ABSTRACT
Introduction:
Care continuum models have supported recent strategies against sexually transmitted diseases, such as HIV and Hepatitis C (HCV).
Methods:
HIV, HCV, and congenital syphilis care continuum models were developed, including all stages of care, from promotion/prevention to clinical control/cure. The models supported the intervention QualiRede, developed by a University-Brazilian National Health System (SUS) partnership focused on managers and other professionals from six priority health regions in São Paulo and Santa Catarina. Indicators were selected for each stage of the care continuum from the SUS information systems and from the Qualiaids and QualiAB facility’s process evaluation questionnaires. The indicators acted as the technical basis of two workshops with professionals and managers in each region: the first one to identify problems and to create a Regional Technical Group; and the second one to design action plans for improving regional performance.
Results:
The indicators are available at www.qualirede.org. The workshops took place in the regions of Alto Tietê, Baixada Santista, Grande ABC, and Registro (São Paulo) and of Foz do Rio Itajaí (Santa Catarina), which resulted in regional action plans in São Paulo, but not in Santa Catarina. A lack of awareness was observed regarding the new HIV and HCV protocols, as well as an incipient use of indicators in routine practices.
Conclusion:
Improving the performance of the care continuum requires appropriation of performance indicators and coordination of care flows at local, regional, and state levels of management.
Keywords:
Sexually transmitted diseases; HIV; Hepatitis C; Health services; Care continuum; Health services evaluation
RESUMO
Introdução:
Modelos de cuidado contínuo baseiam recentes estratégias em HIV, infecções sexualmente transmissíveis e hepatite C (HCV).
Métodos:
Desenvolveram-se modelos de contínuo do cuidado em HIV, HCV e sífilis congênita incluindo todas as etapas da atenção, desde a promoção e a prevenção até o controle clínico/cura. O modelo baseou a intervenção QualiRede, desenvolvida em parceria entre universidade e Sistema Único de Saúde (SUS), direcionada a gestores e demais profissionais de 6 regiões de saúde prioritárias em São Paulo e Santa Catarina. Selecionaram-se indicadores para cada etapa do contínuo do cuidado, provenientes dos sistemas de informação do SUS e dos questionários de avaliação de processo Qualiaids e QualiAB. Os indicadores formaram a base técnica de duas oficinas com profissionais e gestores de cada região: a primeira para identificar problemas e formar um Grupo Técnico Regional; e a segunda para construir planos de ação e metas a fim de melhorar o desempenho regional.
Resultados:
Os indicadores estão disponíveis no website www.qualirede.org. As oficinas ocorreram em quatro regiões de São Paulo (Alto Tietê, Baixada Santista, Grande ABC e Registro) e uma região de Santa Catarina (Foz do Rio Itajaí), resultando em planos regionais em São Paulo, mas não em Santa Catarina. Observou-se domínio limitado dos novos protocolos para HIV e HCV e uso incipiente de indicadores na rotina dos serviços.
Conclusão:
Melhorar o desempenho do contínuo do cuidado exige apropriação dos indicadores de desempenho e coordenação integrada dos fluxos de atenção em todos os níveis de gestão.
Palavras-chave:
Infecções sexualmente transmissíveis; HIV; Hepatite C; Serviços de saúde; Continuidade da assistência ao paciente; Avaliação de serviços de saúde
INTRODUCTION
In Brazil, as worldwide, the need to integrate and improve comprehensive care practices in sexually transmitted infections (STI), HIV/AIDS, and hepatitis B and C is widely acknowledged. In the Brazilian National Health System (SUS), the care onto these diseases are performed by facilities of diverse institutional characteristics, care models and incorporation of resources and process technologies. The way to address these diseases has experienced important innovations in the decade of 2010: new treatment protocols for HIV11. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos. Brasília, DF; 2013. and hepatitis C22. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para hepatite viral C e coinfecções. Brasília, DF; 2016. and the use of medicines for post-exposure prophylaxis (PEP) (33. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para profilaxia antirretroviral pós-exposição de risco à infecção pelo HIV. Brasília, DF; 2015. and pre-exposure prophylaxis (Prep) (44. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância, Prevenção e Controle das Infecções Sexualmente Transmissíveis, do HIV/Aids e das Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para profilaxia pré-exposição (Prep) de risco à infecção pelo HIV. Brasília, DF; 2018. to HIV were incorporated. In the field of STI, vaccination against hepatitis B, besides composing the infant vaccination schedule, was extended to the general population55. Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Programa Nacional de Imunizações: aspectos históricos dos calendários de vacinação e avanços dos indicadores de coberturas vacinais, no período de 1980 a 2013. Boletim Epidemiológico [Internet]. Brasília, DF; 2015 [cited 2019 Feb 2];46(30). Available from: http://bit.ly/2XpfxzY. On the other hand, the number of cases of congenital syphilis is still distant from the elimination goal already achieved in several countries66. Taylor M, Newman L, Ishikawa N, Laverty M, Hayashi C, Ghidinelli M, et al. Elimination of mother-to-child transmission of HIV and Syphilis (EMTCT): process, progress, and program integration. PLoS Medicine. 2017;14(6):1-10. https://doi.org/10.1371/journal.pmed.1002329
https://doi.org/10.1371/journal.pmed.100...
), (77. World Health Organization. Pan American Health Organization. Elimination of mother-to-child transmission of HIV and syphilis in the Americas: update 2016. Washington, DC: PAHO; 2017..
In the international context, important changes in HIV care took place. The possibility of markedly reduce HIV transmission by patients with very low levels of viral load88. Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493-505. https://doi.org/10.1056/NEJMoa1105243
https://doi.org/10.1056/NEJMoa1105243...
supported the TasP (treatment as prevention) strategy, considered capable of ending the AIDS epidemic99. Joint United Nations Programme on HIV/AIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS; 2014.. This strategy started to guide a national response parameter to the epidemic based on a cascade model that estimates the number of people infected in the stages of engagement in the health system, illustrating the loss of follow up that occur between the diagnosis, linkage to the care, retention, initiation of antiretroviral therapy (ART), and suppression of viral load1010. Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793-800. https://doi.org/10.1093/cid/ciq243
https://doi.org/10.1093/cid/ciq243...
. The cascade supported the proposition, in 2013, of the new care strategy called “HIV Care Continuum” (1111. United States Department of Health and Human Services. The HIV/AIDS Continuum of Care. Washington, DC: DHHS; 2013..
In the same year, Brazil established the ART initiation protocol shortly after the diagnosis of HIV, regardless of the immune status of the patient11. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos. Brasília, DF; 2013.. In 2015, Brazil adopted the UNAIDS goal “90-90-90” (90% of those infected diagnosed, 90% of those diagnosed treated, 90% of those treated having viral suppression) (1010. Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793-800. https://doi.org/10.1093/cid/ciq243
https://doi.org/10.1093/cid/ciq243...
. The propositions of “combined prevention” (1212. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Prevenção combinada do HIV: bases conceituais para profissionais, trabalhadores(as) e gestores(as) de saúde. Brasília, DF; 2017.), (1313. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Prevenção combinada do HIV: sumário executivo. Brasília, DF; 2017. were also intensified, including antiretroviral drugs in the prophylaxis of sexual exposure1414. Grangeiro A, Ferraz D, Calazans G, Zucchi EM, Díaz-Bermúdez XP. The effect of prevention methods on reducing sexual risk for HIV and their potential impact on a large-scale: a literature review. Rev Bras Epidemiol. 2015;18(Suppl 1):43-62. http://dx.doi.org/10.1590/1809-4503201500050005
http://dx.doi.org/10.1590/1809-450320150...
.
Considering this international context, a pilot project that tested a method to improve networks of care in HIV and congenital syphilis was carried out at the health system of Bauru (SP) between 2013 and 2015 (PPSUS-Fapesp 2012/51223-7). Its objective was to promote a regional plan to improving the performance of services. Managers and professionals of all facilities involved in the care of these diseases, from primary care to major centers, were invited to take part in the workshops, as well as representatives of the organized civil society.
The support material brought together local indicators of process, outcomes, and impacts, presented according to the stages of a care continuum model. The new model expanded the original1515. McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26(14):1735-8. https://doi.org/10.1097/QAD.0b013e328355d67b
https://doi.org/10.1097/QAD.0b013e328355...
by including the stages of sexual and reproductive health promotion1616. Nasser MA, Nemes MIB, Andrade MC, do Prado RR, Castanheira ERL. Avaliação na atenção primária paulista: ações incipientes em saúde sexual e reprodutiva. Rev Saúde Pública. 2017;51:1-12. http://dx.doi.org/10.11606/s1518-8787.2017051006711
http://dx.doi.org/10.11606/s1518-8787.20...
and prevention of STI, also explaining priorities and main services for each stage. The project showed feasibility and acceptability1717. Loch AP, Nemes MIB, Alves AM, Castanheira ERL, Monroe AA, Nasser MA. Modelo do cuidado contínuo como base do fast-track: QualiRede, uma metodologia para ação local. Anais do 3º Congresso Brasileiro de Política, Planejamento e Gestão em Saúde; 29-30 ago. 2016; Florianópolis (SC). (Saúde & Transformação Social; vol. 7, Supl. 1:130).), (1818. Loch AP, Alves AM, Nasser MA, Mercuri J, Opromolla PA, Castanheira ERL, et al. Integração de indicadores de processo e resultados na elaboração participativa de plano para rede de cuidado local em DST, HIV e Hepatites Virais B e C. Anais 14º Congresso Paulista de Saúde Pública; 26-30 set. 2015; São Carlos (SP). São Paulo; 2015; 24:258-258., relying on logistic and technical support from the São Paulo State Program of STD/AIDS (PE-DST/Aids), integrating the local improvement initiative already in progress in the state1919. Secretaria de Estado da Saúde de São Paulo. Resolução nº 16, de 23 de fevereiro de 2015. Institui a Rede de Cuidados em DST/HIV/AIDS e Hepatites Virais no Estado de São Paulo e dá providencias correlatas. Diário Oficial do Estado de São Paulo [Internet]. 2015 fev 24 [cited 2019 Feb 2];1:33. Available from: http://bit.ly/2JfpF5F
http://bit.ly/2JfpF5F...
.
This initiative of São Paulo included viral hepatitis, which also underwent changes, especially the introduction of high-effectiveness drug treatment2020. Mesquita F, Santos ME, Benzaken A, Corrêa RG, Cattapan E, Sereno LS, et al. The Brazilian comprehensive response to hepatitis C: from strategic thinking to access to interferon-free therapy. BMC Public Health. 2016;16(1):1132. https://doi.org/10.1186/s12889-016-3784-4
https://doi.org/10.1186/s12889-016-3784-...
, incorporated into the Brazilian treatment protocol in 201622. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para hepatite viral C e coinfecções. Brasília, DF; 2016., and the proposition of a continuum model similar to the HIV model, the continuum of viral hepatitis services2121. World Health Organization. Global health sector strategy on viral hepatitis: Towards Ending Viral Hepatitis 2016-2021 [Internet]. Geneva; 2016 [cited 2019 Feb 2]. Available from: http://bit.ly/2Xu5Xfn
http://bit.ly/2Xu5Xfn...
.
The programmatic consonance of the pilot project with the initiatives of the SUS management to improve quality of care networks enabled the proposition of a similar methodology, now extended to hepatitis C (HCV): the intervention project QualiRede HIV, Hepatitis C, and Congenital Syphilis. This article aims to analyze the possibilities and limits of this intervention and contribute to the initiatives to improve care in HIV, HCV, and congenital syphilis at the various care levels of SUS.
METHODS
The QualiRede intervention was planned for six administrative health regions pointed by the state HIV program chiefs of São Paulo and Santa Catarina, the latter whose epidemiological situation had an initiative by the Department of Surveillance, Prevention, and Control of STI, HIV/AIDS, and Viral Hepatitis of the Ministry of Health (DIAHV) of an national cooperation to implement surveillance, prevention, and control actions of the HIV/AIDS epidemic, focused on 12 priority municipalities2222. Brasil. Ministério da Saúde. Termo de Cooperação assinado entre o Ministério da Saúde e a Secretaria Estadual de Saúde de Santa Catarina em 30 de setembro de 2015. Diário Oficial da União, Brasília, DF; 1º out. 2015;3:103.), (2323. Brasil. Ministério da Saúde. Portaria nº 1232, de 30 de junho de 2016. Autoriza o repasse financeiro ao estado de Santa Catarina para implementação de ações contingenciais de vigilância, prevenção e controle da epidemia de HIV/AIDS. Diário Oficial da União [Internet]. 1º jul. 2016 [cited 2019 Feb 2];1:85. Available from: http://bit.ly/2XpPJ1T
http://bit.ly/2XpPJ1T...
. This intervention was planned and conducted in a partnership between the Department of Preventive Medicine of the School of Medicine of the University of São Paulo; researchers from other universities; DIAHV; and the state programs of STD, HIV/AIDS, and viral hepatitis of São Paulo and Santa Catarina (QualiRede-PROADI-SUS 25000.169071/2015-41).
The methodology was guided by the following hypothesis about the situation of care to the focused problems: (1) there are accessible information systems that provide epidemiological, operational, and clinical outcome indicators, as well as reports of survey results with validated instruments for assessing the organization processes of HIV outpatient care. However, some of the managers and professionals had insufficient knowledge of these data or underutilized them; (2) the knowledge of new care technologies in HIV and HCV was insufficient in non-specialized services; (3) the communication between different health care levels was incipient, which aggravate the difficulty of disseminating and incorporating new technologies.
The main guideline for the intervention process was promoting the prominence of state, regional, and municipal managers and the engagement of health providers and who work in direct care in the different services. The first methodological step was to define the logical model of the intervention2424. Champagne F, Brouselle A, Hartz Z, Contandriopoulos AP. Modelizar as intervenções. In: Brouselle A, Champagne F, Contandriopoulos AP, Hartz Z, organizadores. Avaliação: conceitos e métodos. Rio de Janeiro: Fiocruz; 2011. p. 61-76. that explains the QualiRede model of the care continuum (Chart 1) and the indicators that would compose the technical basis of the intervention. The definition of indicators and all the other steps of the intervention were planned in meetings between the authors of this study and in both face-to-face and virtual meetings with managers of the federal and regional levels. Altogether, 39 meetings were held.
For each stage of the care continuum, process indicators of the local services were produced by the pre-validated evaluation questionnaires Qualiaids (to clinics that offer ART) (2525. Nemes MIB, Castanheira ERL, Loch AP, Santos MA, Alves AM, Melchior R, et al. Avaliação de serviços de saúde: a experiência do Qualiaids. Porto Alegre: Rede Unida; 2016. p. 99-152.), (2626. Loch AP, Nemes MIB, Santos MA, Alves AM, Melchior R, Basso CR, et al. Avaliação dos serviços ambulatoriais de assistência a pessoas vivendo com HIV no Sistema Único de Saúde: estudo comparativo 2007/2010. Cad Saúde Pública. 2018;34(2)e00047217. http://dx.doi.org/10.1590/0102-311x00047217
http://dx.doi.org/10.1590/0102-311x00047...
and QualiAB (to primary care services) (2727. Castanheira ERL, Nemes MIB, Almeida MASD, Puttini RF, Soares ID, Patrício KP, et al. QualiAB: desenvolvimento e validação de uma metodologia de avaliação de serviços de atenção básica. Saúde e Soc. 2011;20(4):935-947.. The Health Secretariats of both states decided to invite all registered services to answer the questionnaires, and not only the services of the QualiRede regions.
From the responses to the surveys, 132 Qualiaids indicators were selected, grouped into: General coordination of the work (26), General organization of medical and other professionals care (34), Activities of adherence to treatment and welcoming of new patients (15), Availability of inputs, medicines, lab exams, and referrals (49), and Use of records, evaluation and , monitorin (8). We selected 176 indicators of the QualiAB questionnaire, in its dimension of sexual and reproductive health (SSR) (2828. Nasser, M. A. Avaliação da implementação de ações em saúde sexual e reprodutiva desenvolvidas em serviços de atenção primária à saúde no estado de São Paulo. [tese de doutorado]. [São Paulo]: Faculdade de Medicina, Universidade de São Paulo; 2015., grouped into Promotion of sexual and reproductive health (48), Prevention and care to STI/AIDS (80), and Care to reproductive health (48).
Data were extracted from the SUS information systems to calculate state, regional, and municipal indicators related to clinical processes and outcomes (33) and population impact (8). From the data of the systems and the literature, the cascades of the diseases were estimated for each state. The indicators, classified by disease, region, and stage of the continuum, are published on the intervention website1 1 Available from: www.qualirede.org . Figure 1 shows the format of the cascades and examples of indicators collected.
The next steps consisted of organizing preparatory meetings in the seat municipality of each region, forming regional technical groups (GTR), and conducting regional workshops to elaborate action and goal plans, as summarized in Figure 2.
General model of the workshop methodology of the QualiRede intervention - HIV, congenital syphilis, hepatitis C, and participating regions, Brazil, 2016-2017.
Two workshops were planned in each region, consisting of presentation lecture, group work, and closing plenary. The work of the groups was organized by scripts previously elaborated according to the logical model adapted for each disease. Workshop 1 worked with the dissemination of the model and the identification of problems along the steps of the care continuum. Workshop 2 was structured to address the problems prioritized for each stage of the continuum, aiming to face them by the elaboration of action plans.
Participants were organized based on their preferences and participation in the care or management, to ensure that all groups were composed of participants from different care levels.
In the two workshops, the discussion was coordinated and registered by the project team. At the end of each workshop, the team performed an immediate evaluation on a discussion, and, subsequently, meetings to evaluate and adapt the next workshop scripts were carried out.
The GTR, composed of regional and municipal managers, acted in the definition of the guests for the workshops, in the prioritization of problems, and in the editing and implementation of the resulting action plans. Since the preparatory meeting and throughout the intervention, we sought to maintain the stimulus to its essential role in conducting the processes.
The project was submitted to the Research Ethics Committee of the School of Medicine of USP (CEP-FMUSP), under Protocol no. 15736, with approval on October 14, 2016.
RESULTS
In the first phase, of collection of process indicators, the response rate of the regions of the QualiRede project to Qualiaids was 100% in both states and, to QualiAB, 62% in São Paulo and 73% in Santa Catarina.
For the indicators from the SUS systems, there were difficulties in the collection of municipal indicators. Although the timely submission of 24 local indicators was agreed at the preparatory meeting for Workshop 1, of the 56 participating municipalities, only 10 sent part of the requested indicators and only four sent all of them.
The workshops took place in 2017, in four regions of São Paulo (Alto Tietê, Baixada Santista, Grande ABC, and Registro) and in one region of Santa Catarina (Foz do Rio Itajaí and priority municipalities). It was not possible to carry out the workshops in the Grande Florianópolis region. Considering the high response rate of the primary health care services of Santa Catarina to QualiAB, a workshop not foreseen in the original design was carried, for which the state coordination of primary care invited all managers and professionals of the state (Table 1). This workshop presented the results of QualiAB, with emphasis on the SSR dimension, and discussed ways of using the results to plan activities in municipal services and programs, highlighting the actions related to congenital syphilis.
In the five regions of QualiRede where Workshop 1 was held, 75% of Workshop 1 participants also attended Workshop 2.
The instability or absence of internet in all locations of the workshops precluded the use of the website and dissemination only took place in the form of slideshow.
The care continuum models guided the group activity. The discussion by stages of the continuum stimulated reports about the daily routine in the services and self-criticism about the insufficient systematization and evaluation of their work. However, there was difficulty in some groups, which tended to identify performance problems based on individual experiences, disregarding the indicators.
Awareness of HIV treatment protocols - the one from 2013, updated in 20182929. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para infecção pelo HIV em adultos. Brasília, DF; 2018., and that of post-sexual exposure prophylaxis from 20103030. Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Recomendações para terapia antirretroviral em adultos infectados pelo HIV - 2008: Suplemento III - Tratamento e prevenção. Brasília, DF: Ministério da Saúde; 2010. - was insufficient, mainly on the part of primary health care professionals. The incipient knowledge regarding the relevance of HCV testing in those older than 40 years and of the new treatment protocol was general, except for HCV care providers.
In São Paulo, the workshops resulted in the development of regional plans to address the identified problems and in the maintenance of GTR. The final edition of the plans of the four regions was released at the end of 2017, in a seminar that brought together members of the GTR, coordinators of the STD/AIDS and viral hepatitis programs and primary care, representatives of the central team of the Health Secretariat, and researchers of the involved universities. The GTR remain active in these regions, and the intervention model3131. Secretaria do Estado de São Paulo. Manual de apoio a consolidação da Rede de Cuidados para a resposta à sífilis congênita, ao HIV/Aids e às hepatites virais [Internet]. São Paulo; 2018 [cited 2019 Feb 2]. Available from: http://bit.ly/2JgnM8X
http://bit.ly/2JgnM8X...
), (3232. Secretaria de Estado da Saúde de São Paulo. Diretrizes para implementação da Rede de Cuidados em IST/HIV/Aids: manual de assistência [Internet]. São Paulo; 2017 [cited 2019 Feb 2]. Available from: http://bit.ly/2MAEi7h
http://bit.ly/2MAEi7h...
is being extended to 15 other regions (Chart 2).
Examples of results in 4 regions of the intervention and activities to expand the intervention model to other regions of São Paulo.
In Santa Catarina, the QualiRede workshops did not result in the creation of action plans, neither maintenance of the GTR, nor developments that are known by the state management of the program. There were also no reports of developments in the primary health care evaluation workshop.
At the end of each workshop, participants were asked to respond to a structured anonymous evaluation. Among the 688 respondents (85% of the participants), 91% agreed that “the formation of the groups provided qualified technical discussions”; 85%, that “the workshop participants represented the care network in the three diseases focused”; and 94%, that “the contents discussed were important to discuss the situation of the care network in the region.”
The website of the intervention, already mentioned, had low utilization. Among the respondents of the evaluation, 50% said they “did not access the website” and among those who accessed, only 16% “visited the pages of indicators.” An analysis conducted by Google Analytics showed that during the workshop period (April 20 to December 7, 2017), there were 794 accesses from only eight of the 56 municipalities that took part in the intervention. The website presents two videos about the intervention, also released on YouTube, which had, together, 246 views until October 2018.
DISCUSSION
The workshops, main tools of the QualiRede intervention, were feasible and acceptable in the four regions foreseen in São Paulo and in one of the two foreseen regions of Santa Catarina. However, important differences were observed in the implementation and the products of the workshops between the states.
The diversity of state contexts, alongside the difficulties of implementing care networks, can explain part of this difference. Recognized in several studies3333. Viana ALD, Bousquat A, Melo GA, De Negri Filho A, Medina MG. Regionalização e redes de saúde. Ciênc. Saúde Coletiva. 2018;23(6):1791-1798. http://dx.doi.org/10.1590/1413-81232018236.05502018
http://dx.doi.org/10.1590/1413-812320182...
), (3434. Martin LT, Plough A, Carman KG, Leviton L, Bogdan O, Miller CE. Strengthening integration of health services and systems. Health Aff. 2016;35(11):1976-1981. https://doi.org/10.1377/hlthaff.2016.0605
https://doi.org/10.1377/hlthaff.2016.060...
), (3535. Pratt R, Gyllstrom B, Gearin K, Lange C, Hahn D, Baldwin LM, et al. Identifying barriers to collaboration between primary care and public health: experiences at the local level. Public Health Rep. 2018;133(3):311-317. https://doi.org/10.1177/0033354918764391
https://doi.org/10.1177/0033354918764391...
, some of these difficulties constitute barriers for the implementation of networks, including the fragmentation of the health system, consisting of instances without administrative linkage and with little tradition of organizational linkage, which seems to have affected more negatively the context of the intervention in Santa Catarina.
Specifically, in Santa Catarina, it was possible to observe fragility in the articulation of the state level of the STI, HIV/AIDS, and viral hepatitis program with the municipal facilities. This fragility was partially tackled in the region of Foz do Rio do Itajaí, where it was possible to at least carry out the workshops; however, it prevented the intervention in the region of Grande Florianópolis, whose main municipality - Florianópolis - refused to answer QualiAB and take part in the intervention. Still, there was little commitment from the state level to integrate the actions of QualiRede with those of the national cooperation initiative. This insufficient commitment was also at the center of the failure of the workshops to create action plans.
The context was more favorable in São Paulo, where the DST/Aids State Program, although not administratively linked to care services, has a long tradition of group work, conducting discussion forums and activities of supervision, evaluation, and monitoring. Moreover, it has an organic partnership with the State Program of Viral Hepatitis and develops specific actions directed to primary care, in addition to maintaining a long research partnership with universities3636. Kalichman, AO. A integralidade no cuidado das pessoas vivendo com HIV e AIDS: a experiência do Centro de Referência e Treinamento em DST/AIDS da SES-SP [tese de doutorado]. [São Paulo]: Faculdade de Medicina da Universidade de São Paulo; 2016.. These characteristics, alongside the cooperation in the pilot project, enabled a better development of the intervention in São Paulo.
The continuous care models adapted to the three diseases played an essential role in the intervention. Operating as the guiding axes of the discussions, they allowed an appropriate degree of methodological conceptual homogeneity in the conduction of the groups by the coordinators and ensured that all stages of the continuum were addressed.
Thus, the methodology of Workshop 1 was adequate, because, by aiming to disseminate knowledge about the care continuum, it enabled the dissemination of new technologies of prevention and care. The composition of the groups, ensuring the presence of professionals who work directly with the diseases and at different levels of the network, contributed to this dissemination and for each participant to meet the practices of other professionals and the work developed at other levels of the network.
The inclusion of the stages of promotion and prevention in the care continuum was productive, because, although they are important in the discursive plan of SUS, preventive actions and, especially, promotion ones, are still incipient in the plan of the practices of the services, even among primary care, often pointed out as a strategic care level for these actions1616. Nasser MA, Nemes MIB, Andrade MC, do Prado RR, Castanheira ERL. Avaliação na atenção primária paulista: ações incipientes em saúde sexual e reprodutiva. Rev Saúde Pública. 2017;51:1-12. http://dx.doi.org/10.11606/s1518-8787.2017051006711
http://dx.doi.org/10.11606/s1518-8787.20...
), (3737. Ferraz DAS, Nemes MIB. Avaliação da implantação de atividades de prevenção das DST/AIDS na atenção básica: um estudo de caso na Região Metropolitana de São Paulo, Brasil. Cad. Saúde Pública. 2009;25(Suppl. 2):s240-s250. ttp://dx.doi.org/ 10.1590/S0102-311X2009001400006
ttp://dx.doi.org/ 10.1590/S0102-311X2009...
), (3838. Nasser MA, Nemes MIB, Andrade MC, Alves AM, Prado RR, Castanheira ERL. Desempenho de serviços de Atenção Primária do estado de São Paulo em saúde sexual e reprodutiva, segundo características organizacionais e locorregionais. BIS. 2016;17(2):6-18.), (3939. Sanine PR, Castanheira ERL, Nunes LO, Andrade MC, Nasser MA, Nemes MIB. Sífilis congênita: avaliação em serviços de Atenção Primária do estado de São Paulo, Brasil. BIS. 2016;17(2):128-38..
Still regarding the model, it is recognized in the international scenario that, even where the ART coverage has steadily increased, the HIV rate incidence decreases very slowly to achieve epidemic control. The enthusiasm that followed the “90-90-90” strategy has given rise to the emphasis on the need to articulate the dissemination of ART with prevention strategies4040. Bekker LG, Johnson L, Wallace M, Hosek S. Building our youth for the future. J the Int AIDS Soc. 2015;18(2 Suppl 1):20027. https://doi.org/10.7448/IAS.18.2.20027
https://doi.org/10.7448/IAS.18.2.20027...
and to propose continuum models of prevention (HIV prevention continuum) (4141. McNairy ML, El-Sadr WM. A paradigm shift: focus on the HIV prevention continuum. Clin Infect Dis. 2014;59(Suppl 1):S12-S15. https://doi.org/10.1093/cid/ciu251
https://doi.org/10.1093/cid/ciu251...
) or that combine prevention and treatment in the same model (status-neutral approach to HIV) (4242. Myers, JE, Braunstein, SL, Xia Q, Scanlin K, Edelstein Z, Harriman G, et al. Redefining prevention and care: a status-neutral approach to HIV. Open Forum Infect Dis. 2018;5(6):ofy097. https://doi.org/10.1093/ofid/ofy097
https://doi.org/10.1093/ofid/ofy097...
. The emphasis on prevention has also occurred in research on viral hepatitis4343. Heffernan A, Barber E, Cook NA, Gomaa AI, Harley YX, Jones CR, et al. Aiming at the global elimination of viral hepatitis: challenges along the care continuum. Open Forum Infect Dis. 2017;5(1):ofx252. https://doi.org/10.1093/ofid/ofx252
https://doi.org/10.1093/ofid/ofx252...
. Current studies show the usefulness of the care continuum construct to evaluate public health programs for other diseases4444. Perlman DC, Jordan AE, Nash D. Conceptualizing care continua: lessons from HIV, hepatitis C virus, tuberculosis and implications for the development of improved care and prevention continua. Front Public Health. 2017;4:296. https://doi.org/10.3389/fpubh.2016.00296
https://doi.org/10.3389/fpubh.2016.00296...
), (4545. Anderson ES, Galbraith JW, Deering LJ, Pfeil SK, Todorovic T, Rodgers JB, et al. Continuum of care for hepatitis c virus among patients diagnosed in the emergency department setting. Clin Infect Dis. 2017;64(11):1540-46. https://doi.org/10.1093/cid/cix163
https://doi.org/10.1093/cid/cix163...
.
The conduction of the intervention confirmed the hypothesis about the lack of knowledge of new technologies and communication between the various levels of the care network. There was also a lack of knowledge and use of the indicators available in the SUS information systems and in the reports of Qualiaids and QualiAB. This may explain part of the tendency of some groups to identify performance problems based on personal experiences, which, although valuable, are incapable, by themselves, of producing rational syntheses, as do the indicators.
The indicator-based approach, on the other hand, shows some flaws in the participants’ professional performance. This also makes the intervention be a new evaluative process, which can be uncomfortable for professionals who recognize possible flaws in their practices, sometimes entailing the denial of the situation revealed by the indicators. The very low number of consultations to the website, especially the indicators, confirms, on the one hand, the still incipient “culture” of evaluation and monitoring of SUS services, probably aggravated by the flawed computer and internet structure. However, the intervention was not able to trigger any changes in this situation. The practical impossibility of using the website during the workshops contributed to this situation. Similar international experiences that had a better result showed the importance of intensifying the “exercise” of using the website4646. Joshi A, Amadi C, Katz B, Kulkarni S, Nash D. A Human-Centered Platform for HIV Infection Reduction in New York: development and usage analysis of the Ending the Epidemic (ETE) dashboard. JMIR Public Health Surveill. 2017;3(4):e95. https://doi.org/10.2196/publichealth.8312), (4747. New York. Ending the Epidemic Dashboard. Ending the AIDS Epidemic in New York State by the end of 2020- [Internet]. 2019 [cited 2019 Feb 2]. Available from: www.etedashboardny.org
www.etedashboardny.org...
.
This study was limited to evaluating the panorama of the intervention process. Other implementation characteristics - positive and negative -, as well as the technical contents of the problems pointed out in the workshops and in the action plans, will be addressed in other publications.
CONCLUSIONS
The QualiRede intervention aimed to contribute to improve the performance of the health services involved in the regional networks of the care continuum in HIV, congenital syphilis, and hepatitis C, and was based on theoretical-methodological models adapted from the care continuum for each disease. The methods focused on conducting workshops with managers and other professionals from the regions to discuss and develop regional action plans based on indicators of process, outcomes, and local impacts related to each stage of the care continuum of the three diseases.
The implementation process took place according to the plan in five regions, but resulted in regional action plans in only four of them. In these, the GTR organized in the intervention remain in operation so far.
Both the use of the structured model of care in service network for each disease and the participatory methodology - both by the workshops with local managers and professionals and by the effective practical and theoretical partnership between the university team and the state management technical team of the STD/AIDS and viral hepatitis programs - contributed to the proper conduction of the intervention.
Further studies are needed to analyze the intervention in more detail, as well as its medium-term repercussions in terms of processes and outcomes. However, it is worth noting the impossibility of interventions with limited time and financing, such as survey projects, to overcome many of these limits.
In this sense, it is very promising to observe the current initiative to maintain the goals of the QualiRede intervention in some regions of the project, as well as its developments to other regions.
Acknowledgments
To the colleagues of DIAHV of the Ministry of Health, on behalf of Flávia Moreno A. de Souza, by the institutional support; to the colleagues of CRT STD/Aids SES/SP, on behalf of Artur O. Kalichman, by the logistic support; to the regional interlocutors of the Epidemiological Surveillance Groups (GVE) of the AIDS and Viral Hepatitis Programs and teams; to the professionals, managers, and members of civil society who participated in the project.
REFERENCES
-
1Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para manejo da infecção pelo HIV em adultos. Brasília, DF; 2013.
-
2Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para hepatite viral C e coinfecções. Brasília, DF; 2016.
-
3Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para profilaxia antirretroviral pós-exposição de risco à infecção pelo HIV. Brasília, DF; 2015.
-
4Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Departamento de Vigilância, Prevenção e Controle das Infecções Sexualmente Transmissíveis, do HIV/Aids e das Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para profilaxia pré-exposição (Prep) de risco à infecção pelo HIV. Brasília, DF; 2018.
-
5Brasil. Ministério da Saúde. Secretaria de Vigilância em Saúde. Programa Nacional de Imunizações: aspectos históricos dos calendários de vacinação e avanços dos indicadores de coberturas vacinais, no período de 1980 a 2013. Boletim Epidemiológico [Internet]. Brasília, DF; 2015 [cited 2019 Feb 2];46(30). Available from: http://bit.ly/2XpfxzY
-
6Taylor M, Newman L, Ishikawa N, Laverty M, Hayashi C, Ghidinelli M, et al. Elimination of mother-to-child transmission of HIV and Syphilis (EMTCT): process, progress, and program integration. PLoS Medicine. 2017;14(6):1-10. https://doi.org/10.1371/journal.pmed.1002329
» https://doi.org/10.1371/journal.pmed.1002329 -
7World Health Organization. Pan American Health Organization. Elimination of mother-to-child transmission of HIV and syphilis in the Americas: update 2016. Washington, DC: PAHO; 2017.
-
8Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, Kumarasamy N, et al. Prevention of HIV-1 infection with early antiretroviral therapy. N Engl J Med. 2011;365(6):493-505. https://doi.org/10.1056/NEJMoa1105243
» https://doi.org/10.1056/NEJMoa1105243 -
9Joint United Nations Programme on HIV/AIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Geneva: UNAIDS; 2014.
-
10Gardner EM, McLees MP, Steiner JF, Del Rio C, Burman WJ. The spectrum of engagement in HIV care and its relevance to test-and-treat strategies for prevention of HIV infection. Clin Infect Dis. 2011;52(6):793-800. https://doi.org/10.1093/cid/ciq243
» https://doi.org/10.1093/cid/ciq243 -
11United States Department of Health and Human Services. The HIV/AIDS Continuum of Care. Washington, DC: DHHS; 2013.
-
12Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Prevenção combinada do HIV: bases conceituais para profissionais, trabalhadores(as) e gestores(as) de saúde. Brasília, DF; 2017.
-
13Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Prevenção combinada do HIV: sumário executivo. Brasília, DF; 2017.
-
14Grangeiro A, Ferraz D, Calazans G, Zucchi EM, Díaz-Bermúdez XP. The effect of prevention methods on reducing sexual risk for HIV and their potential impact on a large-scale: a literature review. Rev Bras Epidemiol. 2015;18(Suppl 1):43-62. http://dx.doi.org/10.1590/1809-4503201500050005
» http://dx.doi.org/10.1590/1809-4503201500050005 -
15McNairy ML, El-Sadr WM. The HIV care continuum: no partial credit given. AIDS. 2012;26(14):1735-8. https://doi.org/10.1097/QAD.0b013e328355d67b
» https://doi.org/10.1097/QAD.0b013e328355d67b -
16Nasser MA, Nemes MIB, Andrade MC, do Prado RR, Castanheira ERL. Avaliação na atenção primária paulista: ações incipientes em saúde sexual e reprodutiva. Rev Saúde Pública. 2017;51:1-12. http://dx.doi.org/10.11606/s1518-8787.2017051006711
» http://dx.doi.org/10.11606/s1518-8787.2017051006711 -
17Loch AP, Nemes MIB, Alves AM, Castanheira ERL, Monroe AA, Nasser MA. Modelo do cuidado contínuo como base do fast-track: QualiRede, uma metodologia para ação local. Anais do 3º Congresso Brasileiro de Política, Planejamento e Gestão em Saúde; 29-30 ago. 2016; Florianópolis (SC). (Saúde & Transformação Social; vol. 7, Supl. 1:130).
-
18Loch AP, Alves AM, Nasser MA, Mercuri J, Opromolla PA, Castanheira ERL, et al. Integração de indicadores de processo e resultados na elaboração participativa de plano para rede de cuidado local em DST, HIV e Hepatites Virais B e C. Anais 14º Congresso Paulista de Saúde Pública; 26-30 set. 2015; São Carlos (SP). São Paulo; 2015; 24:258-258.
-
19Secretaria de Estado da Saúde de São Paulo. Resolução nº 16, de 23 de fevereiro de 2015. Institui a Rede de Cuidados em DST/HIV/AIDS e Hepatites Virais no Estado de São Paulo e dá providencias correlatas. Diário Oficial do Estado de São Paulo [Internet]. 2015 fev 24 [cited 2019 Feb 2];1:33. Available from: http://bit.ly/2JfpF5F
» http://bit.ly/2JfpF5F -
20Mesquita F, Santos ME, Benzaken A, Corrêa RG, Cattapan E, Sereno LS, et al. The Brazilian comprehensive response to hepatitis C: from strategic thinking to access to interferon-free therapy. BMC Public Health. 2016;16(1):1132. https://doi.org/10.1186/s12889-016-3784-4
» https://doi.org/10.1186/s12889-016-3784-4 -
21World Health Organization. Global health sector strategy on viral hepatitis: Towards Ending Viral Hepatitis 2016-2021 [Internet]. Geneva; 2016 [cited 2019 Feb 2]. Available from: http://bit.ly/2Xu5Xfn
» http://bit.ly/2Xu5Xfn -
22Brasil. Ministério da Saúde. Termo de Cooperação assinado entre o Ministério da Saúde e a Secretaria Estadual de Saúde de Santa Catarina em 30 de setembro de 2015. Diário Oficial da União, Brasília, DF; 1º out. 2015;3:103.
-
23Brasil. Ministério da Saúde. Portaria nº 1232, de 30 de junho de 2016. Autoriza o repasse financeiro ao estado de Santa Catarina para implementação de ações contingenciais de vigilância, prevenção e controle da epidemia de HIV/AIDS. Diário Oficial da União [Internet]. 1º jul. 2016 [cited 2019 Feb 2];1:85. Available from: http://bit.ly/2XpPJ1T
» http://bit.ly/2XpPJ1T -
24Champagne F, Brouselle A, Hartz Z, Contandriopoulos AP. Modelizar as intervenções. In: Brouselle A, Champagne F, Contandriopoulos AP, Hartz Z, organizadores. Avaliação: conceitos e métodos. Rio de Janeiro: Fiocruz; 2011. p. 61-76.
-
25Nemes MIB, Castanheira ERL, Loch AP, Santos MA, Alves AM, Melchior R, et al. Avaliação de serviços de saúde: a experiência do Qualiaids. Porto Alegre: Rede Unida; 2016. p. 99-152.
-
26Loch AP, Nemes MIB, Santos MA, Alves AM, Melchior R, Basso CR, et al. Avaliação dos serviços ambulatoriais de assistência a pessoas vivendo com HIV no Sistema Único de Saúde: estudo comparativo 2007/2010. Cad Saúde Pública. 2018;34(2)e00047217. http://dx.doi.org/10.1590/0102-311x00047217
» http://dx.doi.org/10.1590/0102-311x00047217 -
27Castanheira ERL, Nemes MIB, Almeida MASD, Puttini RF, Soares ID, Patrício KP, et al. QualiAB: desenvolvimento e validação de uma metodologia de avaliação de serviços de atenção básica. Saúde e Soc. 2011;20(4):935-947.
-
28Nasser, M. A. Avaliação da implementação de ações em saúde sexual e reprodutiva desenvolvidas em serviços de atenção primária à saúde no estado de São Paulo. [tese de doutorado]. [São Paulo]: Faculdade de Medicina, Universidade de São Paulo; 2015.
-
29Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Protocolo clínico e diretrizes terapêuticas para infecção pelo HIV em adultos. Brasília, DF; 2018.
-
30Brasil. Ministério da Saúde. Departamento de DST, Aids e Hepatites Virais. Recomendações para terapia antirretroviral em adultos infectados pelo HIV - 2008: Suplemento III - Tratamento e prevenção. Brasília, DF: Ministério da Saúde; 2010.
-
31Secretaria do Estado de São Paulo. Manual de apoio a consolidação da Rede de Cuidados para a resposta à sífilis congênita, ao HIV/Aids e às hepatites virais [Internet]. São Paulo; 2018 [cited 2019 Feb 2]. Available from: http://bit.ly/2JgnM8X
» http://bit.ly/2JgnM8X -
32Secretaria de Estado da Saúde de São Paulo. Diretrizes para implementação da Rede de Cuidados em IST/HIV/Aids: manual de assistência [Internet]. São Paulo; 2017 [cited 2019 Feb 2]. Available from: http://bit.ly/2MAEi7h
» http://bit.ly/2MAEi7h -
33Viana ALD, Bousquat A, Melo GA, De Negri Filho A, Medina MG. Regionalização e redes de saúde. Ciênc. Saúde Coletiva. 2018;23(6):1791-1798. http://dx.doi.org/10.1590/1413-81232018236.05502018
» http://dx.doi.org/10.1590/1413-81232018236.05502018 -
34Martin LT, Plough A, Carman KG, Leviton L, Bogdan O, Miller CE. Strengthening integration of health services and systems. Health Aff. 2016;35(11):1976-1981. https://doi.org/10.1377/hlthaff.2016.0605
» https://doi.org/10.1377/hlthaff.2016.0605 -
35Pratt R, Gyllstrom B, Gearin K, Lange C, Hahn D, Baldwin LM, et al. Identifying barriers to collaboration between primary care and public health: experiences at the local level. Public Health Rep. 2018;133(3):311-317. https://doi.org/10.1177/0033354918764391
» https://doi.org/10.1177/0033354918764391 -
36Kalichman, AO. A integralidade no cuidado das pessoas vivendo com HIV e AIDS: a experiência do Centro de Referência e Treinamento em DST/AIDS da SES-SP [tese de doutorado]. [São Paulo]: Faculdade de Medicina da Universidade de São Paulo; 2016.
-
37Ferraz DAS, Nemes MIB. Avaliação da implantação de atividades de prevenção das DST/AIDS na atenção básica: um estudo de caso na Região Metropolitana de São Paulo, Brasil. Cad. Saúde Pública. 2009;25(Suppl. 2):s240-s250. ttp://dx.doi.org/ 10.1590/S0102-311X2009001400006
» ttp://dx.doi.org/ 10.1590/S0102-311X2009001400006 -
38Nasser MA, Nemes MIB, Andrade MC, Alves AM, Prado RR, Castanheira ERL. Desempenho de serviços de Atenção Primária do estado de São Paulo em saúde sexual e reprodutiva, segundo características organizacionais e locorregionais. BIS. 2016;17(2):6-18.
-
39Sanine PR, Castanheira ERL, Nunes LO, Andrade MC, Nasser MA, Nemes MIB. Sífilis congênita: avaliação em serviços de Atenção Primária do estado de São Paulo, Brasil. BIS. 2016;17(2):128-38.
-
40Bekker LG, Johnson L, Wallace M, Hosek S. Building our youth for the future. J the Int AIDS Soc. 2015;18(2 Suppl 1):20027. https://doi.org/10.7448/IAS.18.2.20027
» https://doi.org/10.7448/IAS.18.2.20027 -
41McNairy ML, El-Sadr WM. A paradigm shift: focus on the HIV prevention continuum. Clin Infect Dis. 2014;59(Suppl 1):S12-S15. https://doi.org/10.1093/cid/ciu251
» https://doi.org/10.1093/cid/ciu251 -
42Myers, JE, Braunstein, SL, Xia Q, Scanlin K, Edelstein Z, Harriman G, et al. Redefining prevention and care: a status-neutral approach to HIV. Open Forum Infect Dis. 2018;5(6):ofy097. https://doi.org/10.1093/ofid/ofy097
» https://doi.org/10.1093/ofid/ofy097 -
43Heffernan A, Barber E, Cook NA, Gomaa AI, Harley YX, Jones CR, et al. Aiming at the global elimination of viral hepatitis: challenges along the care continuum. Open Forum Infect Dis. 2017;5(1):ofx252. https://doi.org/10.1093/ofid/ofx252
» https://doi.org/10.1093/ofid/ofx252 -
44Perlman DC, Jordan AE, Nash D. Conceptualizing care continua: lessons from HIV, hepatitis C virus, tuberculosis and implications for the development of improved care and prevention continua. Front Public Health. 2017;4:296. https://doi.org/10.3389/fpubh.2016.00296
» https://doi.org/10.3389/fpubh.2016.00296 -
45Anderson ES, Galbraith JW, Deering LJ, Pfeil SK, Todorovic T, Rodgers JB, et al. Continuum of care for hepatitis c virus among patients diagnosed in the emergency department setting. Clin Infect Dis. 2017;64(11):1540-46. https://doi.org/10.1093/cid/cix163
» https://doi.org/10.1093/cid/cix163 -
46Joshi A, Amadi C, Katz B, Kulkarni S, Nash D. A Human-Centered Platform for HIV Infection Reduction in New York: development and usage analysis of the Ending the Epidemic (ETE) dashboard. JMIR Public Health Surveill. 2017;3(4):e95. https://doi.org/10.2196/publichealth.8312
-
47New York. Ending the Epidemic Dashboard. Ending the AIDS Epidemic in New York State by the end of 2020- [Internet]. 2019 [cited 2019 Feb 2]. Available from: www.etedashboardny.org
» www.etedashboardny.org
-
1
Available from: www.qualirede.org
-
Financial support: Programa de Desenvolvimento Institucional do Sistema Único de Saúde (SUS); Fundação de Amparo à Pesquisa do Estado de São Paulo (Fapesp); Secretarias de Estado da Saúde de São Paulo e de Santa Catarina.
Publication Dates
-
Publication in this collection
26 Sept 2019 -
Date of issue
2019
History
-
Received
19 Mar 2019 -
Reviewed
21 May 2019 -
Accepted
24 May 2019

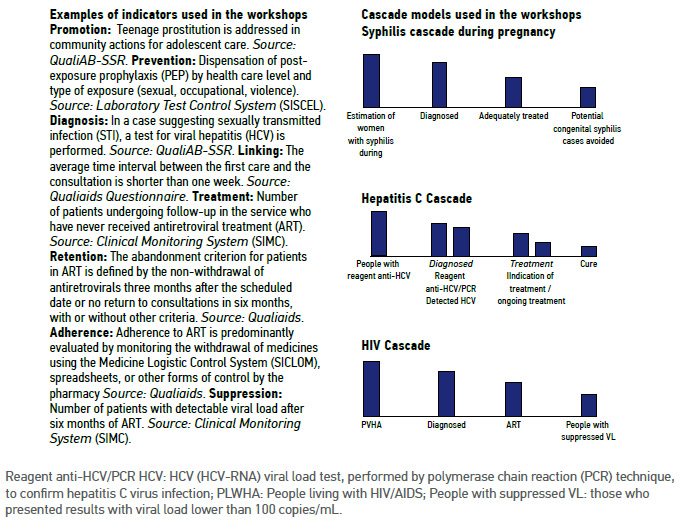 Reagent anti-HCV/PCR HCV: HCV (HCV-RNA) viral load test, performed by polymerase chain reaction (PCR) technique, to confirm hepatitis C virus infection; PLWHA: People living with HIV/AIDS; People with suppressed VL: those who presented results with viral load lower than 100 copies/mL.
Reagent anti-HCV/PCR HCV: HCV (HCV-RNA) viral load test, performed by polymerase chain reaction (PCR) technique, to confirm hepatitis C virus infection; PLWHA: People living with HIV/AIDS; People with suppressed VL: those who presented results with viral load lower than 100 copies/mL.
