ABSTRACT
Background:
Systemic blockade of TNF-α in Rheumatoid arthritis with insulin resistance seems to produce more improvement in insulin sensitivity in normal weight patients with Rheumatoid arthritis than in obese patients with Rheumatoid arthritis, suggesting that systemic-inflammation and obesity are independent risk factors for insulin resistance in Rheumatoid arthritis patients.
Objectives:
To evaluate the insulin resistance in: normal weight patients with Rheumatoid arthritis, overweight patients with Rheumatoid arthritis, obese Rheumatoid arthritis patients, and matched control subjects with normal weight and obesity; and its association with major cytokines involved in the pathogenesis of the disease.
Methods:
Assessments included: body mass index, insulin resistance by Homeostasis Model Assessment, ELISA method, and enzymatic colorimetric assay.
Results:
Outstanding results from these studies include: (1) In Rheumatoid arthritis patients, insulin resistance was well correlated with body mass index, but not with levels of serum cytokines. In fact, levels of cytokines were similar in all Rheumatoid arthritis patients, regardless of being obese, overweight or normal weight (2) Insulin resistance was significantly higher in Rheumatoid arthritis with normal weight than in normal weight (3) No significant difference was observed between insulin resistances of Rheumatoid arthritis with obesity and obesity (4) As expected, levels of circulating cytokines were significantly higher in Rheumatoid arthritis patients than in obesity.
Conclusions:
Obesity appears to be a dominant condition above inflammation to produce IR in RA patients. The dissociation of the inflammation and obesity components to produce IR suggests the need of an independent therapeutic strategy in obese patients with RA.
Keywords:
Insulin resistance; Obesity; Rheumatoid arthritis; TNF-α
RESUMO
Introdução:
O bloqueio sistêmico do Fator de Necrose Tumoral-α (TNF-α) nos indivíduos com artrite reumatoide (AR) com resistência à insulina (RI) parece produzir mais melhoria na sensibilidade à insulina em pacientes com AR com peso normal do que em pacientes obesos com AR. Isso sugere que a inflamação sistêmica e a obesidade são fatores de risco independentes para a RI em pacientes com AR.
Objetivos:
Avaliar a resistência à insulina em pacientes com peso normal com AR (AR-PN), pacientes com sobrepeso com AR (AR-SP), pacientes com AR obesos (AR-OB) e indivíduos controle com peso normal (PN) e obesidade (OB) pareados; e a associação com as principais citocinas envolvidas na patogênese da doença.
Métodos:
As avaliações incluíram: índice de massa corporal (IMC), resistência à insulina com o modelo de avaliação da homeostase (Homa-IR), método Elisa e ensaio colorimétrico enzimático.
Resultados:
Os resultados marcantes do presente estudo incluíram: (1) Em pacientes com AR, a RI estava bem correlacionada com o Índice de Massa Corporal (quanto maior o IMC, maior a RI), mas não com os níveis séricos de citocinas. Na verdade, os níveis de citocinas eram semelhantes em todos os pacientes com AR, independentemente de serem obesos, com sobrepeso ou peso normal. (2) A RI foi significativamente maior no grupo AR-PN do que no grupo PN. (3) Não houve diferença estatisticamente significativa entre a RI de pacientes AR-OB e OB. (4) Como esperado, os níveis circulantes de citocinas foram significativamente maiores em pacientes com AR do que em OB.
Conclusões:
A obesidade parece ser uma condição mais importante do que a inflamação em produzir RI em pacientes com AR. A dissociação dos componentes da inflamação e da obesidade na produção de RI sugere a necessidade de uma estratégia terapêutica independente em pacientes obesos com AR.
Palavras-chave:
Resistência à insulina; Obesidade; Artrite reumatoide; TNF-α
Introduction
Rheumatoid arthritis (RA) is a chronic, systemic, inflammatory disorder of unknown etiology; manifested mostly by joint inflammation. This inflammatory process involves multiple factors. Lymphocytes produce cytokines such as Tumor Necrosis Factor-α (TNF-α), IL-6 and IL-1β, which results in recruitment of several other immune cells to the affected site. When uncontrolled, this may result in joint destruction and deformity.11 Wolfe F. The natural history of rheumatoid arthritis. J Rheumatol Suppl. 1996;44:13-22. Therefore, these incapacitating consequences fully justify the therapeutic use of drugs such as selective inhibitors of TNF-α, IL-6 and IL-1β, aimed at reducing structural damage.11 Wolfe F. The natural history of rheumatoid arthritis. J Rheumatol Suppl. 1996;44:13-22.
2 Bradley JR. TNF-mediated inflammatory disease. J Pathol. 2008;214:149-60.-33 Seriolo B, Ferrone C, Cutolo M. Longterm anti-tumor necrosis factor-alpha treatment in patients with refractory rheumatoid arthritis. J Rheumatol. 2008;35:355-7. These cytokines are mainly produced by macrophages, monocytes and T-cells, but they are also produced by different kinds of non-immune cells, including adipocytes, muscle cells and renal tubular cells.44 Gimeno RE, Klaman LD. Adipose tissue as an active endocrine organ: recent advances. Curr Opin Pharmacol. 2005;5:122-8.
5 Saghizadeh M, Ong JM, Garvey WT, Henry PR, Kern PA. The expression of TNF-α by human muscle. J Clin Invest. 1996;97:1111-6.-66 Maldonado-Cervantes MI, Galicia OG, Moreno-Jaime B, Zapata-Morales JR, Montoya-Contreras A, Bautista-Perez R, et al. Autocrine modulation of glucose transporter SGLT2 by IL-6 and TNF-α in LLC-PK1 cells. J Physiol Biochem. 2012;68:411-20. On the other hand, these pro-inflammatory cytokines are closely related with insulin resistance (IR), by definition IR is known as a diminished cellular response to insulin, moreover compensatory hyperinsulinemia is a clinical feature well-established of IR. The gold standard for evaluating IR is the euglycemic-hyperinsulinemic clamp, but this method is risky, invasive and requires medical intervention; however in many population studies like ours, IR is evaluated with the Homeostasis Model Assessment (HOMA-IR) which estimates the basal homeostasis through fasting levels of glucose and insulin and has a high correlation with the gold standard.77 Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9.
At the cellular level, insulin signaling is impaired in the main insulin-sensitive organs, particularly skeletal muscle, liver, heart and adipose tissue88 Olivares-Reyes JA, Arellano-Plancarte A, Castillo-Hernandez JR. Angiotensin II and the development of insulin resistance: implications for diabetes. Mol Cell Endocrinol. 2009;302:128-39.; this cellular phenomenon is strongly related to a great myriad of metabolic abnormalities as obesity, diabetes mellitus, hyperlipidemia, cardiovascular disease, hypertension, cancer, syndrome of polycystic ovarian and inflammatory disease. Increased serine phosphorylation of the insulin-receptor substrate (IRS-1and 2) by various stimuli including inflammatory cytokines is the principally molecular mechanism identified.88 Olivares-Reyes JA, Arellano-Plancarte A, Castillo-Hernandez JR. Angiotensin II and the development of insulin resistance: implications for diabetes. Mol Cell Endocrinol. 2009;302:128-39. Furthermore these cytokines have been shown to decrease the tyrosine kinase activity of the insulin receptor.99 Moller DE. Potential role of TNF-alpha in the pathogenesis of insulin resistance and type 2 diabetes. Trends Endocrinol Metab. 2000;11:212-7. Several studies provide evidence for TNF-α playing important roles in various aspects of the metabolic syndrome, including obesity-induced IR. Furthermore, it is known that patients with IR have high circulating levels of TNF-α.1010 Miyazaki Y, Pipek R, Mandarino LJ, DeFronzo RA. Tumor necrosis factor α and insulin resistance in obese type 2 diabetic patients. Int J Obes Relat Metab Disord. 2003;27:88-94.,1111 Olson NC, Callas PW, Hanley AJG, Festa A, Haffner SM, Wagenknecht LE, et al. Circulating levels of TNF-α are associated with impaired glucose tolerance, increased insulin resistance, and ethnicity: the Insulin Resistance Atherosclerosis Study. J Clin Endocrinol Metab. 2012;97:1032-40.
Obesity, a low-grade chronic inflammatory condition, has been considered an important risk factor to develop IR. Adipose tissue, particularly the visceral, is now recognized as the primary contributor to the IR syndrome.1212 Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity, and diabetes. Trends Immunol. 2004;25:4-7. TNF-α and IL-6, which are expressed and secreted by the human adipose tissue, show increased plasma levels in human obesity, which are reduced in obese subjects after weight loss. In fact, plasma levels of these cytokines are correlated with the body mass index (BMI). TNF-α has also been proposed as a link between obesity and IR.1212 Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity, and diabetes. Trends Immunol. 2004;25:4-7.,1313 Nieto-Vazquez I, Fernandez-Veledo S, Kramer DK, Vila-Bedmar R, Garcia-Guerra L, Lorenzo M. Insulin resistance associated to obesity: the link TNF-alpha. Arch Physiol Biochem. 2008;114:183-94. Indeed, IR and obesity are prevalent in RA patients.1414 Stavropoulos-Kalinoglou A, Metsios GS, Koutedakis Y, Kitas GD. Obesity in rheumatoid arthritis. Rheumatology. 2011;50:450-62.
Recent studies suggest that systemic TNF-α blockade (using infliximab, etanercept and adalimumab) and IL-6 receptor antagonist (using tocilizumab) may improve IR in patients with RA.33 Seriolo B, Ferrone C, Cutolo M. Longterm anti-tumor necrosis factor-alpha treatment in patients with refractory rheumatoid arthritis. J Rheumatol. 2008;35:355-7.,1515 Smolen JS, Martinez-Avila JC, Aletaha D. Tocilizumab inhibits progression of joint damage in rheumatoid arthritis irrespective of its anti-inflammatory effects: disassociation of the link between inflammation and destruction. Ann Rheum Dis. 2012;71:687-93. Nonetheless, it has been reported that beneficial effect on insulin sensitivity is mainly observed in normal weight but not in obese RA patients,1616 Stavropoulos-Kalinoglou A, Metsios GS, Panoulas VF, Nightingale P, Koutedakis Y, Kitas GD. Anti-tumour necrosis factor alpha therapy improves insulin sensitivity in normal-weight but not in obese patients with rheumatoid arthritis. Arthritis Res Ther. 2012;14:R160. most likely because anti-inflammatory therapy acts upon the “inflammatory component” (pro-inflammatory cytokines) rather than upon the obesity components in these patients.
Hence, the present study aims at evaluating the relationship between IR and plasmatic concentrations of TNF-α, IL-6 and IL-1 in RA patients with and without obesity to evaluate the obesity role as a risk factor for IR in RA patients.
Methods
Study participants
This study was conducted under the guidelines of the declaration of Helsinki of the World Medical Association, which establishes the ethical principles for medical research involving humans. All participants gave informed consent. We recruited 59 adult subjects among 19-70 years old.
RA patients include 27 female fulfilling the American College of Rheumatology 1987 criteria and with active disease admitted to the hospital General and the Mexican Institute of Social Security of Rioverde city, state of San Luis Potosi; Mexico. Total RA patients (RA w/wo OB) were divided into 3 groups: 7 RA patients with normal weight (RA NW), 7 RA patients with overweight (RA OW), and 13 RA patients with obesity (RA OB); RA groups were matched by age, gender and years after diagnosis even though they were under treatment with methotrexate (MTX), glucocorticoids (GCs), and non-steroidal anti-inflammatory drugs (NSAIDs). Inclusion criteria for RA patients were confirmed diagnosis of active RA (assessed by The Disease Activity Score-28 Joints, DAS28 > 3.2), never having selective biologic treatment anti-TNF-α or anti-IL-6, nor anti-IL-1β. Exclusion criteria were patients with a history of allergies, infections, diabetes or any other systemic illness. RA w/wo OB and OB groups were similar in age and gender.
Sixteen normal weight subjects without RA (NW) were include as negative control for IR, and 16 non-diabetic obese women without RA (OB) as positive control for IR.
Anthropometrics and clinical data
Body weight was obtained by using a weighing scale with participants wearing light clothing and no footwear. Height was measured by using a stadiometer, with no footwear. BMI was calculated by dividing the subject's weight in kilograms by the squared height in squared meters. The BMI classifications correspond to the one proposed by the World Health Organization (WHO) and were as follows: normal weight range 18.5-24.9, overweight 25.0-29.9 and obese ≥30.0 (kg/m2). Waist circumference was measured using an anthropometric tape measure. The measurement was taken at the smallest point of circumference between the iliac crest and the rib cage. Also, arterial blood pressure was obtained by indirect method using a manual cuff and sphygmomanometer.
Analyses of samples
Venous blood samples were collected after an overnight fast (8 h) between 7:00 a.m. and 9:00 a.m. by trained personnel using identical, standardized protocols, into non-treated vacutainers. Serum was separated from whole blood by centrifugation (10 min at 3000 rpm) and stored at −20 °C for later analysis. The serum was used to determine the following parameters: glucose, insulin, triglycerides (TG), total cholesterol (TC), HDL-c, TNF-α, IL-6 and IL-1β. Serum glucose was measured by glucose oxidase method, a standard enzymatic colorimetric assay (Spin react S.A. Spain). Serum TC, high-density lipoprotein cholesterol (HDL-C) and TG were measured by enzymatic colorimetric assay using a semiautomatic chemistry analyser (Spin lab, Spain). Low-density lipoprotein cholesterol (LDL-C) was calculated according to the Friedewald formula. Serum insulin was determined by chemiluminescent micro-particle immunoassay (IMMULITE 1000 system). The HOMA-IR was used to evaluate IR in patients and controls. [Fasting insulin (µIU/mL) × fasting glucose (mg/dL)/405]. It established the presence of IR to study subjects when HOMA-IR was >2.5.77 Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9. Serums TNF-α, IL-6 and IL-1β were measured by ELISA method. The ELISA kits were purchased from Invitrogen Corporation and the protocol used in this study was per manufacturer's instructions. The color produced by the enzymatic reaction was measured at 450 nm on an Awareness Stat Fax 303 Plate Reader.
Statistical analysis
All data were expressed as mean ± SEM. Shapiro Wilk test were assessed for normality. The comparison of means between groups was made using: (1) one-way ANOVA with Tukey post-test for parametric data and the Kruskal-Wallis test with Dunns post-test when data were non-parametric for the analysis of the three main groups NW, OB and RA w/wo OB. (2) unpaired t test for analysis between OB vs. RA OB; RA NW vs. RA OB and RA NW vs. NW. The association of two variables was measured with Spearman's r for nonparametric data. Statistical significance was set at p < 0.05.
Results
Demographic and clinical data
A total of 59 consecutive participants were enrolled. The clinical and demographic characteristics were summarized in Table 1. There was no difference in the following parameters: body weight, BMI and waist circumference among normal weight groups (NW vs. RA NW), or between obese groups (OB vs. RA OB). As expected, there were statistical significant differences between RA NW, RA OW and RA OB groups in these parameters (p = 0.0001). Insulin levels were significantly higher in RA NW compared against NW (p = 0.003). On the other hand, the RA NW had significantly lower insulin values than RA OB (p = 0.03); insulin levels between OB and RA OB were not significantly different. The serum TG levels were significantly higher in RA NW vs. NW (p = 0.02), but not among RA subgroups or between RA OB vs. OB. LDL-C/HDL-C index was higher in RA NW vs. NW (p = 0.001), but not among RA subgroups or between RA OB vs. OB. Of the 27 patients with RA, 44% were under treatment with MTX; a little more than 50% with GCs and the most frequent treatment were the NSAIDs (66%).
The IR in RA patients is principally associated with BMI but not to serum levels of TNF-α
Using the homeostatic model (HOMA-IR), the IR status was assessed in 59 subjects that integrated the three main study groups and a HOMA-IR value ≥2.5 was accepted to define the presence of IR.77 Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9. The results show that RA w/wo OB and OB groups have similar values of HOMA-IR (4.32 ± 0.72 and 4.86 ± 0.56 respectively), about 4.5-5 times higher than NW (0.97 ± 0.13) (Fig. 1A).
BMI correlated with HOMA-IR in RA patients. Data are expressed as mean ± SEM. (A) The Kruskal Wallis test with Dunnet's post-test was applied. (B) Unpaired t test was made. (C) Positive correlation between BMI and HOMA-IR in RA patients was found, Spearman correlation test was made for this data analysis. Statistical significance was set at p < 0.05.Insulin resistance was determined by HOMA IR (homeostasis model assessment), BMI, body mass index. The BMI classifications correspond to the one proposed by the World Health Organization (WHO) and were as follows: normal weight range 18.5-24.9, overweight 25.0-29.9 and obese ≥30.0 (kg/m2); NW, subjects normal weight (n = 16); OB, subjects with obesity (n = 16); RA, patients with Rheumatoid arthritis; RA w/wo OB, total RA patients with or without obesity (n = 27); RA NW, RA patients with normal weight (n = 7); RA OW, RA patients with overweight (n = 7); RA OB, RA patients with obesity (n = 13).* vs. NW; Φ vs. RA NW.
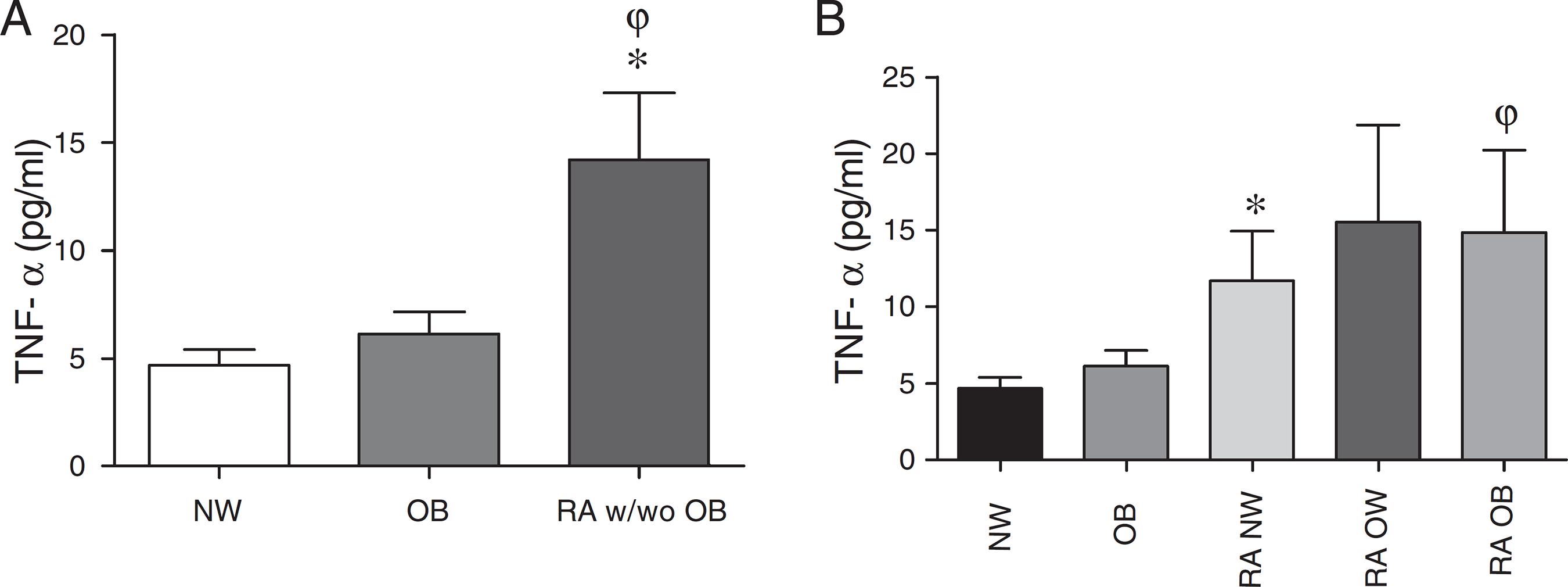
The HOMA-IR value increased, as BMI was higher: RA NW (2.39 ± 0.61), RA OW (3.15 ± 0.64) and RA OB (6.0 ± 1.31, p = 0.01 vs. RA NW) (Fig. 1B). Interestingly, RA NW showed a significantly higher HOMA-IR than NW (2.39 ± 0.61 vs. 0.97 ± 0.13; p = 0.008) (Fig. 1B). As expected, the correlation analysis showed a strong association between BMI and HOMA-IR (Spearman r = 0.6, p = 0.0008) in RA patients (Fig. 1C). Additionally, serum TNF-α levels were significantly elevated in RA w/wo OB (14.22 ± 3.08 pg/mL) compared to NW and OB (4.66 ± 0.74 pg/mL and 6.12 ± 1.01 pg/mL; p = 0.01 and p = 0.05 respectively), around 3 and 2 times higher respectively (Fig. 2A). Furthermore, it was found that serum TNF-α levels of RA OB were significantly higher than OB (14.87 ± 5.36 vs. 6.12 ± 1.0 pg/mL; p = 0.02). Also, RA NW showed higher serum TNF-α levels than NW (11.7 ± 3.22 vs. 4.66 ± 0.74 pg/mL; p = 0.007) (Fig. 2B). Additionally, the serum TNF-α levels did not correlate neither with BMI nor with HOMA-IR by Spearman's r test.
Enhanced serum amounts of TNF-α are dissociated of BMI in RA patients. Data are expressed as mean ± SEM; to compare the means dispersion were used: (A) Kruskal-Wallis test with Dunns's post-test for no-parametric data. (B) Comparisons RA NW vs. NW and RA OB vs. OB were made by unpaired t test. Also, statistical differences between RA subgroups were not found. Statistical significance was set at p < 0.05.The BMI classifications correspond to the one proposed by the World Health Organization (WHO) and were as follows: normal weight range 18.5-24.9, overweight 25.0-29.9 and obese ≥30.0 (kg/m2); NW, subjects normal weight (n = 16); OB, subjects with obesity (n = 16); RA, patients with Rheumatoid arthritis; RA w/wo OB, total RA patients with or without obesity (n = 27); RA NW, RA patients with normal weight (n = 7); RA OW, RA patients with overweight (n = 7); RA OB, RA patients with obesity (n = 13).* vs. NW; φ vs. OB.
Serum levels of IL-6 are increased in RA patients but are not associated with HOMA-IR
The evaluation of serum levels of IL-6 clearly shows that they were significantly higher in RA w/wo OB (12.25 ± 4.55 pg/mL) compared with NW and OB (0.81 ± 0.52 and 1.15 ± 0.48 pg/mL; p < 0.001 and p < 0.05 respectively), almost 15-10 times higher than NW and OB respectively (Fig. 3A). Serum IL-6 levels in RA NW were significantly higher than in NW (17.27 ± 10.47 vs. 0.81 ± 0.52 pg/mL; p = 0.01) and IL-6 levels in RA OB were significantly higher than in OB (9.30 ± 5.85 vs. 1.15 ± 0.48 pg/mL; p = 0.03) (Fig. 3B). Interestingly, in RA patients, we observed a tendency - though not significant-regard to the higher BMI, the lower IL-6 levels. Correlation analysis between IL-6 and BMI, was not significant (Spearman r = −0.1540, p = 0.45; data not shown). Also, correlation analysis between IL-6 levels and HOMA-IR was not significant (Spearman r = −0.21, p = 0.28; data not shown).
Increased serum levels of IL-6 were not associated to BMI in RA patients. Data are expressed as mean ± SEM. (A) Increased serum levels of IL-6 in RA patients were found; Kruskal-Wallis test with Dunns's post-test was applied. (B) Comparisons RA NW vs. NW and RA OB vs. OB were made by unpaired t test. Also, statistical differences between RA subgroups were not found. Statistical significance was set at p < 0.05.The BMI classifications correspond to the one proposed by the World Health Organization (WHO) and were as follows: normal weight range 18.5-24.9, overweight 25.0-29.9 and obese ≥30.0 (kg/m2); NW, subjects normal weight (n = 16); OB, subjects with obesity (n = 16); RA, patients with Rheumatoid arthritis; RA w/wo OB, total RA patients with or without obesity (n = 27); RA NW, RA patients with normal weight (n = 7); RA OW, RA patients with over-weight (n = 7); RA OB, RA patients with obesity (n = 13).* vs. control; φ vs. OB.
Evaluation of plasma levels of IL-1β
Plasma levels of IL-1β were also evaluated in RA NW, RA OW and RA OB (1.52 ± 0.34, 1.72 ± 0.18, 1.51 ± 0.20 pg/mL respectively), these were similar to those found in OB and NW (1.74 ± 0.16, 1.56 ± 0.16 pg/mL respectively) (data not shown). All subgroups of RA showed no differences between them in IL-1β levels. No correlation was found between IL-1β levels and HOMA-IR in RA patients (data not shown).
Discussion
The purpose of this study was to evaluate IR in RA patients with and without obesity and its association with major cytokines involved in the pathogenesis of the disease. Our study indicates that obesity is the main determinant of IR in RA. Furthermore, the degree of IR observed in obese subjects (RA OB or OB) is not attainable even with high serum concentrations of the cytokines involved in the inflammatory process (RA NW). These conclusions are based on the following observations: (1) RA NW, RA OW and RA OB have similar levels of pro-inflammatory cytokines and these are significantly higher than in OB (Figs. 2B and 3B); (2) HOMA-IR between OB and RA OB were not different (Fig. 1B); (3) Despite similar high levels of pro-inflammatory cytokines among RA OB and RA NW patients, this latter had significantly lower HOMA-IR (Fig. 1B); (4) HOMA-IR was significantly higher in RA NW than in NW (Fig. 1B); (5) HOMA-IR was correlated with BMI but not with pro-inflammatory cytokine levels in RA (Fig. 1C).
We selected 27 female patients with active RA with and without obesity of which only 12 patients (44%) were treated with MTX, in doses of 7.5-10 mg per week. No patient has used biologic DMARDs therapy in our study (Table 1). MTX is a folic acid antagonist drug, whose main effect is thought to come from the inhibition of enzymes involved in purine synthesis leading to the accumulation of adenosine and thus inhibiting the T cell activation.1717 Kumar P, Banik S. Pharmacotherapy options in rheumatoid arthritis. Clin Med Insights Arthritis Musculoskelet Disord. 2013;6:35-43. MTX apparently does not affect the TNF-α levels in RA but IL-6 and IL-1β levels are indeed affected.1818 Nishina N, Kaneko Y, Kameda H, Kuwana M, Takeuchi T. Reduction of plasma IL-6 but not TNF-α by methotrexate in patients with early rheumatoid arthritis: a potential biomarker for radiographic progression. Clin Rheumatol. 2013;32:1661-6.,1919 Barrera P, Haagsma CJ, Boerbooms AM, Van-Riel PLCM, Borm GF, Van de Putte LBA, et al. Effect of methotrexate alone or in combination with sulphasalazine on the production and circulating concentrations of cytokines and their antagonists. Longitudinal evaluation in patients with rheumatoid arthritis. Br J Rheumatol. 1995;34:747-55. We observed that the main treatment in RA patients included in our study was diclofenac, a non-selective cyclooxygenase inhibitor (66%) followed by corticosteroids (≈51%). Recent studies show that treatment with high doses of intraperitoneal diclofenac (500 µg/mL) does not affect levels of serum TNF-α and IL-6 in an animal model of fever.2020 Greis A, Murgott J, Rafalzik S, Gerstberger R, Hübschle T, Roth J. Characterization of the febrile response induced by fibroblast-stimulating lipopeptide-1 in guinea pigs. Am J Physiol Regul Integr Comp Physiol. 2007;293:R152-61. Additionally, others have shown that NSAIDs have a slight effect decreasing IL-1β levels,2121 Pelletier JP, Cloutier JM, Martel-Pelletier J. In vitro effects of NSAIDs and corticosteroids on the synthesis and secretion of interleukin 1 by human osteoarthritic synovial membranes. Agents Actions. 1993;39:181-93. while circulating and local levels of IL-6 remain unaffected.2222 Roth J, Hübschle T, Pehl U, Ross G, Gerstberger R. Influence of systemic treatment with cyclooxygenase inhibitors on lipopolysaccharide-induced fever and circulating levels of cytokines and cortisol in guinea-pigs. Pflugers Arch. 2002;443:411-7. On the other hand, treatment with low doses of GCs (<7.5 mg of prednisone), as received by some RA patients in our study does not seem to affect the levels of circulating TNF-α or IL-6,2323 Penesová A, Rádiková Z, Vlček M, Kerlik J, Lukáč J, Rovenský J, et al. Chronic inflammation and low-dose glucocorticoid effects on glucose metabolism in premenopausal females with rheumatoid arthritis free of conventional metabolic risk factors. Physiol Res. 2013;62:75-83. but IL-1β levels are modified.2424 Uehara A, Kohda H, Sekiya C, Takasugi Y, Namiki M. Inhibition of interleukin-1 beta release from cultured human peripheral blood mononuclear cells by prednisolone. Experientia. 1989;45:166-7. The basal TNF-α amounts in our patients were similar to those found by Charles and co-workers in RA patients (14.21 ± 3.08 vs. 15.5 pg/mL)2525 Charles P, Elliott MJ, Davis D, Potter A, Kalden JR, Antoni C, et al. Regulation of cytokines, cytokine inhibitors, and acute-phase proteins following anti-TNF-alpha therapy in rheumatoid arthritis. J Immunol. 1999;163:1521-8. and by Penesová and co-workers in lean patients treated with low-doses of prednisone or equivalent (11.70 ± 3.22 vs. 13.6 ± 53.6 pg/mL).2323 Penesová A, Rádiková Z, Vlček M, Kerlik J, Lukáč J, Rovenský J, et al. Chronic inflammation and low-dose glucocorticoid effects on glucose metabolism in premenopausal females with rheumatoid arthritis free of conventional metabolic risk factors. Physiol Res. 2013;62:75-83. Hence, it seems that treatments received by our RA patients did not have a significant influence on circulating levels of TNF-α and IL-6.
Obesity, IR and inflammation are closely related. In fact the pro-inflammatory cytokines are often elevated in subjects with IR, a “hallmark” of the metabolic syndrome (MS), as well as chronic inflammation.22 Bradley JR. TNF-mediated inflammatory disease. J Pathol. 2008;214:149-60.,1111 Olson NC, Callas PW, Hanley AJG, Festa A, Haffner SM, Wagenknecht LE, et al. Circulating levels of TNF-α are associated with impaired glucose tolerance, increased insulin resistance, and ethnicity: the Insulin Resistance Atherosclerosis Study. J Clin Endocrinol Metab. 2012;97:1032-40. Some authors agree that TNF-α, IL-6 and IL-1 promote IR; it has even been proposed that TNF-α acts as the principal link between obesity and IR.1212 Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity, and diabetes. Trends Immunol. 2004;25:4-7.,1313 Nieto-Vazquez I, Fernandez-Veledo S, Kramer DK, Vila-Bedmar R, Garcia-Guerra L, Lorenzo M. Insulin resistance associated to obesity: the link TNF-alpha. Arch Physiol Biochem. 2008;114:183-94. At this point, it is worth mentioning that we did not observe a significant difference in TNF-α and IL-6 levels between NW and OB groups (Figs. 2 and 3, respectively), even though there is a tendency, as expected, for these levels to be higher in the OB group; this is discussed below. Furthermore, observational studies have shown that RA is associated with an increased prevalence of the MS and inflammatory markers.2626 Rostom S, Mengat M, Lahlou R, Hari A, Bahiri R, Hajjaj-Hassouni N. Metabolic syndrome in rheumatoid arthritis: case control study. BMC Musculoskelet Disord. 2013;14:147. additionally, increased HOMA-IR has been found in RA patients.2727 Chung CP, Oeser A, Solus JF, Gebretsadik T, Shintani A, Avalos I, et al. Inflammation associated insulin resistance: differential effects in rheumatoid arthritis and systemic lupus erythematosus define potential mechanisms. Arthritis Rheum. 2008;58:2105-12.
Although the role of pro-inflammatory cytokines in the pathogenesis of RA is clear, as evidenced by the beneficial damage-preventing effects of anti-rheumatic agents as etanercept and infliximab (anti-TNF-α agents), tocilizumab (IL-6 R blocker) and anakinra (recombinant human IL-1 receptor antagonist),33 Seriolo B, Ferrone C, Cutolo M. Longterm anti-tumor necrosis factor-alpha treatment in patients with refractory rheumatoid arthritis. J Rheumatol. 2008;35:355-7.,1717 Kumar P, Banik S. Pharmacotherapy options in rheumatoid arthritis. Clin Med Insights Arthritis Musculoskelet Disord. 2013;6:35-43.,2828 Scher JU. Monotherapy in rheumatoid arthritis. Bull Hosp Jt Dis. 2013;71:204-7.,2929 Cohen S, Hurd E, Cush J, Schiff M, Weinblatt ME, Moreland LW, et al. Treatment of Rheumatoid Arthritis with Anakinra, a recombinant human interleukin-1 receptor antagonist, in combination with methotrexate results of a twenty-four-week, multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2002;46:614-24. their metabolic roles are still unclear. For example: inhibition of TNF-α results in improved insulin sensitivity in RA patients,33 Seriolo B, Ferrone C, Cutolo M. Longterm anti-tumor necrosis factor-alpha treatment in patients with refractory rheumatoid arthritis. J Rheumatol. 2008;35:355-7.,3030 Seriolo B, Paolino S, Ferrone C, Cutolo M. Effects of etanercept or infliximab treatment on lipid profile and insulin resistance in patients with refractory rheumatoid arthritis. Clin Rheumatol. 2007;26:1799-800.
31 Lai-Shan T, Tomlinson B, Chu TT, Li TK, Li EK. Impact of TNF inhibition on insulin resistance and lipids levels in patients with rheumatoid arthritis. Clin Rheumatol. 2007;26:1495-8.-3232 Stagakis I, Bertsias G, Karvounaris S, Kavousanaki M, Virla D, Raptopoulou A, et al. Anti-tumor necrosis factor therapy improves insulin resistance, beta cell function and insulin signaling in active rheumatoid arthritis patients with high insulin resistance. Arthritis Res Ther. 2013;14:1-11. this suggests that TNF-α plays an important role in the development of IR in RA patients, this is consistent with a similar role of TNF-α in IR development in the cases of obesity and MS.1010 Miyazaki Y, Pipek R, Mandarino LJ, DeFronzo RA. Tumor necrosis factor α and insulin resistance in obese type 2 diabetic patients. Int J Obes Relat Metab Disord. 2003;27:88-94.,1111 Olson NC, Callas PW, Hanley AJG, Festa A, Haffner SM, Wagenknecht LE, et al. Circulating levels of TNF-α are associated with impaired glucose tolerance, increased insulin resistance, and ethnicity: the Insulin Resistance Atherosclerosis Study. J Clin Endocrinol Metab. 2012;97:1032-40. In contrast, however, recent studies cast doubt on the importance of circulating TNF-α in IR development. For example a recent study shows that 1 year of systemic blockade of TNF-α in a group of sixteen RA patients did not have a significant impact on IR status.3333 Ferraz-Amaro I, Arce-Franco M, Muñiz J, López-Fernández J, Hernández-Hernández V, Franco A, et al. Systemic blockade of TNF-α does not improve insulin resistance in humans. Horm Metab Res. 2011;43:801-8. The same was observed in 56 MS patients treated with etanercept for 4 weeks.3434 Bernstein LE, Berry J, Kim S, Canavan B, Grinspoon SK. Effects of etanercept in patients with the metabolic syndrome. Arch Intern Med. 2006;166:902-8. The results of the present work may help to reconcile these contrasting reports, since comparison of RA NW with NW suggests that TNF-α may play a modest role - compared to obesity - in IR development in RA patients, but other obesity-linked factors are more crucial in the determination of IR. Therefore, these additional factors should be taken into account, and may explain the discrepancies among different reports in regard to IR in RA patients.
In this study we evaluated the IR by HOMA-IR in a group of RA patients with and without obesity. We found increased HOMA-IR values in RA OB, similar to the values of the OB group (Fig. 1B). Nonetheless, the comparison of serum TNF-α and IL-6 levels between these two groups was significantly higher in the RA OB (Figs. 2B and 3B). This first observation seems to dissociate the relationship between inflammation and IR. In support of this latter came the following observation: the group of RA NW showed lower HOMA-IR than the RA OB (Fig. 1B), even though both groups had similar high levels of TNF-α and IL-6 (Figs. 2B and 3B). This strongly suggests that high circulating levels of pro-inflammatory cytokines are not necessarily associated with a high degree of IR in RA patients. Indeed we found no correlation between circulating levels of TNF-α and IL-6 vs. HOMA-IR (data not shown), but BMI does correlate with HOMA-IR in RA (Fig. 1C). This is consistent with the findings in the recent study of Penesová et al. where they analyzed the relationship between the inflammatory component and glucose metabolism in a group of RA patients free of metabolic risk factors such as obesity or endocrine disturbances, which may overlap with the effect of inflammation on insulin sensitivity; no relationship was found between high circulating pro-inflammatory cytokines and metabolic parameters.2323 Penesová A, Rádiková Z, Vlček M, Kerlik J, Lukáč J, Rovenský J, et al. Chronic inflammation and low-dose glucocorticoid effects on glucose metabolism in premenopausal females with rheumatoid arthritis free of conventional metabolic risk factors. Physiol Res. 2013;62:75-83. It is likely that the circulating inflammatory component is not the main determinant of IR in RA.3535 Altomonte J, Harbaran S, Richter A, Dong H. Fat depot specific expression of adiponectin is impaired in Zucker fatty rats. Metabolism. 2003;52:958-63. Indeed, although in our study we found that the value of HOMA-IR and serum levels of TNF-α and IL-6 were significantly higher in RA NW than NW (both groups were free of traditional metabolic factor risks), HOMA-IR was significantly higher in RA OB compared with RA NW in spite of having similar high inflammatory cytokine levels. This indicates that IR determination in RA patients could have two independent components: inflammation and obesity. Moreover, obesity plays a main role above inflammation to produce IR. In support of this, a study showed that beneficial effects of anti-TNF-α therapy in regard to insulin sensitivity improvement can be observed only in normal weight RA patients with IR but not in obese RA patients with IR, despite treatment reduced the inflammatory activity of the disease in the same extent in all RA patients.1616 Stavropoulos-Kalinoglou A, Metsios GS, Panoulas VF, Nightingale P, Koutedakis Y, Kitas GD. Anti-tumour necrosis factor alpha therapy improves insulin sensitivity in normal-weight but not in obese patients with rheumatoid arthritis. Arthritis Res Ther. 2012;14:R160. Again, this can be explained because, the systemic blockade of TNF-α in RA patients has a greater impact on IR associated to the inflammatory component (pro-inflammatory cytokines), but not on the obesity components. Many other molecules named adipokines, such as adiponectin, resistin, leptin, and retinol binding protein 4 (RBP4), which are produced by fat tissue, are related to IR induced by obesity. They mediate the regulation of multiple organs and tissues such as the skeletal muscle, the cardiovascular system and the pancreas.3636 Romacho T, Elsen M, Röhrborn D, Eckel J. Adipose tissue and its role in organ crosstalk. Acta Physiol. 2014;210:733-53.,3737 Fang P, Shi M, Yu M, Guo L, Bo P, Zhang Z. Endogenous peptides as risk markers to assess the development of insulin resistance. Peptides. 2014;51:9-14. Interestingly and contrary to other reports, we did not find increased serum levels of pro-inflammatory cytokines (TNF-α and IL-6) (Fig. 3A) in the OB group, although strong IR was found in the OB group in comparison with the NW. It cannot be ruled out that the effect of pro-inflammatory cytokines would be predominantly local rather than systemic to modulate other indirect effects in adipose tissue.3838 Arner P. The adipocyte in insulin resistance: key molecules and the impact of the thiazolidinediones. Trends Endocrinol Metab. 2003;14:137-45.,3939 Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumour necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95:2409-15. For example, TNF-α stimulates the expression of mediators in fat cells, such as FFAs (free fatty acids) and leptin, which might induce IR in other organs.4040 Sethi JK, Hotamisligil GS. The role of TNF-α in adipocyte metabolism. Semin Cell Dev Biol. 1999;10:19-29. Particularly, the availability and utilization of FFAs is widely accepted as an indirect mechanism that contributes to the development of IR in skeletal muscle.4141 Kraegen EW, Cooney GJ. Free fatty acids and skeletal muscle insulin resistance. Curr Opin Lipidol. 2008;19:235-41.
With regard to IL-6, a pleiotropic cytokine with a wide range of biological activities with a pivotal role in the physiopathology of RA which is found in abundance in the synovial fluid and serum of patients with RA,4242 Srinivasan S, Choy EH. The role of Interleukin 6 in the pathophysiology of rheumatoid arthritis. Ther Adv Musculoskelet Dis. 2010;2:247-56. this is consistent with our findings, since all RA groups showed elevated levels of IL-6 in comparison with NW (Fig. 3A). Serum levels of IL-6 in our patients were similar to those found in other studies.1818 Nishina N, Kaneko Y, Kameda H, Kuwana M, Takeuchi T. Reduction of plasma IL-6 but not TNF-α by methotrexate in patients with early rheumatoid arthritis: a potential biomarker for radiographic progression. Clin Rheumatol. 2013;32:1661-6.,2323 Penesová A, Rádiková Z, Vlček M, Kerlik J, Lukáč J, Rovenský J, et al. Chronic inflammation and low-dose glucocorticoid effects on glucose metabolism in premenopausal females with rheumatoid arthritis free of conventional metabolic risk factors. Physiol Res. 2013;62:75-83. However, unlike other reports indicating a positive correlation between IL-6 levels and the degree of obesity,4343 Khaodhiar L, Ling PR, Blackburn GL, Bistrian BR. Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN. 2004;28:410-5. we found that the levels of TNF-α and IL-6 in the OB group were not significantly increased in comparison with the NW group (Fig. 3A), even though a tendency for the levels to be modestly higher in OB is present. In fact, this lack of significance has also been reported by other research groups when measuring these cytokines in blood,3939 Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumour necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95:2409-15. and it is argued that it is at tissue level where higher levels are usually found in the obese, while serum levels may remain in some cases without noticeable differences between NW and OB. Over the last decade, it has been reported, that IL-6 has dual effects on metabolic disorders and the control of body weight.4444 Wallenius K, Wallenius V, Sunter D, Dickson SL, Jansson JO. Intracerebroventricular interleukin-6 treatment decreases body fat in rats. Biochem Biophys Res Commun. 2002;293:560-5. We observed an interesting tendency-though not reaching significance levels - in regard to the higher the BMI the lower the serum levels of IL-6 in RA patients. Evidence by Tekaya et al. and van der Helm-van Mil et al. showed that obesity and BMI have protective effects on the amount of joint destruction, disease progression4545 Tekaya R, Sahli H, Zribi S, Mahmoud I, Ben Hadj Yahia C, Abdelmoula L, et al. Obesity has a protective effect on radiographic joint damage in rheumatoid arthritis. Tunis Med. 2011;89:462-5.,4646 van der Helm-van Mil AH, van der Kooij SM, Allaart CF, Toes RE, Huizinga TW. A high body mass index has a protective effect on the amount of joint destruction in small joints in early rheumatoid arthritis. Ann Rheum Dis. 2008;67:769-74. and disease severity (a high BMI is associated with a less severe disease outcome in anti-CCP-positive patients with RA). This protective effect of obesity could be mediated by a decrease in IL-6 in obese patients with RA.4747 Kaufmann J, Kielstein V, Kilian S, Stein G, Hein G. Relation between body mass index and radiological progression in patients with rheumatoid arthritis. J Rheumatol. 2003;30:2350-5. A study conducted in 2009 by T. Ruge and co-workers found that IL-6 correlated inversely with BMI in patients with hyperglycaemia.4848 Ruge T, Lockton JA, Renstrom F, Lystig T, Sukonina V, Svensson MK, et al. Acute hyperinsulinemia raises plasma interleukin-6 in both non diabetic and type 2 diabetes mellitus subjects, and this effect is inversely associated with body mass index. Metabolism. 2009;58:860-6. This could explain the tendency to inverse correlation between BMI and IL-6 levels that we observed in RA patients. Limitations in our study regarding sample size prevent us from further exploring IL-6levels and BMI in these patients; we need to repeat this approach with a greater sample. In general, more studies are necessary to clarify the role of IL-6 in obese patients with RA.
On the other hand, IL-1β is a potent inflammatory mediator in RA, reported as cytokine actively involved in the progression of the disease by activation of osteoclasts in the joints. Although IL-1β plays a key role, the serum level IL-1β was almost undetectable in our study. It is well acknowledged that this cytokine is present in the joints in RA, but it is difficult to measure in serum.2525 Charles P, Elliott MJ, Davis D, Potter A, Kalden JR, Antoni C, et al. Regulation of cytokines, cytokine inhibitors, and acute-phase proteins following anti-TNF-alpha therapy in rheumatoid arthritis. J Immunol. 1999;163:1521-8. Besides, as we mentioned above, the treatment used by our patients is likely to decrease IL-1β levels. Therefore, this could explain the very low levels of this cytokine in our patients (data not shown). Plasma levels of IL-1β have been shown to decrease in patients treated with MTX and prednisolone.1919 Barrera P, Haagsma CJ, Boerbooms AM, Van-Riel PLCM, Borm GF, Van de Putte LBA, et al. Effect of methotrexate alone or in combination with sulphasalazine on the production and circulating concentrations of cytokines and their antagonists. Longitudinal evaluation in patients with rheumatoid arthritis. Br J Rheumatol. 1995;34:747-55.,2424 Uehara A, Kohda H, Sekiya C, Takasugi Y, Namiki M. Inhibition of interleukin-1 beta release from cultured human peripheral blood mononuclear cells by prednisolone. Experientia. 1989;45:166-7. Nevertheless, there is evidence that therapy with GCs such as dexamethasone destabilizes the mRNA of IL-1α and IL-1β in a dose dependent manner in human monocytes by two mechanisms: (1) by inhibiting transcription of IL-1β gene and (2) by decreasing the stability of mRNA IL-1β,4949 Lee SW, Tsou AP, Chan H, Thomas J, Petrie K, Eugui EM, et al. Glucocorticoids selectively inhibit the transcription of the interleukin 1β gene and decrease the stability of interleukin 1β mRNA. Immunology. 1988;85:1204-8. reducing the plasma IL-1β concentration on animal models and production in primary cultures of human adipocytes.5050 Zhang HH, Kumar S, Barnett AH, Eggo MC. Dexamethasone inhibits tumor necrosis factor-α induced apoptosis and interleukin-1β release in human subcutaneous adipocytes and preadipocytes. J Clin Endocrinol Metab. 2001;86:2817-25. Serum levels of IL-1β do not correlate with HOMA-IR (p = 0.0853) in this study (data not shown).
The sample size is the main limitation of our study. We had a limited number of individuals that fulfilled our inclusion criteria. However, similar published studies have also shown the same limitations.1616 Stavropoulos-Kalinoglou A, Metsios GS, Panoulas VF, Nightingale P, Koutedakis Y, Kitas GD. Anti-tumour necrosis factor alpha therapy improves insulin sensitivity in normal-weight but not in obese patients with rheumatoid arthritis. Arthritis Res Ther. 2012;14:R160.
The main conclusion of this study is that obesity is the main determinant of IR in RA patients. This conclusion is based on comparisons between the OB group (positive control of IR) and the three different RA groups (RA NW, RA OW, RA OB) which were matched by age and gender.
A second limitation in our study is related to the fact that the NW group was not matched neither by gender nor age with the rest of the groups. Thus, the observation that HOMA-IR values were significantly larger in RA NW compared to NW should be taken with caution. Nevertheless, as an argument supporting that this limitation may not be decisive, several studies indicate that metabolic alterations such as IR and glucose intolerance are gender independent.5151 Garmendia ML, Lera L, Sánchez H, Uauy R, Albala C. Homeostasis model assessment (HOMA) values in Chilean elderly subjects. Rev Méd Chile. 2009;137:1409-16.,5252 Iozzo P, Beck-Nielsen H, Laakso M, Smith U, Yki-jä Rvinen H, Ferrannini E. Independent influence of age on basal insulin secretion in nondiabetic humans. J Clin Endocrinol Metab. 1999;84:863-8.
In our study, the RA NW group has an average age significantly larger than NW group, and this may be related to age-dependent variations in glucose and insulin. In turn, this age-related effect may affect HOMA-IR determinations, independently of inflammation and BMI. Even though there is an age-dependent reduction in basal insulin release in non-diabetic subjects, this fact is not reflected in fasting insulin serum levels. The explanation for this observation is related to the fact that insulin clearing is also reduced (to the same extent in men and women), so this keeps insulin serum levels normal, despite the age-dependent reduction in insulin release.5252 Iozzo P, Beck-Nielsen H, Laakso M, Smith U, Yki-jä Rvinen H, Ferrannini E. Independent influence of age on basal insulin secretion in nondiabetic humans. J Clin Endocrinol Metab. 1999;84:863-8. Hence, even though we cannot rule out age-dependent alterations in basal insulin release in our study groups, we have observed that the RA NW group has fasting serum insulin levels even higher than the NW group. These higher levels in the RA NW group could be explained by: (1) a reduction in insulin clearing in fasting conditions which is not accompanied by age-related reduction in insulin release. However, this is unlikely, because reductions in clearing and in release generally occur at the same time.5252 Iozzo P, Beck-Nielsen H, Laakso M, Smith U, Yki-jä Rvinen H, Ferrannini E. Independent influence of age on basal insulin secretion in nondiabetic humans. J Clin Endocrinol Metab. 1999;84:863-8. (2) IR that is not linked to obesity but to inflammation. This is in agreement with the conclusions of our study; those groups with the highest HOMA-IR values also have higher insulin levels, keeping glucose levels very close to the normal values (Table 1). In this way, significantly higher HOMA-IR values are determined by obesity than by inflammation.
In conclusion, these results indicate that obesity is a major determinant of IR in RA patients, more determinant than the circulating inflammatory components, considered in terms of TNFα, IL-6 and IL-1β levels. Additionally, the higher IR in RA NW in comparison to normal weight subjects (NW) appears to be solely explained by the impact of inflammatory components. Since the main conclusion of our study is that obesity plays a dominant role over the inflammation in IR in RA patients, clinicians should much emphasize the importance of weight control in their patients, in order to avoid undesirable and potentially severe complications derived from unhealthy weight gain.
-
FundingThis work was supported by Grant PROMEP/103.5/11/8623 and C12-FAI-03-90.90.
Acknowledgments
The authors are grateful for excellent technical assistance by undergraduate students Melissa Badillo Reyes, Alejandro Martinez-Mendez, Domitila Mendez, Sayra Olvera and Sandra Don-Gonzalez. As well as Family Medicine Unit 9 of IMSS, General Hospital and Health Center of Puente del Carmen of Rioverde, Mexico; by valuable medical assistance with Rheumatoid arthritis patients.
REFERENCES
-
1Wolfe F. The natural history of rheumatoid arthritis. J Rheumatol Suppl. 1996;44:13-22.
-
2Bradley JR. TNF-mediated inflammatory disease. J Pathol. 2008;214:149-60.
-
3Seriolo B, Ferrone C, Cutolo M. Longterm anti-tumor necrosis factor-alpha treatment in patients with refractory rheumatoid arthritis. J Rheumatol. 2008;35:355-7.
-
4Gimeno RE, Klaman LD. Adipose tissue as an active endocrine organ: recent advances. Curr Opin Pharmacol. 2005;5:122-8.
-
5Saghizadeh M, Ong JM, Garvey WT, Henry PR, Kern PA. The expression of TNF-α by human muscle. J Clin Invest. 1996;97:1111-6.
-
6Maldonado-Cervantes MI, Galicia OG, Moreno-Jaime B, Zapata-Morales JR, Montoya-Contreras A, Bautista-Perez R, et al. Autocrine modulation of glucose transporter SGLT2 by IL-6 and TNF-α in LLC-PK1 cells. J Physiol Biochem. 2012;68:411-20.
-
7Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28:412-9.
-
8Olivares-Reyes JA, Arellano-Plancarte A, Castillo-Hernandez JR. Angiotensin II and the development of insulin resistance: implications for diabetes. Mol Cell Endocrinol. 2009;302:128-39.
-
9Moller DE. Potential role of TNF-alpha in the pathogenesis of insulin resistance and type 2 diabetes. Trends Endocrinol Metab. 2000;11:212-7.
-
10Miyazaki Y, Pipek R, Mandarino LJ, DeFronzo RA. Tumor necrosis factor α and insulin resistance in obese type 2 diabetic patients. Int J Obes Relat Metab Disord. 2003;27:88-94.
-
11Olson NC, Callas PW, Hanley AJG, Festa A, Haffner SM, Wagenknecht LE, et al. Circulating levels of TNF-α are associated with impaired glucose tolerance, increased insulin resistance, and ethnicity: the Insulin Resistance Atherosclerosis Study. J Clin Endocrinol Metab. 2012;97:1032-40.
-
12Dandona P, Aljada A, Bandyopadhyay A. Inflammation: the link between insulin resistance, obesity, and diabetes. Trends Immunol. 2004;25:4-7.
-
13Nieto-Vazquez I, Fernandez-Veledo S, Kramer DK, Vila-Bedmar R, Garcia-Guerra L, Lorenzo M. Insulin resistance associated to obesity: the link TNF-alpha. Arch Physiol Biochem. 2008;114:183-94.
-
14Stavropoulos-Kalinoglou A, Metsios GS, Koutedakis Y, Kitas GD. Obesity in rheumatoid arthritis. Rheumatology. 2011;50:450-62.
-
15Smolen JS, Martinez-Avila JC, Aletaha D. Tocilizumab inhibits progression of joint damage in rheumatoid arthritis irrespective of its anti-inflammatory effects: disassociation of the link between inflammation and destruction. Ann Rheum Dis. 2012;71:687-93.
-
16Stavropoulos-Kalinoglou A, Metsios GS, Panoulas VF, Nightingale P, Koutedakis Y, Kitas GD. Anti-tumour necrosis factor alpha therapy improves insulin sensitivity in normal-weight but not in obese patients with rheumatoid arthritis. Arthritis Res Ther. 2012;14:R160.
-
17Kumar P, Banik S. Pharmacotherapy options in rheumatoid arthritis. Clin Med Insights Arthritis Musculoskelet Disord. 2013;6:35-43.
-
18Nishina N, Kaneko Y, Kameda H, Kuwana M, Takeuchi T. Reduction of plasma IL-6 but not TNF-α by methotrexate in patients with early rheumatoid arthritis: a potential biomarker for radiographic progression. Clin Rheumatol. 2013;32:1661-6.
-
19Barrera P, Haagsma CJ, Boerbooms AM, Van-Riel PLCM, Borm GF, Van de Putte LBA, et al. Effect of methotrexate alone or in combination with sulphasalazine on the production and circulating concentrations of cytokines and their antagonists. Longitudinal evaluation in patients with rheumatoid arthritis. Br J Rheumatol. 1995;34:747-55.
-
20Greis A, Murgott J, Rafalzik S, Gerstberger R, Hübschle T, Roth J. Characterization of the febrile response induced by fibroblast-stimulating lipopeptide-1 in guinea pigs. Am J Physiol Regul Integr Comp Physiol. 2007;293:R152-61.
-
21Pelletier JP, Cloutier JM, Martel-Pelletier J. In vitro effects of NSAIDs and corticosteroids on the synthesis and secretion of interleukin 1 by human osteoarthritic synovial membranes. Agents Actions. 1993;39:181-93.
-
22Roth J, Hübschle T, Pehl U, Ross G, Gerstberger R. Influence of systemic treatment with cyclooxygenase inhibitors on lipopolysaccharide-induced fever and circulating levels of cytokines and cortisol in guinea-pigs. Pflugers Arch. 2002;443:411-7.
-
23Penesová A, Rádiková Z, Vlček M, Kerlik J, Lukáč J, Rovenský J, et al. Chronic inflammation and low-dose glucocorticoid effects on glucose metabolism in premenopausal females with rheumatoid arthritis free of conventional metabolic risk factors. Physiol Res. 2013;62:75-83.
-
24Uehara A, Kohda H, Sekiya C, Takasugi Y, Namiki M. Inhibition of interleukin-1 beta release from cultured human peripheral blood mononuclear cells by prednisolone. Experientia. 1989;45:166-7.
-
25Charles P, Elliott MJ, Davis D, Potter A, Kalden JR, Antoni C, et al. Regulation of cytokines, cytokine inhibitors, and acute-phase proteins following anti-TNF-alpha therapy in rheumatoid arthritis. J Immunol. 1999;163:1521-8.
-
26Rostom S, Mengat M, Lahlou R, Hari A, Bahiri R, Hajjaj-Hassouni N. Metabolic syndrome in rheumatoid arthritis: case control study. BMC Musculoskelet Disord. 2013;14:147.
-
27Chung CP, Oeser A, Solus JF, Gebretsadik T, Shintani A, Avalos I, et al. Inflammation associated insulin resistance: differential effects in rheumatoid arthritis and systemic lupus erythematosus define potential mechanisms. Arthritis Rheum. 2008;58:2105-12.
-
28Scher JU. Monotherapy in rheumatoid arthritis. Bull Hosp Jt Dis. 2013;71:204-7.
-
29Cohen S, Hurd E, Cush J, Schiff M, Weinblatt ME, Moreland LW, et al. Treatment of Rheumatoid Arthritis with Anakinra, a recombinant human interleukin-1 receptor antagonist, in combination with methotrexate results of a twenty-four-week, multicenter, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2002;46:614-24.
-
30Seriolo B, Paolino S, Ferrone C, Cutolo M. Effects of etanercept or infliximab treatment on lipid profile and insulin resistance in patients with refractory rheumatoid arthritis. Clin Rheumatol. 2007;26:1799-800.
-
31Lai-Shan T, Tomlinson B, Chu TT, Li TK, Li EK. Impact of TNF inhibition on insulin resistance and lipids levels in patients with rheumatoid arthritis. Clin Rheumatol. 2007;26:1495-8.
-
32Stagakis I, Bertsias G, Karvounaris S, Kavousanaki M, Virla D, Raptopoulou A, et al. Anti-tumor necrosis factor therapy improves insulin resistance, beta cell function and insulin signaling in active rheumatoid arthritis patients with high insulin resistance. Arthritis Res Ther. 2013;14:1-11.
-
33Ferraz-Amaro I, Arce-Franco M, Muñiz J, López-Fernández J, Hernández-Hernández V, Franco A, et al. Systemic blockade of TNF-α does not improve insulin resistance in humans. Horm Metab Res. 2011;43:801-8.
-
34Bernstein LE, Berry J, Kim S, Canavan B, Grinspoon SK. Effects of etanercept in patients with the metabolic syndrome. Arch Intern Med. 2006;166:902-8.
-
35Altomonte J, Harbaran S, Richter A, Dong H. Fat depot specific expression of adiponectin is impaired in Zucker fatty rats. Metabolism. 2003;52:958-63.
-
36Romacho T, Elsen M, Röhrborn D, Eckel J. Adipose tissue and its role in organ crosstalk. Acta Physiol. 2014;210:733-53.
-
37Fang P, Shi M, Yu M, Guo L, Bo P, Zhang Z. Endogenous peptides as risk markers to assess the development of insulin resistance. Peptides. 2014;51:9-14.
-
38Arner P. The adipocyte in insulin resistance: key molecules and the impact of the thiazolidinediones. Trends Endocrinol Metab. 2003;14:137-45.
-
39Hotamisligil GS, Arner P, Caro JF, Atkinson RL, Spiegelman BM. Increased adipose tissue expression of tumour necrosis factor-alpha in human obesity and insulin resistance. J Clin Invest. 1995;95:2409-15.
-
40Sethi JK, Hotamisligil GS. The role of TNF-α in adipocyte metabolism. Semin Cell Dev Biol. 1999;10:19-29.
-
41Kraegen EW, Cooney GJ. Free fatty acids and skeletal muscle insulin resistance. Curr Opin Lipidol. 2008;19:235-41.
-
42Srinivasan S, Choy EH. The role of Interleukin 6 in the pathophysiology of rheumatoid arthritis. Ther Adv Musculoskelet Dis. 2010;2:247-56.
-
43Khaodhiar L, Ling PR, Blackburn GL, Bistrian BR. Serum levels of interleukin-6 and C-reactive protein correlate with body mass index across the broad range of obesity. JPEN. 2004;28:410-5.
-
44Wallenius K, Wallenius V, Sunter D, Dickson SL, Jansson JO. Intracerebroventricular interleukin-6 treatment decreases body fat in rats. Biochem Biophys Res Commun. 2002;293:560-5.
-
45Tekaya R, Sahli H, Zribi S, Mahmoud I, Ben Hadj Yahia C, Abdelmoula L, et al. Obesity has a protective effect on radiographic joint damage in rheumatoid arthritis. Tunis Med. 2011;89:462-5.
-
46van der Helm-van Mil AH, van der Kooij SM, Allaart CF, Toes RE, Huizinga TW. A high body mass index has a protective effect on the amount of joint destruction in small joints in early rheumatoid arthritis. Ann Rheum Dis. 2008;67:769-74.
-
47Kaufmann J, Kielstein V, Kilian S, Stein G, Hein G. Relation between body mass index and radiological progression in patients with rheumatoid arthritis. J Rheumatol. 2003;30:2350-5.
-
48Ruge T, Lockton JA, Renstrom F, Lystig T, Sukonina V, Svensson MK, et al. Acute hyperinsulinemia raises plasma interleukin-6 in both non diabetic and type 2 diabetes mellitus subjects, and this effect is inversely associated with body mass index. Metabolism. 2009;58:860-6.
-
49Lee SW, Tsou AP, Chan H, Thomas J, Petrie K, Eugui EM, et al. Glucocorticoids selectively inhibit the transcription of the interleukin 1β gene and decrease the stability of interleukin 1β mRNA. Immunology. 1988;85:1204-8.
-
50Zhang HH, Kumar S, Barnett AH, Eggo MC. Dexamethasone inhibits tumor necrosis factor-α induced apoptosis and interleukin-1β release in human subcutaneous adipocytes and preadipocytes. J Clin Endocrinol Metab. 2001;86:2817-25.
-
51Garmendia ML, Lera L, Sánchez H, Uauy R, Albala C. Homeostasis model assessment (HOMA) values in Chilean elderly subjects. Rev Méd Chile. 2009;137:1409-16.
-
52Iozzo P, Beck-Nielsen H, Laakso M, Smith U, Yki-jä Rvinen H, Ferrannini E. Independent influence of age on basal insulin secretion in nondiabetic humans. J Clin Endocrinol Metab. 1999;84:863-8.
Publication Dates
-
Publication in this collection
Jul-Aug 2017
History
-
Received
2 Mar 2016 -
Accepted
25 Oct 2016