Abstract
Cytokines are molecules that act as mediators of immune response; cerebral spinal fluid (CSF) IL-6 is found in all meningeal inflammatory diseases, but IL-8 is associated with acute bacterial meningitis (ABM). A case control study was done to ascertain the discriminatory power of these cytokines in differentiating ABM from aseptic meningitis (AM); IL-6 and IL-8 CSF concentrations were tested through ELISA in samples collected from patients who underwent investigation for meningitis. Sixty patients, 18 with AM, nine with bacteriologic confirmed ABM and 33 controls, assisted in 2005 (MA and controls) and 2007 (ABM) were included. Differently from controls, IL-6 concentrations were increased both in MA and ABM patients (p < 0.05). CSF IL-8 levels were higher in ABM than in AM and controls (p < 0.05). Discriminatory power in ABM as assessed by the area under receiver operator (ROC) curve was 0.951 for IL-8, using a cut-off of 1.685 ng/dL (100% of sensitivity and 94% of specificity). The CSF concentration of both IL-6 and IL-8 are increased in the presence of meningeal inflammation, IL-8 could be an important tool to differentiate ABM from AM.
CSF; inflammation meningitis; aseptic meningitis; bacteria; IL-6; IL-8
BRIEF COMMUNICATION
IL-6 and IL-8 in cerebrospinal fluid from patients with aseptic meningitis and bacterial meningitis: their potential role as a marker for differential diagnosis
Vitor Laerte Laerte Pinto JuniorI; Maria Cristina RebeloII; Rachel Novaes GomesIII; Edson Fernandes de AssisIII; Hugo C Castro-Faria-NetoIII; Marcio Neves BóiaIV
IMD, PhD, Oswaldo Cruz Foundation, Brasília, DF, Brazil School of Medicine, Catholic University of Brasília, Brasília, DF, Brazil
IIMeningitis Reference Laboratory, São Sebastião Infectious Diseases Institute, Rio de Janeiro, Brazil
IIIMSc, PhD, Imunofarmacology Laboratory, Oswaldo Cruz Institute, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil
IVMD, PhD Tropical Medicine Post-graduation Program, Oswaldo Cruz Institute, Oswaldo Cruz Foundation, Rio de Janeiro, Brazil
Correspondence to Correspondence to: Vitor Laerte Pinto Junior Oswaldo Cruz Foundation - Brasília University Campus Darcy Ribeiro, UnB Postal Box 04311 ZIP 70904-970 Phone/fax: 55 61 33294600 vitorlaerte@fiocruz.br
ABSTRACT
Cytokines are molecules that act as mediators of immune response; cerebral spinal fluid (CSF) IL-6 is found in all meningeal inflammatory diseases, but IL-8 is associated with acute bacterial meningitis (ABM). A case control study was done to ascertain the discriminatory power of these cytokines in differentiating ABM from aseptic meningitis (AM); IL-6 and IL-8 CSF concentrations were tested through ELISA in samples collected from patients who underwent investigation for meningitis. Sixty patients, 18 with AM, nine with bacteriologic confirmed ABM and 33 controls, assisted in 2005 (MA and controls) and 2007 (ABM) were included. Differently from controls, IL-6 concentrations were increased both in MA and ABM patients (p < 0.05). CSF IL-8 levels were higher in ABM than in AM and controls (p < 0.05). Discriminatory power in ABM as assessed by the area under receiver operator (ROC) curve was 0.951 for IL-8, using a cut-off of 1.685 ng/dL (100% of sensitivity and 94% of specificity). The CSF concentration of both IL-6 and IL-8 are increased in the presence of meningeal inflammation, IL-8 could be an important tool to differentiate ABM from AM.
Keywords: CSF; inflammation meningitis; aseptic meningitis; bacteria; IL-6; IL-8.
INTRODUCTION
Cytokines are molecules involved in the modulation of immune and inflammatory processes. Interleukin-6 (IL-6) is a cytokine of both innate and adaptive immunity and exerts diverse actions. The main cellular action of IL-6 is to stimulate the growth of B lymphocytes which have differentiated into antibody producing cells. Interleukin-8 (IL-8) acts as chemoattractant for neutrophils to the site of inflammation.1
Elevated CSF cytokine levels are undisputed markers of meningeal inflammation,2 but a specific profile of cytokine concentration for differential diagnostic purposes is not yet available. CSF levels of IL-6 are indiscriminately elevated in all kinds of meningitis,3 and do not contribute to this purpose. Some studies that measured CSF IL-8 concentrations found high levels of this chemokine associated mainly with bacterial meningitis, but its role in aseptic meningitis remains elusive.4,5
Differentiation between aseptic meningitis and acute bacterial meningitis (ABM) in some instances can be puzzling. The search for clinical markers and laboratory tests to help in this task is crucial in order to optimize the treatment of these conditions. A suitable diagnostic tool has been pursued for many years, but until now little has been added to clinical practice.6-8 The importance of an early differentiation between these two conditions resides in the choice of the proper treatment regimen and in the need for inpatient care, especially in ABM, which has a poor prognosis if left untreated.
The aim of our study was to measure CSF IL-6 and IL-8 in patients with aseptic meningitis, bacterial meningitis and normal controls in order to investigate these cytokines as potential tools in the differential diagnosis of bacterial meningitis from aseptic meningitis.
PATIENTS AND METHODS
We performed a case-control study with CSF samples from patients assisted in Instituto Estadual de Infectologia São Sebastião (IEISS), the referral center for infectious diseases in Rio de Janeiro State. AM and control samples were collected during the year of 2005, whereas ABM CSF samples were collected in 2007. Sixty patients were selected, 18 had aseptic meningitis, nine had confirmed laboratorial diagnosis of meningitis caused by Neisseria meningitidis, and 33 had no meningitis (controls). The diagnostic criteria for aseptic meningitis were CSF total leukocyte count above five cells, negative bacteriological tests and a clinical condition compatible with meningitis. Patients with bacterial meningitis were selected on the grounds of a positive CSF culture or a reactive latex for N. meningitidis. Controls were included if the CSF analyses were normal.
This study was designed according to Brazilian laws for research involving human beings and was approved by the Ethical Committee of Evandro Chagas Clinical Research Institute, FIOCRUZ, Rio de Janeiro.
CSF samples were selected by simple random sampling from patients undergoing evaluation for meningitis. No patient was submitted to lumbar puncture only for the purpose of collecting samples for the study. The CSF was analyzed for cellular content, protein and glucose levels and bacteriological tests using laboratory routine methods. CSF was stored at -20ºC and centrifuged for cytokine concentration measurement.
We performed IL-6 and IL-8 measurements from CSF samples by ELISA using specific monoclonal antibodies (Duo set kit - R&D systems) according to the manufacturer's instructions. The results were analyzed by Soft Max Pro software based on the concentrations of the standard curves of each assay.
Statistical analyses were performed using SPSS for Windows 13.0 (SPSS Inc., Chicago, IL, USA). Measurements of central tendency and dispersion for continuous variables (median, standard deviation and range) were used and comparisons between them were tested using Mann-Whitney U-test. Receiver operating characteristic curve (ROC) was computed, and the area under the ROC curve (AUROC) was used to evaluate the ability of IL-8 to discriminate bacterial meningitis from aseptic meningitis. The optimum cut-off was defined as the value that maximized the AUROC.
RESULTS
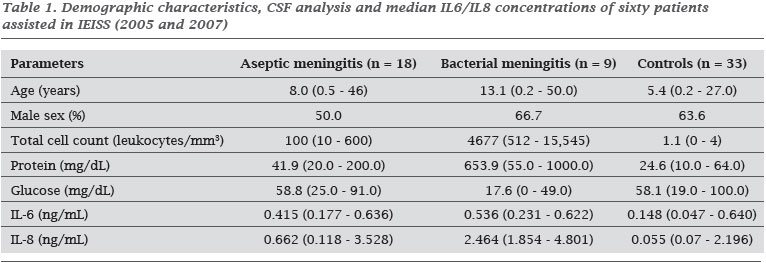
We analyzed 60 CSF samples; the demographical characteristics, the results for routine CSF analysis and IL-6/IL-8 assay results are shown in Table 1. The groups had no statistically significant difference in demographic aspects (p > 0.05), but they were different regarding CSF inflammatory parameters (p < 0.05).
IL-6 concentrations were very similar between aseptic meningitis and bacterial meningitis cases, with no significant difference (p > 0.05). Conversely, CSF IL-8 concentrations were higher in the bacterial meningitis group with a significant difference when compared to the aseptic meningitis group (p < 0.05). Both IL-6 and IL-8 concentrations in meningitis cases (aseptic and bacterial) were markedly different from the concentrations found in the CSF of patients in the control group (p < 0.05).
We calculated the area under the ROC curve to analyze the power of IL-8 to discriminate bacterial meningitis from aseptic meningitis. IL-8 appeared as an excellent marker for differentiating ABM from AM (AUROC = 0.95, 95% CI = 0.855 to 1.046; p < 0.05) when the cut-off level of 1.685 ng/dL was used. At this cut-off, IL-8 had 100% sensitivity and 94% specificity. AUROC for others CSF inflammatory parameters are summarized in Table 2.
DISCUSSION
In our study, we found that IL-6 and IL-8 are important inflammatory mediators in all cases with meningitis. CSF concentrations of these molecules in meningitis cases were significantly different when compared to the control group. Analyzing these mediators individually we found that CSF IL-8 concentration in ABM at the moment of diagnosis was markedly higher than in AM group (p < 0.05).
As a retrospective study performed in a referral center, selection bias is a possible methodological problem, but the different groups were comparable. Another possible limitation was the lack of etiological diagnosis of AM cases, even without laboratorial evidence of bacterial involvement.
IL-6 concentrations were higher in both AM and ABM groups demonstrating that this molecule acts as mediator in meningeal inflammation, serving as a non-specific inflammatory marker.9 This is in agreement with other studies which also compared the levels of IL-6 in cases of bacterial and aseptic meningitis and did not find significant differences.3,10 CSF IL-8 measurement in these two types of meningitis were performed in a study conducted by Lopez-Cortez et al. in 1995.4 Patients with bacterial meningitis had higher concentrations of this chemokine in CSF compared to AM cases. The authors suggested a cut-off of 2.5 ng/dL for CSF IL-8 concentration using only the dispersion graph for this concentration. Ostegaard et al. in 1996 conducted a study in which CSF IL-8 concentrations were also compared between these two groups of patients and controls concluding that IL-8 concentrations were higher in the ABM group. In our study we determined the value of 1.685 ng/dL as the best cut-off, performing a ROC curve, which is designed for this purpose. The accuracy of this cut-off was also excellent. It is important to note that cut-off values for IL-8 may vary depending on variations of the methodology or reagents used, and before standardized tests are available one must determine the specific cut-off value under the conditions employed to ensure the best accuracy.
In order to confirm whether the measurement of CSF IL-8 had the power to discriminate bacterial meningitis from aseptic meningitis, we have performed the AUROC for CSF protein level and total leukocyte count which are of indisputable importance in the differential diagnosis of acute meningitis. The AUROC evidenced that IL-8 had the same power of CSF protein, leukocyte count and glucose level. CSF IL-6 concentration showed little utility in this differentiation.
The cost for cytokines determination in biological samples has decreased significantly over the past decade as availability has increased. In fact, it will probably decrease even further if measurements of cytokines become standard clinical analysis in the hospital setting. Importantly, IL-8 measurements is not a substitute for CSF protein, glucose or leukocyte determinations, but rather an additional and useful input information that may help diagnosis in cases where a clear diagnosis cannot be reached by standard techniques.
Differential diagnosis between aseptic and bacterial meningitis in some instances can be difficult. A trustworthy laboratory marker would facilitate the clinical decision of interrupting antimicrobial therapy and avoiding unnecessary hospitalization. CSF IL-8 concentrations above 1.685 ng/dL would indicate bacterial meningitis confirming other clinical and laboratory findings. More studies performed in suitable models of meningitis are needed in order to establish the routine use of inflammatory markers in the diagnosis of infectious diseases of the central nervous system.
Submitted on: 05/25/2010
Approved on: 11/13/2010
Financial Support: PAPES IV; CNPq, FAPERJ, PRONEX
We declare no conflict of interest.
- 1. Abbas AK, Lichtman AH, Pillai S. Cellular and molecular immunology. 6 ed. Philadelphia: Saunders Elsevier; 2007.
- 2. Nagafuchi M, Nagafuchi Y, Sato R et al. Adult meningism and viral meningitis, 1997-2004: clinical data and cerebrospinal fluid cytokines. Intern Med 2006; 45(21):1209-12.
- 3. Lopez-Cortes LF, Cruz-Ruiz M, Gomez-Mateos J et al Interleukin 6 in cerebrospinal fluid of patients with meningitis is not a useful diagnostic marker in the differential diagnosis of meningitis. Ann Clin Biochem 1997; 34 (Pt 2):165-9.
- 4. Lopez-Cortes LF, Cruz-Ruiz M, Gomez-Mateos J, Viciana-Fernandez P, Martinez-Marcos FJ, Pachon J. Interleukin-8 in cerebrospinal fluid from patients with meningitis of different etiologies: its possible role as neutrophil chemotactic factor. J Infect Dis 1995;172(2):581-4.
- 5. Seki T, Joh K, Oh-ishi T. Augmented production of interleukin-8 in cerebrospinal fluid in bacterial meningitis. Immunology 1993; 80(2):333-5.
- 6. Nigrovic LE, Kuppermann N, Macias CG et al. Clinical prediction rule for identifying children with cerebrospinal fluid pleocytosis at very low risk of bacterial meningitis. Jama 2007; 297(1):52-60.
- 7. Ostergaard C, Benfield TL, Sellebjerg F, Kronborg G, Lohse N, Lundgren JD. Interleukin-8 in cerebrospinal fluid from patients with septic and aseptic meningitis. Eur J Clin Microbiol Infect Dis 1996; 15(2):166-9.
- 8. Spanos A, Harrell FE, Jr., Durack DT. Differential diagnosis of acute meningitis. An analysis of the predictive value of initial observations. Jama 1989; 262(19):2700-7.
- 9. Chavanet P, Bonnotte B, Guiguet M et al. High concentrations of intrathecal interleukin-6 in human bacterial and nonbacterial meningitis. J Infect Dis 1992; 166(2):428-31.
- 10. Mukai AO, Krebs VL, Bertoli CJ, Okay TS. TNF-alpha and IL-6 in the diagnosis of bacterial and aseptic meningitis in children. Pediatr Neurol 2006; 34(1):25-9.
Correspondence to:
Publication Dates
-
Publication in this collection
06 Apr 2011 -
Date of issue
Apr 2011
History
-
Accepted
13 Nov 2010 -
Received
25 May 2010