Abstracts
BACKGROUND: Anxiety disorders are often associated with several non-psychiatric medical conditions. Among the clinical conditions found in association with anxiety stands out the joint hypermobility (JH). OBJECTIVES: To carry out a systematic review of the clinical association between anxiety disorders and JH. METHOD: A survey was conducted in MEDLINE, PsychINFO, LILACS e SciELO databases up to December 2011. We searched for articles using the keywords 'anxiety', 'joint' and 'hypermobility' and Boolean operators. The review included articles describing empirical studies on the association between JH and anxiety. The reference lists of selected articles were systematically hand-searched for other publications relevant to the review. RESULTS: Seventeen articles were included in the analysis and classified to better extract data. We found heterogeneity between the studies relate to the methodology used. Most of the studies found an association between anxiety features and JH. Panic disorder/agoraphobia was the anxiety disorder associated with JH in several studies. Etiological explanation of the relationship between anxiety and JH is still controversial. CONCLUSION: Future research in large samples from the community and clinical setting and longitudinal studies of the association between anxiety and HA and the underlying biological mechanisms involved in this association are welcome.
anxiety; hypermobility; panic disorder; anxiety disorders; methodology; joint hypermobility syndrome
INTRODUÇÃO: Os transtornos de ansiedade estão frequentemente associados a vários quadros clínicos não psiquiátricos. Dentre os quadros clínicos associados à ansiedade destaca-se a hipermobilidade articular (HA). Objetivo: Realizar uma revisão sistemática da associação entre os transtornos de ansiedade e a HA. MÉTODO: Foi realizada uma pesquisa nos bancos de dados MEDLINE, PsychINFO, LILACS e SciELO em busca de artigos publicados até dezembro de 2011. Usamos as palavras-chave anxiety , joint e hypermobility e os operadores boolianos. A revisão incluiu artigos que descrevem estudos empíricos sobre a associação entre ansiedade e HA. As listas de referências dos artigos selecionados foram sistematicamente pesquisadas à mão em busca de publicações relevantes para a revisão. RESULTADOS: Dezessete artigos foram incluídos na análise e classificados para uma melhor extração dos dados. Encontramos heterogeneidade entre os estudos relacionada à metodologia utilizada. A maioria dos estudos encontrou associação entre as características de ansiedade e HA. Transtorno do pânico com agorafobia foi o transtorno de ansiedade associado à HA em vários estudos. A explicação etiológica da relação entre ansiedade e HA permanece controversa. CONCLUSÃO: Estudos futuros com amostras maiores de indivíduos da comunidade e de cenários clínicos e estudos longitudinais da associação entre ansiedade e HA e dos mecanismos biológicos subjacentes envolvidos nessa associação são bem-vindos.
ansiedade; hipermobilidade; transtorno do pânico; transtornos de ansiedade; metodologia; síndrome de hipermobilidade articular
ARTICLE
Anxiety and joint hypermobility association: a systematic review
Simone H. Bianchi SanchesI; Flávia de Lima OsórioII; Marc UdinaIII; Rocío Martín-SantosIV; José Alexandre S. CrippaII
INeurosciences and Behavior Department, Faculdade de Medicina de Ribeirão Preto (FMRP), Universidade de São Paulo (USP-RP), Brazil
IINeurosciences and Behavior Department, FMRP, USP-RP; National Science and Technology Institute (INCT, CNPq) for Translational Medicine, Brazil
IIIDepartment of Psychiatry, Institute of Neurosciences, Hospital Clínic, IDIBAPS, CIBERSAM, Barcelona; Department of Psychiatry and Clinical Psychobiology, University of Barcelona, Spain
IVDepartment of Psychiatry, Institute of Neurosciences, Hospital Clínic, IDIBAPS, CIBERSAM, Barcelona; Department of Psychiatry and Clinical Psychobiology, University of Barcelona, Spain; National Science and Technology Institute (INCT) for Translational Medicine, Brazil
Corresponding author Corresponding author: Simone Bianchi Sanches Av. dos Bandeirantes, 3900. Hospital das Clínicas, 3º andar. Monte Alegre 14048-900, Ribeirão Preto, SP, Brazil Phone: (+55 16) 36022703/36022201 E-mail: shbianchi@uol.com.br
ABSTRACT
BACKGROUND: Anxiety disorders are often associated with several non-psychiatric medical conditions. Among the clinical conditions found in association with anxiety stands out the joint hypermobility (JH).
OBJECTIVES: To carry out a systematic review of the clinical association between anxiety disorders and JH.
METHOD: A survey was conducted in MEDLINE, PsychINFO, LILACS e SciELO databases up to December 2011. We searched for articles using the keywords 'anxiety', 'joint' and 'hypermobility' and Boolean operators. The review included articles describing empirical studies on the association between JH and anxiety. The reference lists of selected articles were systematically hand-searched for other publications relevant to the review.
RESULTS: Seventeen articles were included in the analysis and classified to better extract data. We found heterogeneity between the studies relate to the methodology used. Most of the studies found an association between anxiety features and JH. Panic disorder/agoraphobia was the anxiety disorder associated with JH in several studies. Etiological explanation of the relationship between anxiety and JH is still controversial.
CONCLUSION: Future research in large samples from the community and clinical setting and longitudinal studies of the association between anxiety and HA and the underlying biological mechanisms involved in this association are welcome.
Descriptors: anxiety, hypermobility; panic disorder/agoraphobia; anxiety disorders; methodology; joint hypermobility syndrome.
Introduction
The emotional state of anxiety is universal and has an important adaptive function. It is generally described as a combination of somatic symptoms and subjective signs. States of anxiety are known to be present in non-clinical populations, suggesting a continuum between general and clinical populations. The clinical presentation usually consists of intense anxiety, not justified or proportional to external situations, imposing life restrictions and subjective distress. Thus, clinical cases present with interconnected physical, autonomic, and psychological alterations.1-3
Anxiety disorders are often associated with several nonpsychiatric medical conditions.1,4,5 This association may be the result of many factors, including the physiological consequences of underlying medical conditions, psychological reaction to the experience of being ill, secondary effect of treatment or an overlapping of two simultaneous adverse manifestations-anxiety and a medical condition.6 Among clinical anxiety disorders, panic and social anxiety have been described as the most prevalent. Both require attention due to the interference of symptoms in different areas of life, such as work performance, academic achievement, and daily tasks performance.7,8 The presence of significant comorbidities is another important feature of these disorders.2,3,9 Moreover, despite the significant prevalence of anxiety disorders, most people remain without appropriate diagnosis or treatment.
Among the clinical conditions found in association with anxiety, joint hypermobility (JH) is highlighted.10,11 This medical condition is usually hereditary, has an autonomic dominant pattern, and is present in approximately 10%-20% of the general population.12 A study of twins showed that genetics accounts for at least 70% of the phenotype variance rather than environmental factors (e.g., training)..12 Hypermobility is characterized by an extended range of motion in the joints, an increased distensibility of joints in passive movements, and hypermobility in active movement in the absence of a systemic rheumatologic disease.13 JH is more common in childhood and tends to decline with aging. The prevalent is higher among women (raising questions about the still poorly understood hormonal influences) and the Asian and African populations, with ethnic differences suggestive of genetic variations.6,14,15 JH may be accompanied by multiple organic anomalies, such as mitral valve prolapse (MVP). It is also associated with musculoskeletal dysfunctions, possibly resulting from glycoprotein deficiency and genetic alterations affecting the formation of collagen, which would explain tissue looseness and vulnerability to trauma in these patients.16,17 Musculoskeletal pain is the main complaint of patients with JH, as the flexibility of joints tends to demand greater muscle effort.18-21
The diagnosis of JH is usually established using the ninepoint Beighton scale.14 According to this scale, subjects with a score > 4 are considered as having JH.15,22,23 The condition is characterized through the examination of five body areas, each one receiving a score of hyperextension: little fingers, thumbs, elbows, knees, and trunk (Table 1). Aiming to allow the evaluation of hypermobility in body areas not covered in Beighton's scale, a similar methodology has been introduced and used by Bulbena et al.,24 which increased the body areas evaluated up to 10. In addition to this clinical evaluation, it is important to mention the existence of an easily-self-administered screening instrument for the assessment of hypermobility, called 'the five-part questionnaire for identifying hypermobility',25 which has been reported to have a high correlation with Beighton's score. This instrument also evaluates broad body areas and considers previous history of hypermobility.26 (Table 2).
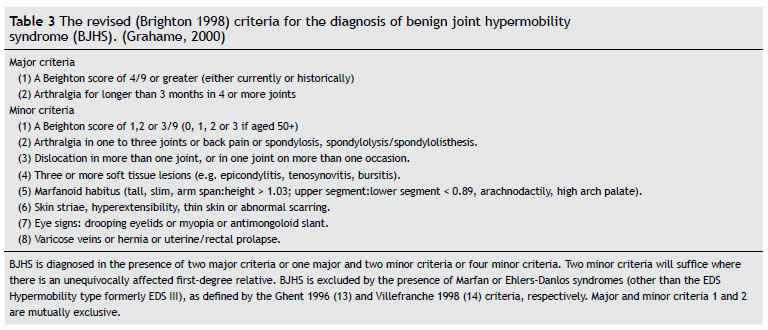
In fact, the clinical presentations of JH may range from simple manifestations that do not require treatment to severe cases in which joints are more easily displaced or other clinical conditions are associated, configurating a syndrome named Hypermobility Syndrome or (Benign) Joint Hypermobility Syndrome.27 However, for some authors, the term 'benign' would hinder the acknowledgement of the legitimacy of some of the complaints of the patient, especially in what concerns distress, painful symptoms, and difficulties in performing daily activities.28 Nowadays, for the diagnosis of joint hypermobility syndrome (JHS), Brighton's criteria are the most commonly used.29 According to these criteria, the syndrome diagnosis is made taking into account not only Beighton's score but also some clinical manifestations associated with hypermobility (Table 3). The minor criteria serve to highlight the common physical findings of the condition. The JHS cases have a combination of marfanoid habitus, increased skin stretch, and others manifestations, such as joint subluxation or dislocation, predisposing to premature osteoarthritis.18
The association of joint hypermobility and anxiety was described in 198810 in a case-control study of a sample of rheumatic outpatients with JH. Hypermobile patients showed a high prevalence of anxiety disorders (~70%), compared to 22% of rheumatic controls, with panic/agoraphobia and simple phobia disorders significantly associated.10 A second study of a sample of psychiatric outpatients with panic/agoraphobia disorder showed that JH was presented in about 70% of them compared to 10% of patients with others psychiatric disorders, or 12% of medical patients without psychiatric disorders.11 Cases with panic/agoraphobia disorders were 17 times more likely to suffer from hypermobility. Subsequently, these results were replicated in a two-phase cross-sectional epidemiologycal study in a sample of 1,300 inhabitants.17,30 It was observed that hypermobile subjects were eight times more likely to suffer from panic disorder and social phobia and six times more likely to suffer from agoraphobia than non hypermobile subjects. No other anxiety or mood disorders were found associated with JH.
These two conditions (anxiety and joint hypermobility) share several common features, such as early age of onset, decreased frequency with age, high prevalence in women, and familial aggregation. The two disorders have genetics factors that are still no well understood. Preliminary studies suggested a cytogenetic mutation in chromosome 15 in pedigrees with both disorders.31 However, these initial results were not yet been replicated.32,33 Furthermore, both share an autonomic alteration, with higher anxiety sensitivity, abnormal pain perception, and higher somatic sensitivity than controls; similar to fibromyalgia, another condition with a high proportion of JH. Hakim et al.34 proposed that the interaction between autonomic, physical, and psychological disturbances are linked in a complex manor in JHS, in the sense that each factor may stimulate each other.
In recent years there is a renewed interest in studying this clinical association from a clinical, epidemiological, and biological point of view.35 The aim of this study was to carry out a systematic review of the clinical association between anxiety disorders and JH, discussing the methodological aspects and main findings.
Method
A systematic search for articles was performed in the electronic databases PubMed, LILACS, PsycInfo, e SciELO using the keywords 'anxiety', 'joint', and 'hypermobility' and Boolean operators. Articles in English, Spanish or Portuguese describing empirical studies designed to investigate the association between JH and anxiety were sought for the review. No time limits were set, and articles published up to December 2011 were included. Exclusion criteria were letters to editors, editorials, review articles, and articles reporting findings on the association between JH and conditions other than anxiety. The reference lists of selected articles were systematically hand-searched for other publications relevant to the review.
Selected articles were first classified according to characteristics of the population studied, study design, and psychopathologic evaluation (anxiety disorder or anxiety symptoms). Furthermore, sociodemographic characteristics, diagnostic criteria for anxiety disorders, presence of a structured interview for psychiatric diagnosis, anxiety rating scales, JH and JHS criteria, data on the prevalence and outcomes of studies on the association were extracted for a properly review.
Results
Flow selection of articles
Thirty-four references were found via PubMed. The search in the other databases yielded no matches. Twelve articles were selected after application of the inclusion and exclusion criteria and another six were included by handsearch.17,36-39 Therefore, a total of 17 articles were included in the review.
Characteristics of selected articles and data extraction
Table 4 presents the main characteristics of the 17 articles describing empirical studies on the association between JH and anxiety.
The articles selected for the review were predominantly from Europe, especially Spain, with one article from Zaragoza40 and eight from Barcelona.10,11,17,24,41-44 The remaining articles came from different parts of the world, including a single North American publication,45 one from Chile39 and others from European and Asian countries: Italy,46 France,38,47 Turkey,37,48 and Israel.36
Selected studies were published between 1993 and 2011. We found eleven case-control studies, five cross< sectional and one cohort study design. All selected articles included a total of 3205 patients and 664 controls. Respecting the sample characteristics, we found articles focused on medical or rheumatic patients (n = 4), anxiety patients (n = 5) or general population, including workers and high school and college students (n = 8). Generally, the studies presented samples of both genders, aged between 18 and 65 years.
Assessment of anxiety, hypermobility, and joint hypermobility syndrome
We selected a group of articles reporting the diagnosis of anxiety disorder according to DSM and a second group of articles reporting symptoms or traits of anxiety without a categorical psychiatric diagnosis (Table 4). Most of the studies that evaluate anxiety disorder used a structured interview for the clinical diagnosis of DSM anxiety disorder (especially the SCID) and hetero-administered scales, such as the Hamilton Anxiety Scale (HAM-A). Studies that just evaluated anxiety symptoms or traits used different self- and hetero-applied assessment instruments for the screening of symptoms, including the Symptom Checklist -90-Revised (SCL-90-R), the State-trait Anxiety Inventory(STAI), and the Fear Survey Schedule (FSS).
Three methods were described for the assessment of hypermobility: Beighton's score,14 the Hospital del Mar criteria,24 and the self-administrated join hypermobility questionnaire.25 Beighton's score was certainly the most used measure.
Although hypermobility is frequently characterized by complaints of chronic pain, only two articles45,46 used specific or indirect instruments to assess this variable, such as the West Haven-Yale Multidimensional Pain Inventory (WHYMPI) and the Function Symptom Frequency (FSF).
Another aspect worth noting is the fact that most articles (n = 14; 82%) used the word 'syndrome' to refer to the clinical picture of JH. Nevertheless, just two more recent studies43,47 clearly mentioned the use of Brighton's criteria for the characterization of the musculoskeletal symptoms that constitute the syndrome. Baeza-Velasco et al.47 suggest some adaptations in the medical terminology to facilitate the self-reporting of the symptoms. This seems to have some similarity to Beighton's proposal to use a screening questionnaire consisting of four simple questions to detect complaints of arthralgia, in his seminal article on JH.14
Association between anxiety and hypermobility
Several studies found an association between anxiety symptoms or traits and JH.38-40,43-45 Regarding DSM anxiety disorders diagnoses, several studies reported an association between JH and panic/agoraphobia disorder10,11,17,41,43 and two studies did not found an association.36,37 Generalized anxiety disorder was not associated with JH.10,11,17,43 Social phobia and simple phobia were related with JH but generally with a weaker association than panic disorder10,17,43 (Table 4).
Discussion
This review includes studies evaluating the association between anxiety and hypermobility. Differences in methodology used in most of the studies made it difficult to compare and compile results. In respect to our first outcome, the relationship between anxiety symptoms or traits and JH, most studies found a correlation between anxiety symptomatology and presence of join hypermobility. In respect to our second outcome, the association between anxiety disorders and JH, the stronger evidence is first for panic/agoraphobia disorder and then for social anxiety disorder and simple phobia. No other anxiety disorder or mood disorder were found in association with JH.
This systematic review has some limitations and strengths. The clinical samples of case-control studies showed that the studies of hypermobile patients were carried out in very different settings and three of them with a small sample size. On the other hand, studies of anxiety patients showed more homogeneity and properly sample size to find the association. All of them use DSM criteria and three of four used a semistructured clinical interview. Raters were trained and blinded to the evaluation of hypermobility. However, one study focused on the role of MVP in the association, which limits the interpretation of the association. The cross-sectional surveys were done in different population with different range of age and gender, which may bias the joint hypermobility prevalence. Moreover, some of them used different cut-off point of Beighton's scale or another JH tools. Lastly, there is an unusual "internet" survey based on "tall people" and the presence of JH and social phobia in a small sample to be representative. Only one cohort study was found. Interestingly, although in a small sample size, the joint hypermobility group was associated with higher risk of developing anxiety disorders. Few studies used the Brighton`s criteria to assess the complete joint hypermobility syndrome.
It should be noted that several studies evaluating anxiety symptoms or traits had reported an association between anxiety and hypermobility, supporting that might be an association between some specific feature of anxiety and JH, even in non-clinical populations. Some studies reported that patients with hypermobility had more indicators of fear trait,42,44 which might have implications for symptoms of panic and agoraphobia and social anxiety; conditions associated with JH. Strong indicators of distress45,46 and somatization were also found, with significant emotional symptoms resembling those of hospitalized patients regarding physical symptoms and bodily concern.46
The prevalence of hypermobility in anxiety patients varies widely between 13%36 and 67.7%.11 These differences between prevalence rates seem to reflect methodological issues. The results of the studies that investigated the prevalence of anxiety among people with hypermobility, however, were quite similar for both clinical samples and the general population. For instance, 69.3% of rheumatic patients with hypermobility had some type of anxiety disorder,10 which is very close to the 62.6% found in the general population.17
Another relevant remark is that the several studies that confirmed the association between anxiety and hypermobility were conducted in Spain, while some studies with divergent results were performed in different contexts and cultures, one in Turkey37 and one in Israel.36 Therefore, some different findings should be considered taking into account the ethnic and social differences and contextual variations in the prevalence of these clinical manifestations. These findings underscore the importance of psychometric studies with these instruments, including analyses of ROC curves and the establishment of the best cut-off points, considering mainly age, gender, and ethnic differences.23 To our knowledge, no such results are available in the literature to date. Nevertheless, the most recent studies had included other measures of hypermobility, such as the self-administrated questionnaire44 or the consideration of the syndrome according to Brighton's criteria,21,43 suggesting a trend of increased attention to the complexity of the criteria used for identifying hypermobility.
As previously mentioned, one article studied the effect of MVP in the association of panic disorder and JH.37 The authors suggested that MVP affects the prevalence of JH in patients with panic disorder. Two more selected studies described investigations on the hypothesis that implicates MVP in the association between anxiety and hypermobility.10,11 From a methodological perspective, mention should be made to the scientific rigor regarding the assessment by blind investigators of psychiatric and rheumatologic diagnoses, as well as to the use of two diagnostic techniques (M-mode and two-dimensional echocardiography), which increase the reliability of assessments. However, these articles did not confirm the association. Thus, there seems to be a tendency toward confirming the connection between hypermobility and MVP, although the latter does not seem to have a significant impact on the association with anxiety.49,50 It should be noted that symptoms previously associated with MVP have currently been considered as suggestive of autonomic alterations in patients with hypermobility.34,50
Another two articles were focused on the hypothesis of the association between somatic (body) characteristics and anxiety disorders. These studies tested patients with thoracic deformity48 and the asthenic somatotype.24 Bulbena et al.24 reported that an asthenic somatotype was associated with panic disorder. Gülsun et al.48 showed that patients with torax deformity presented more prevalence of anxiety disorders than controls. Patients who presented both torax deformity and JH have high score of HAD-A scale than cases without JH. However, it is interesting to note that in their classical epidemiologic study with an African population, Beighton et al.14 reported that the assessment of body constitution in 101 patients indicated no correlation between JH and somatotype.
Additional factors commonly found in the literature on hypermobility have as yet received little attention in what concerns their association with anxiety, such as chronic pain22,23,29,52 and non-musculoskeletal symptoms, like autonomic alterations28,53 and inadequate proprioception.22,53
Conclusions
In general, the articles examined in this review tend to support the association between anxiety and JH. Future research should considerer the study of representative, large, and prospective samples in different settings; the study of the full joint hypermobility syndrome, different anxiety disorders apart from panic and phobia disorders (generalized anxiety, obsessive compulsive disorder, postraumatic disorder) and anxiety traits (more anxiety or fears, higher hypermobility); as well as other psychiatric disorders highly associated with panic, such as bipolar disorders or schizophrenia or the association with other connective tissue disorders. The study of the association is a challenging topic to perform experimental research of the link between JHS and dysautonomia, pain perception, genetic factors, or neuroimaging endophenotypes.
From a clinical standpoint, it seems interesting to consider the association of anxiety in rheumatic patients. JHS may be a risk factor for future anxiety disorders and chronic medical complications (ostheoartrosis, pain, loss of functionality). Clinicians working on the field agree with the need of a multidisciplinary approach for treatment and prevention.
- 1. Chagas MH, Nardi AE, Manfro GG, Hetem LA, Andrada NC, Levitan MN, Salum GA, Isolan L, Ferrari MC, Crippa JA; Associação Médica Brasileira. Guidelines of the Brazilian Medical Association for the diagnosis and differential diagnosis of social anxiety disorder. Rev Bras Psiquiatr. 2010;32(4):444-52.
- 2. Merikangas KR, Risch NJ, Weissman MM. Comorbidity and cotransmission of alcoholism, anxiety and depression. Psychol Med. 1994;24(1):69-80.
- 3. Magee WJ, Eaton WW, Wittchen HU, Mcgonagle KA, Kessler R.C. Agoraphobia, simple phobia, and social phobia in the National Comorbidity Survey. Arch Gen Psychiatry. 1996;53:159-68.
- 4. Sareen JS, Cox BJ, Clara I, Asmundson GJG. The relationship between anxiety disorders and physical disorders in the US National Comorbidity Survey. Depress Anxiety. 2005;21:193-202.
- 5. Martín-Santos R, Crippa JAS. Trastornos de ansiedad en atención primaria. In: Pérez Solá V. Abordaje de los problemas de salud mental en el ámbito extrahospitalario. Barcelona: Colegio Oficial de Médicos de Barcelona, Barcelona, 2003; pp. 17-31.
- 6. Martín-Santos R, Hakim A, Santos Filho A, Grahame R, Louzada P, Crippa JAS. Síndrome de hipermovilidad articular benigno. Relación com la ansiedad. In: José Luis Vázquez-Barquero; Andrés Herrán Gómez. (Org.). Las Fases Iniciales de las Enfermedades Mentales: Transtornos de Ansiedad. Barcelona: Elsevier, 2006, pp. 63-72.
- 7. Bystritsky A, Kerwin L, Niv N, Natoli JL, Abrahami N, Klap R, Wells K, Young AS. Clinical and subthreshold panic disorder. Depress Anxiety. 2010;27(4):381-9.
- 8. Baptista CA, Loureiro SR, de Lima Osório F, Zuardi AW, Magalhães PV, Kapczinski F, Filho AS, Freitas-Ferrari MC, Crippa JA. Social phobia in Brazilian university students: Prevalence, under-recognition and academic impairment in women. J Affect Disord. 2011 Oct 19. [Epub ahead of print]
- 9. Sardinha A, Nardi AE, Zin WA. Are panic attacks really harmless? The cardiovascular impact of panic disorder. Rev Bras Psiquiatr. 2009;31(1):57-62.
- 10. Bulbena A, Duró JC, Porta M, Martín-Santos R, Mateo A, Molina L, Vallescar R, Vallejo J. Anxiety disorders in the joint hypermobility syndrome. Psychiatry Res. 1993;46(1):59-68.
- 11. Martín-Santos R, Bulbena A, Porta M, Gago J, Molina L, Duró JC. Association between joint hypermobility syndrome and panic disorder. Am J Psychiatry. 1998;155(11):1578-83.
- 12. Hakim AJ, Cherkas LF, Grahame R, Spector TD, MacGregor AJ. The genetic epidemiology of joint hypermobility: a population study of female twins. Arthritis Rheum. 2004;50(8):2640-4.
- 13. Beighton P, Grahame R, Bird H. Hypermobility of Joints, 3rd ed. London: Springer-Verlag, 1999.
- 14. Beighton P, Solomon L, Soskolne L. Articular Mobility in as African Population. Ann Rheu Dis. 1973;32:413-418.
- 15. Lewkonia RM. Hypermobility of Joints. Arch Dis Childh. 1987;62:1-2.
- 16. Cavenaghi S, Marino LHC, Oliveira PP, Lamari NM. Hipermobilidade Articular em Pacientes com Prolapso da Valva Mitral. Arq Bras Cardiol. 2009;93(3):307-11.
- 17. Bulbena A, Gago J, Martín-Santos R, Porta M, Dasquens J, Berrios GE. Anxiety disorder and joint laxity: a definitive link. Neurol Psychiatry Brain Res. 2004b;11:137-40.
- 18. Grahame, R. Pain, distress and joint hyperlaxity. Joint Bone Spine. 2000b;67:157-63.
- 19. Roberto AM, Terreri MTRA, Szejnfeld HMOE. Densidade mineral óssea em crianças. Associação com dor músculoesquelética e/ou hipermobilidade articular J Pediatr. 2002;78(6):523-8.
- 20. Simpson MR. Benign Joint Hypermobility Syndrome: Evaluation, Diagnoses and Management. J Am Osteopath Assoc. 2006;106:531-6.
- 21. Baeza-Velasco C, Gély-Nargeot MC, Bulbena A, Bravo JF. Joint hypermobility syndrome: problems that require psychological intervention. Rheumatol Int. 2011;31(9):1131-6.
- 22. Sympson, MR Benign Joint Hypermobility Syndrome: Evaluation, Diagnosis and Management JAOA. 2006;106(9):531-6
- 23. Remvig, L, Jensen, DV, Ward, R. Epidemiology of General Joint Hypermobility and Basis for the Proposal Criteria for Benign Joint Hypermobility Syndrome: Review of the literature. J Rheumathol. 2007;34(4):804-9
- 24. Bulbena A, Martín-Santos R, Porta M, Duró JC, Gago J, Sangorrín J, Gratacós M. Somatotype in panic patients. Anxiety. 1996;2(2):80-5.
- 25. Hakim AJ, Grahame R. A Simple Questionnaire to Detect Hypermobility: an adjunct to the assessment of patients with diffuse musculoskeletal pain. Inter Journal Clin Pract. 2003;57(3):163-6.
- 26. Moraes DA, Baptista CA, Crippa JA, Louzada-Junior P.Translation into Brazilian Portuguese and validation of the five-part questionnaire for identifying hypermobility. Rev Bras Reumatol. 2011;51(1):61-9.
- 27. Kirk JA, Ansell BM, Bywaters GL. The hypermobility Syndrome - Musculoskeletal Complaints Associated with Generalized Joint Hypermobility. Ann Rheum Dis. 1967;26:419-25.
- 28. Bravo, JF, Sanhueza, G, Hakim, AJ. Cardiovascular autonomic dysfunction and chronic fatigue in fibromyalgia and joint hypermobility syndrome. In: Hakim AJ, Keer R, Grahame R eds. Hypermobility, fibromyalgia and chronic pain. London: Churchill Livingstone. Elsevier; 2010, pp. 69-82.
- 29. Grahame R., Bird HA, Child A. The revised (Brighton 1998) criteria for the diagnosis of benign joint hypermobility syndrome (BJHS). J Rheumatol. 2000;27(7):1777-9.
- 30. Gago J. Estudio de prevalencias y asociación de hiperlaxitud articualr y trastornos ansiosos fóbicos en población rural. Barcelona: Universitat Autònoma de Barcelona, 1992.
- 31. Gratacòs M, Nadal M, Martín-Santos R, Pujana MA, Gago J, Peral B, Armengol L, Ponsa I, Miró R, Bulbena A, Estivill X. A polymorphic genomic duplication on human chromosome 15 is a susceptibility factor for panic and phobic disorders. Cell. 2001;106(3):367-79.
- 32. Tabiner M, Youings S, Dennis N, Baldwin D, Buis C, Mayers A, Jacobs PA, Crolla JA. Failure to find DUP25 in patients with anxiety disorders, in control individuals, or in previously reported positive control cell lines. Am J Hum Genet. 2003;72:535-8.
- 33. Weiland Y, Kraus J, Speicher MR. A multiclot FISH assay does not detect DUP25 in control individuals or in reported positive control cells. Am J Hum Genet. 2003;72:1349-52.
- 34. Hakim AJ, Grahame R. Non-musculoskeletal symptoms in joint hypermobility syndrome. Indirect evidence for autonomic dysfunction Rheumatology. 2004;43:1194-5.
- 35. Martín-Santos R, Bulbena A, Crippa JAS. Anxiety disorders, their relationship to hypermobility and their management. In: Hakim, Keer, Grahame eds. Hypermobility, fibromyalgia, and chronic pain. London: Churchill Livingstone. Elsevier; 2010, pp. 53-60.
- 36. Benjamin J, Zen-Bion IZ, Dannon P, Scheirber S, Meiri G, Ofek A, Palatnik A. Lack of association between joint hyperlaxity and, I: panic disorder, and II: reactivity to carbon dioxide in health volunteers. Hum Psychopharmacol Clin Esp. 2011;16(2):189-92.
- 37. Gulpek D, Bayraktar E, Akbay SP, et al. Joint hypermobility syndrome and mitral valve prolapse in panic disorder. Prog Neuropsychopharmacol Biol Psychiatry. 2004;28:969-73.
- 38. Baeza-Velasco C, Bulbena A. Ansiedad social y alteración de colágeno en personas de gran estatura. C Med Psicosom. 2009;89/90:40-46.
- 39. Baeza-Velasco C, Bulbena A, Bravo J. Sintomatología ansiosa y sindrome de hyperlaxitud articular en un grupo de universitarios chilenos. Ansiedad y Estrés. 2010;16(1):1-12.
- 40. Garcia-Campayo J, Asso E, Alda M, Andres EM, Sobradiel N. Association between joint hypermobility syndrome and panic disorder: a case-control study. Psychosomatics. 2010;51(1):55-61.
- 41. Bulbena A, Agulló A, Pailhez G, Martín-Santos R, Porta M, Guitart J, Gago J. Is joint hypermobility related to anxiety in a nonclinical population also? Psychosomatics. 2004a;45(5):432-7.
- 42. Bulbena A, Gago J, Sperry L, Bergé D. The relationship between frequency and intensity of fears and a collagen condition. Depress Anxiety. 2006,23(7):412-7.
- 43. Bulbena A, Gago J, Pailhez G, Sperry L, Fullana MA, Villaroya O. Joint Hypermobility Symdrome is a risk fator trait for anxiety disorders: a 15-year follow-up cohort study. Gen Hosp Psychiatry. 2011;33(4):363-70.
- 44. Pailhez, G, Rosado, S, Cabré, AB, Bulbena, A. Joint Hypermobility, Fears and Chocolate Consumption. J Nerv Ment Dis. 2011;199(11):903-6.
- 45. Lumley MA, Jordan M, Rubenstein R, Tsipouras P, Evans M. Psychosocial Functioning in the Ehlers-Danlos Syndrome. Am J Med Genet. 1994;53:149-152.
- 46. Ercolani M, Galvani M, Franchini C, Baracchini F, Chattat R. Benign joint hypermobility syndrome: psychological features and psychopathological symptoms in a sample pain-free at evaluation. Percept Mot Skills. 2008;107(1):246-56.
- 47. Baeza-Velasco C, Gély-Nargeot MC, Bulbena A, Fenetrier C, Bravo JF. Association between psychopathological factors and joint hypermobility syndrome in a group of undergraduates from a French University. Int J Psychiatry Med. 2011;41(2):187-201.
- 48. Gülsun M, Yilmaz, MB, Pinar M, Tonbul, M, Clik, C, Ozdemir, B, Dumlu, K, Erbas, M. Thorax deformity, joint hypermobility and anxiety disorders. Saudi Med J. 2007;28(12):1840-4.
- 49. Filho AS, Maciel BC, Martín-Santos R, Romano MM, Crippa JA. Does the association between mitral valve prolapse and panic disorder really exist? Prim Care Companion J Clin Psychiatry. 2008;10(1):38-47.
- 50. Filho AS, Maciel BC, Romano MM, Lascala TF, Trzesniak C, Freitas-Ferrari MC, Nardi AE, Martín-Santos R, Zuardi AW, Crippa JA. Mitral Valve Prolapse and Anxiety Disorder. Br J Psychiatry. 2011;199(3):247-8.
- 51. Bravo J. Significado y importancia de estudiar a las personas con hiperlaxitud articular. Rev Chilena de Reumatología. 2008;24(1):4-5.
- 52. Grahame R. Time to take the hypermobility seriously (in adults and children). Rheumatology. 2001;40:485-91.
- 53. Ferrel, WR, Ferrel, PW. Prorioceptive dysfunction in JHS and its management. In: Hakim. AJ, Keer, R, Grahame, R Hypermobility, fibromyalgia and chronic pain London: Churchill Livingstone. Elsevier, 2010; pp. 96-104.
Corresponding author:
Publication Dates
-
Publication in this collection
19 June 2012 -
Date of issue
June 2012