Abstracts
Excessive daytime sleepiness (EDS) imposes a wide range of adverse health-related outcomes in older people, such as disability, which impair everyday activities and may increase the risk of fall. Few studies have explored EDS in Brazilian older people living in the community who are typically cared in primary health services. This study aims to investigate the prevalence of EDS and its sociodemographic, physical and mental health correlates among community-dwelling older adults. This is an exploratory, population-based study derived from Frailty in Brazilian Older Adults (FIBRA) study including adults aged 65 years and older. Participants with a score ≥ 11 points on the Epworth Sleepiness Scale were considered as having excessive daytime sleepiness. A structured, multidimensional questionnaire was used to investigate sociodemographic, physical and mental health, and self-rated health variables. The sample was composed of 776 older adults, of whom 21% (n = 162) presented excessive daytime sleepiness. Multivariate regression analysis revealed that EDS is associated with obesity (OR = 1.50; 95%CI 1.02 - 2.20), urinary incontinence (OR = 1.53; 95%CI 1.01 - 2.31), poor self-rated health (OR = 1.54; 95%CI 1.06 - 2.24), and depression symptoms (OR = 1.49; 95%CI 1.00 - 2.20). Our results suggest that healthcare professionals should identify older adults with EDS and implement intervention strategies to minimize the negative impact of the co-occurrence of this condition with obesity, depression and urinary incontinence over health and quality of life.
Sleep disorders; Health of the elderly; Health status; Epworth scale; Cross-sectional studies; Population-based study
A Sonolência Diurna Excessiva (SDE) está relacionada a vários efeitos adversos na saúde de pessoas idosas, como a incapacidade funcional, que compromete as atividades do cotidiano e aumenta o risco de quedas. Poucos estudos têm explorado a SDE em idosos brasileiros que vivem na comunidade, que são tipicamente cuidados em serviços de atenção primária em saúde. Este estudo tem como objetivo investigar a prevalência da SDE e sua correlação com dados sociodemográficos, físicos e sobre a saúde mental de idosos que vivem na comunidade. Este é um estudo exploratório de base populacional, derivado da Rede de Estudos de Fragilidade de Idosos Brasileiros (FIBRA) com idosos com de 65 anos ou mais. Participantes com um escore ≥ 11 pontos na Escala de Sonolência de Epworth foram considerados como tendo SDE. Um questionário estruturado, multidimensional foi usado para investigar as variáveis sociodemográficas, físicas, saúde mental, e qualidade de vida. A amostra foi composta por 776 idosos, dos quais 21% (n = 162) apresentavam SDE. A análise de regressão múltipla revelou que a SDE está associada à obesidade (OR = 1.50; IC95% 1.02 - 2.20), incontinência urinária (OR = 1.53; IC95% 1.01 - 2.31), má qualidade de vida (OR = 1.54; IC95% 1.06 - 2.24) e sintomas depressivos (OR = 1.49; IC95% 1.00 - 2.20). Nossos resultados sugerem que profissionais da saúde devem identificar os idosos com SDE e implementar intervenções para minimizar o impacto negativo da coocorrência dessas condições com obesidade, depressão e incontinência urinária sobre a saúde e qualidade de vida.
Transtornos do sono; Saúde do idoso; Nível de saúde; Escala de Epworth; Estudos transversais; Estudo populacional
INTRODUCTION
Sleep disorders are common among the older adult population11 Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep 1995; 18(6): 425-32.. More than half of the people aged 65 and over presented at least one chronic sleep disorder11 Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep 1995; 18(6): 425-32. , 22 Maggi S, Langlois JA, Minicuci N, Grigoletto F, Pavan M, Foley DJ, et al. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. J Am Geriatr Soc 1998; 46(2): 161-8. causing insufficient sleep33 Young TB. Epidemiology of daytime sleepiness: definitions, symptomatology, and prevalence. J Clin Psychiatry 2004; 65 Suppl 16: 12-6. that may lead to excessive daytime sleepiness11 Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep 1995; 18(6): 425-32..
Excessive daytime sleepiness (EDS) is commonly a secondary symptom of sleep disorders and it is characterized by the difficult in maintaining awake in the wake period44 ICSD-3. The International Classification of Sleep Disorders. Darien, IL: American Academy of Sleep Medicine; 2014.. The severity of sleepiness is based on frequency and degree of impairment on daily activities33 Young TB. Epidemiology of daytime sleepiness: definitions, symptomatology, and prevalence. J Clin Psychiatry 2004; 65 Suppl 16: 12-6.. The prevalence of excessive daytime sleepiness varies between 11 and 25% for the general population55 Hublin C, Kaprio J, Partinen M, Heikkila K, Koskenvuo M. Daytime sleepiness in an adult, Finnish population. J Intern Med 1996; 239(5): 417-23. , 66 Walsleben JA, Kapur VK, Newman AB, Shahar E, Bootzin RR, Rosenberg CE, et al. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep 2004; 27(2): 293-8. and may reach up to 30%33 Young TB. Epidemiology of daytime sleepiness: definitions, symptomatology, and prevalence. J Clin Psychiatry 2004; 65 Suppl 16: 12-6. in the older adult population. In Brazil, studies with older adults have shown a prevalence varying between 13 and 18%77 Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7. , 88 Souza JC, Magna LA, Reimão R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arqu Neuropsiquiatr 2002; 60(3-A): 558-62.,
EDS is a symptom typically related to sleep disturbances, such as obstructive sleep apnea, narcolepsy and idiopathic hypersomnia99 Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and Associations With Excessive Daytime Sleepiness in an Australian Older Population. Asia Pac J Public Health 2013 .. In addition, it is also related to poor health status1010 Spira AP, Covinsky K, Rebok GW, Punjabi NM, Stone KL, Hillier TA, et al. Poor sleep quality and functional decline in older women. J Am Geriatr Soc 2012; 60(6): 1092-8. , low physical activity levels, disability in daily activities1010 Spira AP, Covinsky K, Rebok GW, Punjabi NM, Stone KL, Hillier TA, et al. Poor sleep quality and functional decline in older women. J Am Geriatr Soc 2012; 60(6): 1092-8. and an increased number of depression symptoms1111 Maglione JE, Ancoli-Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, et al. Depressive symptoms and subjective and objective sleep in community-dwelling older women. J Am Geriatr Soc 2012; 60(4): 635-43.. Among older people, napping for long periods during the day is related to an increased risk of falling1212 St George RJ, Delbaere K, Williams P, Lord SR. Sleep quality and falls in older people living in self- and assisted-care villages. Gerontology 2009; 55(2): 162-8..
Some methods used for objective assessment of excessive sleepiness are polysomnography and multiple sleep latency. These assessments are time-consuming, require high financial investment and specifics sleep laboratories, preventing their use in epidemiological studies. Subjective measurements include some scales as Stanford Sleepiness1313 Hoddes E, Zarcone V, Smythe H, Phillips R, Dement W. Quantification of sleepiness: a new approach. Psychophysiology 1973; 10(4): 431-6. and Karolinska Sleepiness1414 Åkerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosc 1990; 52(1-2): 29-37. that assesses EDS in the moment of application. To determine subjectively as EDS may influence daily activities, the most appropriate scale is Epworth1515 Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14(6): 540-5. that assess the probability of sleep in activities.
A substantial rise in the proportion of older adults in the Brazilian population is predicted to come within the next decades, reaching 30% of the population in 20501616 Gragnolati M, Jorgensen OH, Rocha R, Fruttero A. Growing Old in an Older Brazil: Implications of Population Aging on Growth, Poverty, Public Finance, and Service Delivery. Washington, D.C.: The Word Bank; 2011., demanding integrated, systemic, and comprehensive interventions to minimize the negative impact on health and quality of life imposed by the cumulative and multifactorial nature of comorbidities and clinical conditions in later life. The aim of this study is to estimate the prevalence and to investigate sociodemographic, physical and mental health correlates of EDS in community-dwelling older adults.
METHOD
This is a cross-sectional exploratory, population-based study derived from a Frailty in Brazilian Older Adults (FIBRA) network study. The sample for this study was composed of older adults aged 65 or older, living in the municipalities of Barueri, São Paulo (Human Development Index - HDI of 0.786) and Cuiabá, Mato Grosso (HDI: 0.785), both in Brazil. The study was carried out from March 2009 to April 2010.
Participants' exclusion criteria were
-
cognitive impairment according the Mini-Mental State Examination, adjusted for educational level1717 Bertolucci PHF, Brucki SMD, Campacci SR, Juliano Y. O Mini-Exame do Estado Mental em uma população geral: Impacto da escolaridade. Arqu Neuropsiquiatr 1994; 52(1): 1-7. ;
-
inability to walk temporarily or permanently, even with a walking device;
-
localized strength loss and aphasia caused by stroke;
-
Parkinson's disease (either severe or unstable state);
-
severe hearing or visual impairment that impairs communication; or
-
terminal illness.
The evaluation was carried out by trained researchers in two phases, the first consisting of a semi-structured interview carried out at home in sessions that lasted from 40 to 120 minutes. The second phase consisted of a data-gathering session using physical-functioning tests that lasted from 20 to 30 minutes that was carried out in public schools, community centers, and health centers close to the older adults' homes.
The Epworth Sleepiness Scale1818 Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Menna Barreto SS, Johns MW. Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol 2009; 35(9): 877-83. was used to determine the degree of excessive sleepiness. It is a scale composed of eight items, in which the subject marks the possibility of napping in routine situations, such as watching television, lying down to rest, and while being a passenger in a vehicle. The scoring for each item varies from 0 (no chance of napping) to 3 (great probability of napping). A score of ≥ 11 points indicates excessive daytime sleepiness.
The eight-item scale has a reliability coefficient (Cronbach's α) of 0.83. The scale has been validated for older American women and has an adequate internal consistency (α = 0.76)1919 Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui L-Y, Ensrud K, et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med 2012; 13(1): 36-42., In Brazil it has been validated for adults1818 Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Menna Barreto SS, Johns MW. Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol 2009; 35(9): 877-83. and its feasibility was tested in institutionalized older people2020 Frohnhofen H, Popp R, Willmann V, Heuer H, Firat A. Feasibility of the Epworth Sleepiness Scale in a sample of geriatric in-hospital patients. J Physiol Pharmacol 2009; 60 Suppl 5: 45-9. , demonstrating that is possible use this instrument. Despite the limitations, this is a widely used scale for EDS assessment in older population88 Souza JC, Magna LA, Reimão R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arqu Neuropsiquiatr 2002; 60(3-A): 558-62. , 99 Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and Associations With Excessive Daytime Sleepiness in an Australian Older Population. Asia Pac J Public Health 2013 . , 1111 Maglione JE, Ancoli-Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, et al. Depressive symptoms and subjective and objective sleep in community-dwelling older women. J Am Geriatr Soc 2012; 60(4): 635-43. , 2121 Lopes JM, Dantas FG, Medeiros JL. Excessive daytime sleepiness in the elderly: association with cardiovascular risk, obesity and depression. Rev Bras Epidemiol 2013; 16(4): 872-9. , 2222 Hayley AC, Williams LJ, Berk M, Kennedy GA, Jacka FN, Pasco JA. The relationship between excessive daytime sleepiness and depressive and anxiety disorders in women. Aust N Z J Psychiatry 2013; 47(8): 772-8..
Sociodemographic variables analyzed were: gender, age (grouped 65 - 69, 70 - 74, 75 - 79 and 80 years and older), education level (0 - 1, 1 - 4, 5 - 8, 9 years or more), and gross monthly family income (0 - 1, 1 - 3, 3 - 5, 5 minimum wages and above).
Self-rated health was assessed by asking the participant to evaluate the general status of his or her health (very good, good, regular, bad, or very bad).
The presence of diseases diagnosed by a physician in the last year was identified by self-report1313 Hoddes E, Zarcone V, Smythe H, Phillips R, Dement W. Quantification of sleepiness: a new approach. Psychophysiology 1973; 10(4): 431-6.. The following diseases were considered: hypertension, arthritis, heart diseases, diabetes mellitus, stroke, depression, osteoporosis, bronchitis/emphysema. Participants were considered obese if they had a Body Mass Index (BMI) ≥ 30 kg/m2. The health conditions evaluated were urinary incontinence, sleeping problems, and single falls (only one fall) and recurrent falls (two or more falls) in the last 12 months. The presence of depression symptoms was assessed by the 15-item Geriatric Depression Scale2323 Paradela EM, Lourenco RA, Veras RP. [Validation of geriatric depression scale in a general outpatient clinic]. Rev Saude Publica 2005; 39(6): 918-23. [Article in Portuguese] . Participants were also questioned about the regular use of medications. The number of medications was counted and the presence of polypharmacy (use of four or more regular medications in the last three months1414 Åkerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosc 1990; 52(1-2): 29-37.) was ascertained.
Frailty was established accordingly to the phenotype proposed by Fried et al.2424 Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56(3): M146-56. Older adults who presented three or more of the following criteria were rated as frail:
-
unintentional weight loss within the last year (over 4,5 kg or 5% of body weight);
-
exhaustion or fatigue, based on answers to the Center for Epidemiologic Studies Depression Scale (CES-D);
-
low handgrip strength measured with a dynamometer (SAEHANW - SH 5001), indicated by values below the first quintile of the sample, adjusted by gender and BMI;
-
low gait speed, indicated by values above the 80th percentile of time needed to walk a distance of 4.6 meters, adjusted by height and gender;
-
low energy expenditure in kilocalories per week, which was indicated by values below the first quintile of the sample, adjusted by gender, measured by a summarized version of the Minnesota Leisure Time Activities Questionnaire (Q-MLTPA)2525 Lustosa LP, Pereira DS, Dias RC, Britto RR, Parentoni AN, Pereira LSM. Tradução e adaptação transcultural do Minnesota Leisure Time Activities Questionnaire em idosos. Geriatria & Gerontologia 2011; 5: 57-65..
The Pontifícia Universidade Católica (PUCSP) and the Ethics in Research Committee of the Hospital das Clínicas de Ribeirão Preto of the Universidade de São Paulo (HCRP-USP) Ethics Committees approved this study. All participants gave written informed consent before data collection began.
A descriptive analysis of the variables was made using simple frequency. The comparison between groups with or without excessive daytime sleepiness was carried out using the χ2 or Fisher's exact test for categorical variables, while the t-test was used for quantitative variables. The level of significance was maintained at α < 0.05. Afterwards, we performed a multivariate logistic regression analysis. Items with p < 0.05 were excluded from the analysis one by one, following the sequence of the value of p. In case an item was eliminated, that variable was considered as a confusion factor if there was a change in the rest of the parameter that exceeded 20% (coefficient β). Fatigue was conceived of as a confounding variable during analysis, and was eliminated in the final model. The odds ratios with respective (95%CI) and the values of p were reported. We evaluated the adjustment of the multiple-regression model by the Hosmer-Lemeshow goodness-of-fit test. Discrimination was quantified using area under the curve (ROC curve) with 95%CI. The statistics package used for data analysis was SPSS 19.0 for Windows.
RESULTS
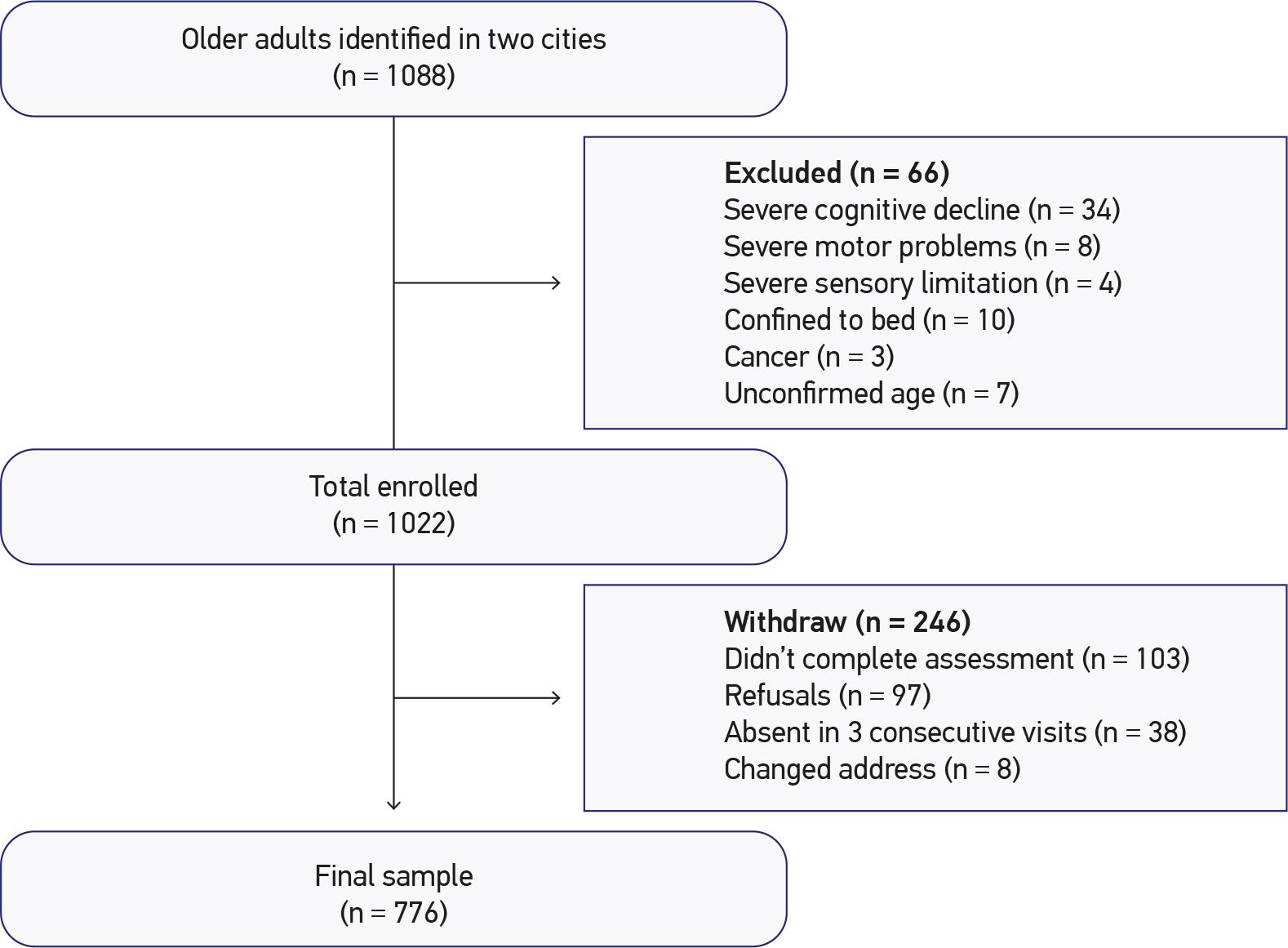
Were enrolled 1,088 older people in the homes belonging to assorted census regions and 776 of these were included in this study, 391 of them from the city of Cuiabá, Mato Grosso, Brazil, and 385 from the city of Barueri, São Paulo, Brazil. The study flowchart is presented in Figure 1.
The average age of the participants in this study was 71.9 years (± 5.9), 496 of them (64%) being female. Of all the participants, 333 (43%) reported trouble sleeping and 162 (21%) presented excessive daytime sleepiness. Considering only those older people who reported sleeping problems, 70 (21%) had excessive daytime sleepiness.
Sociodemographic characteristics, physical and mental health and self-rated health characteristics among older adults with and without EDS are presented in Table 1 and Table 2, respectively. The final multivariate logistic regression model pointed out that excessive daytime sleepiness is associated with obesity, urinary incontinence, depressive symptoms, and poor self-rated health (Table 3).
DISCUSSION
About 20% of the older adults presented excessive daytime sleepiness, which was not associated with sociodemographic factors (gender, age, schooling, and income), but with clinical factors (urinary incontinence, obesity and depression symptoms) and also with poor self-rated health among community-dwelling older adults.
The prevalence of excessive daytime sleepiness observed in our study is greater when compared to studies carried out with similar populations99 Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and Associations With Excessive Daytime Sleepiness in an Australian Older Population. Asia Pac J Public Health 2013 . , 2626 Baldwin CM, Griffith KA, Nieto FJ, O'Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 2001; 24(1): 96-105. , 2727 Teo JS, Briffa NK, Devine A, Dhaliwal SS, Prince RL. Do sleep problems or urinary incontinence predict falls in elderly women? Aust J Physiother 2006; 52(1): 19-24., including a study conducted in Brazil, in which the prevalence was 13%77 Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7.. According to Hara et al.77 Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7., a possible explanation for this disagreement observed in the literature may rely on the distinct definitions used for sleepiness. In addition, different scales with different cut-off points have been used to identify EDS, which may also justify, at least in part the observed difference in prevalence. For example, similarly to our study, Souza et al.88 Souza JC, Magna LA, Reimão R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arqu Neuropsiquiatr 2002; 60(3-A): 558-62. used the Epworth Sleepiness Scale and observed a prevalence of EDS close to the proportion observed in our study (18%). However, in the study of Hara et al.77 Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7., which used a different questionnaire, the prevalence was smaller (13%), possibly because they questioned about the presence of sleepiness occurring three or more times per week.
The assessment of EDS in population-based studies commonly uses questionnaires for measurement, as Epworth Scale. In Brazil, this scale was validated only for adults1818 Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Menna Barreto SS, Johns MW. Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol 2009; 35(9): 877-83. but is widely use in older population88 Souza JC, Magna LA, Reimão R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arqu Neuropsiquiatr 2002; 60(3-A): 558-62. , 99 Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and Associations With Excessive Daytime Sleepiness in an Australian Older Population. Asia Pac J Public Health 2013 .. The use of the gold standard of sleep disorders, such as polysomnography and multiple sleep latency, are time-consuming, expensive and needing of specific laboratories, making it impossible to use in studies realized in the community.
We did not find an association with gender. The results concerning gender are contradictory; whereas some authors indicate that sleepiness is related to the male gender88 Souza JC, Magna LA, Reimão R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arqu Neuropsiquiatr 2002; 60(3-A): 558-62. , 99 Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and Associations With Excessive Daytime Sleepiness in an Australian Older Population. Asia Pac J Public Health 2013 . , 2626 Baldwin CM, Griffith KA, Nieto FJ, O'Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 2001; 24(1): 96-105., others say that it prevails within the female gender2828 Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med 2006; 12(6): 383-9. , 2929 Rockwood K, Davis HS, Merry HR, MacKnight C, McDowell I. Sleep disturbances and mortality: results from the Canadian Study of Health and Aging. J Am Geriatr Soc 2001; 49(5): 639-41.. Specifically within the Brazilian population, a greater prevalence of EDS was observed among women77 Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7.. The authors suggested that it may be explained by the presence of some clinical conditions, such as depression, insomnia and restless legs syndrome among women77 Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7. Hormonal and body composition differences among men and women could also play a role in the rate of EDS2828 Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med 2006; 12(6): 383-9..
In this study participants were not submitted to medical assessment, so the presence of disease was identified by self-report. To minimize this influence in the results, the interviewer enquired if the participant had some medical diagnosis in the last year and about recent exams, for example.
Studies carried out with the older adult population show a substantial relationship between depressive symptoms and excessive daytime sleepiness1111 Maglione JE, Ancoli-Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, et al. Depressive symptoms and subjective and objective sleep in community-dwelling older women. J Am Geriatr Soc 2012; 60(4): 635-43., as does our study, in which older adults with depression symptoms had a higher probability of presenting EDS when compared with older adults without depressive symptoms. Hayley et al.2222 Hayley AC, Williams LJ, Berk M, Kennedy GA, Jacka FN, Pasco JA. The relationship between excessive daytime sleepiness and depressive and anxiety disorders in women. Aust N Z J Psychiatry 2013; 47(8): 772-8. discussed that sleepiness is commonly associated with anxiety in older women, suggesting that one must be careful when evaluating the mental state of patients who present daytime sleepiness.
Evidences have associated EDS with the use of medications that act in the Central Nervous System influencing in regulation of neurotransmitters responsible for modulation of sleep and wakefulness1212 St George RJ, Delbaere K, Williams P, Lord SR. Sleep quality and falls in older people living in self- and assisted-care villages. Gerontology 2009; 55(2): 162-8. , 3030 Pagel J. Excessive daytime sleepiness. Am Fam Physician 2009; 79(5): 391-6. , In this study was not observed any relation between polypharmacy and EDS, maybe due the fact that we did not ask about the use of psychotropic, for example, just for the number of medications in use.
Urinary incontinence was found to be related to sleep problems2727 Teo JS, Briffa NK, Devine A, Dhaliwal SS, Prince RL. Do sleep problems or urinary incontinence predict falls in elderly women? Aust J Physiother 2006; 52(1): 19-24.. In our study, participants who presented urinary incontinence also presented 1.5 times greater probability of presenting EDS when compared with those who didn't report having urinary incontinence. Teo et al.2727 Teo JS, Briffa NK, Devine A, Dhaliwal SS, Prince RL. Do sleep problems or urinary incontinence predict falls in elderly women? Aust J Physiother 2006; 52(1): 19-24. pointed out that female older adults presenting urinary urgency and excessive sleepiness were almost two times more prone to fall when compared with other females who did not present that clinical condition. We have not observed in our study any association between excessive daytime sleepiness and falling or recurrent falling. It is possible that we didn't observe any association with falls due to the fact that we did not discriminate incontinence type, once the urinary urgency requires older people to take more risky behaviors, especially during night time to get up and go to the bathroom3131 Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation '2003 Sleep in America'Poll. Am J Geriatr Psychiatry 2007; 15(4): 344-50. In addition, nocturia may cause difficult to initiating and maintaining sleep at night3131 Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation '2003 Sleep in America'Poll. Am J Geriatr Psychiatry 2007; 15(4): 344-50., with a negative impact on motor and cognitive performance, mainly because of reduced awareness levels during the day3232 Pilcher JJ, Huffcutt AI. Effects of sleep deprivation on performance: a meta-analysis. Sleep 1996; 19(4): 318-26. . Sleepiness may hamper the ability to process and integrate information (visual, tactile, auditory, and proprioceptive), compromising reaction time and balance anticipatory adjustments, resulting in stumbles and falls2727 Teo JS, Briffa NK, Devine A, Dhaliwal SS, Prince RL. Do sleep problems or urinary incontinence predict falls in elderly women? Aust J Physiother 2006; 52(1): 19-24..
Another health condition that has been shown to be associated with excessive sleepiness is obesity. In this study 34% of EDS population were obese. Evidences shows that obese older people has fragmented sleep at night and an increased nap during the day3333 Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA, et al. The association between sleep duration and obesity in older adults. Int J Obesity 2008; 32(12): 1825-34.. The causes of EDS in obese people is still uncertain44 ICSD-3. The International Classification of Sleep Disorders. Darien, IL: American Academy of Sleep Medicine; 2014. , 3434 Akinnusi ME, Saliba R, Porhomayon J, El-Solh AA. Sleep disorders in morbid obesity. Eur J Intern Med 2012; 23(3): 219-26. but some studies frequent suggests that EDS is a secondary symptom of other sleep disorders, as Obstrutive Sleep Apnea (OSA), snoring and narcolepsy44 ICSD-3. The International Classification of Sleep Disorders. Darien, IL: American Academy of Sleep Medicine; 2014.. It is important to note that in this research was assessed the EDS.
The association between self-rated health and EDS in our study is noteworthy, since self-rated health is considered a significant and powerful indication of overall health1919 Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui L-Y, Ensrud K, et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med 2012; 13(1): 36-42. and is related to increased mortality and poorer quality of life among older adults1515 Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14(6): 540-5..
The results of this study allow healthcare professionals, especially those who are primary health care practitioners, to identify older adult profiles with higher odds of presenting excessive daytime sleepiness. The early identification of EDS and its correlates may help to prevent the well-known negative consequences of this condition for community-dwelling older adults' health and quality of life2020 Frohnhofen H, Popp R, Willmann V, Heuer H, Firat A. Feasibility of the Epworth Sleepiness Scale in a sample of geriatric in-hospital patients. J Physiol Pharmacol 2009; 60 Suppl 5: 45-9. , 3535 Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Arch Intern Med 1999; 159(19): 2349-56. , 3636 Clinical Practice Guidelines for the Management of Patients with Insomnia in Primary Care. Community of Madrid: Ministry of Science and Innovation; 2009..
This research is cross-sectional, which not allows the identification of casual factors. However, it must be noted that this is a population-based study, with a good external validity. Future longitudinal studies could investigate risk factors, particularly the effects of excessive daytime sleepiness and sleep disorders on functional performance restraint in Brazilian older adults.
CONCLUSION
Excessive daytime sleepiness in community-dwelling older adults is related with depression, obesity, urinary incontinence, and poor perceived health. Our results suggest that healthcare professionals should identify older adults with EDS and implement intervention strategies to minimize the negative impact of the co-occurrence of this condition with obesity, depression and urinary incontinence on health and quality of life.
REFERENCES
-
1Foley DJ, Monjan AA, Brown SL, Simonsick EM, Wallace RB, Blazer DG. Sleep complaints among elderly persons: an epidemiologic study of three communities. Sleep 1995; 18(6): 425-32.
-
2Maggi S, Langlois JA, Minicuci N, Grigoletto F, Pavan M, Foley DJ, et al. Sleep complaints in community-dwelling older persons: prevalence, associated factors, and reported causes. J Am Geriatr Soc 1998; 46(2): 161-8.
-
3Young TB. Epidemiology of daytime sleepiness: definitions, symptomatology, and prevalence. J Clin Psychiatry 2004; 65 Suppl 16: 12-6.
-
4ICSD-3. The International Classification of Sleep Disorders. Darien, IL: American Academy of Sleep Medicine; 2014.
-
5Hublin C, Kaprio J, Partinen M, Heikkila K, Koskenvuo M. Daytime sleepiness in an adult, Finnish population. J Intern Med 1996; 239(5): 417-23.
-
6Walsleben JA, Kapur VK, Newman AB, Shahar E, Bootzin RR, Rosenberg CE, et al. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep 2004; 27(2): 293-8.
-
7Hara C, Rocha FL, Costa ÉC, Fuzikawa C, Uchoa E, Lima-Costa MF. Prevalence of excessive daytime sleepiness in Brazilian community-dwelling older adults with very low levels of schooling, and its association with sociodemographic characteristics and lifestyle: the Bambuí Health and Ageing Study (BHAS). J Bras Psiquiatr 2008; 57(2): 91-7.
-
8Souza JC, Magna LA, Reimão R. Excessive daytime sleepiness in Campo Grande general population, Brazil. Arqu Neuropsiquiatr 2002; 60(3-A): 558-62.
-
9Vashum KP, McEvoy MA, Hancock SJ, Islam MR, Peel R, Attia JR, et al. Prevalence of and Associations With Excessive Daytime Sleepiness in an Australian Older Population. Asia Pac J Public Health 2013 .
-
10Spira AP, Covinsky K, Rebok GW, Punjabi NM, Stone KL, Hillier TA, et al. Poor sleep quality and functional decline in older women. J Am Geriatr Soc 2012; 60(6): 1092-8.
-
11Maglione JE, Ancoli-Israel S, Peters KW, Paudel ML, Yaffe K, Ensrud KE, et al. Depressive symptoms and subjective and objective sleep in community-dwelling older women. J Am Geriatr Soc 2012; 60(4): 635-43.
-
12St George RJ, Delbaere K, Williams P, Lord SR. Sleep quality and falls in older people living in self- and assisted-care villages. Gerontology 2009; 55(2): 162-8.
-
13Hoddes E, Zarcone V, Smythe H, Phillips R, Dement W. Quantification of sleepiness: a new approach. Psychophysiology 1973; 10(4): 431-6.
-
14Åkerstedt T, Gillberg M. Subjective and objective sleepiness in the active individual. Int J Neurosc 1990; 52(1-2): 29-37.
-
15Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 1991; 14(6): 540-5.
-
16Gragnolati M, Jorgensen OH, Rocha R, Fruttero A. Growing Old in an Older Brazil: Implications of Population Aging on Growth, Poverty, Public Finance, and Service Delivery. Washington, D.C.: The Word Bank; 2011.
-
17Bertolucci PHF, Brucki SMD, Campacci SR, Juliano Y. O Mini-Exame do Estado Mental em uma população geral: Impacto da escolaridade. Arqu Neuropsiquiatr 1994; 52(1): 1-7.
-
18Bertolazi AN, Fagondes SC, Hoff LS, Pedro VD, Menna Barreto SS, Johns MW. Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol 2009; 35(9): 877-83.
-
19Beaudreau SA, Spira AP, Stewart A, Kezirian EJ, Lui L-Y, Ensrud K, et al. Validation of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older black and white women. Sleep Med 2012; 13(1): 36-42.
-
20Frohnhofen H, Popp R, Willmann V, Heuer H, Firat A. Feasibility of the Epworth Sleepiness Scale in a sample of geriatric in-hospital patients. J Physiol Pharmacol 2009; 60 Suppl 5: 45-9.
-
21Lopes JM, Dantas FG, Medeiros JL. Excessive daytime sleepiness in the elderly: association with cardiovascular risk, obesity and depression. Rev Bras Epidemiol 2013; 16(4): 872-9.
-
22Hayley AC, Williams LJ, Berk M, Kennedy GA, Jacka FN, Pasco JA. The relationship between excessive daytime sleepiness and depressive and anxiety disorders in women. Aust N Z J Psychiatry 2013; 47(8): 772-8.
-
23Paradela EM, Lourenco RA, Veras RP. [Validation of geriatric depression scale in a general outpatient clinic]. Rev Saude Publica 2005; 39(6): 918-23. [Article in Portuguese]
-
24Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci 2001; 56(3): M146-56.
-
25Lustosa LP, Pereira DS, Dias RC, Britto RR, Parentoni AN, Pereira LSM. Tradução e adaptação transcultural do Minnesota Leisure Time Activities Questionnaire em idosos. Geriatria & Gerontologia 2011; 5: 57-65.
-
26Baldwin CM, Griffith KA, Nieto FJ, O'Connor GT, Walsleben JA, Redline S. The association of sleep-disordered breathing and sleep symptoms with quality of life in the Sleep Heart Health Study. Sleep 2001; 24(1): 96-105.
-
27Teo JS, Briffa NK, Devine A, Dhaliwal SS, Prince RL. Do sleep problems or urinary incontinence predict falls in elderly women? Aust J Physiother 2006; 52(1): 19-24.
-
28Krishnan V, Collop NA. Gender differences in sleep disorders. Curr Opin Pulm Med 2006; 12(6): 383-9.
-
29Rockwood K, Davis HS, Merry HR, MacKnight C, McDowell I. Sleep disturbances and mortality: results from the Canadian Study of Health and Aging. J Am Geriatr Soc 2001; 49(5): 639-41.
-
30Pagel J. Excessive daytime sleepiness. Am Fam Physician 2009; 79(5): 391-6.
-
31Foley DJ, Vitiello MV, Bliwise DL, Ancoli-Israel S, Monjan AA, Walsh JK. Frequent napping is associated with excessive daytime sleepiness, depression, pain, and nocturia in older adults: findings from the National Sleep Foundation '2003 Sleep in America'Poll. Am J Geriatr Psychiatry 2007; 15(4): 344-50.
-
32Pilcher JJ, Huffcutt AI. Effects of sleep deprivation on performance: a meta-analysis. Sleep 1996; 19(4): 318-26.
-
33Patel SR, Blackwell T, Redline S, Ancoli-Israel S, Cauley JA, Hillier TA, et al. The association between sleep duration and obesity in older adults. Int J Obesity 2008; 32(12): 1825-34.
-
34Akinnusi ME, Saliba R, Porhomayon J, El-Solh AA. Sleep disorders in morbid obesity. Eur J Intern Med 2012; 23(3): 219-26.
-
35Blumenthal JA, Babyak MA, Moore KA, Craighead WE, Herman S, Khatri P, et al. Effects of exercise training on older patients with major depression. Arch Intern Med 1999; 159(19): 2349-56.
-
36Clinical Practice Guidelines for the Management of Patients with Insomnia in Primary Care. Community of Madrid: Ministry of Science and Innovation; 2009.
-
Financial support: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPQ), CTCNPq/MS-SCTIE-DECIT (protocol number 17/2006).
Publication Dates
-
Publication in this collection
Sept 2015
History
-
Received
24 Apr 2014 -
Reviewed
02 Aug 2014 -
Accepted
30 Sept 2014