski TP, Perruquet JL, Harrington TM. Pyomyositis: clinical features and predisposing conditions. J Rheumatol 1997; 24(9):1734-8.
-
9Scharschmidt TJ, Weiner SD, Myers JP. Bacterial pyomiosytis. Curr Infect Dis Rep 2004; 6(5):393-6.
-
10Azevedo PS, Matsui M, Matsubara LS et al Piomiosite tropical: apresentações atípicas. Rev Soc Bras Med Trop 2004; 37(3):273-8.
-
11Ejnisman B, Sayum Filho J, Andreolli CV, Monteiro GC, Pochini AC, Cohen M. Piomiosite multifocal em atleta: relato de caso. Rev Bras Ortop 2007; 42(5):157-60.
Pyomyositis associated with diabetes mellitus and liver cirrhosis
Publication Dates
-
Publication in this collection
08 Sept 2010 -
Date of issue
Aug 2010
History
-
Received
28 July 2009 -
Accepted
26 May 2010