Abstracts
Inflammatory bowel diseases (Crohn's disease and ulcerative rectocolitis) have extraintestinal manifestations 25% of the patients, with the most common one being the enteropathic arthritis. METHODS: Prospective, observational, multicenter study with patients from 29 reference centers participating in the Brazilian Registry of Spondyloarthritis (RBE), which incorporates the RESPONDIA (Ibero-American Registry of Spondyloarthritis) group. Demographic and clinical data were collected from 1472 patients and standardized questionnaires for the assessment of axial mobility, quality of life, enthesitic involvement, disease activity and functional capacity were applied. Laboratory and radiographic examinations were performed. The aim of this study is to compare the clinical, epidemiological, genetic, imaging, treatment and prognosis characteristics of patients with enteropathic arthritis with other types of spondyloarthritis in a large Brazilian cohort. RESULTS: A total of 3.2% of patients were classified as having enteroarthritis, 2.5% had spondylitis and 0.7%, arthritis (peripheral predominance). The subgroup of individuals with enteroarthritis had a higher prevalence in women (P < 0.001), lower incidence of inflammatory axial pain (P < 0.001) and enthesitis (P = 0.004). HLA-B27 was less frequent in the group with enteroarthritis (P = 0.001), even when considering only those with the pure axial form. There was a lower prevalence of radiographic sacroiliitis (P = 0.009) and lower radiographic score (BASRI) (P = 0.006) when compared to patients with other types of spondyloarthritis. They also used more corticosteroids (P < 0.001) and sulfasalazine (P < 0.001) and less non-steroidal anti-inflammatory drugs (P < 0.001) and methotrexate (P = 0.001). CONCLUSION: There were differences between patients with enteroarthritis and other types of spondyloarthritis, especially higher prevalence of females, lower frequency of HLA-B27, associated with less severe axial involvement.
Enteropathic arthritis; Crohn's Disease; Ulcerative rectocolitis; Registry studies
As doenças inflamatórias intestinais (doença de Crohn e retocolite ulcerativa) apresentam manifestações extraintestinais em um quarto dos pacientes, sendo a mais comum a artrite enteropática. MÉTODOS: Estudo prospectivo, observacional e multicêntrico, realizado com pacientes de 29 centros de referência participantes do Registro Brasileiro de Espondiloartrites (RBE), que se incorpora ao grupo RESPONDIA (Registro Ibero-americano de Espondiloartrites). Dados demográficos e clínicos de 1472 pacientes foram colhidos, e aplicaram-se questionários padronizados de avaliação de mobilidade axial, de qualidade de vida, de envolvimento entesítico, de atividade de doença e de capacidade funcional. Exames laboratoriais e radiográficos foram realizados. Objetivamos, neste presente artigo, comparar as características clínicas, epidemiológicas, genéticas, imagenológicas, de tratamento e prognóstico de enteroartríticos com os outros espondiloartríticos nesta grande coorte brasileira. RESULTADOS: Foram classificados como enteroartrite 3,2% dos pacientes, sendo que 2,5% tinham espondilite e 0,7%, artrite (predomínio periférico). O subgrupo de indivíduos com enteroartrite apresentava maior prevalência de mulheres (P < 0,001), menor incidência de dor axial inflamatória (P < 0,001) e de entesite (P = 0,004). O HLA-B27 foi menos frequente no grupo de enteroartríticos (P = 0,001), mesmo se considerado apenas aqueles com a forma axial pura. Houve menor prevalência de sacroiliíte radiológica (P = 0,009) e também menor escore radiográfico (BASRI) (P = 0,006) quando comparado aos pacientes com as demais espondiloartrites. Também fizeram mais uso de corticosteroides (P < 0,001) e sulfassalasina (P < 0,001) e menor uso de anti-inflamatórios não hormonais (P < 0,001) e metotrexato (P = 0,001). CONCLUSÃO: Foram encontradas diferenças entre as enteroartrites e as demais espondiloartrites, principalmente maior prevalência do sexo feminino, menor frequência do HLA-B27, associados a uma menor gravidade do acometimento axial.
Artrite enteropática; Doença de Crohn; Retocolite ulcerativa; Estudos de registro
ORIGINAL ARTICLE
I Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brasil
II Instituto Insper de Educação e Pesquisa, São Paulo, SP, Brasil
III Disciplina de Reumatologia, Universidade de São Paulo, São Paulo, SP, Brasil
IV Universidade de Brasília, Brasília, DF, Brasil
V Hospital Geral de Goiânia, Goiânia, GO, Brasil
VI Universidade de Campinas, Campinas, SP, Brasil
VII Universidade Federal do Amazonas, Manaus, AM, Brasil
VIII Pontifícia Universidade Católica, Porto Alegre, RS, Brasil
IX Faculdade de Medicina de São José do Rio Preto, São José do Rio Preto, SP, Brasil
X Hospital Evangélico de Curitiba, Curitiba, PR, Brasil
XI Universidade Federal do Rio de Janeiro, Rio de Janeiro, RJ, Brasil
XII Universidade Federal do Paraná, Curitiba, PR, Brasil
XIII Hospital Geral de Fortaleza, Fortaleza, CE, Brasil
XIV Universidade Estadual do Rio de Janeiro, Rio de Janeiro, RJ, Brasil
XV Santa Casa do Rio de Janeiro, Rio de Janeiro, RJ, Brasil
XVI Pontifícia Universidade Católica, Campinas, SP, Brasil
XVII Santa Casa de São Paulo, São Paulo, SP, Brasil
XVIII Hospital de Base, Brasília, DF, Brasil
XIX Universidade Federal do Mato Grosso do Sul, Campo Grande, MS, Brasil
XX Universidade Federal de Pernambuco, Recife, PE, Brasil
XXI Universidade Federal do Rio Grande do Sul, Porto Alegre, RS, Brasil
XXII Faculdade de Medicina Souza Marques, Rio de Janeiro, RJ, Brasil
XXIII Hospital do Servidor Público Estadual, São Paulo, SP, Brasil
XXIV Instituto de Ortopedia e Traumatologia, Universidade de São Paulo, São Paulo, SP, Brasil
XXV Universidade Federal de Santa Catarina, Florianópolis, SC, Brasil
XXVI Universidade Federal de São Paulo, São Paulo, SP, Brasil
XXVII Santa Casa de Belo Horizonte, Belo Horizonte, MG, Brasil
XXVIII Universidade Federal do Ceará, Fortaleza, CE, Brasil
XXIX Escola de Medicina e Saúde Pública, Salvador, BA, Brasil
XXX Universidade Federal do Pará, Belém, PA, Brasil
XXXI Universidade Federal do Espírito Santo, Vitória, ES, Brasil
ABSTRACT
Inflammatory bowel diseases (Crohn's disease and ulcerative rectocolitis) have extraintestinal manifestations 25% of the patients, with the most common one being the enteropathic arthritis.
METHODS: Prospective, observational, multicenter study with patients from 29 reference centers participating in the Brazilian Registry of Spondyloarthritis (RBE), which incorporates the RESPONDIA (Ibero-American Registry of Spondyloarthritis) group. Demographic and clinical data were collected from 1472 patients and standardized questionnaires for the assessment of axial mobility, quality of life, enthesitic involvement, disease activity and functional capacity were applied. Laboratory and radiographic examinations were performed. The aim of this study is to compare the clinical, epidemiological, genetic, imaging, treatment and prognosis characteristics of patients with enteropathic arthritis with other types of spondyloarthritis in a large Brazilian cohort.
RESULTS: A total of 3.2% of patients were classified as having enteroarthritis, 2.5% had spondylitis and 0.7%, arthritis (peripheral predominance). The subgroup of individuals with enteroarthritis had a higher prevalence in women (P < 0.001), lower incidence of inflammatory axial pain (P < 0.001) and enthesitis (P = 0.004). HLA-B27 was less frequent in the group with enteroarthritis (P = 0.001), even when considering only those with the pure axial form. There was a lower prevalence of radiographic sacroiliitis (P = 0.009) and lower radiographic score (BASRI) (P = 0.006) when compared to patients with other types of spondyloarthritis. They also used more corticosteroids (P < 0.001) and sulfasalazine (P < 0.001) and less nonsteroidal anti-inflammatory drugs (P < 0.001) and methotrexate (P = 0.001).
CONCLUSION: There were differences between patients with enteroarthritis and other types of spondyloarthritis, especially higher prevalence of females, lower frequency of HLA-B27, associated with less severe axial involvement.
Keywords: Enteropathic arthritis; Crohn's Disease; Ulcerative rectocolitis; Registry studies
Introduction
Inflammatory bowel disease (IBD) is the term currently used to designate two diseases considered idiopathic to date: Crohn's disease (CD) and ulcerative rectocolitis (URC). Although grouped together, the two can be differentiated by defined clinical, endoscopic, histological, and etiopathogenic characteristics.
Both diseases affect men and women equally and have a peak incidence in the second and third decades of life; the prevalence of each is estimated at 25-250 per 100,000 individuals, with a slight predominance of URC.Their main symptoms are diarrhea, abdominal pain, and gastrointestinal bleeding, in addition to systemic symptoms such as fever, weight loss, and fatigue. They often have an intermittent course, alternating periods of exacerbation and remission.
CD is characterized by transmural (granulomatous in only approximately 30%) and discontinuous inflammation of the digestive tract, and it affects mainly the distal small intestine (ileum), but with potential to reach any other segment, from the mouth to the anus. Due to its tendency to cause fibrosis, it can lead to stenosis and obstruction, and because of the possibility of micro-perforations, fistulas may appear.
URC, in turn, is characterized by a superficial and continuous involvement of the colonic mucosa, almost invariably involving the rectum and sometimes extending proximally. It is usually classified (regarding the severity and extent of involvement) as mild when only the rectum or rectosigmoid are affected (proctitis or proctosigmoiditis); as moderate, when the descending colon is also affected (left colitis); and as severe, when it reaches the cecum (pancolitis).
Other extraintestinal manifestations can be associated to IBD in approximately 25% of patients; the most common are those caused by joint (axial or peripheral), eye (uveitis and episcleritis), skin (erythema nodosum and pyoderma gangrenosum), and biliary tract (sclerosing cholangitis) involvement. These symptoms may precede, coexist with, or follow the intestinal manifestations.1-4
Enteroarthritis is the most common extraintestinal manifestation of IBD, whose prevalence varies from 14% to 44%.5-8 It has two main patterns of clinical expression: the peripheral and axial forms. The first can be divided into two subgroups: type I, which is often self-limited, oligoarticular (< five joints involved), accompanies outbreaks of intestinal inflammatory activity, and is not associated with the presence of HLA-B27; and type II, polyarticular, usually follows an independent course from the intestinal disease. The latter rarely becomes chronic. The axial form can include sacroiliitis and/or spondylitis unrelated to the bowel disease activity, and may even precede its onset by years.9-12 This is associated with the presence of HLA-B27 in 50% to 75% of cases - a similar frequency, although lower, than that found in idiopathic spondylitis.13-15 There is often some overlapping between these forms, and periarticular involvement is possible, whether of the entheses, tendons, or the periosteum.5,16-18
CARD15 gene polymorphisms have been associated with an increased risk of developing CD, and are considered predictors of both chronic inflammatory bowel disease in patients with spondyloarthritis and sacroiliitis in those with CD. This gene encodes an intracellular protein expressed in several cell types, which act as receptor for components of bacterial cell wall, and is involved in the activation of nuclear factor kappaβ (NF-kβ) and apoptosis.8,19,20
In this article, the main characteristics of the sample of enteropathic arthritis of the Brazilian Registry of Spondyloarthritis (Registro Brasileiro de Espondiloartrites - RBE) are discussed.
Methods
This was a prospective, observational, multicenter study, conducted with patients from 29 reference centers participating in the RBE. All patients met the criteria of the European Spondyloarthropathy Study Group (ESSG).21 Data were collected from June 2006 to December 2009. The RBE is a member of the Ibero-American Registry of Spondyloarthritis (RESPON-DIA) group, which consists of nine Latin American countries (Argentina, Brazil, Costa Rica, Chile, Ecuador, Mexico, Peru, Uruguay, and Venezuela) and the two countries of the Iberian Peninsula (Spain and Portugal).
In this study, a standard protocol was applied to the 1,472 patients. The diagnosis of enteroarthritis was considered when a patient had peripheral or axial inflammatory joint involvement associated with CD or URC, diagnosed by a physician and confirmed by radiographic or endoscopic examination.
Demographic and clinical data were collected, and the following questionnaires, previously translated and validated for Brazilian Portuguese) were applied : Bath Ankylosing Spondylitis Metrologic Index (BASMI), to assess spinal mobility;22 Ankylosing Spondylitis Quality of Life (ASQoL), to assess quality of life;23 Maastricht Ankylosing Spondylitis enthesitis score (MASES), to assess enthesitic involvement;24 Bath Ankylosing Spondylitis Disease Activity Index (BASDAI), to assess disease activity,25 and Bath Ankylosing Spondylitis Functional Index (BASfi) to assess functional capacity.26
Laboratory test results (HLA-B27, erythrocyte sedimentation rate [ESR] and C-reactive protein [CRP]) were also recorded, as well as radiographs of the cervical and lumbosacral spine and the sacroiliac and coxofemoral joints. Radiological damage was evaluated using the Bath Ankylosing Spondylitis Radiologic Index (BASRI).27
Statistical analysis
Pearson's chi-squared test was used to analyze the association between enteroarthritis and categorical variables, and Student's t-test was used to compare means of numerical variables between patients with enteroarthritis and other types of spondyloarthritis. An alpha of 5% was used in all tests: those with P < 0.05 were considered to be statistically significant.
Results
Of a total of 1,472 patients, 65.4% (N = 963) were classified as having ankylosing spondylitis (AS), 18.4% (N = 271) as psoriatic arthritis (PA), 6.7% (N = 98) as undifferentiated spondyloarthritis (USpA), 3.3% (N = 49) as reactive arthritis (ReA), and 3.2% (N = 48) as enteropathic arthritis (EA), with 2.5% (N = 7) of spondylitis associated with IBD and 0.7% (N = 11) of arthritis associated with IBD. Also, 2.9% were classified as having juvenile spondyloarthritis (JSpA) (Fig. 1).
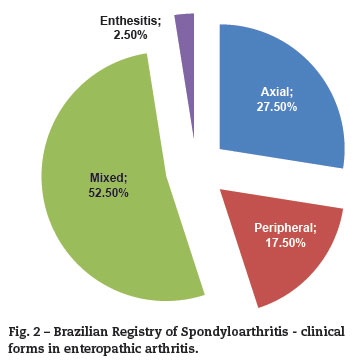
Regarding the clinical forms identified among individuals with enteroarthritis, it was observed that the overlapping (mixed form, with both axial and peripheral involvement) was the most common phenotype with 52.5%, followed by the pure axial with 27.5%; isolated peripheral form, with 17.5%; and enthesitic form, without axial or peripheral joint involvement, with 2.5% (Fig. 2).
When comparing the clinical characteristics (Table 1) of the enteroarthritis group and of other types of spondyloarthritis, a statistically significant difference was observed regarding the higher frequency of females (P < 0.001) and the lower frequency of inflammatory axial pain (P < 0.001) and of enthesitis (P = 0.004) in patients with enteropathic arthritis.
Patients with enteropathic arthritis showed lower mean disease duration (9.6 years vs. 14.1 years, P = 0.005), fewer inflamed joints (0.77 vs. 1.61, P = 0.004), as well as better rates of mobility in the lumbar spine (mean lateral lumbar flexion of 31.5 cm vs. 25.4 cm, P = 0.03; and Schober index of 6.2 cm vs. 4.8 cm, P = 0.051). No statistical difference was observed between the prevalence of extra-articular manifestations, although there was a trend of lower incidence of ocular disease (anterior uveitis) in patients with enteroarthritis (10.4% vs. 20.3% in other types of spondyloarthritis, P = 0.092) (Table 1).
Positivity for HLA-B27 was also statistically significant, with a lower frequency in patients with enteroarthritis (p = 0.001). There was also a statistical difference in CRP measurements between the two groups, with lower values among those with enteropathic arthritis (5.48 mg/L vs. 10.29 mg/L, P = 0.001). Conversely, the latter showed a statistical trend to higher values of ESR (31.3 mm vs. 24.7 mm. P = 0.08).
Regarding radiographic alterations, there was a lower prevalence of radiographic sacroiliitis, considering at least grade II bilateral or III unilateral (modified New York criteria)28 in individuals from the enteroarthritis group (60.4% vs. 76.8% P = 0.009). BASRI scores were also lower, with a mean of 5.2 and 7.1 in enteroarthritis and other diseases (P = 0.006), respectively and of the BASRI coxofemoral-component (0.6 vs. 1.2; P = 0.001).
No statistical differences were observed between the two groups regarding professional activity, work disability, exercise habits, or ASQoL, BASDAI, BASfi, and MASES scores (Table 2).
As for the therapeutic regimens used (Table 3), a more frequent use of corticosteroids was observed (62.5% vs. 34.6%; P < 0.001) and less frequent use of nonsteroidal anti-inflammatory drugs (NSAIDs) (43.8% vs. 68.2%; P < 0.001).There was also a difference regarding the evaluation of NSAIDs efficacy by patients. In the enteroarthritis group, only 35.4% of the patients described NSAIDs as being effective (i.e., capable of effectively improving pain within 48 hours), compared with 69.3% of individuals with the other diseases (P < 0.001). There is a limitation on the scoring for this comparison, since different drug doses and regimens were grouped under the same category.
Among the disease-modifying antirheumatic drugs (DMARDs), there was also a statistical difference between the use of methotrexate (with lower use in enteroarthritis, 29.2% vs. 52.6%, P = 0.001) and sulfasalazine (with greater use in this group, 79.2% vs. 43.2 %, P < 0.001). Among the anticytokine agents, infliximab showed only a statistical trend in the frequency of use between the groups (use in the enteroarthritis group, 25%, and in other diseases, 15%, P = 0.057).There was no difference between the groups regarding the use of other anti-TNF agents, adalimumab, and etanercept; it is noteworthy that the latter drugs were introduced more recently in Brazil.
Discussion
The enteroarthritides, classified within the group of spondyloarthritides, have peculiar characteristics that differ in some aspects from idiopathic ankylosing spondylitis and other diseases in this group. In this study, a small predominance of the female gender was observed among patients with enteroarthritis, in contrast with other types of spondyloarthritis (where the male/female ratio approaches 3:1). The findings are consistent with the results of studies that found a balance5,6,9,29-31 or higher frequency in the female gender,32-34 although some authors found a male predominance even among patients with enteropathic arthritis.8,10,17,35-37
These discrepancies may reflect population differences, but above all, they can be related to the fact that some of the aforementioned studies did not subdivide their patients into more specific groups, such as axial or peripheral involvement, or did not consider only patients with enteropathic arthritis, but also individuals with inflammatory bowel disease without joint involvement, which in practice greatly diminishes the validity of the comparison.
Regarding the clinical presentation, no significant differences were observed between the groups with enteropathic arthritis and other types of spondyloarthritis. In both groups, there was a predominance of mixed form in approximately 50% of patients, followed by axial and peripheral forms, and less frequently, the enthesitic form. These data are similar to those found in other studies.17,38,39
A less severe axial involvement was observed in patients with enteroarthritis when compared to individuals with other types of spondyloarthritis, verified by the lower prevalence of inflammatory axial pain, better rates of mobility in the lumbosacral spine, lower frequency of radiographic sacroiliitis, and lower BASRI scores (lower radiographic damage). Nevertheless, no difference was observed between measures of functional capacity, disease activity and quality of life. However, this finding does not necessarily indicate a more "benign" nature of IBD-related spondylitis, as it may be due to the difference in time of evolution between the two groups in this sample (on average, patients with enteropathic arthritis had approximately four years and six months less time of symptoms than the others).Some authors have found a positive association between the duration of bowel disease and the likelihood of developing extraintestinal manifestations, reinforcing this hypothesis.9,10,40 A number of case series are consistent with the finding of lower radiographic grade in patients with IBD, even in symptomatic axial disease.29,41,42 In other studies, however, the radiographic classification of severity was similar between classical and enteropathic spondylitis.43,44
When comparing the frequency of radiographic sacroiliitis among patients with enteropathic arthritis in the current sample (60%) with several other studies (20% to 61%),17,31,36,37,45 a high frequency of these alterations was confirmed, even without a clear clinical correlation, i.e., no history of pain in the buttocks or lumbar region, constituting what some authors call subclinical or asymptomatic sacroiliitis.6,7,40,41,46-49 Nevertheless, the comparison of these data is possibly flawed, given the great variation among the selected populations, imaging methods used, the criteria used, and the observers according to different studies - many of which were multicenter, including the present study.
This study also found a lower prevalence of HLA-B27 in individuals with enteroarthritis when compared to other types of spondyloarthritis (38.5% vs. 70.1%; P = 0.001), although this difference decreases when the subgroup with pure axial involvement (IBD-related spondylitis), in which the presence of this antigen reaches 47.6, is analyzed separately. Among those classified as having the pure peripheral form that were tested, none had it. The results are consistent with those of studies that found a higher prevalence of HLA-B27 in patients with IBD and axial form than in patients without the axial form (albeit at a lower frequency when compared to that found in idiopathic ankylosing spondylitis).10,17,35,40,48,50
However, the population frequency of the allele should always be considered when interpreting data on the prevalence of genetic markers, which may explain discrepancies between different studies with different populations.35,51
Regarding the medications, the lower frequency of use of NSAIDs and higher use of corticosteroids have also been observed in other studies,17,50 and probably reflect the fear of administering NSAIDs to patients with IBD at risk of exacerbation of bowel symptoms.This risk, however, has no consensus regarding its real magnitude.52
In the present study, differences between patients with enteroarthritis and other spondyloarthritides were observed, especially higher prevalence in females, and lower frequency of HLA-B27, even in those with the pure axial form and associated with the lower degree of severity of axial involvement. These peculiarities should be taken into account when managing patients with IBD and musculoskeletal complaints.
Conflicts of interest
The electronic version of the Brazilian Registry of Spondyloarthritis is supported by a grant from Wyeth/Pfizer Brazil, which had no influence on the collection and analysis of data or in the writing and publication of articles. Percival Sampaio-Barros received a research grant from the Federico Foundation.
REFERENCES
-
1Greenstein A, Janowitz H, Sachar D. The extra-intestinal complications of Crohn's disease and ulcerative colitis:a study of 700 patients. Medicine (Baltimore). 1976;55(5):401-12.
-
2Münch H, Purrmann J, Reis H, Bertrams J, Zeidler H, Stolze T, et al. Clinical features of inflammatory joint and spine manifestations in Crohn's disease. Hepatogastroenterology. 1986;33(3):123-7.
-
3Veloso F, Carvalho J, Magro F. Immune-related systemic manifestations of inflammatory bowel disease. A prospective study of 792 patients. J Clin Gastroenterol. 1996;23(1):29-34.
-
4Maeda K, Okada M, Yao T, Sakurai T, Iida M, Fuchigami T, et al. Intestinal and extraintestinal complications of Crohn's disease:Predictors and cumulative probability of complications. J Gastroenterol. 1994;29:577-82.
-
5Vavricka S. Frequency and Risk Factors for Extraintestinal Manifestations in the Swiss Inflammatory Bowel Disease Cohort. Am J Gastroenterol. 2011;106:110-19.
-
6Queiro R, Maiz O, Intxausti J, de Dios J, Belzuneghi J, Gonzáles C, et al. Subclinical sacroiliitis in Inflammatory Bowel Disease:A clinical and follow-up study. Clin Rheumatol. 2000;19:445-49.
-
7Turkcapar N, Toruner M, Soykan I, Aydintug O, Cetinkaya H, Duzgun N, et al. The prevalence of extraintestinal manifestations and HLA association in patients with inflammatory bowel disease. Rheumatol Int. 2006;26:663-68.
-
8Larsen S, Bendtzen K, Nielsen O. Extraintestinal manifestations of inflammatory bowel disease:Epidemiology, diagnosis, and management. Annals of Medicine. 2010;42:97-114.
-
9Palm Ø, Moum B, Jahnsen J, Gran J. The prevalence and incidence of peripheral arthritis in patients with inflammatory bowel disease, a prospective population-based study (the IBSEN study). Rheumatology. 2001;40:1256-61.
-
10Palm Ø, Moum B, Ongre A, Gran J. Prevalence of Ankylosing Spondylitis and Other Spondyloarthropathies Among Patients with Inflammatory Bowel Disease:A Population Study (The IBSEN Study). J Rheumatol. 2002;29(3):511-15.
-
11Carvalho M, Lage R. Espondiloartropatias. In Carvalho M, Lanna C, Bértolo M. Reumatologia - Diagnóstico e Tratamento. 3rd ed. Rio de Janeiro:Guanabara Koogan SA; 2008.
-
12Holden W, Orchard T, Wordsworth P. Enteropathic arthritis. Rheum Dis Clin N Am 2003;29:513-30.
-
13Orchard T, Wordsworth B, Jewell D. Peripheral arthropathies in inflammatory bowel disease:their articular distribution and natural history. Gut. 1998;42:387-91.
-
14Rudwaleit M, Baeten D. Ankylosing spondylitis and bowel disease. Best Pract Res Clinical Rheumatol. 2006;20(3):451-71.
-
15Voulgari PV. Rheumatological manifestations in inflammatory bowel disease. Ann Gastroenterol. 2011;24(3):173-80.
-
16Lanna C, Ferrari M, Carvalho M, Cunha A. Manifestações Articulares em Pacientes com Doença de Crohn e Retocolite Ulcerativa. Rev Bras Reumatol. 2006;46(S1):45-51.
-
17Collantes E, Zarco P, Munoz E, Juanola X, Mulero J, Fernandez-Sueiro J, et al Disease pattern of spondyloarthropathies in Spain:description of the first national registry (REGISPONSER)-extended report. Rheumatology 2007;46:1309-15.
-
18Salvarani C, Fries W. Clinical features and epidemiology of spondyloarthritides associated with inflammatory bowel disease. World J Gastroenterol 2009;15(20):2449-55.
-
19Laukens D, Peeters H, Marichal D, Vander Cruyssen B, Mielants H, Elewaut D. CARD15 gene polymorphisms in patients with spondyloarthropathies identify a specific phenotype previously related to Crohn's disease. Ann Rheum Dis 2005;64:930-35.
-
20Peeters H, Vander Cruyssen B, Laukens D, Coucke P, Marichal D, Van Den Berghe M, et al Radiological sacroiliitis, a hallmark of spondylitis, is linked with CARD15 gene polymorphisms in patients with Crohn's disease. Ann Rheum Dis 2004;63:1131-34.
-
21Dougados M, van der Linden S, Juhlin R, Huitfeldt, Amor B, Calin A, et al. The European Spondyloarthropathy Study Group preliminary criteria for the classification of spondyloarthropathy. Arthritis Rheum 1991;34:1218-27.
-
22Jones SD, Porter J, Garrett SL, Kennedy LG, Whitelock H, Calin A. A new scoring system for the Bath Ankylosing Spondylitis Metrology Index (BASMI). J Rheumatol 1995;22:1609.
-
23Doward LC, Spoorenberg A, Cook SA, Whalley D, Helliwell PS, Kay LJ, et al. Development of the ASQoL:a quality of life instrument specific to ankylosing spondylitis. Ann Rheum Dis 2003;62:20-6.
-
24Heuft-Dorenbosch L, Spoorenberg A, van Tubergen R, Landewé R, van der Tempel H, Mielants H, et al. Assessment of enthesitis in ankylosing spondylitis. Ann Rheum Dis 2003;62:127-32.
-
25Garrett S, Jenkinson T, Kennedy LG, Whitelock H, Gaisford P, Calin A. A new approach to defining disease status in ankylosing spondylitis:the Bath Ankylosing Spondylitis Disease Activity Index. J Rheumatol 1994;21:2286-91.
-
26Calin A, Garrett S, Whitelock H, Kennedy LG, O'Hea J, Malorie P, et al. A new approach to defining functional ability in ankylosing spondylitis:the development of the Bath Ankylosing Functional Index. J Rheumatol 1994;21:2281-5.
-
27Wanders AJ, Landewe RB, Spoorenberg A, Dougados M, van der Linden S, Mielants H, et al. What is the most appropriate radiologic scoring method for ankylosing spondylitis? A comparison of the available methods based on the Outcome Measures in Rheumatology Clinical Trials filter. Arthritis Rheum 2004;50:2622-32.
-
28Moll J, Wright V. New York clinical criteria for ankylosing spondylitis. Ann Rheum Dis 1973;32:354-63.
-
29Alamino R, Cocco J, Citera G, Arturi P, Mellado J, Sampaio-Barros PD, et al Differential Features Between Primary Ankylosing Spondylitis and Spondylitis Associated with Psoriasis and Inflammatory Bowel Disease. J Rheumatol 2011;38(8):1656-60.
-
30Al-Shamali MA, Kalaouib M, Pattyb I, Hasana F, Khajahb A, Al-Nakiba B. Ulcerative Colitis in Kuwait:A Review of 90 Cases. Digestion 2003;67:218-24.
-
31Lanna C, Ferrari M, Rocha S, Nascimento E, Carvalho M, Cunha A. A cross-sectional study of 130 Brazilian patients with Crohn's disease and ulcerative colitis:analysis of articular and ophthalmologic manifestations. Clin Rheumatol 2008;27:503-8.
-
32Goldfarb M, Leite N, Rubinstein J, Lederman R, Guimarães S, Mesquita M, et al. Manifestaçöes reumáticas na retocolite ulcerativa idiopática:estudo de 98 casos no HSE e revisäo da literatura. Rev Bras Reumatol. 1985;25(2):53-6.
-
33Souza MHLP, Troncon LEA, Rodrigues CM, Viana CFG, Onofre PHC, Monteiro RA, et al. Evolução da ocorrência (1980-1999) da doença de Crohn e da Retocolite Ulcerativa Idiopática e análise das suas características clínicas em um hospital universitário do sudeste do Brasil. Arq Gastroenterol. 2002;39(2):98-105.
-
34Salvarani C, Vlachonikolis I, Van der Heijde D, Fornaciari G, Macchioni P, Beltrami M, et al. Musculoskeletal Manifestations in a Population-based Cohort of Inflammatory Bowel Disease Patients. Scand J Gastroenterol. 2001;12:1307-13.
-
35Dekker-Saeys BJ, Meuwissen S, Van Den Berg-Loonen EM, De Haas W, Meijers KA, Tytgat G. Clinical characteristics and results of histocompatibility typing (HLA B27) in 50 patients with both ankylosing spondylitis and inflammatory bowel disease. Ann Rheum Dis. 1978;37:36-41.
-
36Dekker-Saeys BJ, Meuwissen S, Van Den Berg-Loonen EM, De Haas W, Meijers KA, Tytgat G. Prevalence of peripheral arthritis, sacroiliitis, and ankylosing spondylitis in patients suffering from inflammatory bowel disease. Ann Rheum Dis. 1978;37:33-35.
-
37Christodoulou D, Katsanos K, Kitsanou M, Stergiopouloul C, Hatzisl J, Tsianos E. Frequency of extraintestinal manifestations in patients with inflammatory bowel disease in Northwest Greece and review of the literature. Digest Liver Dis. 2002;34:781-6.
-
38Gallinaro AL, Ventura C, Sampaio-Barros PD, Gonçalves CR. Espondiloartrites:Análise de uma série brasileira comparada a uma grande casuística ibero-americana (estudo RESPONDIA). Rev Bras Reumatol. 2010;50(5):581-89.
-
39Tayel M, Soliman E, El Baz W, El Labaan A, Hamaad Y, Ahmed M. Registry of the clinical characteristics of spondyloarthritis in a cohort of Egyptian population. Rheumatol Int. 2011. Avaiable from http://www.springerlink.com/content/btv18k0768422704/fulltext.pdf
-
40De Vlan K, Mielants H, Cuvelier C, De Keyser F, Veys EM, De Vos M. Spondyloarthropathy is underestimated in Inflammatory Bowel Disease:Prevalence and HLA association. J Rheumatol. 2000;27(12):2860-65.
-
41Scarpa R, del Puente A, D'Arienzo A, di Girolamo C, della Valle G, Panarese A, et al. The arthritis of ulcerative colitis:clinical and genetic aspects. J Rheumatol. 1992;19(3):373-7.
-
42Podswiadek M, Punzi L, Stramare R, D'Incà R, Ferronato A, Lo Nigro A, et al. Prevalenza delle sacroileiti radiologiche clinicamente sintomatiche nelle malattie infiammatorie croniche intestinali. Reumatismo. 2004;50(2):110-13.
-
43Helliwell S, Hickling P, Wright V. Do the radiological changes of classic ankylosing spondylitis differ from the changes found in the spondylitis associated with inflammatory bowel disease, psoriasis, and reactive arthritis? Ann Rheum Dis. 1998;57:135-40.
-
44McEwen C, DiTata D, Lingg C, Porini A, Good A, Rankin T. Ankylosing spondylitis and spondylitis accompanying ulcerative colitis, regional enteritis, psoriasis and Reiter's disease. A comparative study. Arthritis Rheum. 1971;14(3):291-318.
-
45Mendoza J, Lana R, Taxonera C, Alba C, Izquierdo S, Diaz-Rublo M. Manifestaciones extraintestinales en la enfermedad inflamatoria intestinal:diferencias entre la enfermedad de Crohn y la colitis ulcerosa. Med Clin (Barc). 2005;125:297-300.
-
46Steer S, Jons H, Hibbert J, Kondeatis E, Vaughan R, Sanderson J, et al. Low back pain, sacroiliitis, and the relationship with HLA-B27 in Crohn's Disease. J Rheumatol. 2003;30(3):518-22.
-
47Scott WJ, Fishman E, Kuhlman J, Caskey C, O'Brien J, Walia G, et al. Computed tomography evaluation of the sacroiliac joints in Crohn disease. Radiologic/clinical correlation. Skeletal Radiol. 1990;19(3):207-10.
-
48Gravallese E, Kantrowitz F. Arthritic manifestations of inflammatory bowel disease. Am J Gastroenterol. 1988;83(7):703-9.
-
49McEniff N, Eustace S, McCarthy C, O'Malley M, O'Morain C, Hamilton S. Asymptomatic sacroiliitis in inflammatory bowel disease. Assessment by computed tomography. Clin Imaging. 1995;19(4):258.
-
50D'Incàa R, Podswiadekb M, Ferronatoa A, Punzib L, Salvagninic M, Sturnioloa G. Articular manifestations in inflammatory bowel disease patients:A prospective study. Digestive and Liver Disease. 2009;41:565-9.
-
51Haglund E, Bremander A, Petersson I, Strömbeck B, Bergman S. Prevalence of spondyloarthritis and its subtypes in southern Sweden. Ann Rheum Dis. 2011;70:943-48.
-
52Bonner G, Fakhri A, Vennamaneni S. A long-term cohort study of nonsteroidal anti-inflammatory drug use and disease activity in outpatients with inflammatory bowel disease. Inflamm Bowel Dis. 2004;10(6):751.
Enteropathic arthritis in Brazil: data from the brazilian registry of spondyloarthritis
Publication Dates
-
Publication in this collection
23 May 2014 -
Date of issue
Dec 2013
History
-
Received
02 June 2012 -
Accepted
04 Apr 2013