Abstract
We aimed to analyze the geographic distribution, the structure of healthcare services and the human resources of all units of the Sistema Único de Saúde (SUS - the Unified Health System) that provide sexual and reproductive health (SRH) services to the adolescent population in the second largest city in Brazil. We conducted a cross-sectional study with geographical mapping and data collection through a questionnaire applied in person with coordinators of the units or their representatives in 147 outpatient clinics in Rio de Janeiro that have SSR services. We found that in over 90% of the units, adolescents are treated together with the adult population, without particular shifts or rooms for this age group. In more than 10% of services, treatment is only provided with the presence of the guardian. In cases of sexual violence, this proportion is 34%. Specific educational activities for this age group are only carried out in 12.9% of units and less than one third of doctors had received some kind of training to deal with adolescent health. In conclusion, despite the wide geographic distribution of health facilities, the structure of care and the human resources do not meet the specific needs of adolescents.
Sexual and reproductive health; Adolescent; Health services accessibility
Resumo
Objetivamos analisar a distribuição geográfica, a estrutura de atendimento e os recursos humanos das unidades do Sistema Único de Saúde (SUS) que prestam serviços em saúde sexual e reprodutiva (SSR) à população adolescente, na segunda maior cidade do Brasil. Realizamos estudo transversal com mapeamento geográfico e coleta de dados por meio de questionário aplicado aos coordenadores, em todas as 147 unidades ambulatoriais do Rio de Janeiro, dispostas ao atendimento em SSR. Verificamos que todas as Regiões Administrativas (RA) desse município dispõem de unidades de atendimento para adolescentes, entretanto, em mais de 90% delas, eles são atendidos juntamente com a população adulta, sem turnos ou salas específicas. Em mais de 10% dos serviços, a assistência só é dada na presença do responsável. Em casos de violência sexual a proporção mostrou-se ainda maior, chegando a atingir 34% dos casos. Em apenas 12,9% das unidades são realizadas atividades educativas direcionadas a adolescentes e constatou-se que menos de 1/3 dos médicos estava capacitado para lidar com a saúde do adolescente. Em conclusão, apesar da larga distribuição geográfica das unidades de saúde, a estrutura do atendimento e os recursos humanos não atendem a contento as especificidades do público adolescente.
Saúde sexual e reprodutiva; Adolescente; Acesso aos serviços de saúde
Introduction
Data from the 2010 census of the Instituto Brasileiro de Geografia e Estatística (IBGE - Brazilian Institute of Geography and Statistics)11. Instituto Brasileiro de Geografia e Estatística (IBGE). Censo Demográfico 2010. Características da População e dos Domicílios: Resultados do universo. [acessado 2014 jun 01]. Disponível em: http://www.ibge.gov.br
http://www.ibge.gov.br...
confirms that 17.9% of the Brazilian population consists of individuals aged 10-19, the age group that represents adolescence, as defined by the World Organization Health22. World Health Organization (WHO). Young People´s Health - a Challenge for Society. Report of a WHO Study Group on Young People and Health for All. Technical Report Series 731. Geneva: WHO; 1986. [acessado 2014 jun 1]. Disponível em: http://apps.who.int/iris/bitstream/10665/41720/1/WHO_TRS_731.pdf
http://apps.who.int/iris/bitstream/10665...
. In the municipality of Rio de Janeiro, the proportion is a little lower, representing 14% of the total11. Instituto Brasileiro de Geografia e Estatística (IBGE). Censo Demográfico 2010. Características da População e dos Domicílios: Resultados do universo. [acessado 2014 jun 01]. Disponível em: http://www.ibge.gov.br
http://www.ibge.gov.br...
.
It is known that this particular age group requires differentiated sexual and reproductive health (SRH) care33. Mibzvo MT, Zaidi S. Addressing critical gaps in achieving universal access to sexual and reproductive health (SRH): the case for improving adolescent SRH, preventing unsafe abortion, and enhancing linkages between SRH and HIV interventions. Int J Gynaecol Obstet 2010; 110(Supl.):S3-S6.. However, in seeking these services, adolescents encounter obstacles in addition to those common among other age groups. Two decades ago, psychosocial barriers were identified as playing a significant role, hindering the access of this population to health care units44. Knishkowy B, Palti H. GAPS (AMA Guidelines for Adolescent Preventive Services). Where are the gaps? Arch Pediatr Adolesc Med 1997;151(2):123-128.. Some of the barriers included: fear of diagnosis, preferences for whether the health professional was a man or woman, and an inability to seek care without the presence of a guardian. It was these psychological and / or cultural issues that led potential users to avoid visiting health services55. Bertrand JT, Hardee K, Magnani RJ, Angle MA. Access, quality of care and medical barriers in family planning programs. Int Fam Plan Perspect 1995; 21(2):64-69..
In 2002, the World Health Organization (WHO) proposed to create “youth-friendly” services, an approach directed specifically at this group, with the goal of tailoring services towards young people66. World Health Organization (WHO). Adolescent friendly health services: an agenda for change. Geneva: WHO; 2002. [acessado 2014 nov 30]. Disponível em: http://www.who.int/maternal_child_adolescent/documents/fch_cah_02_14/en/
http://www.who.int/maternal_child_adoles...
. To make this possible, such services were offered at different times and a series of trained professionals were identified for dealing with adolescents, so that young people would feel welcomed into such services while at the same time their autonomy was respected.
Nonetheless, recent studies demonstrate that there are still poor results in sexual and reproductive health services for the population in their second decade of life, suggesting important lacunas in healthcare for this age group77. Tylee A, Haller DM, Graham T, Churchill R, Sanci LA. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet 2007; 369(9572):1565-1573.,88. Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, Patton GC. Adolescence: a foundation for future health. Lancet 2012; 379(9826):1630-1640.. Despite the overall decline observed in maternal mortality rates in adolescents, complications related to pregnancy and childbirth are still the second leading cause of death in 15 to 19 year-old girls99. World Health Organization (WHO). Health for the World’s Adolescents. A second chance in the second decade. Geneva: WHO; 2014. [acessado 2016 mar 03]. Disponível em: http://apps.who.int/adolescent/second-decade/
http://apps.who.int/adolescent/second-de...
. In addition, there is a high STD / AIDS rate among adolescents and young people in Brazil and in less developed countries1010. Brasil. Ministério da Saúde (MS). Boletim epidemiológico HIV-Aids. Brasília: MS; 2014. [acessado 2016 mar 3]. Disponível em: http://www.aids.gov.br/sites/default/files/anexos/publicacao/2014/56677/boletim_2014_final_pdf_15565.pdf
http://www.aids.gov.br/sites/default/fil...
,1111. Hindin MJ, Fatusi AO. Adolescent Sexual and Reproductive Health in Developing Countries: An Overview of Trends and Interventions. Int Perspect Sex Reprod Health 2009; 35(2):58-62..
The municipality of Rio de Janeiro is the second most populous city in Brazil and in 1999 had 78 clinical service units within the ‘Sistema Único de Saúde’ (SUS), 49 of which were taking part in the ‘Programa de Saúde do Adolescente’ (PROSAD - Adolescent Health Care Program)1212. Brasil. Ministério da Saúde (MS). Programa de Saúde do Adolescente - Bases Programáticas. 2ª ed. Brasília: MS; 1996. [acessado 2014 nov 30]. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/cd03_05.pdf
http://bvsms.saude.gov.br/bvs/publicacoe...
, an initiative directed at this age group1313. Ruzany MH, Andrade CL, Esteves MA, Pina MF, Szwarcwald CL. Avaliação das condições de atendimento do Programa de Saúde do Adolescente no Município do Rio de Janeiro. Cad Saude Publica 2002; 18(3):639-649.. In 2002, there were found to be 100 units that carried out at least one activity aimed at adolescents, such as specific service shifts, group activities and miscellaneous projects1414. Branco VMC. Os sentidos da saúde do adolescente para os profissionais [dissertação]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 2002..
From 1998 onwards, the ‘Estratégia de Saúde da Família’ (ESF - Family Health Strategy)1515. Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica. Brasília: MS; 2012., a government program aimed at meeting the health demands of the population in a broader and more comprehensive manner, was rolled out as the Ministry of Health’s main policy for restructuring the healthcare model around primary healthcare. These actions, essential for the healthcare of all ages of the population, are nonetheless not tailored to the specific needs of adolescents1616. Fonseca DC, Ozella S. As concepções de adolescência construídas por profissionais da Estratégia de Saúde da Família (ESF). Interface (Botucatu) 2010;14(33):411-424.. Recent studies have shown that adolescents are an ‘invisible’ group within the context of the ESF and are treated just for very specific issues, particularly those that involve greater risks, including pregnancies, STDs and drug use1717. Ventura M, Corrêa S. Adolescência, sexualidade e reprodução: construções culturais, controvérsias normativas, alternativas interpretativas. Cad Saude Publica 2006; 22(7):1505-1509.,1818. Osis MJD, Faúndes A, Makuch MY, Mello MB, Souza MH, Araújo MJO. Atenção ao planejamento familiar no Brasil hoje: reflexões sobre os resultados de uma pesquisa. Cad Saude Publica 2006; 22(11):2481-2490..
In 2012, data from Rio de Janeiro on pregnancy among adolescents, one of the most frequently used indicators for SRH, pointed to a rate of 16.8% adolescent mothers. At the same time, in some areas of the city this number was over 30%, raising questions about the factors behind such a difference1919. Rio de Janeiro. Secretaria Municipal de Saúde (SMS). Número de nascidos vivos, segundo a idade da mãe segundo área de planejamento (AP) e região administrativa (RA) de residência. Rio de Janeiro: SMS; 2012. [acessado 2014 nov 30]. Disponível em: http://www.saude.rio.rj.gov.br
http://www.saude.rio.rj.gov.br...
. The rate of pregnancy in adolescence is calculated by dividing the total number of live births among mothers under the age of 20 by the total number of live births. It is noteworthy that although women’s fertility has come down in recent years, it remains high in the 15-19 age group. According to the 2006 National Demographics and Health Survey for Children and Women (PNDS), the reproductive process in Brazil was found to be happening at a younger age. The fertility of younger women (15 to 19) in 2006, now represents 23% of the total rate, in contrast to 17% in the year 19962020. Brasil. Ministério da Saúde (MS). Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher. Brasília: MS; 2006. [acessado 2016 mar 17]. Disponível em: http://bvsms.saude.gov.br/bvs/pnds/index.php
http://bvsms.saude.gov.br/bvs/pnds/index...
.
On the other hand, STD rates among young people are high and the dynamic profile of the AIDS epidemic in the 13 to 19 range is peculiar, with a greater burden among women compared with what is found for other age groups, and increased incidence rates among men who have sex with men1010. Brasil. Ministério da Saúde (MS). Boletim epidemiológico HIV-Aids. Brasília: MS; 2014. [acessado 2016 mar 3]. Disponível em: http://www.aids.gov.br/sites/default/files/anexos/publicacao/2014/56677/boletim_2014_final_pdf_15565.pdf
http://www.aids.gov.br/sites/default/fil...
,2121. Taquette SR, Matos HJ, Rodrigues AO, Bortolotti LR, Amorim E. A epidemia de Aids em adolescentes de 13 a 19 anos no município do Rio de Janeiro: descrição espaço-temporal. Rev Soc Bras Med Trop 2011; 44(4):467-470..
Thus, this study aimed to analyze the geographical distribution, the structure of healthcare and the human resources in SUS units offering clinical SRH care to adolescents in the municipality of Rio de Janeiro.
Methods
A cross-sectional study was carried out based on data gathered at all of the clinical units in Rio de Janeiro that provided an SRH service in 2011. We used the global positioning system (GPS) for the geographical location and applied in-person questionnaires with coordinators or representatives at a date scheduled in advance. The questionnaire was comprised of 13 sections including: structure and registration data of the units, activities developed (including education), human resources for adolescent care (including the number of doctors), training of professionals in adolescent health (considering any training, regardless of duration), type of care provided in SRH (prenatal, postnatal, gynecology, STD, AIDS and sexual violence), laboratory tests performed, distribution of supplies, medicines and contraceptives, as well as the ethical aspects of care (requiring the presence of a guardian for marking or carrying out the consultation). Census data from the Brazilian Institute of Geography and Statistics (IBGE)11. Instituto Brasileiro de Geografia e Estatística (IBGE). Censo Demográfico 2010. Características da População e dos Domicílios: Resultados do universo. [acessado 2014 jun 01]. Disponível em: http://www.ibge.gov.br
http://www.ibge.gov.br...
were used to collect information about the number of adolescents; and data about the 2010 Human Development Index (HDI) were obtained from the United Nations Development Programme (UNDP)2222. Programa das Nações Unidas para o Desenvolvimento (PNUD). Ranking IDHM dos Municípios, 2010. Brasília: PNUD; 2013. [acessado 2015 mar 30]. Disponível em: http://www.pnud.org.br/atlas/ranking/Ranking-IDHM-Municipios-2010.aspx#
http://www.pnud.org.br/atlas/ranking/Ran...
.
The research process involved the participation of interviewers who were trained and tested prior to beginning data collection. The internal consistency of the questionnaire was satisfactory, with a Cronbach’s alpha coefficient of 0.7. This factor is particularly relevant because it measures the internal consistency of the survey instrument by identifying the degree to which presented items are interrelated, thereby providing an estimate of reliability2323. Green SB, Lissitz RW, Mulaik SA. Limitations of coefficient alpha as an index of test unidimensionality. Educ Psychol Meas 1977; 37(4):827-838..
The absolute and relative frequencies, mean, standard deviation and position measurements were calculated to describe the distribution of units in the city and its characteristics. To check the availability of care for adolescents in health units, we decided to assess the number of adolescents per doctor and not the number of health units per adolescent, given that units with a greater number of physicians have a higher service capacity. We used linear correlation and a linear regression model, adjusted for HDI, to investigate the relationship between the quantity of adolescents (10-19 years) and the number of doctors per administrative region (RA). The analyses were carried out using the Epi-Info 3.5.2 program, R-Project version 3.2.2 and ArcGIS 10.0.
The study complies with the ethical standards contained in the Resolution of the National Health Council, CNS 466/2012, and was approved by the Research Ethics Committees of the Municipal Health Secretariat of Rio de Janeiro and of Rio de Janeiro State University.
Results
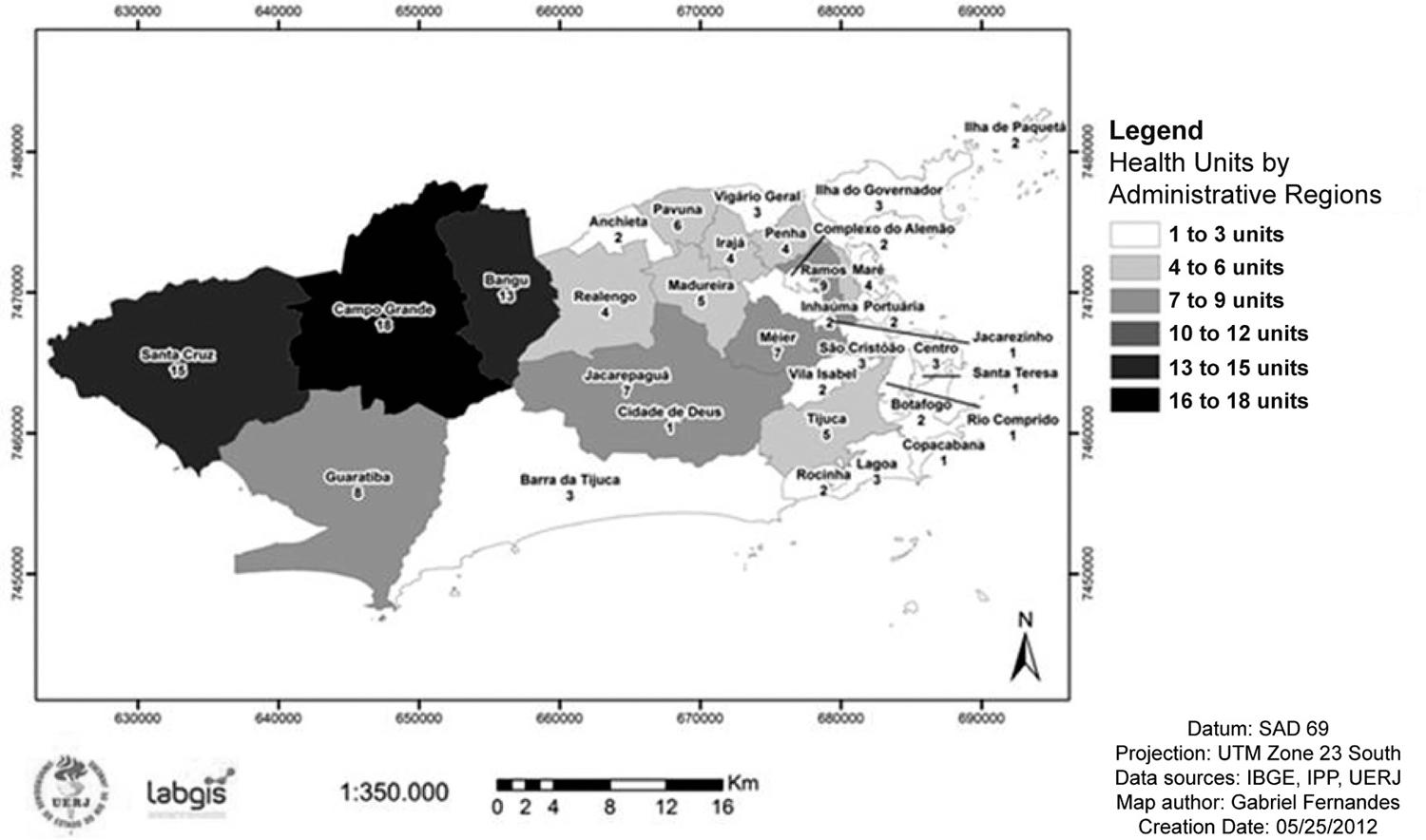
The city of Rio de Janeiro is divided into five planning areas (AP), which break down into 10 sub-areas, 33 administrative regions (RA) and 160 districts. Of the 229 units providing clinical treatment within the SUS, 148 offer sexual and reproductive health services. It was not possible to obtain information at one of the units, due to difficulties in gaining authorization for research. In this way, 147 units were analyzed. The location of the assessed health units is demonstrated in Figure 1. All RAs were found to have health units that treat adolescents. Thirty-one per cent (46/148) of all units are concentrated in the RAs of Bangu, Campo Grande and Santa Cruz. Some RAs have only one health unit (Rio Comprido, Santa Teresa, Copacabana and Jacarezinho).
Heath units of SUS in municipality of Rio de Janeiro with reproductive health services to adolcescents (population between 10 and 19 years).
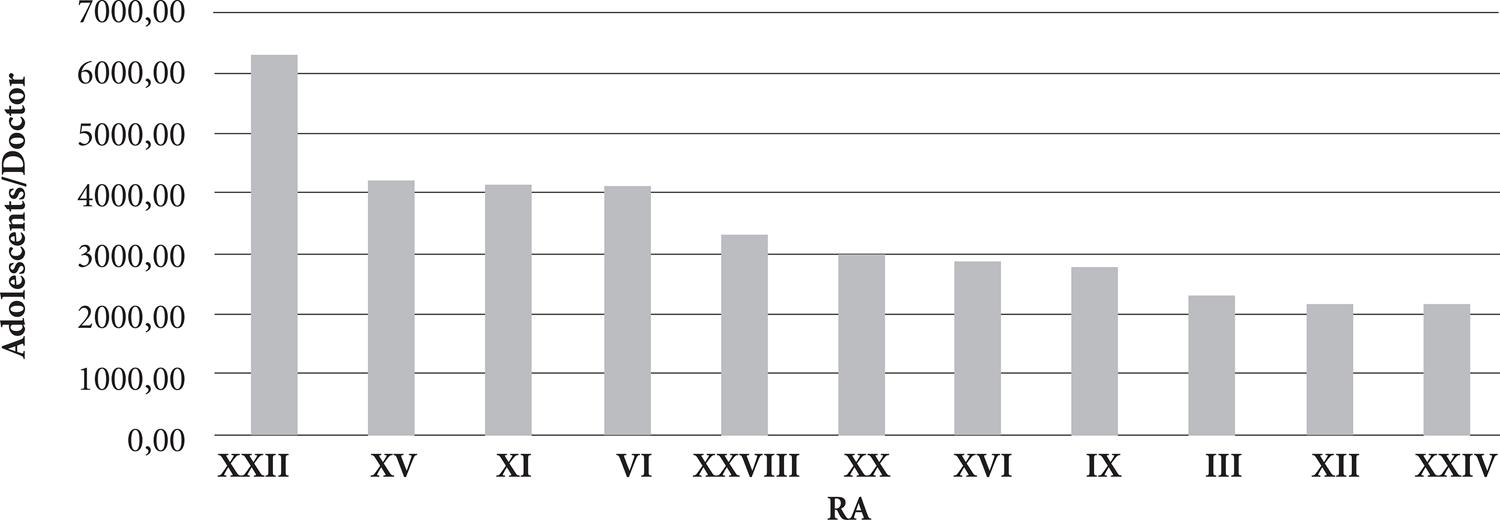
Figure 2 shows the distribution of RAs with more than 200 adolescents per physician. In four (12%) RAs (Anchieta, Madureira, Penha and Lagoa), the number of adolescents living in the area for every doctor working in the health unit is over 4,000. In six (18%) RAs (Ilha do Governador, Jacarepagua, Jacarezinho, Inhaúma, Barra da Tijuca and Vigário Geral), the number of adolescents per doctor is over 2,000. In only 10 (30%) of the RAs (Ilha de Paquetá, Cidade de Deus, Guaratiba, Rocinha, São Cristóvão, Ramos, Santa Teresa, Campo Grande and Portuária), the number of adolescents per doctor is below 1.000.
Figure 3 shows the associations of RAs with the number of adolescents, number of doctors, and HDI. Diagrams A and B represent the HDI relations with the number of adolescents and the number of physicians, respectively. These diagrams suggest that the lower the HDI, the greater the population of adolescents and doctors available in units (p-value > 0.05). Diagram C shows a positive correlation between the number of doctors and the number of adolescents and indicates that the higher the adolescent population, the greater the number of doctors per RA (= 0.76; p-value < 0.0001). Finally, Diagram D shows the linear relationship between the number of adolescents and the number of doctors adjusted by HDI. Furthermore, this diagram presents the average number of adolescents per physician, considering the HDI, and corresponds to 977.34 (IC 95% 638.98-1315.71; p-value < 0.0001). It should be noted that certain units have up to 38 doctors and others have only one or even no professionals, as we observed in two of them.
Relationship between: A) HDI and number of adolescents, B) HDI and number of physicians, C) number of physicians and number of adolescents, D) Average number of adolescents (Ŷ) and number of doctors (X1) adjusted by HDI (X2) according to the administrative region of the city of Rio de Janeiro (Ŷ = 209.25+977.34 X1+11711.82 X2).
Regarding the services available in the units, prenatal and postnatal services and the distribution of supplies, medicines and contraceptives were found to be available in more than 95% of units. On the other hand, gynecological care was found in 80.4% (IC 95% 73.1-86.5) of the units, orientation in sexuality in 86.5% (IC 95% 79.9-91.5), sexual violence in 65% (IC 95% 56.6-72.5) and AIDS in only 45.3% (IC 95% 37.1-53.7). Both services aimed at the general population and specific to adolescents are described in Table 1.
Regarding the availability of laboratory tests, we observed disparities in the results: while syphilis and Hepatitis B are tested in more than 90% of the units, HIV testing is performed in fewer than 40% of them. And with regard to the pregnancy diagnostic test, this is done in approximately 80% of services.
Specific educational activities for this age group take place in 12.9% (19/147) of units. A lack of capacity and precariousness of human resources (HR) were highlighted as the principal barriers to the development of work with adolescents in 50.3% and 57.1% of units respectively. Only 28.8% of doctors reported any type of capacity for treating this population group.
Table 2 shows the percentage of services that impose barriers to adolescent access, in that they require the presence of a guardian for marking the consultation or for their own care. In 34.4% of units, support for cases of sexual violence was found to only be provided in the presence of a guardian.
Discussion
This is the first study to include all health units of the SUS, detailing their geographical positioning, service structure and human resources that provide SRH services to adolescents in the second largest city in Brazil.
Accessibility is one of eight components considered to be important in adolescent care2424. Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013; 52(6):670-681.. With particular regard to the location and distribution of services, health units are actually more concentrated in areas where there is a larger population of adolescents. The greater the number of adolescents, the higher the number of physicians in the RA (Figures 1 and 3). However, when assessing the association between the number of adolescents and doctors adjusted by HDI, there is a ratio of approximately 977 adolescents for each doctor, indicating a small number of doctors to the adolescent population (Figure 3). The literature is not clear in establishing the optimal number of adolescents or even adults for each doctor. However, the Department of Primary Care of the Brazilian Ministry of Health recommends that you have a family health team to a maximum of every 4,000 inhabitants, preferably 3,000. Since 17.9% of the population is composed of adolescents, each team should be responsible for about 716 individuals of this age2525. Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica. Brasília: MS; 2012. [acessado 2014 set 13]. Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf
http://189.28.128.100/dab/docs/publicaco...
. According to Brazilian law, service coverage should be universal, i.e. available to the entire population2626. Brasil. Lei no 8.080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União 1990; 19 set., even though not every adolescent residing in regions analyzed use public health services2727. Jairnilson P, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet 2011; 77(9779):1778-1797.. Moreover, it is necessary bearing in mind that doctors at the health units are not geared exclusively to adolescent care.
It is worth mentioning that inputs that are fundamental to SRH services, including male condoms and oral contraceptives, were found to be distributed in most units. On the other hand, the lower coverage of additional tests may be one of the factors contributing to increasing levels of AIDS among adolescents. The early diagnosis of a positive STD or HIV diagnosis is considered to be an important coping measure for the AIDS epidemic. Proof of this is that developed countries that have adopted this policy – such as France – have shown very low incidence rates compared to those found in Brazil2828. Taquette SR. Epidemia de HIV/Aids em adolescentes no Brasil e na França: semelhanças e diferenças. Saude Soc 2013; 22(2):618-628..
At the same time, an analysis of how the units function clearly points to an absence of health policies aimed at adolescents2929. Ferrari RAP, Thomson Z, Melchior R. Atenção à saúde dos adolescentes: percepção dos médicos e enfermeiros das equipes de saúde da família. Cad Saude Publica 2006; 22(11):2491-2495.. The Ministry of Health says it is important to create or adapt environments to the care of this age group in order to make them more comfortable, since young people generally feel shy or embarrassed when they are among children and / or adults, in waiting rooms. This can be seen as a major barrier to demand for health services among adolescents3030. Brasil. Ministério da Saúde (MS). Saúde Integral de Adolescentes e Jovens. Orientações para a Organização de Serviços de Saúde. Brasília: MS; 2005. [acessado 2016 abr 7]. Disponível em: http://files.bvs.br/upload/MS/2005/Brasil_Saude_integral.pdf
http://files.bvs.br/upload/MS/2005/Brasi...
.
Fewer than 10% of SRH services in Rio de Janeiro were found to have specific shifts or separate rooms for the care of young people (Table 1). Most of the time, they are treated as part of a service aimed at the general population. It is important to state that the creation of new centers of reference is not required for this purpose, since the existing health system is organized to meet the specific needs of adolescents. Adjustments such as flexibility in service hours, a separate physical space for young people (or in the absence of a physical structure, specific shifts for teens), a safety guarantee, as well as brochures and information targeted at this audience, support their care3131. Braeken D, Rondinelli I. Sexual and reproductive health needs of young people: matching needs with systems. Int J Gynaecol Obstet 2012; 119(Supl. 1):S60-S63.
32. Fox HB, McManus MA, Irwin Junior CE, Kelleher, KJ, Peake K. A research agenda for adolescent-centered primary care in the United States. J Adolesc Health 2013; 53(3):307-310.-3333. Shaw D. Access to sexual and reproductive health for young people: Bridging the disconnect between rights and reality. Int J Gynaecol Obstet 2009; 106(2):132-136.. The data demonstrate no such adjustment in most services, since the service is in the same environment as the adult population.
Furthermore, only 12.9% of units were found to offer some type of educational activities specifically for adolescents and the majority of coordinators report difficulties in locating professionals to develop this work. The precarious nature of human resources and the lack of capacity for such work are barriers highlighted in more than half of the units. Within Brazil, the vast majority of professional training schools in the area of health care have not yet incorporated technical content into their curriculum which build capacity among the recently-trained for servicing this group of the population in a way that is competent and appropriate3434. Nogueira MJ, Modena CM, Schall VT. Políticas públicas de atenção às adolescentes grávidas – uma revisão bibliográfica. Adolesc Saude 2013;10(1):37-44.. This is reflected in the fact that less than one third of doctors show some type of capacity in adolescent health. It is important that educational and preventative work is attractive for adolescents and that the treatment team is prepared to deal with this age group.
Interdisciplinarity is another aspect that plays an important role in adolescent health care. However, the family health teams are comprised of doctors, nurses, or auxiliary nurses and community health workers technicians, and do not include professionals from other fields, such as a psychologist, nutritionist or social worker2525. Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica. Brasília: MS; 2012. [acessado 2014 set 13]. Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf
http://189.28.128.100/dab/docs/publicaco...
. In the international context, we highlight the recommendation that arose from the conference held in Washington DC in 2012, that indicated it is essential to that physical, behavioral and reproductive health services are integrated for the improvement of primary healthcare aimed at adolescents3232. Fox HB, McManus MA, Irwin Junior CE, Kelleher, KJ, Peake K. A research agenda for adolescent-centered primary care in the United States. J Adolesc Health 2013; 53(3):307-310..
The availability of emergency treatment in over 80% of units makes services more accessible. However, the requirements of the presence of a guardian for setting the appointment and treatment highlights the lack of preparation of health units for dealing with this age group. The attitudes and behavior of healthcare professionals are known to represent a major barrier to access to services for this population3434. Nogueira MJ, Modena CM, Schall VT. Políticas públicas de atenção às adolescentes grávidas – uma revisão bibliográfica. Adolesc Saude 2013;10(1):37-44.. When compared to adults, adolescents are more susceptible to discriminatory approaches3131. Braeken D, Rondinelli I. Sexual and reproductive health needs of young people: matching needs with systems. Int J Gynaecol Obstet 2012; 119(Supl. 1):S60-S63.
32. Fox HB, McManus MA, Irwin Junior CE, Kelleher, KJ, Peake K. A research agenda for adolescent-centered primary care in the United States. J Adolesc Health 2013; 53(3):307-310.-3333. Shaw D. Access to sexual and reproductive health for young people: Bridging the disconnect between rights and reality. Int J Gynaecol Obstet 2009; 106(2):132-136.. Surprisingly, in more than 10% of SRH services, adolescents are only treated in the presence of their guardian. In some units, adolescents are not allowed to make an appointment (Table 2). That is, there is a disregard for ethical standards in care for adolescents3535. Taquette SR, Vilhena MM, Silva MM, Vale MP. Conflitos éticos no atendimento à saúde de adolescentes. Cad Saude Publica 2005; 21(6):1717-1725.. Moreover, the requirement for the presence of a guardian is a violation of the principles of autonomy and confidentiality provided for under the Brazilian Statute for Children and Adolescents, which outlines the fundamental right to health and freedom of young individuals. After all, this could lead to what would be considered a major impediment to a healthy life3636. Brasil. Ministério da Saúde (MS). Marco Legal. Saúde, um direito de Adolescentes. Brasília: MS; 2007. [acessado 2016 abr 07] Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/07_0400_M.pdf
http://bvsms.saude.gov.br/bvs/publicacoe...
. It is clear, therefore, that there is a violation of the rights to privacy, confidentiality and secrecy, all of which are key pillars to adolescent access to health services77. Tylee A, Haller DM, Graham T, Churchill R, Sanci LA. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet 2007; 369(9572):1565-1573.,2525. Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica. Brasília: MS; 2012. [acessado 2014 set 13]. Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf
http://189.28.128.100/dab/docs/publicaco...
,3131. Braeken D, Rondinelli I. Sexual and reproductive health needs of young people: matching needs with systems. Int J Gynaecol Obstet 2012; 119(Supl. 1):S60-S63.
32. Fox HB, McManus MA, Irwin Junior CE, Kelleher, KJ, Peake K. A research agenda for adolescent-centered primary care in the United States. J Adolesc Health 2013; 53(3):307-310.
33. Shaw D. Access to sexual and reproductive health for young people: Bridging the disconnect between rights and reality. Int J Gynaecol Obstet 2009; 106(2):132-136.
34. Nogueira MJ, Modena CM, Schall VT. Políticas públicas de atenção às adolescentes grávidas – uma revisão bibliográfica. Adolesc Saude 2013;10(1):37-44.
35. Taquette SR, Vilhena MM, Silva MM, Vale MP. Conflitos éticos no atendimento à saúde de adolescentes. Cad Saude Publica 2005; 21(6):1717-1725.
36. Brasil. Ministério da Saúde (MS). Marco Legal. Saúde, um direito de Adolescentes. Brasília: MS; 2007. [acessado 2016 abr 07] Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/07_0400_M.pdf
http://bvsms.saude.gov.br/bvs/publicacoe...
-3737. Bankole A, Malarcher S. Removing barriers to adolescents’ access to contraceptive information and services. Stud Fam Plann 2010; 41(2):117-124..
On analyzing treatment for victims of violence, in more than a third of units, the presence of a guardian was found to be required (Table 2). This fact represents a major obstacle to healthcare, since many cases of abuse and sexual violence in this age group are committed by relatives3838. Pfeiffer L, Salvagni EP. Visão atual do abuso sexual na infância e adolescência. J Pediatr 2005;81(5 Supl.):S197-204.. The autonomy of the adolescent is compromised and the lack of preparation of services for treating this age group is highlighted. Administrative barriers are added to communication barriers, in waiting rooms where the adolescent is treated together with the adult population in more than 90% of units.
In conclusion, the study showed that although there is a broad geographic distribution of health facilities, the structure of care and human resources available to implement the current health policy directed at primary care is not, on average, enough nor does it meet the specific needs of a teenage audience. Therefore, to improve such services, it is fundamental to raise awareness among unit managers, leaders and coordinators for training and capacity building of multi-disciplinary teams. The right to autonomy and confidentiality must be universally respected. Additional studies that focus on adolescents users’ perceptions about the supply and quality of services will undoubtedly be of great benefit as a complement to these results.
Acknowledgments
Survey financed by FAPERJ.
Referências
-
1Instituto Brasileiro de Geografia e Estatística (IBGE). Censo Demográfico 2010. Características da População e dos Domicílios: Resultados do universo [acessado 2014 jun 01]. Disponível em: http://www.ibge.gov.br
» http://www.ibge.gov.br -
2World Health Organization (WHO). Young People´s Health - a Challenge for Society. Report of a WHO Study Group on Young People and Health for All Technical Report Series 731. Geneva: WHO; 1986. [acessado 2014 jun 1]. Disponível em: http://apps.who.int/iris/bitstream/10665/41720/1/WHO_TRS_731.pdf
» http://apps.who.int/iris/bitstream/10665/41720/1/WHO_TRS_731.pdf -
3Mibzvo MT, Zaidi S. Addressing critical gaps in achieving universal access to sexual and reproductive health (SRH): the case for improving adolescent SRH, preventing unsafe abortion, and enhancing linkages between SRH and HIV interventions. Int J Gynaecol Obstet 2010; 110(Supl.):S3-S6.
-
4Knishkowy B, Palti H. GAPS (AMA Guidelines for Adolescent Preventive Services). Where are the gaps? Arch Pediatr Adolesc Med 1997;151(2):123-128.
-
5Bertrand JT, Hardee K, Magnani RJ, Angle MA. Access, quality of care and medical barriers in family planning programs. Int Fam Plan Perspect 1995; 21(2):64-69.
-
6World Health Organization (WHO). Adolescent friendly health services: an agenda for change. Geneva: WHO; 2002. [acessado 2014 nov 30]. Disponível em: http://www.who.int/maternal_child_adolescent/documents/fch_cah_02_14/en/
» http://www.who.int/maternal_child_adolescent/documents/fch_cah_02_14/en/ -
7Tylee A, Haller DM, Graham T, Churchill R, Sanci LA. Youth-friendly primary-care services: how are we doing and what more needs to be done? Lancet 2007; 369(9572):1565-1573.
-
8Sawyer SM, Afifi RA, Bearinger LH, Blakemore SJ, Dick B, Ezeh AC, Patton GC. Adolescence: a foundation for future health. Lancet 2012; 379(9826):1630-1640.
-
9World Health Organization (WHO). Health for the World’s Adolescents. A second chance in the second decade Geneva: WHO; 2014. [acessado 2016 mar 03]. Disponível em: http://apps.who.int/adolescent/second-decade/
» http://apps.who.int/adolescent/second-decade/ -
10Brasil. Ministério da Saúde (MS). Boletim epidemiológico HIV-Aids Brasília: MS; 2014. [acessado 2016 mar 3]. Disponível em: http://www.aids.gov.br/sites/default/files/anexos/publicacao/2014/56677/boletim_2014_final_pdf_15565.pdf
» http://www.aids.gov.br/sites/default/files/anexos/publicacao/2014/56677/boletim_2014_final_pdf_15565.pdf -
11Hindin MJ, Fatusi AO. Adolescent Sexual and Reproductive Health in Developing Countries: An Overview of Trends and Interventions. Int Perspect Sex Reprod Health 2009; 35(2):58-62.
-
12Brasil. Ministério da Saúde (MS). Programa de Saúde do Adolescente - Bases Programáticas 2ª ed. Brasília: MS; 1996. [acessado 2014 nov 30]. Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/cd03_05.pdf
» http://bvsms.saude.gov.br/bvs/publicacoes/cd03_05.pdf -
13Ruzany MH, Andrade CL, Esteves MA, Pina MF, Szwarcwald CL. Avaliação das condições de atendimento do Programa de Saúde do Adolescente no Município do Rio de Janeiro. Cad Saude Publica 2002; 18(3):639-649.
-
14Branco VMC. Os sentidos da saúde do adolescente para os profissionais [dissertação]. Rio de Janeiro: Universidade Federal do Rio de Janeiro; 2002.
-
15Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica Brasília: MS; 2012.
-
16Fonseca DC, Ozella S. As concepções de adolescência construídas por profissionais da Estratégia de Saúde da Família (ESF). Interface (Botucatu) 2010;14(33):411-424.
-
17Ventura M, Corrêa S. Adolescência, sexualidade e reprodução: construções culturais, controvérsias normativas, alternativas interpretativas. Cad Saude Publica 2006; 22(7):1505-1509.
-
18Osis MJD, Faúndes A, Makuch MY, Mello MB, Souza MH, Araújo MJO. Atenção ao planejamento familiar no Brasil hoje: reflexões sobre os resultados de uma pesquisa. Cad Saude Publica 2006; 22(11):2481-2490.
-
19Rio de Janeiro. Secretaria Municipal de Saúde (SMS). Número de nascidos vivos, segundo a idade da mãe segundo área de planejamento (AP) e região administrativa (RA) de residência Rio de Janeiro: SMS; 2012. [acessado 2014 nov 30]. Disponível em: http://www.saude.rio.rj.gov.br
» http://www.saude.rio.rj.gov.br -
20Brasil. Ministério da Saúde (MS). Pesquisa Nacional de Demografia e Saúde da Criança e da Mulher Brasília: MS; 2006. [acessado 2016 mar 17]. Disponível em: http://bvsms.saude.gov.br/bvs/pnds/index.php
» http://bvsms.saude.gov.br/bvs/pnds/index.php -
21Taquette SR, Matos HJ, Rodrigues AO, Bortolotti LR, Amorim E. A epidemia de Aids em adolescentes de 13 a 19 anos no município do Rio de Janeiro: descrição espaço-temporal. Rev Soc Bras Med Trop 2011; 44(4):467-470.
-
22Programa das Nações Unidas para o Desenvolvimento (PNUD). Ranking IDHM dos Municípios, 2010 Brasília: PNUD; 2013. [acessado 2015 mar 30]. Disponível em: http://www.pnud.org.br/atlas/ranking/Ranking-IDHM-Municipios-2010.aspx#
» http://www.pnud.org.br/atlas/ranking/Ranking-IDHM-Municipios-2010.aspx# -
23Green SB, Lissitz RW, Mulaik SA. Limitations of coefficient alpha as an index of test unidimensionality. Educ Psychol Meas 1977; 37(4):827-838.
-
24Ambresin AE, Bennett K, Patton GC, Sanci LA, Sawyer SM. Assessment of youth-friendly health care: a systematic review of indicators drawn from young people’s perspectives. J Adolesc Health 2013; 52(6):670-681.
-
25Brasil. Ministério da Saúde (MS). Política Nacional de Atenção Básica Brasília: MS; 2012. [acessado 2014 set 13]. Disponível em: http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf
» http://189.28.128.100/dab/docs/publicacoes/geral/pnab.pdf -
26Brasil. Lei no 8.080, de 19 de setembro de 1990. Dispõe sobre as condições para a promoção, proteção e recuperação da saúde, a organização e o funcionamento dos serviços correspondentes e dá outras providências. Diário Oficial da União 1990; 19 set.
-
27Jairnilson P, Travassos C, Almeida C, Bahia L, Macinko J. The Brazilian health system: history, advances, and challenges. Lancet 2011; 77(9779):1778-1797.
-
28Taquette SR. Epidemia de HIV/Aids em adolescentes no Brasil e na França: semelhanças e diferenças. Saude Soc 2013; 22(2):618-628.
-
29Ferrari RAP, Thomson Z, Melchior R. Atenção à saúde dos adolescentes: percepção dos médicos e enfermeiros das equipes de saúde da família. Cad Saude Publica 2006; 22(11):2491-2495.
-
30Brasil. Ministério da Saúde (MS). Saúde Integral de Adolescentes e Jovens. Orientações para a Organização de Serviços de Saúde. Brasília: MS; 2005. [acessado 2016 abr 7]. Disponível em: http://files.bvs.br/upload/MS/2005/Brasil_Saude_integral.pdf
» http://files.bvs.br/upload/MS/2005/Brasil_Saude_integral.pdf -
31Braeken D, Rondinelli I. Sexual and reproductive health needs of young people: matching needs with systems. Int J Gynaecol Obstet 2012; 119(Supl. 1):S60-S63.
-
32Fox HB, McManus MA, Irwin Junior CE, Kelleher, KJ, Peake K. A research agenda for adolescent-centered primary care in the United States. J Adolesc Health 2013; 53(3):307-310.
-
33Shaw D. Access to sexual and reproductive health for young people: Bridging the disconnect between rights and reality. Int J Gynaecol Obstet 2009; 106(2):132-136.
-
34Nogueira MJ, Modena CM, Schall VT. Políticas públicas de atenção às adolescentes grávidas – uma revisão bibliográfica. Adolesc Saude 2013;10(1):37-44.
-
35Taquette SR, Vilhena MM, Silva MM, Vale MP. Conflitos éticos no atendimento à saúde de adolescentes. Cad Saude Publica 2005; 21(6):1717-1725.
-
36Brasil. Ministério da Saúde (MS). Marco Legal. Saúde, um direito de Adolescentes Brasília: MS; 2007. [acessado 2016 abr 07] Disponível em: http://bvsms.saude.gov.br/bvs/publicacoes/07_0400_M.pdf
» http://bvsms.saude.gov.br/bvs/publicacoes/07_0400_M.pdf -
37Bankole A, Malarcher S. Removing barriers to adolescents’ access to contraceptive information and services. Stud Fam Plann 2010; 41(2):117-124.
-
38Pfeiffer L, Salvagni EP. Visão atual do abuso sexual na infância e adolescência. J Pediatr 2005;81(5 Supl.):S197-204.
Publication Dates
-
Publication in this collection
June 2017
History
-
Received
11 Dec 2015 -
Reviewed
24 Oct 2016 -
Accepted
26 Oct 2016