ABSTRACT:
Introduction:
Frailty is a preventable and reversible syndrome characterized by a cumulative decline of physiological systems, causing greater vulnerability to adverse conditions.
Objective:
To describe the prevalence of frailty among older adults and analyze its associated factors and progression.
Method:
This is a longitudinal study that used the Health, Well-being, and Aging Study (Saúde, Bem-Estar e Envelhecimento - SABE) database of 2006 and 2010. Five components identified the frailty syndrome: weight loss; fatigue; decreased strength, low physical activity, and reduced walking speed. Older adults were classified as “pre-frail” (1-2 components) and “frail” (3 or more). We used a hierarchical multiple multinomial regression to analyze associated factors.
Results:
Out of the total number of older adults (n = 1,399), 8.5% were frail, and the associated factors were age, functional impairment, cognitive decline, hospitalization, and multimorbidity. In four years, 3.3% of non-frail and 14.7% of pre-frail older adults became frail.
Conclusion:
Identifying the prevalence of frailty and its associated factors can help to implement adequate interventions early to improve the quality of life of older adults.
Keywords:
Aged. Aged; 80 and over. Frail elderly
RESUMO:
Introdução:
Fragilidade é uma síndrome evitável e reversível caracterizada pelo declínio cumulativo dos sistemas fisiológicos, causando maior vulnerabilidade às condições adversas.
Objetivos:
Descrever a prevalência de fragilidade entre os idosos, analisar os fatores associados e a evolução da síndrome.
Método:
Estudo longitudinal que utilizou a base de dados do Estudo Saúde, Bem-Estar e Envelhecimento (SABE), nos anos de 2006 e 2010. A síndrome de fragilidade foi identificada por cinco componentes: perda de peso; fadiga; redução de força, de atividade física e de velocidade de caminhada. Os idosos foram classificados como “pré-frágeis” (1-2 componentes) e “frágeis” (3 ou +). Utilizou-se regressão multinomial múltipla hierárquica para análise dos fatores associados.
Resultados:
Do total de idosos (n = 1.399), 8,5% eram frágeis tendo como fatores associados idade, comprometimento funcional, declínio cognitivo, hospitalização e multimorbidade. Em quatro anos, tornaram-se frágeis 3,3% dos idosos não frágeis e 14,7% dos pré-frágeis.
Conclusão:
A identificação da prevalência e dos fatores associados à fragilidade pode ajudar a implementar intervenções adequadas precocemente, de modo a garantir melhorias na qualidade de vida dos idosos.
Palavras-chave:
Idoso; Idoso de 80 anos ou mais; Idoso fragilizado
INTRODUCTION
Identifying, assessing, and treating frail older people tend to be the focus of attention in Geriatrics and Gerontology in this century. This condition is highly prevalent among long-lived older adults, a group that is growing fast in this population. The effective care of these people and the prevention of the syndrome are directly related to the training of qualified professionals in adequate numbers, and with enough resources, recognizing that the assistance given to this group requires special skills and a higher intervention time11. Duarte YAO, Lebrão ML. Fragilidade e envelhecimento. In: Freitas EV, Py L, Cançado FAX, Doll J, Gorzoni ML. Tratado de geriatria e gerontologia. 3. ed. Rio de Janeiro: Guanabara Koogan; 2013. p. 1285-1298..
Frailty is a clinical syndrome characterized by decreased strength, endurance, and physiological function, which increase the individual’s vulnerability to greater dependence and/or dying22. Morley JE, Vellas B, Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty Consensus: A Call to Action. J Am Med Dir Assoc 2013; 14(6): 392-7. https://dx.doi.org/10.1016%2Fj.jamda.2013.03.022
https://dx.doi.org/10.1016%2Fj.jamda.201...
. Simple and fast screening tests have been developed and validated to allow the identification of frail people since the syndrome is preventable or treatable22. Morley JE, Vellas B, Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty Consensus: A Call to Action. J Am Med Dir Assoc 2013; 14(6): 392-7. https://dx.doi.org/10.1016%2Fj.jamda.2013.03.022
https://dx.doi.org/10.1016%2Fj.jamda.201...
,33. Nunes DP, Duarte YA, Santos JL, Lebrão ML. Screening for frailty in older adults using a self-reported instrument. Rev Saúde Pública. 2015; 49: 1-9..
The frailty physiopathological process results from changes in several mechanisms and biological systems culminating in the disruption of the homeostatic balance44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.,55. Ho YY, Matteini AM, Beamer B, Fried L, Xue QL, Arking DE, et al. Exploring Biologically Relevant Pathways in Frailty. J Gerontol A Biol Sci Med Sci 2011; 66(9): 975-9. https://doi.org/10.1093/gerona/glr061
https://doi.org/10.1093/gerona/glr061...
. In general, the imbalance of multiple systems can lead to an overall decline in the ability of the organism as a whole in tolerating stressors, thus increasing the risk of adverse outcomes associated with frailty66. Lipsitz LA. Dynamics of stability: the physiologic basis of functional health and frailty. J Gerontol A Biol Sci Med Sci 2002; 57(3): B115-25.,77. Ruggiero C, Ferrucci L. The endeavor of high maintenance homeostasis: resting metabolic rate and the legacy of longevity. J Gerontol A Biol Sci Med Sci 2006; 61(5): 466-71.,88. Espinoza S, Walston JD. Frailty in older adults: insights and interventions. Cleve Clin J Med 2005; 72(12): 1105-12.,99. Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc 2006; 54(6): 991-1001. https://doi.org/10.1111/j.1532-5415.2006.00745.x
https://doi.org/10.1111/j.1532-5415.2006...
.
Such changes could cause a downward spiral of functional decline. Fried et al.44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56. proposed a unique and well-defined pathogenetic mechanism as a decreasing energy cycle whose clinical manifestations would increase as frailty worsened. This cycle (Figure 1) had clinical signs such as decreased strength, fatigue, reduced walking speed, low physical activity, and weight loss44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.,55. Ho YY, Matteini AM, Beamer B, Fried L, Xue QL, Arking DE, et al. Exploring Biologically Relevant Pathways in Frailty. J Gerontol A Biol Sci Med Sci 2011; 66(9): 975-9. https://doi.org/10.1093/gerona/glr061
https://doi.org/10.1093/gerona/glr061...
,1010. Fried LP, Walston J. Frailty and failure to thrive. In: Hazzard W, Reubin A, editors. Principles of geriatric medicine and gerontology. 4ª ed. Nova York: McGraw-Hill; 1998. p. 1387-402.. The presence of one or two phenotype components evidenced a high risk of developing the syndrome (pre-frail), and three or more components indicated frail older adults44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.. This construct can identify older people with a high risk of disability, falling, hospitalization, fracture, and death99. Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc 2006; 54(6): 991-1001. https://doi.org/10.1111/j.1532-5415.2006.00745.x
https://doi.org/10.1111/j.1532-5415.2006...
,1111. Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004; 59(3): 255-63.,1212. Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med 2011; 27(1): 17-26. http://doi.org/10.1016/j.cger.2010.08.008
http://doi.org/10.1016/j.cger.2010.08.00...
.
Decreasing energy cycle that could lead to frailty11. Duarte YAO, Lebrão ML. Fragilidade e envelhecimento. In: Freitas EV, Py L, Cançado FAX, Doll J, Gorzoni ML. Tratado de geriatria e gerontologia. 3. ed. Rio de Janeiro: Guanabara Koogan; 2013. p. 1285-1298..
Considering the worldwide demographic transition and the growth in the older adult population1313. United Nations. Department of Economic and Social Affairs - Population Division. World Population Prospects: The 2006 Revision. Nova York: United Nations; 2007., frailty has been increasingly recognized as a public health issue, and represents a challenge for societies in general, especially in developing countries, due to its negative impact on health and quality of life of older adults1414. Masel MC, Graham JE, Reistetter TA, Markides KS, Ottenbacher KJ. Frailty and health related quality of life in older Mexican Americans. Health Qual Life Outcomes 2009; 7: 70. https://doi.org/10.1186/1477-7525-7-70
https://doi.org/10.1186/1477-7525-7-70...
, and the higher use of health services1515. Farhat JS, Velanovich V, Falvo AJ, Horst HM, Swartz A, Patton JH, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg 2012; 72(6): 1526-31. https://doi.org/10.1097/TA.0b013e3182542fab
https://doi.org/10.1097/TA.0b013e3182542...
.
Previous studies showed associations between frailty and age1616. Ottenbacher KJ, Ostir GV, Peek MK, Snih SA, Raji MA, Markides KS. Frailty in older Mexican Americans. J Am Geriatr Soc 2005; 53(9): 1524-31. https://doi.org/10.1111/j.1532-5415.2005.53511.x
https://doi.org/10.1111/j.1532-5415.2005...
, gender1717. Newman AB, Gottdiener JS, Mcburnie MA, Hirsch CH, Kop WJ, Tracy R, et al. Associations of subclinical cardiovascular disease with frailty. J Gerontol A Biol Sci Med Sci 2001; 56(3): M158-66.,1818. Alvarado BE, Zunzunegui MV, Béland F, Bamvita JM. Life course social and health conditions linked to frailty in Latin American older men and women. J Gerontol A Biol Sci Med Sci 2008; 63(12): 1399-406., income and education66. Lipsitz LA. Dynamics of stability: the physiologic basis of functional health and frailty. J Gerontol A Biol Sci Med Sci 2002; 57(3): B115-25.,1919. Morley JE, Perry HM, Miller DK. Something about frailty. J Gerontol A Biol Sci Med Sci 2002; 57(11): M698-704., chronic diseases2020. Vetrano DL, Palmer K, Marengoni A, Marzetti E, Lattanzio F, Roller-Wirnsberger R, et al. Frailty and multimorbidity: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci 2018. http://doi.org/10.1093/gerona/gly110
http://doi.org/10.1093/gerona/gly110...
, self-perceived health2121. González-Pichardo AM, Navarrete-Reyes AP, Adame-Encarnación H, Aguilar-Navarro S, García-Lara JM, Amieva H, et al. Association between self-reported health status and frailty in community-dwelling elderly. J Frailty Aging 2014; 3(2): 104-8. http://doi.org/10.14283/jfa.2014.9
http://doi.org/10.14283/jfa.2014.9...
, cognitive function44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56., depression2222. Vaughan L, Corbin AL, Goveas JS. Depression and frailty in later life: a systematic review. Clin Interv Aging 2015; 10: 1947-58. http://doi.org/10.2147/CIA.S69632
http://doi.org/10.2147/CIA.S69632...
, and functional impairment2323. Makizako H, Shimada H, Doi T, Tsutsumimoto K, Suzuki T. Impact of physical frailty on disability in community-dwelling older adults: a prospective cohort study. BMJ Open 2015; 5(9): e008462. http://doi.org/10.1136/bmjopen-2015-008462
http://doi.org/10.1136/bmjopen-2015-0084...
.
Identifying factors that influence frailty in older adults in Brazil can help public policy planners in adopting preventive strategies and elaborating more appropriate public policies, aiming to reduce the harmful effects of certain determinants, and providing an extension of well-being and quality of life for this population.
Thus, the objective of this study was to describe the prevalence of frailty according to cognitive decline and age group; and analyze the factors associated with this syndrome and its evolution in a period of four years (2006-2010).
METHODS
This is a longitudinal study that used the Health, Well-being, and Aging Study (Saúde, Bem-Estar e Envelhecimento - SABE) database of 2006 and 2010. The baseline sample consisted of older adults from cohorts A and B, in 2006, totaling 1,399 subjects. We excluded 14 individuals who had no information about frailty components. The participant older adults had a follow-up after four years to evaluate the progression of the frailty syndrome.
The frailty syndrome was identified based on the phenotype proposed by Fried et al.44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56., which consists of five components:
-
unintentional weight loss: we used the question “In the past three months, have you lost weight without following a diet?”. Older adults who reported losing over 3 kg scored in this criterion;
-
self-reported fatigue: based on two questions from the Center for Epidemiological Studies - Depression (CES-D), validated for Brazilian older adults 2424. Batistoni SST, Neri AL, Cupertino APFB. Validade da escala de depressão do Center for Epidemiological Studies entre idosos brasileiros. Rev Saude Publica. 2007; 41(4):598-605.: a) “In the past week, how often have you felt that everything you have done demanded a great effort?”; b) “In the past week, how often have you felt that you could not handle your things?”. The answers to both questions were: 0 = rarely or never (< 1 day), 1 = part of the time (1-2 days), 2 = a moderate amount of time (3-4 days), or 3 = all the time. Older adults who answered “2” or “3” in at least one of the two questions scored positively in this component;
-
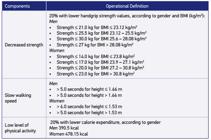
decreased strength: we used the handgrip strength, measured by a dynamometer. The older adults who scored in this component were in the lowest quintile of distribution, stratified by gender and body mass index quartile (Chart 1);
-
slow walking speed: obtained by the three-meter walking test, part of the Short Physical Performance Battery Assessing Lower Extremity Function 2525. Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A Short Physical Performance Battery Assessing Lower-Extremity Function - Association With Self-Reported Disability And Prediction Of Mortality And Nursing-Home Admission. J Gerontol. 1994; 49(2): M85-M94.. The older adults who scored in this component were in the highest quintile of distribution, stratified by gender and median height value (Chart 1);
-
low level of physical activity: we used the International Physical Activity Questionnaire (IPAQ) filled with self-reported information about walking, moderate activities (light cycling, swimming, dancing, light aerobic exercises, playing recreational volleyball, carrying light weights, working on household, backyard, or garden tasks - sweeping, vacuuming, tending the garden), and vigorous activities (running, aerobic exercises, playing soccer, fast cycling, using a treadmill, playing basketball, working on heavy household, backyard, or garden tasks, and carrying heavy weights).
Cut-off points adopted to operationalize the frailty phenotype. SABE Study. São Paulo, 2006.
First, we calculated the time spent (minutes) in performing each activity and curtailed values above 180 minutes. Next, each activity was classified in metabolic equivalent (MET), with walking valuing 3.3 METs; moderate activities, 4.0 METs; and vigorous activities, 8.0 METs. The total of METs performed weekly was estimated by the sum of each type of activity multiplied by time (minutes), number of days, and MET value. Lastly, the calorie expenditure consisted of the total MET of activities multiplied by the division of the older adult’s weight by 60. The estimate of weekly calorie expenditure was stratified into quintiles according to gender, scoring in this criterion the older adults classified in the lowest quintile (Chart 1).
We considered “non-frail” the older adults who showed none of the five phenotype components, “pre-frail” those who presented one or two components, and “frail” the ones with three or more components44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56..
Independent variables included:
-
sociodemographic and economic characteristics: gender, age, years of schooling, marital status (with or without a partner), living alone, and reported income sufficiency;
-
health conditions: multimorbidity, cognitive decline, depression symptoms, functional impairment, and falling and hospitalization in the past year.
We considered multimorbidity the report of two or more chronic diseases such as hypertension, diabetes, cancer, chronic pulmonary disease, heart disease, stroke, joint disease, and osteoporosis. The Mini-Mental State Examination (MMSE) assessed the cognitive state of older adults, considering decline a result ≤ 18 points44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.. The brief version of the Geriatric Depression Scale evaluated depression symptoms, assuming a cut-off point equal to or greater than 62626. Almeida OP; , Almeida SA. Confiabilidade da versao brasileira da Escala de Depressao Geriatrica (GDS) versao reduzida. Arq Neuropsiquiatr, 1999, ; 57(12B): 421-426..
Functional impairment was identified by the reported difficulty in performing at least one of the basic activities of daily living (ADLs) - feeding, bathing/showering, dressing, toileting, transferring, and ambulating - or instrumental activities daily living (IADLs) - managing finances, using transportation, shopping, using the telephone, and taking medicines.
For the analysis, we used the χ2 test with Rao-Scott correction, taking sample weights into account for estimates with population weights. The hierarchical multiple multinomial analysis evaluated the factors associated with frailty. We adopted a distal-proximal orientation, starting with sociodemographic and economic characteristics (Block 1), followed by variables related to health conditions of older adults (Block 2), considering a significance level of 5%. The software Stata®, version 11 analyzed the data.
The Committee for Ethics in Research (Comitê de Ética em Pesquisa - COEP) of the School of Public Health at Universidade de São Paulo approved the SABE Study in 2006 and 2010.
RESULTS
The sample comprised 1,399 older people who had full data related to frailty, representing 1,019,243 older adults living in the city of São Paulo. In this group, 59.4% were females, 58.9% were 60 to 69 years old, 57.3% reported having a partner, 38.8% stated they had four to seven years of schooling, and 55.1% declared that their income was insufficient for their needs.
Over half of the population reported having two or more diseases (55.8%), with the prevalence of hypertension (62.5%). Part of them showed a cognitive decline (9.4%), depression symptoms (14.2%), and difficulty in performing ADLs (13.2%) and IADLs (45.6%).
The prevalence rates related to frailty components were: 25.2% of decreased handgrip strength, 20.0% of low physical activity, 17.0% of reduced walking speed, 13.2% of fatigue, and 7.8% of unintentional weight loss.
The analysis of cognitive decline revealed statistically significant differences in all components assessed, except weight loss. Non-frail older adults corresponded to 50.0% of the population, pre-frail to 41.5%, and frail to 8.5%, and the proportion of frail older adults was higher among those with decline (38.9%) when compared to those without decline (5.3%) (Table 1). Among frail older adults, 54.7% had multimorbidity and ADL impairment (Figure 2.
Distribution (%) of older adults according to frailty components and cognitive decline. City of São Paulo, 2006 (n = 1,399).
Venn diagram representing the overlap between frailty and impairment in basic activities of daily living (ADL) and multimorbidity (≥ 2 diseases). City of São Paulo, 2006 (n = 1,399).
The analysis of different ages (Table 2) indicated that the proportion of frailty components increased according to age group and presented statistically significant differences, except for weight loss. The prevalence of frailty was 4.1% for sexagenarians, 8.4% for septuagenarians, 28.0% for octogenarians, and 55.9% for nonagenarians and centenarians.
We found a higher proportion of frail older adults among individuals without a partner (11.7%), the illiterate (15.4%), those with multimorbidity (12.1%), depression symptoms (13.8%), functional impairment in ADLs (36.0%) and IADLs (16.8%), who fell (10.5%), and were hospitalized (26.3%) (Table 3).
The factors associated with pre-frailty and frailty were age (≥ 80 years), functional impairment, cognitive decline, and hospitalization in the year prior to the interview. Perceived income insufficiency and fall were associated only with the pre-frail condition. Older adults who reported multimorbidity had a higher chance of presenting frailty (Table 4).
After four years of follow-up, 71.3% of these older adults were reinterviewed, 11.8% died, 16.6% were not found, and 0.3% were institutionalized. The proportion of deaths among non-frail, pre-frail, and frail older adults was 6.0, 13.1, and 39.8%, respectively. The percentage of institutionalized pre-frail and frail older adults was 0.5% and 1.3%, respectively.
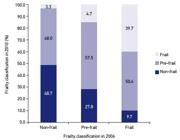
The analysis of components of the syndrome in 2010 indicated that 36.0% of older adults demonstrated a low level of physical activity, 25.9% showed decreased muscle strength, 23.4% presented reduced walking speed, 9.9% declared fatigue, and 7.0% reported unintentional weight loss. The prevalence of frailty increased to 9.8%. Progression to frailty was 3.3% among the non-frail and 14.7% among the pre-frail. On the other hand, 27.8% of older adults classified as pre-frail and 9.7% considered frail in 2006 reverted to the condition of non-frail in 2010 (Figure 3).
Progression of older adults according to frailty classification. City of São Paulo (SP), 2006-2010 (n = 823) (p= 0.000).
DISCUSSION
The prevalence of frailty among non-institutionalized older adults was 8.5% and was associated with age, functional impairment, cognitive decline, hospitalization, and multimorbidity.
Authors found a wide variation in prevalence of frailty - 6.9 to 21% for the frail state and 33 to 55% for the pre-frail state. This variability can be justified by the lack of consensus regarding the definition of the syndrome2727. Tribess S, Oliveira RJ. Síndrome da fragilidade biológica em idosos: revisão sistemática. Rev Salud Pública 2011; 13(5): 853-64. http://dx.doi.org/10.1590/S0124-00642011000500014
http://dx.doi.org/10.1590/S0124-00642011...
. However, a systematic review on Frailty Phenotype found a mean prevalence of frail older people of 13.6% (95%CI 13.2 - 14.0) and pre-frail of 33.5% (95%CI 32.9 - 34.1)2828. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012; 60(8): 1487-92. https://doi.org/10.1111/j.1532-5415.2012.04054.x
https://doi.org/10.1111/j.1532-5415.2012...
.
In Brazil, the Study on Frailty in Brazilian Older Adults (Estudo sobre Fragilidade em Idosos Brasileiros - FIBRA) assessed a convenience sample of 3,478 older adults (65 years and older) in seven Brazilian cities and found 9.1% of frail, 51.8% of pre-frail, and 39.1% of non-frail individuals2929. Neri AL, Yassuda MS, Araújo LF, Eulálio MC, Cabral BE, Siqueira MEC, et al. Metodologia e perfil sociodemográfico, cognitivo e de fragilidade de idosos comunitários de sete cidades brasileiras: Estudo FIBRA. Cad Saúde Pública 2013; 29(4): 778-92. http://dx.doi.org/10.1590/S0102-311X2013000400015
http://dx.doi.org/10.1590/S0102-311X2013...
. In 2009, the SABE Study conducted in the city of São Paulo evaluated 433 long-lived older adults (age ≥ 75 years) and classified 37% of them as frail33. Nunes DP, Duarte YA, Santos JL, Lebrão ML. Screening for frailty in older adults using a self-reported instrument. Rev Saúde Pública. 2015; 49: 1-9..
Silva et al.3030. Silva RN, Guarda FRB, Hallal PC, Martelli PJL. Avaliabilidade do Programa Academia da Saúde no Município do Recife, Pernambuco, Brasil. Cad Saúde Pública 2017; 33(4): e00159415. http://dx.doi.org/10.1590/0102-311x00159415
http://dx.doi.org/10.1590/0102-311x00159...
assessed older adults who participated in a Community Center in the city of Campina Grande/PB and the prevalence of frail older people was 6%, and pre-frail was 71.1%. Augusti et al.3131. Augusti ACV, Falsarella GR, Coimbra AMV. Análise da síndrome da fragilidade em idosos na atenção primária: Estudo transversal. Rev Bras Med Fam Comunidade 2017; 12(39): 1-9. https://doi.org/10.5712/rbmfc12(39)1353
https://doi.org/10.5712/rbmfc12(39)1353...
analyzed 306 older adults (≥ 65 years) living in the inland of São Paulo and found 21.5% of frail, 71.5% of pre-frail, and 6.0% of non-frail individuals.
In the present study, older adults with cognitive decline showed a higher prevalence of frailty and pre-frailty. Studies have demonstrated that the mean MMSE score is lower among the frail, negatively impacting the health of older adults, which can accelerate the frailty process3232. Alencar MA, Dias JMD, Figueiredo LC, Dias RC. Frailty and cognitive impairment among community-dwelling elderly. Arq Neuropsiquiatr 2013; 71(6): 362-7. https://doi.org/10.1590/0004-282X20130039
https://doi.org/10.1590/0004-282X2013003...
,3333. Chen S, Honda T, Narazaki K, Chen T, Nofuji Y, Kumagai S. Global cognitive performance and frailty in non-demented community-dwelling older adults: Findings from the Sasaguri Genkimon Study. Geriatr Gerontol Int 2016; 16(6): 729-36. https://doi.org/10.1111/ggi.12546. Chen et al.3333. Chen S, Honda T, Narazaki K, Chen T, Nofuji Y, Kumagai S. Global cognitive performance and frailty in non-demented community-dwelling older adults: Findings from the Sasaguri Genkimon Study. Geriatr Gerontol Int 2016; 16(6): 729-36. https://doi.org/10.1111/ggi.12546 underline that frailty and pre-frailty are reversible and deserve effective interventions to interrupt the progression of the syndrome.
The literature has consolidated that the prevalence of frailty significantly increases among long-lived older adults, corroborating the results found in this study. Fried et al.44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56. identified frailty in 3.9% of older adults aged 65 to 74 years, 11.6% among those aged 75 to 84 years, and 25% in individuals aged 85 years or older. Collard et al.2828. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012; 60(8): 1487-92. https://doi.org/10.1111/j.1532-5415.2012.04054.x
https://doi.org/10.1111/j.1532-5415.2012...
also identified a higher prevalence of frailty among older adults aged 80 to 84 years (15.7%) and in those older than 84 years of age (26.1%).
In a study conducted in various Brazilian localities, evaluating older adults aged 60 years and older, the prevalence of frailty corresponded to approximately 9% of the total population, but this number increased in older age groups - 11.8% for those aged 75 to 79 years, and 19.7% for those aged 80 years and older, results close to the ones found in this study2929. Neri AL, Yassuda MS, Araújo LF, Eulálio MC, Cabral BE, Siqueira MEC, et al. Metodologia e perfil sociodemográfico, cognitivo e de fragilidade de idosos comunitários de sete cidades brasileiras: Estudo FIBRA. Cad Saúde Pública 2013; 29(4): 778-92. http://dx.doi.org/10.1590/S0102-311X2013000400015
http://dx.doi.org/10.1590/S0102-311X2013...
. Sánchez-García et al.3434. Sánchez-García S, García-Peña C, Salvà A, Sánchez-Arenas R, Granados-García V, Cuadros-Moreno J, et al. Frailty in community-dwelling older adults: association with adverse outcomes. Clin Interv Aging 2017: 12; 1003-11. https://doi.org/10.2147/CIA.S139860
https://doi.org/10.2147/CIA.S139860...
evaluated 1,252 older adults in Mexico City and found that the proportion of frail individuals was 1.8% among 60- to 69-year-olds, 7.7% among 70- to 79-year-olds, and 22.8% among those aged 80 years and older.
The research findings indicate that older adults who fell in the previous year had higher chances of pre-frailty. Frailty and falls can be bidirectionally related. In the same way that falling could lead older adults to frailty, frailty could lead them to fall44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.,3535. Fhon JRS, Rosset I, Freitas CP, Silva AO, Santos JLF, Rodrigues RAP. Prevalência de quedas de idosos em situacão de fragilidade. Rev Saúde Pública 2013; 47(2): 266-73. http://dx.doi.org/10.1590/S0034-8910.2013047003468
http://dx.doi.org/10.1590/S0034-8910.201...
. The association between fall and frailty can cause other health issues such as reduced functional capacity and hospitalization, worsening the quality of life of older adults3636. Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures and mortality in older men. J Am Geriatr Soc 2009; 57(3): 492-8. http://dx.doi.org/10.1111/j.1532-5415.2009.02137.x
http://dx.doi.org/10.1111/j.1532-5415.20...
.
Another factor associated with pre-frailty was the report of income insufficiency. Studies have shown that higher incomes have a positive effect on frailty since purchasing power can provide and reflect a higher degree of psychophysical well-being and, consequently, less dependence in activities of daily living44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.,3737. Santos-Eggimann B, Cuénoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci 2009; 64(6): 675-81. https://doi.org/10.1093/gerona/glp012
https://doi.org/10.1093/gerona/glp012...
,3838. Stringhini S, Dugravot A, Shipley M, Goldberg M, Zins M, Kivimäki M, et al. Health behaviours, socioeconomic status, and mortality: Further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med 2011; 8(2): e1000419. https://doi.org/10.1371/journal.pmed.1000419
https://doi.org/10.1371/journal.pmed.100...
,3939. Trevisan C, Veronese N, Maggi S, Baggio G, Toffanello ED, Zambon S, et al. Factors influencing transitions between frailty states in elderly adults: The Progetto Veneto Anziani Longitudinal Study. J Am Geriatr Soc 2017; 65(1): 179-84. https://doi.org/10.1111/jgs.14515
https://doi.org/10.1111/jgs.14515...
.
This study associated older adults hospitalized in the previous year with pre-frailty and frailty. A systematic review showed a significant relationship between frailty and a higher risk of hospitalization2828. Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012; 60(8): 1487-92. https://doi.org/10.1111/j.1532-5415.2012.04054.x
https://doi.org/10.1111/j.1532-5415.2012...
. Avila-Funes et al.4040. Avila-Funes JA, Helmer C, Amieva H, Barberger-Gateau P, Le Goff M, Ritchie K, et al. Frailty among community-dwelling elderly people in France: the three-city study. J Gerontol A Biol Sci Med Sci. 2008; 63A(10):1089-1096. monitored 6,030 French older adults, and, during the four years of follow-up, 30.2% of frail, 23.5% of pre-frail, and 20.5% of non-frail individuals had at least one hospitalization, regardless of their cognitive state.
This study associated multimorbidity with frailty, as did other studies2020. Vetrano DL, Palmer K, Marengoni A, Marzetti E, Lattanzio F, Roller-Wirnsberger R, et al. Frailty and multimorbidity: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci 2018. http://doi.org/10.1093/gerona/gly110
http://doi.org/10.1093/gerona/gly110...
,4141. Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493?737 UK Biobank participants. Lancet Public Health 2018; 3(7). https://doi.org/10.1016/S2468-2667(18)30091-4
https://doi.org/10.1016/S2468-2667(18)30...
. Bergman et al.4242. Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, et al. Frailty: an emerging research and clinical paradigm - issues and controversies. J Gerontol A: Biol Sci Med Sci 2007; 62(7): 731-7. believe in the probability that the frailty preceding the onset of chronic disease is only its subclinical and not diagnosed manifestation.
Frailty is not synonymous with multimorbidity and disability; each one has specific care needs for older adult patients1111. Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004; 59(3): 255-63.. The concept of frailty provides a foundation that departs from approaches based on organs and diseases to adopt one of integration based on health. Some studies suggest that increased vulnerability might precede the onset of chronic diseases4242. Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, et al. Frailty: an emerging research and clinical paradigm - issues and controversies. J Gerontol A: Biol Sci Med Sci 2007; 62(7): 731-7.,4343. Topinková E. Aging, disability and frailty. Ann Nutr Metab 2008; 52(Supl. 1): 6-11. https://doi.org/10.1159/000115340
https://doi.org/10.1159/000115340...
.
In the follow-up, we found that the frailty condition had worsened for most older adults - among individuals classified as non-frail at the beginning of the study, less than 50% remained in this group after four years.
Despite not being a condition inherent only to normal aging, frailty can progress as a result of physiological changes, regardless of diseases or incapacity, such as sarcopenia and anorexia related to aging. However, in most cases, frailty settles in more quickly or worsens with the presence of chronic diseases that accelerate the process of losing endurance to stressors. The data revealed in the present study corroborates this fact, given that 48.7% of non-frail participants remained in this category, despite their age, which demonstrates that frailty is not necessarily a condition inherent to normal aging - relatively healthy individuals can remain non-frail as they grow old.
In addition, another important result found was the fact that a significant part of the population reversed the development of the syndrome in the follow-up period. Among older adults considered frail at the beginning of the study, almost 51% changed their condition to pre-frail, that is, improved in one or more components. Most older adults classified as pre-frail at the beginning of the study remained in this condition, but approximately 28% moved to the non-frail group, that is, these individuals no longer scored in any component of the syndrome.
The longitudinal study Progetto Veneto Anziani, conducted with 2,925 individuals in Italy, revealed that among frail older adults approximately 40% died, and 26.5% returned to a pre-frail condition. Among non-frail subjects, 50% remained in this group, 26.7% became pre-frail, 6.3% progressed to frail, and 17.0% died. Out of pre-frail individuals, 12.3% reverted to non-frail, 20.7% became frail, and 36.4% continued in the same state3939. Trevisan C, Veronese N, Maggi S, Baggio G, Toffanello ED, Zambon S, et al. Factors influencing transitions between frailty states in elderly adults: The Progetto Veneto Anziani Longitudinal Study. J Am Geriatr Soc 2017; 65(1): 179-84. https://doi.org/10.1111/jgs.14515
https://doi.org/10.1111/jgs.14515...
.
This finding is important as it corroborates the assertion of researchers in the area who claim that frailty is a reversible syndrome, that is, with targeted preventive and recovery actions, it is possible to revert some of the components shown and reduce the risk of frailty44. Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.,3232. Alencar MA, Dias JMD, Figueiredo LC, Dias RC. Frailty and cognitive impairment among community-dwelling elderly. Arq Neuropsiquiatr 2013; 71(6): 362-7. https://doi.org/10.1590/0004-282X20130039
https://doi.org/10.1590/0004-282X2013003...
,4444. Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med 2006; 166(4): 418-23. https://doi.org/10.1001/archinte.166.4.418
https://doi.org/10.1001/archinte.166.4.4...
.
Effective interventions, such as physical activities, physiotherapy exercises, and adequate diet, not only can restrain the progress of the syndrome but reverse it after its establishment. Regular physical activity reduces the risk of frailty and promotes health benefits, including improved quality of life and reduced risk of chronic diseases4545. Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the Osteoarthritis Initiative: a graded relationship. Arthritis Rheum 2011; 63(1): 127-36. https://doi.org/10.1002/art.27760
https://doi.org/10.1002/art.27760...
,4646. Savela SL, Koistinen P, Stenholm S, Tilvis RS, Strandberg AY, Pitkälä KH, et al. Leisure-time physical activity in midlife is related to old age frailty. J Gerontol A Biol Sci Med Sci 2013; 68(11): 1433-8. https://doi.org/10.1093/gerona/glt029
https://doi.org/10.1093/gerona/glt029...
. Regarding adequate diet, the Study on Nutrition and Cardiovascular Risk Factors (Estudio de Nutrición y Riesgo Cardiovascular - ENRICA), developed in Spain during two years, with 2,614 older adults, showed associations between higher intake of animal protein and reduced risk of slow walking speed, and between higher intake of monounsaturated fatty acids and lower risk of unintentional weight loss4747. Sandoval-Insausti H, Pérez-Tasigchana RF, López-García E, García-Esquinas E, Rodríguez-Artalejo F, Guallar-Castillón P. Macronutrients intake and incident frailty in older adults: a prospective cohort study. J Gerontol A Biol Sci Med Sci [Internet] 2016 [acessado em 14 nov. 2017]; 71(10): 1329-34. Disponível em: https://doi.org/10.1093/gerona/glw033
https://doi.org/10.1093/gerona/glw033...
.
Lastly, the findings of this study can provide information about older adults with a high risk of disability and worse prognosis, and help to identify reversible risk factors.
CONCLUSION
The results of this study show that half of the older adults were frail or in the process of becoming frail and that the syndrome was associated with advanced age, functional impairment, multimorbidity, and cognitive decline.
Identifying the prevalence of frailty and its associated factors is important for the development of healthcare policies since this syndrome is predictable and preventable. Implementing adequate interventions can contribute to the treatment and reversal of the syndrome, which could improve the quality of life of older adults and delay adverse events.
REFERÊNCIAS
-
1Duarte YAO, Lebrão ML. Fragilidade e envelhecimento. In: Freitas EV, Py L, Cançado FAX, Doll J, Gorzoni ML. Tratado de geriatria e gerontologia. 3. ed. Rio de Janeiro: Guanabara Koogan; 2013. p. 1285-1298.
-
2Morley JE, Vellas B, Kan GA, Anker SD, Bauer JM, Bernabei R, et al. Frailty Consensus: A Call to Action. J Am Med Dir Assoc 2013; 14(6): 392-7. https://dx.doi.org/10.1016%2Fj.jamda.2013.03.022
» https://dx.doi.org/10.1016%2Fj.jamda.2013.03.022 -
3Nunes DP, Duarte YA, Santos JL, Lebrão ML. Screening for frailty in older adults using a self-reported instrument. Rev Saúde Pública. 2015; 49: 1-9.
-
4Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol 2001; 56(3): M146-56.
-
5Ho YY, Matteini AM, Beamer B, Fried L, Xue QL, Arking DE, et al. Exploring Biologically Relevant Pathways in Frailty. J Gerontol A Biol Sci Med Sci 2011; 66(9): 975-9. https://doi.org/10.1093/gerona/glr061
» https://doi.org/10.1093/gerona/glr061 -
6Lipsitz LA. Dynamics of stability: the physiologic basis of functional health and frailty. J Gerontol A Biol Sci Med Sci 2002; 57(3): B115-25.
-
7Ruggiero C, Ferrucci L. The endeavor of high maintenance homeostasis: resting metabolic rate and the legacy of longevity. J Gerontol A Biol Sci Med Sci 2006; 61(5): 466-71.
-
8Espinoza S, Walston JD. Frailty in older adults: insights and interventions. Cleve Clin J Med 2005; 72(12): 1105-12.
-
9Walston J, Hadley EC, Ferrucci L, Guralnik JM, Newman AB, Studenski SA, et al. Research agenda for frailty in older adults: toward a better understanding of physiology and etiology: summary from the American Geriatrics Society/National Institute on Aging Research Conference on Frailty in Older Adults. J Am Geriatr Soc 2006; 54(6): 991-1001. https://doi.org/10.1111/j.1532-5415.2006.00745.x
» https://doi.org/10.1111/j.1532-5415.2006.00745.x -
10Fried LP, Walston J. Frailty and failure to thrive. In: Hazzard W, Reubin A, editors. Principles of geriatric medicine and gerontology. 4ª ed. Nova York: McGraw-Hill; 1998. p. 1387-402.
-
11Fried LP, Ferrucci L, Darer J, Williamson JD, Anderson G. Untangling the concepts of disability, frailty, and comorbidity: Implications for improved targeting and care. J Gerontol A Biol Sci Med Sci 2004; 59(3): 255-63.
-
12Rockwood K, Mitnitski A. Frailty defined by deficit accumulation and geriatric medicine defined by frailty. Clin Geriatr Med 2011; 27(1): 17-26. http://doi.org/10.1016/j.cger.2010.08.008
» http://doi.org/10.1016/j.cger.2010.08.008 -
13United Nations. Department of Economic and Social Affairs - Population Division. World Population Prospects: The 2006 Revision. Nova York: United Nations; 2007.
-
14Masel MC, Graham JE, Reistetter TA, Markides KS, Ottenbacher KJ. Frailty and health related quality of life in older Mexican Americans. Health Qual Life Outcomes 2009; 7: 70. https://doi.org/10.1186/1477-7525-7-70
» https://doi.org/10.1186/1477-7525-7-70 -
15Farhat JS, Velanovich V, Falvo AJ, Horst HM, Swartz A, Patton JH, et al. Are the frail destined to fail? Frailty index as predictor of surgical morbidity and mortality in the elderly. J Trauma Acute Care Surg 2012; 72(6): 1526-31. https://doi.org/10.1097/TA.0b013e3182542fab
» https://doi.org/10.1097/TA.0b013e3182542fab -
16Ottenbacher KJ, Ostir GV, Peek MK, Snih SA, Raji MA, Markides KS. Frailty in older Mexican Americans. J Am Geriatr Soc 2005; 53(9): 1524-31. https://doi.org/10.1111/j.1532-5415.2005.53511.x
» https://doi.org/10.1111/j.1532-5415.2005.53511.x -
17Newman AB, Gottdiener JS, Mcburnie MA, Hirsch CH, Kop WJ, Tracy R, et al. Associations of subclinical cardiovascular disease with frailty. J Gerontol A Biol Sci Med Sci 2001; 56(3): M158-66.
-
18Alvarado BE, Zunzunegui MV, Béland F, Bamvita JM. Life course social and health conditions linked to frailty in Latin American older men and women. J Gerontol A Biol Sci Med Sci 2008; 63(12): 1399-406.
-
19Morley JE, Perry HM, Miller DK. Something about frailty. J Gerontol A Biol Sci Med Sci 2002; 57(11): M698-704.
-
20Vetrano DL, Palmer K, Marengoni A, Marzetti E, Lattanzio F, Roller-Wirnsberger R, et al. Frailty and multimorbidity: a systematic review and meta-analysis. J Gerontol A Biol Sci Med Sci 2018. http://doi.org/10.1093/gerona/gly110
» http://doi.org/10.1093/gerona/gly110 -
21González-Pichardo AM, Navarrete-Reyes AP, Adame-Encarnación H, Aguilar-Navarro S, García-Lara JM, Amieva H, et al. Association between self-reported health status and frailty in community-dwelling elderly. J Frailty Aging 2014; 3(2): 104-8. http://doi.org/10.14283/jfa.2014.9
» http://doi.org/10.14283/jfa.2014.9 -
22Vaughan L, Corbin AL, Goveas JS. Depression and frailty in later life: a systematic review. Clin Interv Aging 2015; 10: 1947-58. http://doi.org/10.2147/CIA.S69632
» http://doi.org/10.2147/CIA.S69632 -
23Makizako H, Shimada H, Doi T, Tsutsumimoto K, Suzuki T. Impact of physical frailty on disability in community-dwelling older adults: a prospective cohort study. BMJ Open 2015; 5(9): e008462. http://doi.org/10.1136/bmjopen-2015-008462
» http://doi.org/10.1136/bmjopen-2015-008462 -
24Batistoni SST, Neri AL, Cupertino APFB. Validade da escala de depressão do Center for Epidemiological Studies entre idosos brasileiros. Rev Saude Publica. 2007; 41(4):598-605.
-
25Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A Short Physical Performance Battery Assessing Lower-Extremity Function - Association With Self-Reported Disability And Prediction Of Mortality And Nursing-Home Admission. J Gerontol. 1994; 49(2): M85-M94.
-
26Almeida OP; , Almeida SA. Confiabilidade da versao brasileira da Escala de Depressao Geriatrica (GDS) versao reduzida. Arq Neuropsiquiatr, 1999, ; 57(12B): 421-426.
-
27Tribess S, Oliveira RJ. Síndrome da fragilidade biológica em idosos: revisão sistemática. Rev Salud Pública 2011; 13(5): 853-64. http://dx.doi.org/10.1590/S0124-00642011000500014
» http://dx.doi.org/10.1590/S0124-00642011000500014 -
28Collard RM, Boter H, Schoevers RA, Oude Voshaar RC. Prevalence of frailty in community-dwelling older persons: a systematic review. J Am Geriatr Soc 2012; 60(8): 1487-92. https://doi.org/10.1111/j.1532-5415.2012.04054.x
» https://doi.org/10.1111/j.1532-5415.2012.04054.x -
29Neri AL, Yassuda MS, Araújo LF, Eulálio MC, Cabral BE, Siqueira MEC, et al. Metodologia e perfil sociodemográfico, cognitivo e de fragilidade de idosos comunitários de sete cidades brasileiras: Estudo FIBRA. Cad Saúde Pública 2013; 29(4): 778-92. http://dx.doi.org/10.1590/S0102-311X2013000400015
» http://dx.doi.org/10.1590/S0102-311X2013000400015 -
30Silva RN, Guarda FRB, Hallal PC, Martelli PJL. Avaliabilidade do Programa Academia da Saúde no Município do Recife, Pernambuco, Brasil. Cad Saúde Pública 2017; 33(4): e00159415. http://dx.doi.org/10.1590/0102-311x00159415
» http://dx.doi.org/10.1590/0102-311x00159415 -
31Augusti ACV, Falsarella GR, Coimbra AMV. Análise da síndrome da fragilidade em idosos na atenção primária: Estudo transversal. Rev Bras Med Fam Comunidade 2017; 12(39): 1-9. https://doi.org/10.5712/rbmfc12(39)1353
» https://doi.org/10.5712/rbmfc12(39)1353 -
32Alencar MA, Dias JMD, Figueiredo LC, Dias RC. Frailty and cognitive impairment among community-dwelling elderly. Arq Neuropsiquiatr 2013; 71(6): 362-7. https://doi.org/10.1590/0004-282X20130039
» https://doi.org/10.1590/0004-282X20130039 -
33Chen S, Honda T, Narazaki K, Chen T, Nofuji Y, Kumagai S. Global cognitive performance and frailty in non-demented community-dwelling older adults: Findings from the Sasaguri Genkimon Study. Geriatr Gerontol Int 2016; 16(6): 729-36. https://doi.org/10.1111/ggi.12546
-
34Sánchez-García S, García-Peña C, Salvà A, Sánchez-Arenas R, Granados-García V, Cuadros-Moreno J, et al. Frailty in community-dwelling older adults: association with adverse outcomes. Clin Interv Aging 2017: 12; 1003-11. https://doi.org/10.2147/CIA.S139860
» https://doi.org/10.2147/CIA.S139860 -
35Fhon JRS, Rosset I, Freitas CP, Silva AO, Santos JLF, Rodrigues RAP. Prevalência de quedas de idosos em situacão de fragilidade. Rev Saúde Pública 2013; 47(2): 266-73. http://dx.doi.org/10.1590/S0034-8910.2013047003468
» http://dx.doi.org/10.1590/S0034-8910.2013047003468 -
36Ensrud KE, Ewing SK, Cawthon PM, Fink HA, Taylor BC, Cauley JA, et al. A comparison of frailty indexes for the prediction of falls, disability, fractures and mortality in older men. J Am Geriatr Soc 2009; 57(3): 492-8. http://dx.doi.org/10.1111/j.1532-5415.2009.02137.x
» http://dx.doi.org/10.1111/j.1532-5415.2009.02137.x -
37Santos-Eggimann B, Cuénoud P, Spagnoli J, Junod J. Prevalence of frailty in middle-aged and older community-dwelling Europeans living in 10 countries. J Gerontol A Biol Sci Med Sci 2009; 64(6): 675-81. https://doi.org/10.1093/gerona/glp012
» https://doi.org/10.1093/gerona/glp012 -
38Stringhini S, Dugravot A, Shipley M, Goldberg M, Zins M, Kivimäki M, et al. Health behaviours, socioeconomic status, and mortality: Further analyses of the British Whitehall II and the French GAZEL prospective cohorts. PLoS Med 2011; 8(2): e1000419. https://doi.org/10.1371/journal.pmed.1000419
» https://doi.org/10.1371/journal.pmed.1000419 -
39Trevisan C, Veronese N, Maggi S, Baggio G, Toffanello ED, Zambon S, et al. Factors influencing transitions between frailty states in elderly adults: The Progetto Veneto Anziani Longitudinal Study. J Am Geriatr Soc 2017; 65(1): 179-84. https://doi.org/10.1111/jgs.14515
» https://doi.org/10.1111/jgs.14515 -
40Avila-Funes JA, Helmer C, Amieva H, Barberger-Gateau P, Le Goff M, Ritchie K, et al. Frailty among community-dwelling elderly people in France: the three-city study. J Gerontol A Biol Sci Med Sci. 2008; 63A(10):1089-1096.
-
41Hanlon P, Nicholl BI, Jani BD, Lee D, McQueenie R, Mair FS. Frailty and pre-frailty in middle-aged and older adults and its association with multimorbidity and mortality: a prospective analysis of 493?737 UK Biobank participants. Lancet Public Health 2018; 3(7). https://doi.org/10.1016/S2468-2667(18)30091-4
» https://doi.org/10.1016/S2468-2667(18)30091-4 -
42Bergman H, Ferrucci L, Guralnik J, Hogan DB, Hummel S, Karunananthan S, et al. Frailty: an emerging research and clinical paradigm - issues and controversies. J Gerontol A: Biol Sci Med Sci 2007; 62(7): 731-7.
-
43Topinková E. Aging, disability and frailty. Ann Nutr Metab 2008; 52(Supl. 1): 6-11. https://doi.org/10.1159/000115340
» https://doi.org/10.1159/000115340 -
44Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med 2006; 166(4): 418-23. https://doi.org/10.1001/archinte.166.4.418
» https://doi.org/10.1001/archinte.166.4.418 -
45Dunlop DD, Song J, Semanik PA, Sharma L, Chang RW. Physical activity levels and functional performance in the Osteoarthritis Initiative: a graded relationship. Arthritis Rheum 2011; 63(1): 127-36. https://doi.org/10.1002/art.27760
» https://doi.org/10.1002/art.27760 -
46Savela SL, Koistinen P, Stenholm S, Tilvis RS, Strandberg AY, Pitkälä KH, et al. Leisure-time physical activity in midlife is related to old age frailty. J Gerontol A Biol Sci Med Sci 2013; 68(11): 1433-8. https://doi.org/10.1093/gerona/glt029
» https://doi.org/10.1093/gerona/glt029 -
47Sandoval-Insausti H, Pérez-Tasigchana RF, López-García E, García-Esquinas E, Rodríguez-Artalejo F, Guallar-Castillón P. Macronutrients intake and incident frailty in older adults: a prospective cohort study. J Gerontol A Biol Sci Med Sci [Internet] 2016 [acessado em 14 nov. 2017]; 71(10): 1329-34. Disponível em: https://doi.org/10.1093/gerona/glw033
» https://doi.org/10.1093/gerona/glw033
-
Financial support: Research Support Foundation of the State of São Paulo (Fundação de Amparo à Pesquisa do Estado de São Paulo - Fapesp)
Publication Dates
-
Publication in this collection
04 Feb 2019 -
Date of issue
2018
History
-
Received
27 July 2018 -
Reviewed
29 Aug 2018 -
Accepted
10 Sept 2018






 Source: SABE Study, 2006-2010.
Source: SABE Study, 2006-2010.