Abstracts
PURPOSE:
to evaluate temporomandibular joint, mastication and deglutition in asymptomatic women with and without generalized joint hypermobility and the association between these variables.
METHODS:
forty-three volunteers were evaluated at the Speech-Language-Hearing Service of Federal University of Santa Maria. Hypermobility was evaluated according to the Beighton score and, based on the obtained scores, the volunteers were distributed into two groups: with (n=17) and without hypermobility (n=26). The temporomandibular joint was examined by Research Diagnostic Criteria for Temporomandibular Disorders instrument, and mastication and deglutition functions were assessed through a myofunctional orofacial assessment.
RESULTS:
the clinical evaluation of the temporomandibular joint showed predominance of joint sounds during jaw movement (52.9%) and mouth opening deviation (76.5%) in the hypermobility group, without statistical significant difference. In the examination of the masticatory function, although most of the volunteers showed a bilateral chewing pattern, the frequency of this pattern was significantly lower in the hypermobility group (p=0.05). A significant association (p=0.02) between chewing and mouth opening pattern was found only in the group without hypermobility, and there was no difference between groups regarding the deglutition function.
CONCLUSION:
asymptomatic women showed evidence that hypermobility predisposes the occurrence of mouth opening deviation and joint sounds. There was no difference in the deglutition function, but lower frequency of alternating bilateral chewing was found in the group with hypermobility compared to the group without hypermobility.
Joint Instability; Temporomandibular Joint; Mastication; Deglutition
OBJETIVO:
avaliar a articulação temporomandibular, as funções de mastigação e deglutição em mulheres assintomáticas com e sem hipermobilidade articular generalizada e a associação entre estas variáveis.
MÉTODOS:
foram avaliadas 43 voluntárias no Serviço de Atendimento Fonoaudiológico da Universidade Federal de Santa Maria. Ahipermobilidadefoi avaliada pelo Escore de Beighton e, a partir dos escores obtidos, as voluntárias foram distribuídas em dois grupos: com (n=17) e sem hipermobilidade (n=26). A articulação temporomandibular foi examinada pelo instrumento Critérios de Diagnóstico para Pesquisa de Desordens Temporomandibularese as funções de mastigação e deglutição foram avaliadas por meio do exame miofuncional orofacial.
RESULTADOS:
a avaliação clínica da articulação temporomandibular demonstrou predomínio de ruídos articulares durante movimentos mandibulares (52,9%) e de desvio na abertura da boca (76,5%) nas voluntárias do grupo com hipermobilidade, sem diferença significante entre os grupos. No exame da função mastigatória, apesar da maioria das voluntárias apresentar padrão de mastigação bilateral alternado, a frequência desse foisignificantemente menor no grupo com hipermobilidade (p=0,05). Foi verificada uma associação significante(p=0,02) entre o padrão de mastigação e de abertura da boca, apenas no grupo sem hipermobilidade, e não houve diferença na deglutição entre os grupos.
CONCLUSÃO:
as mulheres assintomáticas apresentaram indícios de que a hipermobilidade predispõe à ocorrência de desvio na abertura da boca e ruídos articulares. Não houve diferença na função de deglutição, porém verificou-se uma frequência menor de mastigação bilateral alternada no grupo com hipermobilidade em relação ao sem hipermobilidade.
Instabilidade Articular; Articulação Temporomandibular; Mastigação; Deglutição
Introduction
Generalized joint hypermobility (GJH) is an inherited non-pathologic clinical
condition; it represents an extreme variation of normal joint mobility in most of the
joints, including temporomandibular joint (TMJ)11. Egri D, Yoshinari NH. Hipermobilidade articular generalizada.
RevBrasReumatol. 1999;39(4):231-6.
2. Marino LHC, Lamari N, Marino Júnior NW. Hipermobilidade articular nos
joelhos da criança. ArqCiênc Saúde. 2004;11(2):2-4.
3. Cavenaghi S, Folchine ERA, Marino LHC, Lamari NM. Prevalência de
hipermobilidade articular e sintomas álgicos em trabalhadores industriais. ArqCiênc
Saúde. 2006;13(2):64-8.
-
44. Moraes DA, Baptista CA, Crippa JA, Louzada-Junior P. Tradução e
validação do The fivepartquestionnaire for identifyinghypermobility para a língua
portuguesa do Brasil. RevBrasReumatol. 2011;51(1):53-69..
Due to changes in the collagen that makes up the connective tissues of the body,
ligamentous laxity provides low afferent regulation to the muscle stretch receptor,
reducing proprioception. Thus, it follows that the movements of the joints are
impaired in subjects with GJH, because motor coordination depends crucially on
proprioceptive feedback 11. Egri D, Yoshinari NH. Hipermobilidade articular generalizada.
RevBrasReumatol. 1999;39(4):231-6.
,
33. Cavenaghi S, Folchine ERA, Marino LHC, Lamari NM. Prevalência de
hipermobilidade articular e sintomas álgicos em trabalhadores industriais. ArqCiênc
Saúde. 2006;13(2):64-8.
4. Moraes DA, Baptista CA, Crippa JA, Louzada-Junior P. Tradução e
validação do The fivepartquestionnaire for identifyinghypermobility para a língua
portuguesa do Brasil. RevBrasReumatol. 2011;51(1):53-69.
5. Grahame R. The hypermobility syndrome. Ann Rheum Dis.
1990;49:199-200.
-
66. Ferrell WR, Tennant N, Sturrock RD, Ashton L, Creed G, Brydson G et
al. Amelioration of Symptoms by Enhancement of Proprioception in Patients With Joint
Hypermobility Syndrome. Arthritis &Rheumatism.
2004;50(10):3323-8..
Although there are numerous studies that associate GJH and TMJ, there are few studies that investigate stomatognathic functions in hypermobile individuals. It is believed that the involvement of TMJ between hypermobile joints can affect the functions performed by the latter, due to resulting changes in proprioception and coordination.
One of the major stomathognatic functions is mastication, understood as a complex
sensory-motor activity whereby food is crushed and ground by means of a pattern of
rhythmic movements77. Marchesan IQ. Fundamentos em Fonoaudiologia: Aspectos clínicos da
motricidade oral. Rio de Janeiro: Guanabara Koogan, 2005.
8. Escudeiro Santos C, Freitas O, Spadaro ACC, Mestriner-Junior W.
Development of a colorimetric system for evaluation of the masticatory efficiency.
Braz Dent J. 2006;17(2):95-9.
9. van der Bilt A, Engelen L, Pereira LJ, van der Glass HW, Abbink JH.
Oral physiology and mastication. Physiology & Behavior.
2006;89:22-7.
10. Gomes SGF, Custodio W, Moura Jufer JS, Del Bel Cury AA, Rodrigues
Garcia RCM. Correlation of mastication and masticatory movements and effect of
chewing side preference. Braz Dent J. 2010;21(4):351-5.
11. Nascimento GKBO, Cunha DA, Lima LM, Moraes KJR, Pernambuco LA, Régis
RMFL et al. Eletromiografia de superfície do músculo masseter durante a mastigação:
uma revisão sistemática. Rev CEFAC. 2012;14(4):725-31.
-
1212. Ohkubo C, Morokuma M, Yoneyama Y, Matsuda R, Lee JS. Interactions
between occlusion and human brain function activities. Journal of Oral
Rehabilitation. 2013;40:119-29..
Aspects such as strength, time and type of mastication can be affected by changes in proprioception1313. van der Bilt A . Assessment of mastication with implications for oral rehabilitation: a review. Journalof Oral Rehabilitation. 2011;38:754-80., and changes in neuromuscular coordination may lead to mastication and deglutition disorders 77. Marchesan IQ. Fundamentos em Fonoaudiologia: Aspectos clínicos da motricidade oral. Rio de Janeiro: Guanabara Koogan, 2005. , 1414. Maciel CTV, Barbosa MH, Toldo CA, Faza FCB, Chiappetta ALML. Disfunções Orofaciais nos Pacientes em Tratamento Ortodôntico. Rev CEFAC. 2006;8(4)456-66..
Deglutition is a complex neuromuscular action comprising a set of coordinated motor mechanisms whose purpose is to take intraoral contents into the stomach 77. Marchesan IQ. Fundamentos em Fonoaudiologia: Aspectos clínicos da motricidade oral. Rio de Janeiro: Guanabara Koogan, 2005. , 1515. Mezzomo CL, Machado PG, Pacheco AB, Gonçalves BFT, Hoffmann CF. As implicações da classe II de Angle e da desproporção esquelética tipo classe II no aspecto miofuncional. Rev CEFAC. 2011;13(4)728-34.. For deglutition to take place normally, balance between the perioral, masticatory and tongue muscles is required. Any disruption of this balance may lead to changes in deglutition1616. Fernandes LFT, Kochenborger R, Woitchunas FE, Woitchunas DR. A influência da deglutição atípica no padrão craniofacial e na morfologia mandibular. RFO. 2010;15(1):52-7..
Knowledge of the effect of GJH on TMJ may contribute to clinical practice, because joint instability can hinder the maintenance of the results of myofunctional therapy. Given the above, the objective of this research was to evaluate TMJ and mastication and deglutition in asymptomatic women with and without GJH.
Methods
This research is an observational, cross-sectional controlled study with a quantitative approach. The study was part of the project Cranio-cervical-mandibular system: diagnosis and multifactorial therapy. It was approved by the Research Ethics Committee of the Federal University of Santa Maria (UFSM) under protocol number 23081.019091/2008-65, according to Resolution no. 196/1996.
The research was conducted at the Laboratory of Orofacial Motricity of the Speech-Language-Hearing Service (SAF-UFSM) (Santa Maria, RS).
Inclusion criteria were: females, aged between 18 and 35 years, who have signed an Informed Consent Form. Exclusion criteria: tooth loss (more than two teeth - except for third molar); use of dental prosthesis; signs of psychomotor impairment; malformations, tumors, surgery or trauma in the head and neck; prior or current speech therapy and physical therapy for orofacial motricity; symptoms of TMJ pain, mouth breathing, and subjects who did not complete the evaluations.
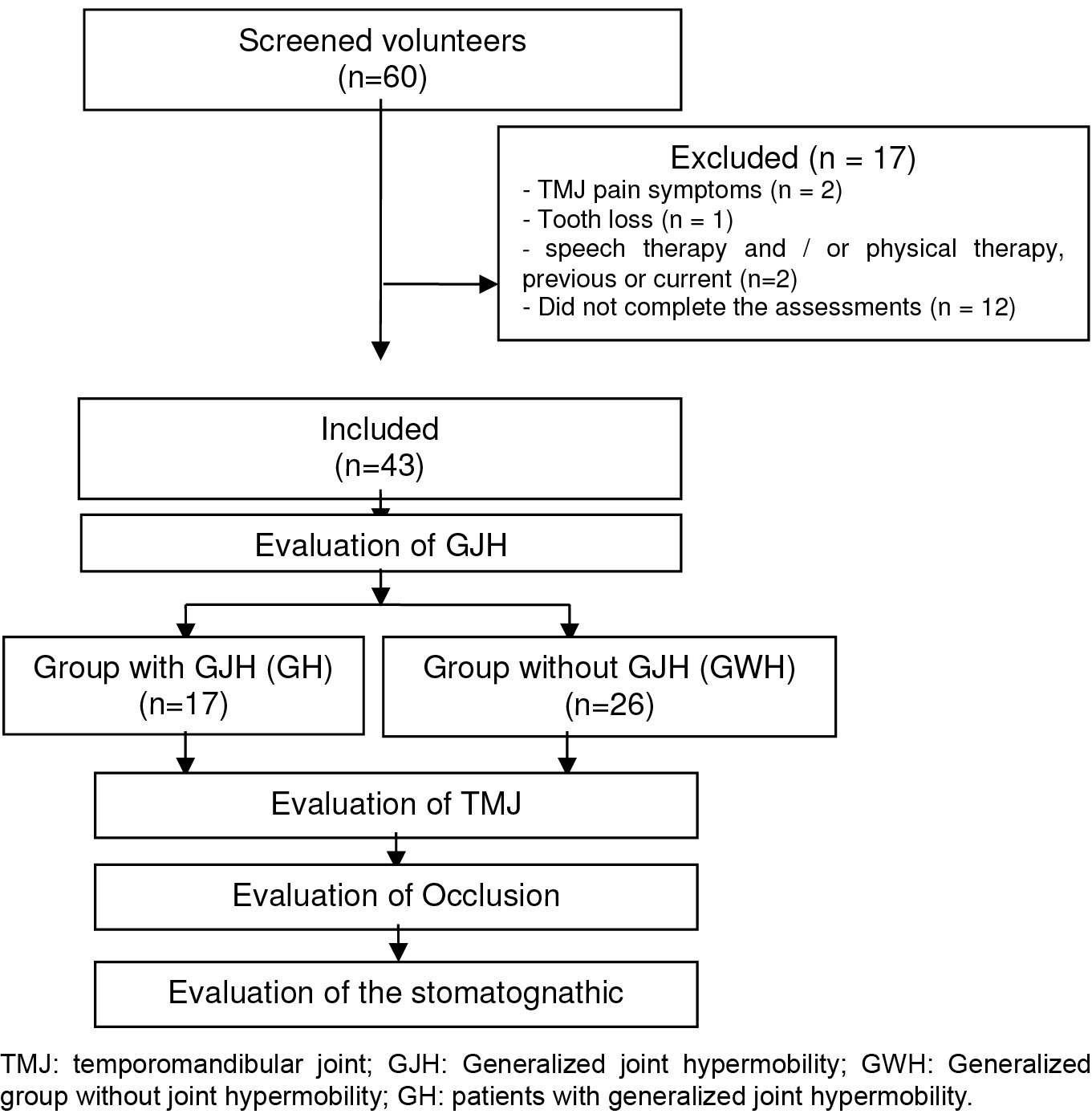
Data collection procedures occurred as shown in the flow chart in Figure 1.
Women who met the inclusion criteria were evaluated by a physical therapist and a speech therapist, who had experience in orofacial motricity. The physical therapist assessed the presence of GJH and TMJ, and the speech therapist performed the protocol of orofacial myofunctional assessment.
GJH was evaluated by the criteria of Carter and Wilkinson, modified by Beighton1717. Beighton P, Solomon L, Soskolne CL. Articular mobility in a African population. Ann Rheum Dis. 1973;(32):413-8., comprising five tests, as shown in Figure 2 (Beighton Score) 1818. Pasinato F, Souza JA, Corrêa ECR, Silva AMT. Temporomandibular disorder and generalized joint hypermobility: application of diagnostic criteria. Braz. j. otorhinolaryngol, 2011;77(4):418-25..
The scale ranges from zero to nine points. GJH is observed in individuals with scores equal to or greater than four points. Based on the scores they had in this test, the volunteers were distributed into two groups: with GJH (GH) and without GJH (GWH).
The TMJ of the volunteers was assessed by a trained physical therapist with Axis I of the Research Diagnostic Criteria for Temporomandibular Disorders (RDC/ TMD) 1919. Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibulardisoders: Review, criteria, examinations and specifications, critique. Journal of Craniomandibular Disorders. 1992;6:301-55. in order to determine the range of jaw motion and signs that could be related to GJH, such as presence of joint sounds and jaw opening deviations.
The stomatognathic system was evaluated by a speech therapist using the MBGR 2020. Genaro KF, Berretin-Felix G, Rehder MIBC, Marchesan IQ . Avaliação Miofuncional Orofacial - Protocolo MBGR. Rev CEFAC. 2009;11(2):237-55. protocol, which encompasses an orofacial myofunctional assessment. The mastication and deglutition functions were recorded on video.
Bread rolls were offered as food for assessment of mastication. The volunteers were instructed to chew and swallow as usual, and the test was repeated three times. Then, deglutition of liquids was performed, using 200 ml of water, offered in a transparent plastic cup.
The video recordings were analyzed by three speech therapists, and the following aspects of deglutition were taken into account: biting, crushing, chewing pattern, lip closure and atypical muscle contractions. Analysis of deglutition focused on lip closure, lip posture, food holding behavior, atypical muscle contractions and coordination. The speech therapists were blinded to the presence of GJH, and the degree of agreement between the analyses was obtained by the Kappa coefficient.
The Kappa coefficient values were interpreted as no agreement (K <0), slight agreement (K = 0-0.20), fair agreement (K = 0.21 to 0.40), moderate agreement (K = 0, 41-.60), substantial agreement (K = 0.60-0.80) and almost perfect agreement (K> 0.80) 2121. Viera AJ, Garret JM. Understanding Interobserver Agreement: The Kappa Statistic. Research Series. 2005;37(5):360-3. , 2222. Pacheco AB . Avaliação antroposcópica e cefalométrica do perfil e da tendência facial e sua relação com as funções estomatognáticas [Dissertação]. Santa Maria (RS): Universidade Federal de Santa Maria; 2013..
The remaining analyses were performed using software Statistica version 9.0 for Windows. Descriptive statistics were determined for all variables, and chi-square or Fisher's exact tests were used to assess the association between: chewing pattern, presence of atypical contractions during mastication and deglutition; presence of noise and mouth opening pattern, assuming a significance level of 5%.
Results
Forty-three volunteers met the inclusion criteria and completed the evaluations. Twenty-six of them took part of the group without GJH (GWH) (60.5%), with a mean age and standard deviation of 23.3 ± 4.9 years; and 17 of them took part of the group with GJH (GH) (39.5%) with a mean age and standard deviation of 23.5 ± 4.4 years.
According to the assessment by the RDC/TMD instrument, measures of range of jaw motion were within the normal range 2323. Pehling J, Schiffman E, Look J, Shaefer J, Lenton P, Fricton J. Interexaminer Reliability and Clinical Validity of the Temporomandibular Index: A New Outcome Measure for Temporomandibular Disorders. J OrofacPain. 2002;16(4):296-304., and there was no difference between groups (Table 1).
The presence of joint sounds during jaw motion prevailed in GH (52.9%), compared with GWH (38.5%), but this difference was not significant (p = 0.56).
Table 2 shows the pattern of mouth opening evaluated in the volunteers, which showed high prevalence of uncorrected deviation, especially in GH, although there was no significant difference.
The analysis of mastication and deglutition showed that all volunteers presented the following aspects: biting, crushing, lip closure, lip posture, food holding behavior and unchanged coordination. Bilateral chewing pattern predominated in both groups, but there was a significantly lower frequency of this pattern in GH (p = 0.05) (Table 3). The presence of atypical muscle contractions was observed both in mastication and in deglutition, with no significant difference between groups (Figure 3).
Frequency of atypical contractions during mastication and deglutition in patients with and without generalized joint hypermobility.
The kappa coefficient was used to describe the degree of agreement between the speech therapists who evaluated mastication and deglutition. Such coefficient showed slight agreement (K = 0.17) for the variable atypical contractions during mastication, and fair agreement for the variables chewing pattern (K = 0.34) and atypical contractions in deglutition (K = 0.22).
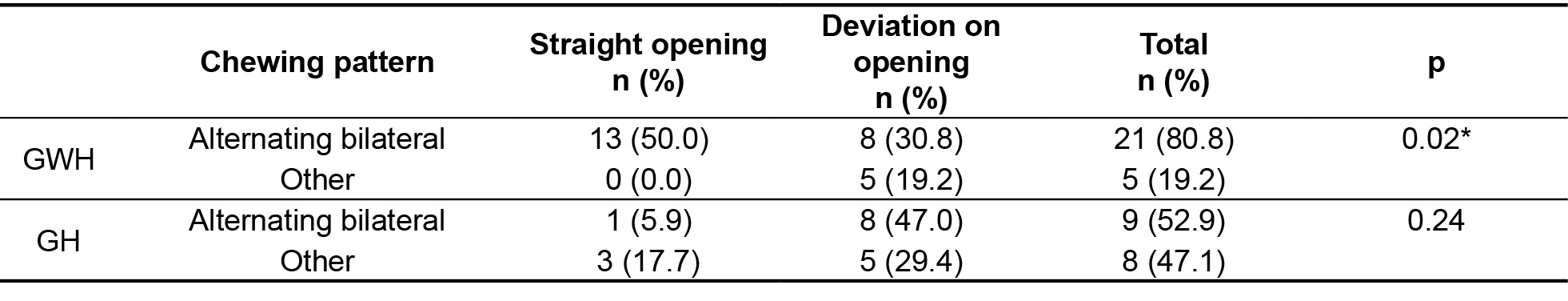
Associations between chewing pattern, presence of atypical contractions in mastication and deglutition, presence of noise and standard mouth opening were analyzed. There was only one significant association between chewing and mouth opening patterns in GWH (Table 4).
Discussion
The evaluation of TMJ by the RDC/TMD instrument showed that GJH did not influence the range of jaw motion. However, joint sounds were present with the highest percentage in GH (52.9%). Similar results were found in a study 2424. Hirsch C, John MT, Stang A. Association between generalized joint hypermobility and signs and diagnoses of temporomandibular disorders. Eur J Oral Sci. 2008;116:525-30. that used the same tools to evaluate GJH and the evaluation of TMJ, namely the Beighton criteria and the RDC/TMD, respectively.
This study2424. Hirsch C, John MT, Stang A. Association between generalized joint hypermobility and signs and diagnoses of temporomandibular disorders. Eur J Oral Sci. 2008;116:525-30. investigated 893 subjects aged between 20 and 60 years, 8.4% of them with GJH, and found increased risk of cracking sounds in hypermobile individuals (70%), although there was no TMJ pain, whether myofascial pain or arthralgia. However, other studies1818. Pasinato F, Souza JA, Corrêa ECR, Silva AMT. Temporomandibular disorder and generalized joint hypermobility: application of diagnostic criteria. Braz. j. otorhinolaryngol, 2011;77(4):418-25. , 2525. Sáez-Yuguero MR, Linares-Tovar E, Calvo-Guirado JL, Bermejo-Fenoll A, Rodríguez-Lozano F. Joint hypermobility and disk displacement confirmed by magnetic resonance imaging: A study of women with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2009;107(6):54-7., which also used the Beighton criteria, found no association between GJH and TMD.
Besides the presence of noise, deviation of mouth opening did not differ significantly between groups, but volunteers from GH had a higher percentage of uncorrected deviation. This may be indicative of disk displacement 2626. Teixeira MJ, Siqueira JTT. Dores Orofaciais: diagnóstico e tratamento. São Paulo: Artes Médicas, 2012., and it may also result from anatomical changes such as condylar hypoplasia, joint inflammation, lack of occlusal guides2727. Chiodelli L, Weber P, Pasinato F, Souza JA, Corrêa ECR . Manifestações clínicas de desordem temporomandibular e inclinação lateral da cabeça. Ter Man. 2012;10(50):383-8. , 2828. Figueiredo VMG, Cavalcanti AL, Farias ABL, Nascimento SR. Prevalência de sinais, sintomas e fatores associados em portadores de disfunção temporomandibular. Acta. Sci. Health. Sci. 2009;31(2):159-63., and masticatory muscle imbalance.
Such an imbalance can occur in individuals with GJH due to joint instability associated with proprioceptive deficits. The reduction of proprioception in individuals with GJH should be considered, because it seems to affect the pattern of muscle electrical activity, force, motion, as well as time and pattern of chewing1313. van der Bilt A . Assessment of mastication with implications for oral rehabilitation: a review. Journalof Oral Rehabilitation. 2011;38:754-80. , 2929. Pasinato F, Souza JA, Corrêa ECR, Silva AMT . Temporomandibular disorder and generalized joint hypermobility: electromyographic analysis of the masticatory muscles. Braz J Oral Sci. 2011;10(2):146-51. , 3030. Gomes SGF, Custodio W, Faot F, Del BelCury AA, Garcia RCMR. Chewing side, bite force symmetry, and occlusal contact area of subjects with different facial vertical patterns. Braz Oral Res. 2011;25(5):446-52..
As for stomatognathic functions, it is known that alternating bilateral chewing is essential for prevention of myofunctional disorders, periodontal problems and TMD 77. Marchesan IQ. Fundamentos em Fonoaudiologia: Aspectos clínicos da motricidade oral. Rio de Janeiro: Guanabara Koogan, 2005. , 1010. Gomes SGF, Custodio W, Moura Jufer JS, Del Bel Cury AA, Rodrigues Garcia RCM. Correlation of mastication and masticatory movements and effect of chewing side preference. Braz Dent J. 2010;21(4):351-5. , 3131. Slavicek G, Schimmer C. Analysis of human mastigation behavior: a new approach using planar calculations of fragmented chewing sequences. J. Stomat. Occ. Med. 2010;3(1):61-7.. In this study, although most of the volunteers from both groups have shown this pattern, a higher and significant percentage of the volunteers from GH showed changes in mastication. In GWH, on the other hand, there was prevalence of alternating bilateral chewing as well as mouth opening without deviation, with significant association between these variables.
These results corroborate previous studies66. Ferrell WR, Tennant N, Sturrock RD, Ashton L, Creed G, Brydson G et al. Amelioration of Symptoms by Enhancement of Proprioception in Patients With Joint Hypermobility Syndrome. Arthritis &Rheumatism. 2004;50(10):3323-8. , 3232. Simpson MR. Benign Joint Hypermobility Syndrome: Evaluation, Diagnosis, and Management. J Am Osteopath Assoc. 2006;106(9):531-6., in which hypermobile subjects had impaired proprioceptive feedback. Although these studies have not investigated TMJ, it is suggested that women without GJH, in the present study, showed better stability and neuromuscular coordination.
There was no difference between groups for the presence of atypical contractions during mastication and deglutition. A recent study3333. Weber P, Corrêa ECR, Bolzan GP, Ferreira FDS, Soares JC, Silva AMT . Mastigação e deglutição em mulheres jovens com desordem temporomandibular. CoDAS. 2013;25(4):375-80. found that effort of the lips and exaggerated involvement of the perioral muscles occurred more frequently in a group with TMD. This finding is corroborated by the presence of painful symptoms. This study does not corroborate the present research because an exclusion criterion of the study was the presence of TMJ pain.
Painful symptoms could be a confounding factor in the results, as facial pain can impair the action of the masticatory muscles and hence, the stomatognathic functions3333. Weber P, Corrêa ECR, Bolzan GP, Ferreira FDS, Soares JC, Silva AMT . Mastigação e deglutição em mulheres jovens com desordem temporomandibular. CoDAS. 2013;25(4):375-80..
In this study, the aspects relative to deglutition appeared to be normal, except for the presence of atypical contractions during deglutition, which occurred in both groups, with no difference between them. No studies, to date, have investigated deglutition in patients with GJH; however, it is suggested that atypical contractions have occurred due to an imbalance between perioral, masticatory and tongue muscles1616. Fernandes LFT, Kochenborger R, Woitchunas FE, Woitchunas DR. A influência da deglutição atípica no padrão craniofacial e na morfologia mandibular. RFO. 2010;15(1):52-7., and this was not associated with GJH.
Stomatognathic functions were evaluated by three speech therapists, and the agreement between them ranged from slight to fair (K = 0.17, 0.34 and 0.22). This aspect agrees with a recent study2222. Pacheco AB . Avaliação antroposcópica e cefalométrica do perfil e da tendência facial e sua relação com as funções estomatognáticas [Dissertação]. Santa Maria (RS): Universidade Federal de Santa Maria; 2013.which used the same protocol, and observed moderate agreement for deglutition (K = 0.50) and almost perfect agreement for the masticatory variables (K = 0.94). Because it is a subjective test, the analysis of the results obtained in myofunctional evaluation depends on the experience and perception of each judge; thus, training and calibration of judges is crucial.
Besides the low agreement between speech therapist evaluations, this study did not evaluate dental occlusion and did not address aspects such as tone of masticatory muscles and facial asymmetry. Thus, it is suggested that these issues are investigated in future studies. These aspects, as well as sample size, can be considered as limitations of this study.
The influence of GJH on TMJ and the masticatory function justifies the importance of diagnosis and multidisciplinary attention to this condition. Physical therapy can both prevent and treat TMD, promoting better joint stability in hypermobile individuals. Still, it is speculated that physical therapy, through the strengthening of masticatory muscles, helps maintain the results of orofacial myofunctional therapy. Further research is suggested to support the need for such treatment.
Conclusion
Asymptomatic women evaluated in this study showed signs that hypermobility predisposes the occurrence of mouth opening deviation and joint noises. There was no difference in the deglutition function, but there was a lower frequency of the alternating bilateral chewing pattern in the group with hypermobility compared with the group without hypermobility.
-
1Egri D, Yoshinari NH. Hipermobilidade articular generalizada. RevBrasReumatol. 1999;39(4):231-6.
-
2Marino LHC, Lamari N, Marino Júnior NW. Hipermobilidade articular nos joelhos da criança. ArqCiênc Saúde. 2004;11(2):2-4.
-
3Cavenaghi S, Folchine ERA, Marino LHC, Lamari NM. Prevalência de hipermobilidade articular e sintomas álgicos em trabalhadores industriais. ArqCiênc Saúde. 2006;13(2):64-8.
-
4Moraes DA, Baptista CA, Crippa JA, Louzada-Junior P. Tradução e validação do The fivepartquestionnaire for identifyinghypermobility para a língua portuguesa do Brasil. RevBrasReumatol. 2011;51(1):53-69.
-
5Grahame R. The hypermobility syndrome. Ann Rheum Dis. 1990;49:199-200.
-
6Ferrell WR, Tennant N, Sturrock RD, Ashton L, Creed G, Brydson G et al. Amelioration of Symptoms by Enhancement of Proprioception in Patients With Joint Hypermobility Syndrome. Arthritis &Rheumatism. 2004;50(10):3323-8.
-
7Marchesan IQ. Fundamentos em Fonoaudiologia: Aspectos clínicos da motricidade oral. Rio de Janeiro: Guanabara Koogan, 2005.
-
8Escudeiro Santos C, Freitas O, Spadaro ACC, Mestriner-Junior W. Development of a colorimetric system for evaluation of the masticatory efficiency. Braz Dent J. 2006;17(2):95-9.
-
9van der Bilt A, Engelen L, Pereira LJ, van der Glass HW, Abbink JH. Oral physiology and mastication. Physiology & Behavior. 2006;89:22-7.
-
10Gomes SGF, Custodio W, Moura Jufer JS, Del Bel Cury AA, Rodrigues Garcia RCM. Correlation of mastication and masticatory movements and effect of chewing side preference. Braz Dent J. 2010;21(4):351-5.
-
11Nascimento GKBO, Cunha DA, Lima LM, Moraes KJR, Pernambuco LA, Régis RMFL et al. Eletromiografia de superfície do músculo masseter durante a mastigação: uma revisão sistemática. Rev CEFAC. 2012;14(4):725-31.
-
12Ohkubo C, Morokuma M, Yoneyama Y, Matsuda R, Lee JS. Interactions between occlusion and human brain function activities. Journal of Oral Rehabilitation. 2013;40:119-29.
-
13van der Bilt A . Assessment of mastication with implications for oral rehabilitation: a review. Journalof Oral Rehabilitation. 2011;38:754-80.
-
14Maciel CTV, Barbosa MH, Toldo CA, Faza FCB, Chiappetta ALML. Disfunções Orofaciais nos Pacientes em Tratamento Ortodôntico. Rev CEFAC. 2006;8(4)456-66.
-
15Mezzomo CL, Machado PG, Pacheco AB, Gonçalves BFT, Hoffmann CF. As implicações da classe II de Angle e da desproporção esquelética tipo classe II no aspecto miofuncional. Rev CEFAC. 2011;13(4)728-34.
-
16Fernandes LFT, Kochenborger R, Woitchunas FE, Woitchunas DR. A influência da deglutição atípica no padrão craniofacial e na morfologia mandibular. RFO. 2010;15(1):52-7.
-
17Beighton P, Solomon L, Soskolne CL. Articular mobility in a African population. Ann Rheum Dis. 1973;(32):413-8.
-
18Pasinato F, Souza JA, Corrêa ECR, Silva AMT. Temporomandibular disorder and generalized joint hypermobility: application of diagnostic criteria. Braz. j. otorhinolaryngol, 2011;77(4):418-25.
-
19Dworkin SF, Leresche L. Research diagnostic criteria for temporomandibulardisoders: Review, criteria, examinations and specifications, critique. Journal of Craniomandibular Disorders. 1992;6:301-55.
-
20Genaro KF, Berretin-Felix G, Rehder MIBC, Marchesan IQ . Avaliação Miofuncional Orofacial - Protocolo MBGR. Rev CEFAC. 2009;11(2):237-55.
-
21Viera AJ, Garret JM. Understanding Interobserver Agreement: The Kappa Statistic. Research Series. 2005;37(5):360-3.
-
22Pacheco AB . Avaliação antroposcópica e cefalométrica do perfil e da tendência facial e sua relação com as funções estomatognáticas [Dissertação]. Santa Maria (RS): Universidade Federal de Santa Maria; 2013.
-
23Pehling J, Schiffman E, Look J, Shaefer J, Lenton P, Fricton J. Interexaminer Reliability and Clinical Validity of the Temporomandibular Index: A New Outcome Measure for Temporomandibular Disorders. J OrofacPain. 2002;16(4):296-304.
-
24Hirsch C, John MT, Stang A. Association between generalized joint hypermobility and signs and diagnoses of temporomandibular disorders. Eur J Oral Sci. 2008;116:525-30.
-
25Sáez-Yuguero MR, Linares-Tovar E, Calvo-Guirado JL, Bermejo-Fenoll A, Rodríguez-Lozano F. Joint hypermobility and disk displacement confirmed by magnetic resonance imaging: A study of women with temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral RadiolEndod. 2009;107(6):54-7.
-
26Teixeira MJ, Siqueira JTT. Dores Orofaciais: diagnóstico e tratamento. São Paulo: Artes Médicas, 2012.
-
27Chiodelli L, Weber P, Pasinato F, Souza JA, Corrêa ECR . Manifestações clínicas de desordem temporomandibular e inclinação lateral da cabeça. Ter Man. 2012;10(50):383-8.
-
28Figueiredo VMG, Cavalcanti AL, Farias ABL, Nascimento SR. Prevalência de sinais, sintomas e fatores associados em portadores de disfunção temporomandibular. Acta. Sci. Health. Sci. 2009;31(2):159-63.
-
29Pasinato F, Souza JA, Corrêa ECR, Silva AMT . Temporomandibular disorder and generalized joint hypermobility: electromyographic analysis of the masticatory muscles. Braz J Oral Sci. 2011;10(2):146-51.
-
30Gomes SGF, Custodio W, Faot F, Del BelCury AA, Garcia RCMR. Chewing side, bite force symmetry, and occlusal contact area of subjects with different facial vertical patterns. Braz Oral Res. 2011;25(5):446-52.
-
31Slavicek G, Schimmer C. Analysis of human mastigation behavior: a new approach using planar calculations of fragmented chewing sequences. J. Stomat. Occ. Med. 2010;3(1):61-7.
-
32Simpson MR. Benign Joint Hypermobility Syndrome: Evaluation, Diagnosis, and Management. J Am Osteopath Assoc. 2006;106(9):531-6.
-
33Weber P, Corrêa ECR, Bolzan GP, Ferreira FDS, Soares JC, Silva AMT . Mastigação e deglutição em mulheres jovens com desordem temporomandibular. CoDAS. 2013;25(4):375-80.
-
Research grant sponsor: Coordination for the Improvement of Higher Education Personnel (CAPES)
Publication Dates
-
Publication in this collection
May-Jun 2015
History
-
Received
07 July 2014 -
Accepted
22 Sept 2014