ABSTRACT
OBJECTIVE
: To evaluate functional outcomes of patients submit-ted to proximal row carpectomy for the treatment of wrist arthri-tis
METHODS
: This is a retrospective study using wrist motion and grip strenght of patients diagnosed with Kienböck disease and scaphoid non-union surgically treated by this technique
RESULTS
: Eleven patients with 2-year follow-up were evaluated. Wrist motion (flexion, extension and ulnar deviation) and grip strength were significantly better from preoperative values. Ho-wever, no difference in radial deviation was observed in these patients
CONCLUSION
: Proximal row carpectomy provides an alternative option for treatment of wrist arthritis, resulting in better active range of motion and grip strength in the long run. Level of Evidence IV, Case Series.
Keywords:
Osteonecrosis; Carpal Bones/surgery; Pseudarthrosis
INTRODUCTION
The proximal carpectomy is a surgical procedure used in de-generative diseases of the wrist that preserves the possibility of movement.1Wall LB, Didonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am. 2013;38(8):1498-504. 3Chim H, Moran SL. Long-term outcomes of proximal row carpectomy: a sys-tematic review of the literature. J Wrist Surg. 2012;1(2):141-8. Indications are late conditions secondary to injury of the scapholunate ligament (scapholunate advanced collap-se, SLAC); nonunion of scaphoid (scaphoid nonunion advan-ced collapse, SNAC); Kienböck disease; failure of implants to the scaphoid or lunate, and chronic perilunate dislocations.1Wall LB, Didonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am. 2013;38(8):1498-504. 4Godinho DR, Barros F, Barros F, Argotte W. Carpectomia proximal. Rev Bras Ortop. 1996;31(3):225-30. 5Severo LA, Costa M, Lopes Junior OV, Piluski P, Lech O . Análise funcional da artrodese dos quatro cantos comparada com a carpectomia proximal.. Rev Bras Ortop 2006;41:14-21. Contraindications include chondral lesions in the proximal pole of the capitate or lunate fossa on the distal radius.6Culp RW, McGuigan FX, Turner MA, Lichtman DM, Osterman AL, McCar-roll HR. Proximal row carpectomy: a multicenter study.. J Hand Surg Am 1993;18(1):19-25.
The aim of this study was to analyze the functional results (ran-ge of motion and palmar grip strength) of patients undergoing proximal carpectomy in the treatment of traumatic or non-trau-matic degenerative conditions of the wrist.
MATERIALS AND METHODS
This is a retrospective analysis of patients operated between February 2002 and February 2012, approved by the Institution's Ethics Committee under CAAE number 36705614.7.0000.5440. We evaluated 21 patients undergoing proximal carpectomy. Data were collected from medical records and functional as-sessments of patients by the Hand Therapy team in the preop-erative, immediate postoperative and late postoperative period. The functional evaluation consisted of analogic goniometry of the active range of motion of the wrist (flexion, extension, ra-dial deviation and ulnar deviation) and grip strength measured by a Jamar(r) dynamometer (USA) in the affected wrist and its contralateral side. Flexion and extension goniometry was per-formed with the goniometer's arms on the dorsal side of the third metacarpal and the other on the dorsal side of the radius. For measuring radial deviation and ulnar deviation, the center of the goniometer was placed on the head of the capitate on the dorsal surface of the wrist, one arm on the third metacarpal and the other on the dorsal side of radius.7Pardini Júnior AG. Punho. In: Barros Filho TEP, Lech O . Exame físico em ortopedia. São Paulo: Sarvier; 2002. p. 157-70.The measurement of strength was always made with the limb parallel to the upper torso, elbow in 90° flexion, forearm and wrist in a neutral position and the dynamometer set at the second position (specific to assess grip strength).8Silva JB, Del Rio JT, Fernandes HF, Diniz S, Fridman M. Carpectomia proximal do carpo na artrose radioescafolunar.. Rev Bras Ortop 1997;32(11):894-8. 9Caporrino FA, Faloppa F, Santos JBG, Ressio C, Soares FHC, Nakachima LR, et al. Estudo populacional da força de preensão palmar com dinamômetro Jamar .. Rev Bras Ortop 1998;33(2):150-4. The simple arithmetic mean of three measurements with one minute interval between them, alternat-ing between the dominant and non-dominant side was consid-ered. For comparative analysis, we considered the measures made one week before the surgery and two years afterwards. Statistical analysis was performed using the non-parametric Wilcoxon-Mann-Whitney test for dependent variables, due to the small sample size. p-Value was calculated by normal approach.
Surgical Technique
All patients underwent anesthetic block of the brachial plexus and operated supine over a hand table. Venous drainage was gravitational and with the help of Esmarch bandage. The tour-niquet was set at the arm level.
The access was longitudinal between the third and fourth ex-tender compartments until exposure of the capsule, which was also split longitudinally. The articular surfaces were inspected to investigate possible chondral lesions, especially in the lunate fossa and the proximal pole of the capitate. Resection was always initiated by the lunate and pyramidal, and ended in the scaphoid, which was removed cutting to pieces with a gouge. Care was taken to preserve the volar radiocarpal ligaments, thus preventing possible ulnar translation of the carpal. In no case the distal pole of the scaphoid was left. Likewise, radial styloidectomy and neurectomy of the posterior interosseous nerve were also not performed in any case. After the removal of the tourniquet and hemostasis revision, the capsule was closed anatomically with non-absorbable thread, without bringing in the radiocarpal joint. Any kind of internal or external fixation was ever used. The volar splint, placed in the immediate postope-rative period, was maintained in all cases for four to six weeks, when the movement of the wrist was started gradually, assisted by the Hand Therapy team.10Stern PJ, Agabegi SS, Kiefhaber TR, Didonna ML. Proximal row carpectomy. J Bone Joint Surg Am. 2005 ;87(Suppl 1)(Pt 2):166-74.
RESULTS
Of the 21 patients who underwent proximal carpectomy, six did not return for clinical evaluation, three requested discharge from the outpatient facility before completing one year after surgery and one died. In all, 11 patients completed follow-up and were followed until at least two years after surgery for func-tional evaluation. Of these, two were female and 9 male. Four patients had Kienböck disease (stage IIIb) and seven presented non-union of the scaphoid (SNAC). The right side was affected eight times and left, three times. Only in two cases the affected side was not the dominant side. The mean age for the final func-tional evaluation, two years after surgery, was 42.6 years old.
Statistical analysis
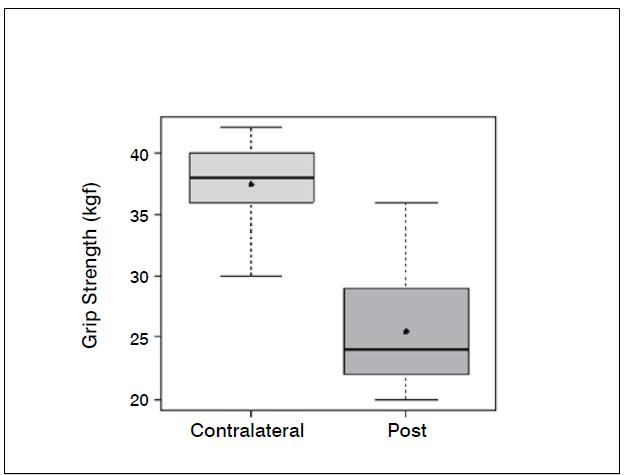
Statistical analysis showed significant differences (p <0.05) in the comparison of wrist flexion pre and postoperatively (p--value = 0.0006); extension (p-value = 0.0337); ulnar deviation (p=0.0289); grip strength (p-value = 0.0006) and when com-paring the contralateral wrist (not affected) and the operated wrist (p-value=0.0002). The evaluation of the contralateral wrist grip strength averaged 37.45 kgf, standard deviation 3.8 kgf, minimum 30 kgf, maximum 42 kgf and a median of 38 kgf. There was no significant difference comparing radial deviation before and after surgery (p-value = 0.3475).
Tables 1-3 and Figures 1-6 present these data and those regarding measurement (goniometer and grip strength) pre and postoperative.
DISCUSSION
A Jamar(r) dynamometer (USA), recommended by the American Society of Hand Therapists and used in in most studies was used to assess grip strength. The second prehension position was used for all patients, since it facilitates the comparison of results between them and among other works in the literature. However, there is a possibility of adjusting the position accor-ding to the hand size of each individual.
We adopted a minimum interval of one minute between me-asurements to ensure that there was no influence of the fac-tor muscle fatigue. We used simple arithmetic mean of the three measures. Caporrino et al.9Caporrino FA, Faloppa F, Santos JBG, Ressio C, Soares FHC, Nakachima LR, et al. Estudo populacional da força de preensão palmar com dinamômetro Jamar .. Rev Bras Ortop 1998;33(2):150-4.considered the highest mark achieved between the three measures. Probably the difference between these methods is minimal and the important thing is to maintain the same measurement standard before and after surgery.
Boxplot comparing extension of the wrist (degrees) preoperative and two years after surgery.
Boxplot comparing radial deviation of the wrist (degrees) preopera-tive and two years after surgery.
Boxplot comparing ulnar deviation of the wrist (degrees) preopera-tive and two years after.
Boxplot comparing grip strength of the wrist (kgf) preoperative and two years after surgery
Boxplot comparing grip strength of the contralateral wrist (kgf) preoperative and two years after surgery.
Of the 11 patients who were evaluated after two years of sur-gery, the causative basis of diagnosis of degenerative clinical handle frame was nonunion of scaphoid fractures (SNAC) and Kienböck disease. There were no cases secondary to the injury of scapholunate ligament (SLAC), which could be included in the functional evaluation. Other medical conditions where the proximal carpectomy can be indicated such as rheumatoid arthritis, flexion contractures (congenital or acquired), chronic perilunate dislocations and replantation were not observed, however, they would be excluded from the series according to their unique characteristics that hinder a comparative analysis. The data show that there was a significant improvement in the ability to actively bend (15.6° to 37.0°) and extend (from 14.0° to 29.4°) the wrist, and ulnar deviation (12.5° to 21.1°). There was no significant gain in the radial deviation (5.1° to 6.2°). The largest portion of the population shows flexion between 70-80°, and extension 60-70°, 45° ulnar deviation and 15° radial devia-tion.7Pardini Júnior AG. Punho. In: Barros Filho TEP, Lech O . Exame físico em ortopedia. São Paulo: Sarvier; 2002. p. 157-70. The total range of motion for flexion-extension showed an average increase of 29.6° to 66.4°, which represents a much better ability to spatial positioning of the hand and obvious functional gain. The pronosupination and goniometry of passive movement of the wrist were not evaluated in this study. Although not being fundamental parameters in this situation, they could enrich the final evaluation.
Grip strength also improved significantly, from 18.2 kgf in the preoperative evaluation to 25.4 kgf after two years of surgery. The comparison with the unaffected side shows that there is an important difference, since the average was 37.4 kgf. Popula-tion studies in our midst show that the difference between the dominant and non-dominant hand is around 10 to 12%.10Stern PJ, Agabegi SS, Kiefhaber TR, Didonna ML. Proximal row carpectomy. J Bone Joint Surg Am. 2005 ;87(Suppl 1)(Pt 2):166-74.
Pre and postoperative pain has not been systematically evalu-ated with visual or numerical scales. After two years of surgery, according to medical records, five patients (46%) had no pain or pain was reported as mild and tolerable and went back to work. There is no reference to the type of work or if there was function exchange. Three patients (27%) had pain equal to the preoperative situation, but did not want another surgery. Of these, two returned to work; there is no information about the third. Three patients (27%) had worsened pain relative to baseline, one of which evolved with clinical signs compatible with complex regional pain syndrome. These three cases were subsequently submitted to total wrist arthrodesis.
Our results show correspondence to other studies with high-er postoperative follow-ups; 1Wall LB, Didonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am. 2013;38(8):1498-504. 3Chim H, Moran SL. Long-term outcomes of proximal row carpectomy: a sys-tematic review of the literature. J Wrist Surg. 2012;1(2):141-8. 11Ali MH, Rizzo M, Shin AY, Moran SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (NY). 2012;7(1):72-8. and comparisons between techniques.2Zinberg EM, Chi Y. Proximal row carpectomy versus scaphoid excision and intercarpal arthrodesis: intraoperative assessment and procedure selection.. J Hand Surg Am 2014;39(6):1055-62. 5Severo LA, Costa M, Lopes Junior OV, Piluski P, Lech O . Análise funcional da artrodese dos quatro cantos comparada com a carpectomia proximal.. Rev Bras Ortop 2006;41:14-21.
Auxiliary surgical techniques can bring improvement in pain symptoms, such as the interposition of the volar capsule,12Kwon BC, Choi SJ, Shin J, Baek GH. Proximal row carpectomy with capsular interposition arthroplasty for advanced arthritis of the wrist. J Bone Joint Surg Br. 2009;91(12):1601-6.osteochondral grafts13Fowler JR, Tang PC, Imbriglia JE. Osteochondral resurfacing with proximal row carpectomy: 8-year follow-up. Orthopedics. 2014;37(10):e856-9. and posterior interosseous neurecto-my, however, they were not used in this series. Further studies should be conducted to compare the results of the association or not of these procedures, as well as the proximal arthroscopic carpectomy.14Weiss ND, Molina RA, Gwin S. Arthroscopic proximal row carpectomy.. J Hand Surg Am 2011;36(4):577-82.
Function scores (DASH, QuickDASH, MHQ - Michigan Hand Questionaire15Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire.. J Hand Surg Am 1998;23(4):575-87. and MWS-Mayo Wrist Score16Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, Linscheid RL. Scaphoid malunion.. J Hand Surg Am 1989;14(4):679-87.) and radiographic review for staging of osteoarthritis radiocapitate6Culp RW, McGuigan FX, Turner MA, Lichtman DM, Osterman AL, McCar-roll HR. Proximal row carpectomy: a multicenter study.. J Hand Surg Am 1993;18(1):19-25. 17Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study.. J Hand Surg Am 2003;28(4):561-9. can also be used in future studies as a way to refine the evaluation of results in the medium and long term.
CONCLUSION
The proximal carpectomy is an alternative in the treatment of degenerative disorders of the wrist, improving range of motion and grip strength, when compared to preoperative status.
REFERENCES
- Wall LB, Didonna ML, Kiefhaber TR, Stern PJ. Proximal row carpectomy: minimum 20-year follow-up. J Hand Surg Am. 2013;38(8):1498-504.
- Zinberg EM, Chi Y. Proximal row carpectomy versus scaphoid excision and intercarpal arthrodesis: intraoperative assessment and procedure selection.. J Hand Surg Am 2014;39(6):1055-62.
- Chim H, Moran SL. Long-term outcomes of proximal row carpectomy: a sys-tematic review of the literature. J Wrist Surg. 2012;1(2):141-8.
- Godinho DR, Barros F, Barros F, Argotte W. Carpectomia proximal. Rev Bras Ortop. 1996;31(3):225-30.
- Severo LA, Costa M, Lopes Junior OV, Piluski P, Lech O . Análise funcional da artrodese dos quatro cantos comparada com a carpectomia proximal.. Rev Bras Ortop 2006;41:14-21.
- Culp RW, McGuigan FX, Turner MA, Lichtman DM, Osterman AL, McCar-roll HR. Proximal row carpectomy: a multicenter study.. J Hand Surg Am 1993;18(1):19-25.
- Pardini Júnior AG. Punho. In: Barros Filho TEP, Lech O . Exame físico em ortopedia. São Paulo: Sarvier; 2002. p. 157-70.
- Silva JB, Del Rio JT, Fernandes HF, Diniz S, Fridman M. Carpectomia proximal do carpo na artrose radioescafolunar.. Rev Bras Ortop 1997;32(11):894-8.
- Caporrino FA, Faloppa F, Santos JBG, Ressio C, Soares FHC, Nakachima LR, et al. Estudo populacional da força de preensão palmar com dinamômetro Jamar .. Rev Bras Ortop 1998;33(2):150-4.
- Stern PJ, Agabegi SS, Kiefhaber TR, Didonna ML. Proximal row carpectomy. J Bone Joint Surg Am. 2005 ;87(Suppl 1)(Pt 2):166-74.
- Ali MH, Rizzo M, Shin AY, Moran SL. Long-term outcomes of proximal row carpectomy: a minimum of 15-year follow-up. Hand (NY). 2012;7(1):72-8.
- Kwon BC, Choi SJ, Shin J, Baek GH. Proximal row carpectomy with capsular interposition arthroplasty for advanced arthritis of the wrist. J Bone Joint Surg Br. 2009;91(12):1601-6.
- Fowler JR, Tang PC, Imbriglia JE. Osteochondral resurfacing with proximal row carpectomy: 8-year follow-up. Orthopedics. 2014;37(10):e856-9.
- Weiss ND, Molina RA, Gwin S. Arthroscopic proximal row carpectomy.. J Hand Surg Am 2011;36(4):577-82.
- Chung KC, Pillsbury MS, Walters MR, Hayward RA. Reliability and validity testing of the Michigan Hand Outcomes Questionnaire.. J Hand Surg Am 1998;23(4):575-87.
- Amadio PC, Berquist TH, Smith DK, Ilstrup DM, Cooney WP 3rd, Linscheid RL. Scaphoid malunion.. J Hand Surg Am 1989;14(4):679-87.
- Jebson PJ, Hayes EP, Engber WD. Proximal row carpectomy: a minimum 10-year follow-up study.. J Hand Surg Am 2003;28(4):561-9.
-
1
Work developed at Universidade de São Paulo, Faculdade de Medicina de Ribeirão Preto, Hospital das Clínicas, Ribeirão Preto, SP, Brasil
Publication Dates
-
Publication in this collection
Nov-Dec 2015
History
-
Received
25 May 2015 -
Accepted
07 July 2015