Abstract
Federalism is basis of the Republic of Brazil which is made up of the union of states, municipalities and the Federal District, with the basic principle of political and administrative decentralization in all political, economic and social relations. In the health sector, the primary health care provider should be able to integrate all care that the patient receives through the coordination of health services. This article aims to evaluate the results of referrals for consultations and outpatient examinations in primary health care in the municipality of Rio de Janeiro, highlighting the advances, limitations and challenges for management at the local level. A quantitative study was designed using administrative databases from the Registry of National Health Establishments (CNES), the National Regulatory System (SISREG), and a linkage between them. Between 2011 and 2015, the number of scheduled procedures increased by 86%, reflecting the decentralization of outpatient regulation for family doctors. It can be inferred that there is no shortage of specialists for outpatient care in the city in almost all areas. There are actually artificial bottlenecks that arise as a result of the lack of regulation of most of the workload contracted in specialist areas, that is, the number of vacancies is smaller than the capacity of health services available in health units at the municipal, state, federal levels and those contracted by the Unified Health System (SUS).
Regulation; Primary Health Care; Waiting lists
Resumo
O federalismo é o pilar da República, composta pela união dos Estados, dos Municípios e do Distrito Federal, tendo como princípio básico a descentralização político-administrativa, nas relações políticas, econômicas e sociais. Na saúde, o provedor de atenção primária deve ser capaz de integrar todo cuidado que o paciente recebe através da coordenação entre os serviços. Objetiva-se avaliar os resultados dos encaminhamentos de consultas e exames ambulatoriais da APS do município do Rio de Janeiro, demonstrando os avanços, limites e desafios para a gestão no nível local. Estudo quantitativo que utilizou as bases de dados administrativas do Cadastro Nacional de Estabelecimentos de Saúde (CNES) e o Sistema Nacional de Regulação (SISREG), além de uma “linkage” entre ambas as bases. Entre 2011 e 2015, o nº de procedimentos agendados teve um aumento de 86%, como reflexo da descentralização da regulação ambulatorial para os médicos de família. Pode-se inferir que não há falta de especialistas para atendimento ambulatorial no SUS carioca em quase todas as áreas. Existem gargalos artificiais pela ausência de regulação da maior parte da carga horária contratada na especialidade, ou seja, a oferta de vagas é menor do que a capacidade instalada das unidades municipal, estaduais, federais e conveniadas ao SUS.
Regulação; Atenção Primária à Saúde; Listas de espera
Introduction
Federalism is the central pillar of the Federal Republic of Brazil, comprised of the indissoluble union of the states, municipalities, and the Federal District, wherein political and administrative decentralization in political, economic, and social relations is a basic principle11. Lassance A. Federalismo no Brasil: trajetória institucional e alternativas para um novo patamar de construção do Estado. In: Linhares PTF, Mendes CC, Lassance A, organizadores. Federalismo à Brasileira: questões para discussão. Brasília: IPEA; 2012. p. 23-36. v. 8. (Série: Diálogos para o Desenvolvimento).,22. Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil. Rio de Janeiro: Editora Companhia das Letras; 2012..
In article 196, the Federal Constitution of 1988 stipulates health as “a right of all people and the obligation of the State,” and Law Number 8.080 initially operationalized this with the Unified Health System (or SUS), defining it in a broad way as the physical and mental well-being of the individual and their experience living in society. It also included in this definition the idea that health actions and services must be integrated into the public sphere, in a structured and local-level network, oriented by the guidelines of governmental decentralization, integrated care, and community participation.
After a wait of more than 20 years, Law 8.080/90 was put into effect by Decree 7.508/11, which aimed at clarifying various concepts within the limits of the Constitution, and which advocates universal access to the health actions and services carried out by the SUS. It organized the following: health region; organizational contract of public health actions; points of entry; interagency commissions; health map; healthcare network; open access special services; clinical protocol; and therapeutic guidelines. With its Article 11, it also officially made Primary Health Care into the automatic first-contact access point to the SUS.
In this period between the Law and the Decree, we can observe two distinct periods of relations between federal entities. The first occurred during the decades of 1990/2000, with the strong political-administrative decentralization of the municipalities in a process known as “municipalization.” The second occurred in the second half of the decade of 2000 with the “Pact For Health”33. Brasil. Ministério da Saúde (MS). Secretaria Executiva. Departamento de Apoio à Descentralização. Coordenação de Integração Programática. Regionalização solidária e cooperativa: orientações para sua implementação no SUS. Brasília: MS; 2006. (Série Pactos pela Saúde 2006, v. 3)., which continues until the present day, with the optimization and streamlining of the SUS using the strategy of regionalization.
Nevertheless, as Albuquerque Netto44. Albuquerque Netto JA. O direito à saúde no federalismo: repartição de competência na assistência farmacêutica [monografia]. Brasília: Instituto Brasiliense de Direito Público; 2010. observes, the Constitution presented its own rules so that each federal entity would be made responsible for a set number of duties, with the goal of not duplicating the execution of a given task, thus guaranteeing better attention to peoples’ health.
In the field of health, this institutional structure called “Brazilian sanitary federalism” introduces innumerable challenging questions for management at the three levels of government in the political-administrative sphere, beginning with the substantial geographic differences between entities. For example, the state of Minas Gerais has 853 municipalities; Rio de Janeiro has 92, and Roraima only 15. In addition, among the total of 5,570 municipalities, 69% have less than 20,000 inhabitants55. Instituto Brasileiro de Geografia e Estatística (IBGE). Estimativas populacionais para os municípios brasileiros em 01.07.2014. Diretoria de Pesquisas - DPE -Coordenação de População e Indicadores Sociais – COPIS, 2014. [acessado 2016 jul 2]. Disponível em: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2014/estimativa_dou.shtm
http://www.ibge.gov.br/home/estatistica/...
.
In 2006, the main strategy for increasing first-contact access to health services became the National Policy of Primary Care (Política Nacional de Atenção Básica, or PNAB), and was revised afterward in 201166. Brasil. Ministério da Saúde (MS). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Política nacional de atenção básica. Brasília: MS; 2006. (Série A. Normas e Manuais Técnicos. Série Pactos pela Saúde. v. 4).,77. Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica (PNAB). Brasília: MS; 2012. (Série E. Legislação em Saúde). (Brasil, 2005b; 2012). The new version of the PNAB authorizes partial work agreements for the first time, facilitating the contracting of doctors for the Family Health Teams (Equipes de Saúde da Familia, or ESF), especially in large cities, which was found to be a barrier to the expansion of the ESF88. Mendonça MHM, Martins MIC, Giovanella L, Escorel S. Desafios para gestão do trabalho a partir de experiências exitosas de expansão da Estratégia de Saúde da Família. Cien Saude Colet 2010; 15(5):2355-2365.. Nevertheless, as Costa99. Costa NR. A Estratégia de Saúde da Família, a atenção primária e o desafio das metrópoles brasileiras. Cien Saude Colet 2016; 21(5):1389-1398. emphasizes, the PNAB falls short in relation to the large municipalities and metropolises in indicating an option for a national, single-payer format, which favors the poorer, smaller municipalities with lesser demographic density. Furthermore, it also advocates a closed model for the formation of a minimal team for the Family Health Strategy.
Primary Health Care: the main point of entry and coordinator of care
For “Primary Health Care” (PHC), we use the broader concept coined by Starfield1010. Starfield B. Atenção primária: equilíbrio entre necessidades de saúde, serviços e tecnologia. Brasília: Unesco, Ministério da Saúde; 2002. that is based on four essential attributes and three derived attributes. The four essential attributes of PHC are: (1) first-contact access: accessibility and utilization of the health services as a source of care with each new problem or new episode of an existing health problem, with the exception of genuine medical emergencies; (2) longitudinality: existence of a continuous source of care, as well as its use over time, (3) comprehensiveness: the list of services available and offered by Primary Health Care. Actions that the health service must offer so that its users receive comprehensive care - as much from the perspective of the bio-psycho-social process of health and illness, as well as the actions of promotion, prevention, curing, and rehabilitation suitable to the context of this level of attention - even though some actions cannot be offered inside the PHC units. This includes referrals to other medical and non-medical specialists, hospitals, and others, which relates to (4) – coordination of care. Coordination of care presuppose some form of continuity, whether in the form of visits with the same professional, the use of patient records, or both, in addition to the recognition of problems treated by other services and the integration of that care in the total care of the patient. The provider of primary care must be capable of integrating all the care the patient receives via the coordination among the services.
The coordination of care, the fourth attribute of primary care, is essential for acquiring the other aspects of care. According to this same author, without it, continuity would lose its potential, comprehensiveness would be made difficult, and the function of first contact would become a purely administrative function. Not all needs can be tended to in primary care, and for this reason people tend to go to other locales. For the author, the challenges of coordination can be subdivided into three aspects: (1) in the establishment of health itself, when the users are seen by different members of the team and the information regarding the patient are generated in different places (including laboratories and clinics); (2) with other specialists called upon to give counseling or short-term interventions; and (3) with other specialists that deal with a specific patient for a long period of time, due to the presence of a specific disturbance. The care coordination of the PHC includes the issue of referrals to other specialists, among other aspects.
Until 2009 in the city of Rio de Janeiro, the Regulatory System of medical appointments and elective procedures was practically nonexistent, with the burden falling on the patient to go to the centers and secure an appointment for the desired procedure when they would receive referrals. This generated costs for the user in the form of travel expenses, lost work days, and a profound inequity of access, aside from the enormous lines for scheduling and changing appointments. With the creation of Polyclinic Coordination and the strengthening of the regulatory activity of the Undersecretary General, a product of the organizational reform of the Municipal Health Secretariat (Secretaria Municipal de Saúde – SMS), it became possible to utilize a National Regulation System of the Health Ministry for the greater number of healthcare units. By the end of 2011, 790,091 procedures for the year had been regulated in a centralized manner, with long wait times relative to the demand, and with the greater part of these procedures receiving automatic regulation by the computerized system. Because of the fragility of the system, this automatic scheduling did not demonstrate good performance in evaluating the wait time and distance from the residence, permitting disordered appointments that conflicted with the regionalization of the city, and also did not offer a process of control and protection against unnecessary referrals. Following the influence of European reforms of their health systems1111. Calnan M, Hutten J, Tiljak H. The challenge of coordination: the role of primary care professionals in promoting integration across the interface. In: Saltman RB, Rico A, Boerma W, editors. Primary care in the driver's seat? organizational reform in European primary care. Maidenhead, New York: Open University Press; 2006. p. 85-104., the Municipal Health Secretary profoundly altered their model of outpatient regulation, decentralizing it to the primary care units in the second semester of 2012; that is, the family doctors responsible for almost 200 healthcare establishments began to schedule the available procedures (exams and consultations) of different medical and non-medical specialties directly through an official Ministry of Health Information System.
In the municipality of Rio de Janeiro, which for the aims of health administration is divided into ten planning areas formed by existing neighborhoods, the expansion of the ESF occurred in a heterogeneous way in these areas from 2009 to 2016. This movement for change, referred to as “Primary Healthcare Reform,” had reached 39.8% coverage by 2012, and by December 2015 it had passed 50%1212. Soranz D, Pinto LF, Penna GO. Eixos e a Reforma dos Cuidados em Atenção Primária em Saúde (RCPHC) na cidade do Rio de Janeiro, Brasil. Cien Saude Colet 2016; 21(5):1327-1338..
The goal of this article is to evaluate the observed results of the referrals of visits and outpatient exams in the city of Rio de Janeiro in the context of Brazilian sanitary federalism, demonstrating the advances, limits, and challenges indicated for management at the local level.
Methodology
This is a quantitative study that will utilize the databases of the National Registry of Health Centers (Cadastro Nacional de Estabelecimentos de Saúde, or CNES) and the National Regulatory System (Sistema Nacional e Regulação, or SISREG), both organized within the Ministry of Health, and operated by the Municipal Health Secretary in the management of their health planning areas. One of the analyses was carried out via a linkage by health center to the municipal CNES and SISREG data using the variables of CPF (taxpayer registration number) and name of the health professional, available in both databases.
CNES
As Pinto1313. Pinto LFS. Estratégias de integração e utilização de bancos de dados nacionais para avaliação de políticas de saúde no Brasil [tese]. Rio de Janeiro: Fiocruz; 2006. indicated, the CNES represents a unified standard of identification of health professionals and units. It was instituted by Decree No.376 of the SAS/Ministry of Health on October 3, 2000, issued after the agreement of the Inter-administrative Tripartite Commission (Comissão Intergestora Tripartite, or CIT) and made available for public consultation until December of 2000. It standardized the registration of health units licensed by the Unified Health System (Sistema Único de Saúde, or SUS) as well as non-licensed units (non-SUS) in all of the national territory. The Registry was based on many of the variables of the Research Project on Medical-Sanitary Assistance (AMS/IBGE) carried out in 1999 and 2002. In addition, other sources were considered: (i) forms from the Outpatient Information System of SUS (SIA-SUS), (ii) forms from the Hospital Information System of SUS (SIH-SUS), (iii) forms from the APAC Authorization System, (iv) forms from the National Health Registry, and (v) suggestions received by administrators and society in general.
SISREG
SISREG is an online administrative system of the Ministry of Health, created for the management of the entire regulatory complex, ranging from the basic network to hospital stays and complex procedures, aiming for the humanization of services, better control of the patient flow, and optimization of the use of hospital and outpatient resources specialized at the municipal, state, and federal levels, as well as private providers licensed by SUS, including university systems1414. Brasil. Departamento de Informática do SUS/ Secretaria Executiva/Ministério da Saúde, 2016. Sistema Nacional de Regulação (SISREG). [acessado 2016 jul 4]. Disponível em: http://datasus.saude.gov.br/sistemas-e-aplicativos/regulacao/sisreg
http://datasus.saude.gov.br/sistemas-e-a...
.
The municipal outpatient SISREG chooses different priority criteria to represent the desired maximum time for attending patients, assigning them to colors. “Red” are serious clinical situations and/or in need of priority scheduling up to 30 days; “yellow” are clinical situations that need priority scheduling up to 90 days; “green” patients can wait up to 180 days; and “blue” are clinical situations that do not need priority scheduling and can wait more than 180 days1515. Rio de Janeiro. SISREG – Protocolo para o Regulador. Protocolo Clínico de Critérios para Regulação de Vagas Ambulatoriais. Rio de Janeiro: Secretaria Municipal de Saúde; 2014.. Between 2011 and 2015, the number of procedures, exams, and scheduled visits had an increase of 86%, growing from 790,091 to 1,469,771, as a response to the decentralization of outpatient regulation for family doctors in each health unit. The reported proportion of procedures done in adequate time was different for each color. The difficulty of attending cases classified as “red” in an opportune time is noteworthy, varying between 30 and 50% in the period between 2011 and May of 2016. Patients prioritized as “yellow” managed to be attended between 60 and 80% of the time (Graph 1).
Distribution of the proportion of procedures, exams, and scheduled appointments carried out in adequate time in SISREG according to the priority criteria of the Municipality of Rio de Janeiro – 2011 – 2016.
For the present article, the following variables were selected: “outpatient workload” reported by CNES and “number of weekly openings” in the SISREG offered through the SMS-RJ to the municipal, state, federal, or SUS-licensed service providers, according to a set of medical and non-medical specializations eligible for regulation. A conservative estimate is that for each hour recorded in the CNES, two procedures, exams, or scheduled appointments could potentially be carried out: in other words, an average of 30 minutes per patient service. This generated the variable “number of expected consultations”.
Regionalization and Outpatient Regulation
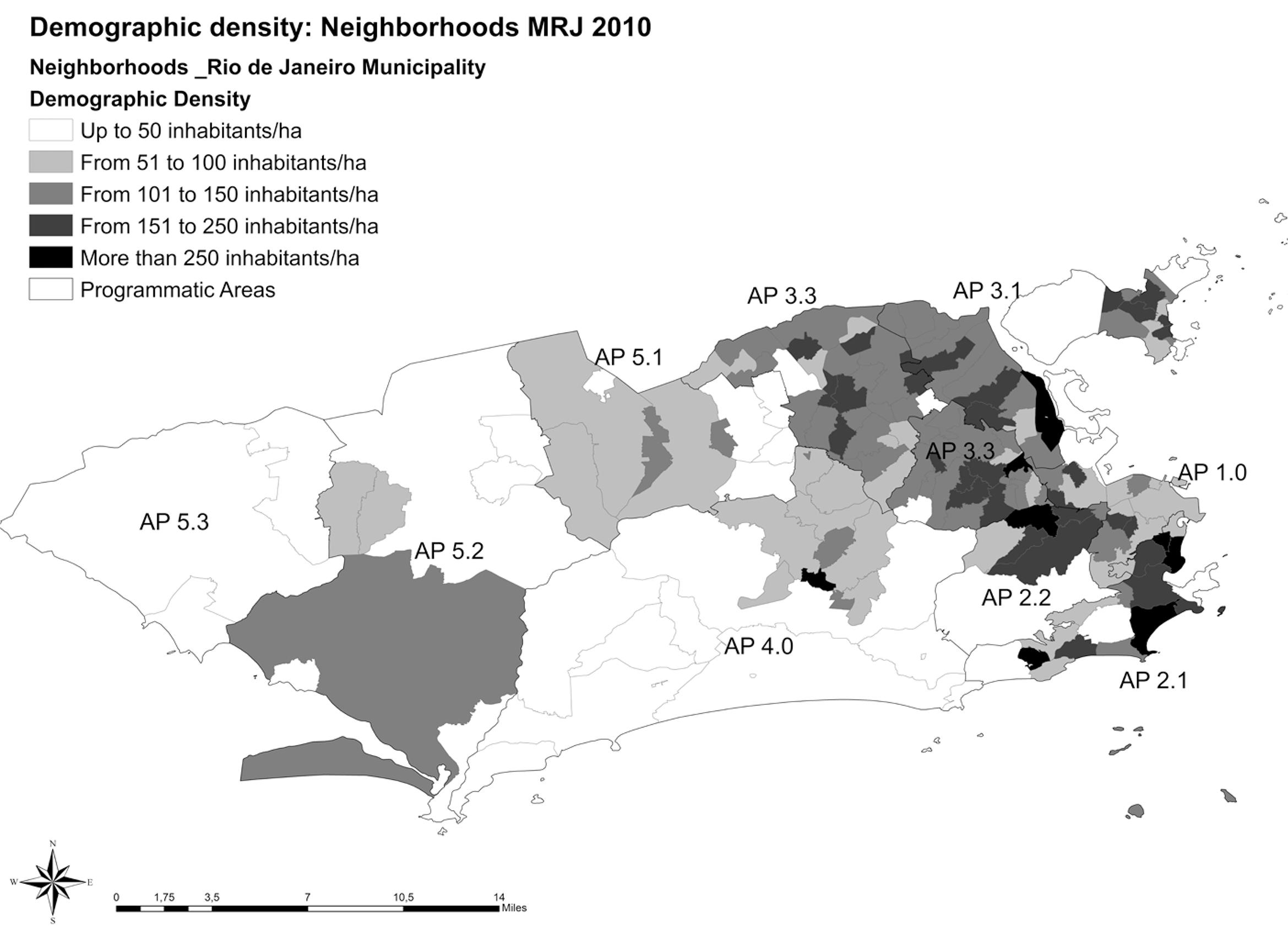
The Municipality of Rio de Janeiro is the second largest metropolis in the country in terms of population, corresponding to an area of 1,224.56km22. Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil. Rio de Janeiro: Editora Companhia das Letras; 2012., divided into administrative regions instituted by the Municipal Organic Law No.141 of December 11, 1979 and modified by Municipal Decree No.3158 on July 23, 19811616. Rio de Janeiro. Lei Orgânica Municipal nº 141, de 11 de dezembro de 1979. Diário Oficial do Município 1979; 12 dez.. The distribution of the population in the neighborhoods that comprise the Planning Areas (Áreas de Planejamento, or AP) do not lend themselves in a homogenous way to the various nuclei of population density (Figure 1).
The population densities of the PHC varied from 2,246 inhabitants/km22. Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil. Rio de Janeiro: Editora Companhia das Letras; 2012. in AP 5.3 to 21,731 inhabitants /km22. Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil. Rio de Janeiro: Editora Companhia das Letras; 2012. in AP 5.2. The largest densities after AP 5.2 are AP 2.1 with 14,094 inhabitants/km22. Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil. Rio de Janeiro: Editora Companhia das Letras; 2012. and AP 3.3 with 13,821 inhabitants /km22. Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil. Rio de Janeiro: Editora Companhia das Letras; 2012.. These values show us that there are at least three distinct groups of population density among the PHC of Rio de Janeiro, which suggests in advance the need for differentiated planning of health service offerings capable of catering to the different populations of the health regions.
The incipient nature of services offered in the SISREG of the municipality has direct implications in the efficiency of attending the user, in that the classification of risk and wait times are fundamental for the efficacy of treatment.
There will necessarily be breaks in the territorial boundaries of each AP for the referral of patients to the locales where medium to high complexity services are available, causing the movement of patients from one point to another within the city limits.
The SISREG system, when used properly, allows greater transparency of the availability of appointments, however it does not enable a regionalization of the regulated procedures offered, leaving the selection of the local where the patient should be seen up to the regulator.
The city maintains the centralized regulation and scheduling of specialized dental procedures in the Program Area Coordinating Bodies, in which it was agreed that the regulating dentists must only schedule patients in their own region. The SISREG data show that with this measure in place, the patient remains in a waiting list while there are openings in other regions, showing that a simple limitation by territory is not sufficient to reduce the wait time for attendance1818. Moura I. A Reforma da Regulação dos procedimentos odontológicos especializados no Rio de Janeiro [dissertação]. Rio de Janeiro: UFRJ; 2015..
Some authors1919. Conil EM, Giovanella L, Almeida PF. Listas de espera em sistemas públicos: da expansão da oferta para um acesso oportuno? Considerações a partir do Sistema Nacional de Saúde espanhol. Cien Saude Colet 2011; 16(6):2783-2794.,2020. Siciliani L, Verzulli R. Waiting times and socioeconomic status among elderly Europeans: evidence from SHARE. Health Econ 2009; 18(11):1295-1306. have written that the reduction of waiting periods for procedures of medium and high complexity is one of the main aspects with room for improvement in the health system. On the other hand, regulation systems that allow the movement of patients to different regions, often distant from the patient’s residence, should be accompanied by measures that address absenteeism and that strengthen the link between the health professional and the patient. Such measures insert the referencing of the patient into the coordination of care, highlighting the articulation between policy which originates from the center of the organizations and practice inside the health units.
Findings of the advances achieved
For a typical, representative month in 2015, of the total 186,326 contracted hours, there was an expected 372,652 consultations and only 45,980 were regulated: in other words, only 12.3% of the expected total consultations were made available. In this period, estimated weekly outpatient production was 437,291 procedures, exams, and consultations. There are large differences among the administrative spheres, with the municipal level being the largest provider responsible for 63.3% of appointments offered in SISREG, with 38.4% by the municipal units themselves, 24.9% by units licensed by SUS, 9% state, and federal with the least at 2.3% (Table 1).
After the linkage between the CNES and municipal SISREG variables, the selection of some specialties and procedures demonstrate great disparities between the proportion of consultations regulated by SMS-RJ in relation to the total of expected consultations, oscillating between 5.7% for physiotherapy consultations, 8.1% for gynecological consultations – surgery of low and medium risk, and 48.3% for general ophthalmology consultations (Table 2). This means that in some cases listed in Table 2, there would not be a wait, or even that the average time for carrying out the procedures would be sufficiently reduced, if the professionals had offered part of their workload through the SISREG. Therefore, we can infer that there is not a lack of specialists for attending outpatients in nearly all areas of Rio de Janeiro’s SUS. Rather, there exist artificial bottlenecks caused by the absence of regulation of the greater part of the contracted workload of the specialization. In other words, the offer of openings for regulation is severely less than the installed capacity of the healthcare units, (Column D, Table 2), which can be proven by the lack of updating the schedules of the SISREG professionals, and by the fact that outpatient production presented in the information systems (SIA) is greater than the existing supply in SISREG. The unreliability of updating the scheduling of appointments in SISREG, on the other hand, results in great variations in the average wait time over the course of months.
Findings on the observed limits and discussion of the literature
For the subgroup of selected consultations and exams (those with the greatest number of pending solicitations), the average general wait time was 80 days for a consultation and 72 days for exams (non-tabulated data). Barua2121. Barua B. Waiting your turn. Wait times for health care in Canada. 2015 Report. Fraser Institute, 2015. [acessado 2016 jul 4]. Disponível em: https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2015-report
https://www.fraserinstitute.org/studies/...
presented findings from a report on the managements of wait times in Canada, stratified by area and measuring the time in weeks. In that country, the average wait time for a family doctor to refer another specialist for a first consultation was 8.5 weeks (or approximately 60 days). Wait times are not exclusively a problem of supply, in that there exist countries that invest heavily in healthcare, beds, or doctors that have long wait times. The countries of the OECD have specific policies for the monitoring and management of wait times, with the most common of these being the adoption of mechanisms and flows that establish the guarantee of a maximum wait time, which is widely publicized in the channels of communication for the entire population2222. Organisation for Economic Co-operation and Development (OECD). Waiting Time Policies in the Health Sector: What Works? OECD Publishing, Paris, 2013. [acessado 2016 jul4]. Disponível em: http://www.oecd.org/health/waiting-times-for-elective-surgery-what-works-9789264179080-en.htm
http://www.oecd.org/health/waiting-times...
,2323. Borowitz M, Moran V, Siciliani L. A review of waiting times policies in 13 OECD countries. In: Waiting Time Policies in the Health Sector: What Works? Paris: OECD Publishing; 2013. p. 49-68.. The wait times for elective (non-emergency) procedures are one of the main preoccupations of health policy in various countries. In the Brazilian case, the lack of systematization and publicizing of these times in the majority of capital cities and states in the country is notable. The Organization for Economic Cooperation and Development (OECD) notes the importance of the systematization and divulging of this information as a principal strategy for resolving the problem2424. Siciliani L, Moran V, Borowitz M. Measuring and comparing health care waiting times in OECD countries. Paris: OECD Publishing; 2013. OECD Health Working Papers Nº 67.. Other authors2525. Richardson J, Peacock S. Will more doctors increase or decrease death rates? An econometric analysis of australian mortality statistics. Victoria: Monash University; 2003. Working Paper 137. Centre for Health Program Evaluation. emphasize that excessive access to medical services without utilization of solid scientific evidence causes more damage than benefits to the population.
In the city of Rio de Janeiro, the average wait times (lines) could be reduced and, in various exams and consultations, could be almost eliminated if the state and federal units would offer at least half of the contracted outpatient workload through the municipal SISREG. The analysis of a set of consultations and exams reveals that the existing average time for a scheduled consultation or procedure in Rio’s population oscillated between 30 days (consultation in general physiotherapy) and 123 days (consultation in reconstructive plastic surgery). On the other hand, the number of accumulated pending solicitations waiting to be scheduled varied between 439 (consultation in cardiology) up to 15,845 (consultation in general ophthalmology) (Table 3).
Discussion of challenges for local management
Brazilian sanitary federalism grants various powers and responsibilities to the municipal, state, and federal entities. In July of 2015, at the CIB-RJ No.3.470, the creation of the Unified Regulation Center (Central Unificada de Regulação, or REUNI-RJ) was agreed upon. It was determined that the coordination of the REUNI-RJ would be organized by the State Secretary of Health (SES-RJ) (paragraph 2) and would be central in the operationalization of regulation of access of the municipalities in the state of Rio to the procedures defined as strategic that are located in the Municipality of Rio de Janeiro. The SES-RJ thus came to regulate the outpatient procedures that until 2015 had been regulated by SMS-RJ, such as: oncology, radiotherapy, hematology, cardiovascular surgery, trauma and orthopedic services, neurosurgery, and strategic high-risk pre-natal care2626. Rio de Janeiro. Comissão Intergestores Bipartite (CIB). Deliberação CIB-RJ nº 3.470 de 20 de julho de 2015. Pactua a criação de uma Central Unificada de Regulação - REUNI-RJ para ordenação do acesso de serviços estratégicos localizados no município do Rio de Janeiro, 2015. [acessado 2016 jul 5]. Disponível em: http://www.cib.rj.gov.br/arquivos-para-baixar/anexos/1865--292/file.html acessado
http://www.cib.rj.gov.br/arquivos-para-b...
,2727. Rio de Janeiro. Comissão Intergestores Bipartite (CIB). Deliberação CIB-RJ nº 3.534 de 18 de setembro de 2015. Agrega procedimentos estratégicos a serem regulados exclusivamente pela REUNI/RJ, 2015b. [acessado 2016 jul5]. Disponível em: http://www.cib.rj.gov.br/arquivos-para-baixar/anexos/1905--329/file.html
http://www.cib.rj.gov.br/arquivos-para-b...
.
The creation of a new regulation center under the administration of another Secretary (at the state level), and the use of an information system different from the SISREG of the Ministry of Health, caused reports of a disoriented user population of Rio’s SUS, which since the second semester of 2012 would experience the organized flow of access in the city of Rio de Janeiro established by the PHC. This also impaired the integration of necessary data for planning and management at the local level, principally among the procedures that had come to be regulated by the State Secretary of Health in the municipality of Rio de Janeiro.
For example, this disaggregation is an obstacle to studies of the supply of contracting needs from private providers to complement the services not available through Rio SUS, as well as not making the professionals responsible for accompanying the progress of the users in carrying out these regulated procedures. This follow-up should be made by Primary Healthcare of the municipality, which is the level of care closest to the people themselves, and which coordinates care and maintains the professional-user-family link over time.
At the Municipal Health Secretary of Rio de Janeiro, users receive counsel from the primary healthcare unit regarding the confirmation and scheduling of their consultation. This responsibility for accompanying the process is facilitated by the sending of a Short Message Service (SMS) for each appointment carried out by SISREG and by the local tool “Where to be get help,” developed to territorialize the entire population of the city, even those without ESF2828. Rio de Janeiro. Onde ser Atendido? Rio de Janeiro: Superintendência de Atenção Primária/ Subsecretaria de Atenção Primária, Vigilância e Promoção da Saúde, Secretaria Municipal de Saúde, 2012. [acessado 2016 jul 6]. Disponível em: http://www.rio.rj.gov.br/web/sms/onde-ser-atendido
http://www.rio.rj.gov.br/web/sms/onde-se...
, informing each person or family of their reference unit in the PHC. Such management processes are not available in the State Regulatory System (Sistema Estadual de Regulação, or SER), jeopardizing access to information and coordination of care. However, even with this tool, one of the limitations of the current SISREG is the issue of the difficulty of territorial parameterization among the units that offer appointments and the locale of residence of the population, which impedes the geographic accessibility of the users. In this way, for example, a person that lives in the west zone of the city can be scheduled for an exam in the downtown city center of Rio, which involves a distance of 63 kilometers and possible absenteeism.
Perspectives
As we can see, the greatest challenges for the Municipal Secretary of Health of Rio de Janeiro is in the reduction of wait times associated with the areas of ophthalmology, urology, cardiology, gastroenterology, radiology, angiology, neurology, general surgery, pediatric surgery, gynecological surgery, vascular surgery, and general physiotherapy. A global analysis of this and other sets of specialties that can supply appointments for scheduling reveals that more than 80% of professionals registered with CNES do not offer any appointments whatsoever through SMS-RJ. Therefore, if the municipal manager could have fulfilled the role advocated by SUS to be the “one and only” manager for at least half the contracted outpatient workload together with the professionals registered in CNES, and if this could be allocated to appointments offered to the state and federal units in the municipal SISREG, the wait times would be drastically reduced and, in some specializations, even eliminated. Another portion of the workload should be made available to the municipalities in the interior of the state of Rio de Janeiro. After all, this attribution of responsibility, follow-up, and coordination of care of the municipalities in primary healthcare belongs to the municipal manager, and at some point must be politically and economically reinforced, agreed upon by the managers of the three administrative spheres, without jeopardizing the third and fourth-tier health establishments that comprise the network of healthcare and training for the SUS health professionals.
Health resources are scarce, and the Rio population can be better tended to with specialized outpatient referrals if, as Temporão2929. Temporão JG. Discurso de posse no cargo de Ministro da Saúde em 19 de março de 2007. Informativo da Associação Brasileira de Pós-graduação em Saúde Coletiva (ABRASCO) 2007; 24(98):6-10. has argued, there was a new federal agreement for primary healthcare at the three levels of management with a genuine allocation of at least half of the contracted outpatient workload for the health professionals together with SUS in a Unified Regulation System in the capital of Rio de Janeiro. The supply earmarked for the other municipalities in the state of Rio de Janeiro can have regulation handled by the State Secretary of Health among those with low institutional capacity for healthcare management. To understand the problem- to decipher, map out, and publicize the wait time of the municipal health network of Rio de Janeiro – helps to understand decades of disorganization in the outpatient queues of local SUS, considering the installed capacity of public services in this city that once was the capital of the country, and which inherited an enormous hospital network, while preventing this “riddle” from paralyzing action on the part of local managers who seek to improve access for Rio’s citizens.
Referências
-
1Lassance A. Federalismo no Brasil: trajetória institucional e alternativas para um novo patamar de construção do Estado. In: Linhares PTF, Mendes CC, Lassance A, organizadores. Federalismo à Brasileira: questões para discussão Brasília: IPEA; 2012. p. 23-36. v. 8. (Série: Diálogos para o Desenvolvimento).
-
2Leal VN. Coronelismo, enxada e voto: o município e o regime representativo no Brasil Rio de Janeiro: Editora Companhia das Letras; 2012.
-
3Brasil. Ministério da Saúde (MS). Secretaria Executiva. Departamento de Apoio à Descentralização. Coordenação de Integração Programática. Regionalização solidária e cooperativa: orientações para sua implementação no SUS Brasília: MS; 2006. (Série Pactos pela Saúde 2006, v. 3).
-
4Albuquerque Netto JA. O direito à saúde no federalismo: repartição de competência na assistência farmacêutica [monografia]. Brasília: Instituto Brasiliense de Direito Público; 2010.
-
5Instituto Brasileiro de Geografia e Estatística (IBGE). Estimativas populacionais para os municípios brasileiros em 01.07.2014 Diretoria de Pesquisas - DPE -Coordenação de População e Indicadores Sociais – COPIS, 2014. [acessado 2016 jul 2]. Disponível em: http://www.ibge.gov.br/home/estatistica/populacao/estimativa2014/estimativa_dou.shtm
» http://www.ibge.gov.br/home/estatistica/populacao/estimativa2014/estimativa_dou.shtm -
6Brasil. Ministério da Saúde (MS). Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Política nacional de atenção básica Brasília: MS; 2006. (Série A. Normas e Manuais Técnicos. Série Pactos pela Saúde. v. 4).
-
7Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica (PNAB) Brasília: MS; 2012. (Série E. Legislação em Saúde).
-
8Mendonça MHM, Martins MIC, Giovanella L, Escorel S. Desafios para gestão do trabalho a partir de experiências exitosas de expansão da Estratégia de Saúde da Família. Cien Saude Colet 2010; 15(5):2355-2365.
-
9Costa NR. A Estratégia de Saúde da Família, a atenção primária e o desafio das metrópoles brasileiras. Cien Saude Colet 2016; 21(5):1389-1398.
-
10Starfield B. Atenção primária: equilíbrio entre necessidades de saúde, serviços e tecnologia Brasília: Unesco, Ministério da Saúde; 2002.
-
11Calnan M, Hutten J, Tiljak H. The challenge of coordination: the role of primary care professionals in promoting integration across the interface. In: Saltman RB, Rico A, Boerma W, editors. Primary care in the driver's seat? organizational reform in European primary care Maidenhead, New York: Open University Press; 2006. p. 85-104.
-
12Soranz D, Pinto LF, Penna GO. Eixos e a Reforma dos Cuidados em Atenção Primária em Saúde (RCPHC) na cidade do Rio de Janeiro, Brasil. Cien Saude Colet 2016; 21(5):1327-1338.
-
13Pinto LFS. Estratégias de integração e utilização de bancos de dados nacionais para avaliação de políticas de saúde no Brasil [tese]. Rio de Janeiro: Fiocruz; 2006.
-
14Brasil. Departamento de Informática do SUS/ Secretaria Executiva/Ministério da Saúde, 2016. Sistema Nacional de Regulação (SISREG) [acessado 2016 jul 4]. Disponível em: http://datasus.saude.gov.br/sistemas-e-aplicativos/regulacao/sisreg
» http://datasus.saude.gov.br/sistemas-e-aplicativos/regulacao/sisreg -
15Rio de Janeiro. SISREG – Protocolo para o Regulador. Protocolo Clínico de Critérios para Regulação de Vagas Ambulatoriais Rio de Janeiro: Secretaria Municipal de Saúde; 2014.
-
16Rio de Janeiro. Lei Orgânica Municipal nº 141, de 11 de dezembro de 1979. Diário Oficial do Município 1979; 12 dez.
-
17Instituto Brasileiro de Geografia e Estatística (IBGE). População Total: Brasil em 2010 [acessado 2015 fev 2]. Disponível em: http://www.ibge.gov.br
» http://www.ibge.gov.br -
18Moura I. A Reforma da Regulação dos procedimentos odontológicos especializados no Rio de Janeiro [dissertação]. Rio de Janeiro: UFRJ; 2015.
-
19Conil EM, Giovanella L, Almeida PF. Listas de espera em sistemas públicos: da expansão da oferta para um acesso oportuno? Considerações a partir do Sistema Nacional de Saúde espanhol. Cien Saude Colet 2011; 16(6):2783-2794.
-
20Siciliani L, Verzulli R. Waiting times and socioeconomic status among elderly Europeans: evidence from SHARE. Health Econ 2009; 18(11):1295-1306.
-
21Barua B. Waiting your turn. Wait times for health care in Canada. 2015 Report. Fraser Institute, 2015. [acessado 2016 jul 4]. Disponível em: https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2015-report
» https://www.fraserinstitute.org/studies/waiting-your-turn-wait-times-for-health-care-in-canada-2015-report -
22Organisation for Economic Co-operation and Development (OECD). Waiting Time Policies in the Health Sector: What Works? OECD Publishing, Paris, 2013. [acessado 2016 jul4]. Disponível em: http://www.oecd.org/health/waiting-times-for-elective-surgery-what-works-9789264179080-en.htm
» http://www.oecd.org/health/waiting-times-for-elective-surgery-what-works-9789264179080-en.htm -
23Borowitz M, Moran V, Siciliani L. A review of waiting times policies in 13 OECD countries. In: Waiting Time Policies in the Health Sector: What Works? Paris: OECD Publishing; 2013. p. 49-68.
-
24Siciliani L, Moran V, Borowitz M. Measuring and comparing health care waiting times in OECD countries Paris: OECD Publishing; 2013. OECD Health Working Papers Nº 67.
-
25Richardson J, Peacock S. Will more doctors increase or decrease death rates? An econometric analysis of australian mortality statistics Victoria: Monash University; 2003. Working Paper 137. Centre for Health Program Evaluation.
-
26Rio de Janeiro. Comissão Intergestores Bipartite (CIB). Deliberação CIB-RJ nº 3.470 de 20 de julho de 2015. Pactua a criação de uma Central Unificada de Regulação - REUNI-RJ para ordenação do acesso de serviços estratégicos localizados no município do Rio de Janeiro, 2015. [acessado 2016 jul 5]. Disponível em: http://www.cib.rj.gov.br/arquivos-para-baixar/anexos/1865--292/file.html acessado
» http://www.cib.rj.gov.br/arquivos-para-baixar/anexos/1865--292/file.html -
27Rio de Janeiro. Comissão Intergestores Bipartite (CIB). Deliberação CIB-RJ nº 3.534 de 18 de setembro de 2015. Agrega procedimentos estratégicos a serem regulados exclusivamente pela REUNI/RJ, 2015b. [acessado 2016 jul5]. Disponível em: http://www.cib.rj.gov.br/arquivos-para-baixar/anexos/1905--329/file.html
» http://www.cib.rj.gov.br/arquivos-para-baixar/anexos/1905--329/file.html -
28Rio de Janeiro. Onde ser Atendido? Rio de Janeiro: Superintendência de Atenção Primária/ Subsecretaria de Atenção Primária, Vigilância e Promoção da Saúde, Secretaria Municipal de Saúde, 2012. [acessado 2016 jul 6]. Disponível em: http://www.rio.rj.gov.br/web/sms/onde-ser-atendido
» http://www.rio.rj.gov.br/web/sms/onde-ser-atendido -
29Temporão JG. Discurso de posse no cargo de Ministro da Saúde em 19 de março de 2007. Informativo da Associação Brasileira de Pós-graduação em Saúde Coletiva (ABRASCO) 2007; 24(98):6-10.
Publication Dates
-
Publication in this collection
Apr 2017
History
-
Received
28 May 2016 -
Reviewed
04 Aug 2016 -
Accepted
23 Sept 2016


 Source: Municipal SISREG, Rio de Janeiro, 2016.Note: The data for 2016 refers to the portion of the year until May of 2016.
Source: Municipal SISREG, Rio de Janeiro, 2016.Note: The data for 2016 refers to the portion of the year until May of 2016.
 Source: IBGE, population estimate using the 2010 census on February 2, 201517.
Source: IBGE, population estimate using the 2010 census on February 2, 201517.