Abstract
Objective:
To provide a comprehensive picture of mental health problems (MHPs) in Brazilian medical students by documenting their prevalence and association with co-factors.
Methods:
We systematically searched the MEDLINE/PubMed, SciELO, LILACS, and PsycINFO databases for cross-sectional studies on the prevalence of MHPs among medical students in Brazil published before September 29, 2016. We pooled prevalences using a random-effects meta-analysis, and summarized factors associated with MHP.
Results:
We included 59 studies in the analysis. For meta-analyses, we identified the summary prevalence of different MHPs, including depression (25 studies, prevalence 30.6%), common mental disorders (13 studies, prevalence 31.5%), burnout (three studies, prevalence 13.1%), problematic alcohol use (three studies, prevalence 32.9%), stress (six studies, prevalence 49.9%), low sleep quality (four studies, prevalence 51.5%), excessive daytime sleepiness (four studies, prevalence 46.1%), and anxiety (six studies, prevalence 32.9%). Signs of lack of motivation, emotional support, and academic overload correlated with MHPs.
Conclusion:
Several MHPs are highly prevalent among future physicians in Brazil. Evidence-based interventions and psychosocial support are needed to promote mental health among Brazilian medical students.
Mental health; depression; medical students; mental disorders
Introduction
Mental health problems (MHPs) and mental distress can significantly impair quality of life11. Lins L, Carvalho FM, Menezes MS, Porto-Silva L, Damasceno H. Health-related quality of life of students from a private medical school in Brazil. Int J Med Educ. 2015;6:149-54. and empathy.22. Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86:996-1009. Furthermore, higher mental well-being is positively associated with empathy33. Shanafelt TD, West C, Zhao X, Novotny P, Kolars J, Habermann T, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20:559-64. and negatively associated with suicidal ideation, unprofessional behaviors, and burnout.44. Dyrbye LN, Harper W, Moutier C, Durning SJ, Power DV, Massie FS, et al. A multi-institutional study exploring the impact of positive mental health on medical students’ professionalism in an era of high burnout. Acad Med. 2012;87:1024-31. From this perspective, MHPs may have a serious impact on a student’s life, affecting capacity to organize highly demanding study hours, socialize, and perform academically. Among students of the health professions, this could affect patient care, since empathy and professionalism might be impaired.
The literature reports that medical students display poorer psychosocial wellbeing when compared to peers of the same age55. Pagnin D, de Queiroz V. Comparison of quality of life between medical students and young general populations. Educ Health (Abingdon). 2015;28:209-12. and exhibit higher prevalence of depression and burnout than the general population,66. Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443-51. presumably due to the intense workload expected. In particular, a number of potentially stressful factors have been reported among Brazilian medical undergraduates. These include a highly stressful environment, competitiveness, excessive workload, sleep deprivation, peer pressure, and many other personal, curricular, institutional, and affective factors.11. Lins L, Carvalho FM, Menezes MS, Porto-Silva L, Damasceno H. Health-related quality of life of students from a private medical school in Brazil. Int J Med Educ. 2015;6:149-54.,77. Tempski P, Bellodi PL, Paro HB, Enns SC, Martins MA, Schraiber LB. What do medical students think about their quality of life? A qualitative study. BMC Med Educ. 2012;12:106.,88. Figueiredo AMd, Ribeiro GM, Reggiani ALM, Pinheiro BdA, Leopoldo GO, Duarte JAH, et al. Percepções dos estudantes de medicina da ufop sobre sua qualidade de vida. Rev Bras Educ Med. 2014;38:435-43. Additionally, undergraduate medical education in Brazil is facing new challenges, such as conciliating a Unified Health System (SUS)-centered national curriculum guideline with the psychosocial needs of students88. Figueiredo AMd, Ribeiro GM, Reggiani ALM, Pinheiro BdA, Leopoldo GO, Duarte JAH, et al. Percepções dos estudantes de medicina da ufop sobre sua qualidade de vida. Rev Bras Educ Med. 2014;38:435-43. within the framework of a 6-year curriculum divided into three cycles: a basic (preclinical) cycle, a clinical-theoretical cycle, and the more practical “internship” cycle.
Research into factors associated with MHPs is important for the development of interventions, especially at this paradigm-changing stage of curriculum planning. Factors known to be associated with MHPs in medical students include female gender,99. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73.,1010. Meyer C, Guimarães ACdA, Machado Z, Parcias SR. Qualidade de vida e estresse ocupacional em estudantes de medicina. Rev Bras Educ Med. 2012;36:489-98. maladaptive personalities,99. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73. financial difficulties,1010. Meyer C, Guimarães ACdA, Machado Z, Parcias SR. Qualidade de vida e estresse ocupacional em estudantes de medicina. Rev Bras Educ Med. 2012;36:489-98. pre-existing mental health problems,1111. Yates J, James D, Aston I. Pre-existing mental health problems in medical students: a retrospective survey. Med Teach. 2008;30:319-21. and exposure to an older, fragmented, and more theoretical curricular structure.1212. Zuardi AW, Prota Fdel G, Del-Ben CM. Reduction of the anxiety of medical students after curricular reform. Rev Bras Psiquiatr. 2008;30:136-8.
In a study of 62,728 medical students, the overall prevalence of depression was reported to be 28.0%.1313. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-68. Existing systematic reviews and meta-analyses on this issue have been generated for medical students from Asia,1414. Cuttilan AN, Sayampanathan AA, Ho RC. Mental health issues amongst medical students in Asia: a systematic review [2000-2015]. Ann Transl Med. 2016;4:72.,1515. Lei XY, Xiao LM, Liu YN, Li YM. Prevalence of depression among chinese university students: a meta-analysis. PLoS One. 2016;11:e0153454. North America,99. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73. English-speaking countries outside North America,1616. Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ. 2014;48:963-79. and more globally.1313. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-68.,1717. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214-36. To our knowledge, only one review1818. Baldassin S. Ansiedade e depressão no estudante de medicina: revisão de estudos brasileiros. Cadernos ABEM. 2010;6:19-26. relates to Brazilian medical students, but was limited to a range of depressive and anxiety disorders and did not include statistical analysis or provide a detailed description of methodology to enable future replication.
This study aims to provide a comprehensive insight into Brazilian medical student mental health, by addressing the following questions relating to medical students in Brazil: 1) what is the prevalence of MHPs and 2) which co-factors are associated with MHPs. We hypothesized that the most investigated MHPs would be depression, anxiety, and burnout; that clinically significant depression would affect a significant proportion of medical students; and that female students would be generally more affected by mental health issues, given this trend in the general public.
Methods
We registered the protocol of this review in the International Prospective Register of Systematic Reviews (PROSPERO; record no. CRD42016048236).1919. Pacheco JPG, Ribeiro TB, Francischetto EC, Arab C, Lourenço CB, Bezerra IMP, et al. Prevalence of depression and other mental health problems amongst medical students in Brazil: systematic review and meta-analysis [Internet]. Heslington: University of York. 2016 [cited 2017 Apr 15]. http://crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016048236
http://crd.york.ac.uk/PROSPERO/display_r...
Searches
On September 29, 2016, one reviewer (JPP) searched MEDLINE (via PubMed) from 1966 to 2016, SciELO from 1909 to 2016, LILACS from 1980 to 2016, and PsycINFO from 1927 to 2016. The review team developed a common search strategy, including terms related to Brazil, medical students, mental health, mental disorder, and other related terms. The complete search strategy is available from the registered protocol.1919. Pacheco JPG, Ribeiro TB, Francischetto EC, Arab C, Lourenço CB, Bezerra IMP, et al. Prevalence of depression and other mental health problems amongst medical students in Brazil: systematic review and meta-analysis [Internet]. Heslington: University of York. 2016 [cited 2017 Apr 15]. http://crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016048236
http://crd.york.ac.uk/PROSPERO/display_r...
We did not apply limitations to the search. In addition, we manually screened the references of the included papers for potential inclusion in the review.
Inclusion criteria
We only included cross-sectional studies that evaluated the prevalence of MHPs amongst medical students in Brazil. We included studies if: 1) they were cross-sectional; 2) they assessed medical students enrolled in Brazilian medical schools; 3) they reported prevalence of one or more MHPs. For this review, we defined an MHP as any diagnosable mental disorder or symptom of mental disorder (e.g., depression, burnout, suicidal ideation).
Exclusion criteria
We excluded studies if: 1) they included medical student participants with non-medical students in the same group, but provided no subgroup analysis; 2) MHPs were not the main focus of the questionnaire/diagnostic instrument (e.g., the focus was quality of life); 3) they used instruments not validated for the Portuguese language and for Brazilian populations (linguistic and cultural validation was required); or 4) the full study was not available.
Outcomes
The primary outcomes for this review were the prevalence of depression and common mental disorders (CMD). The secondary outcomes were the prevalence of other MHPs and factors associated with MHPs.
Study selection and data extraction
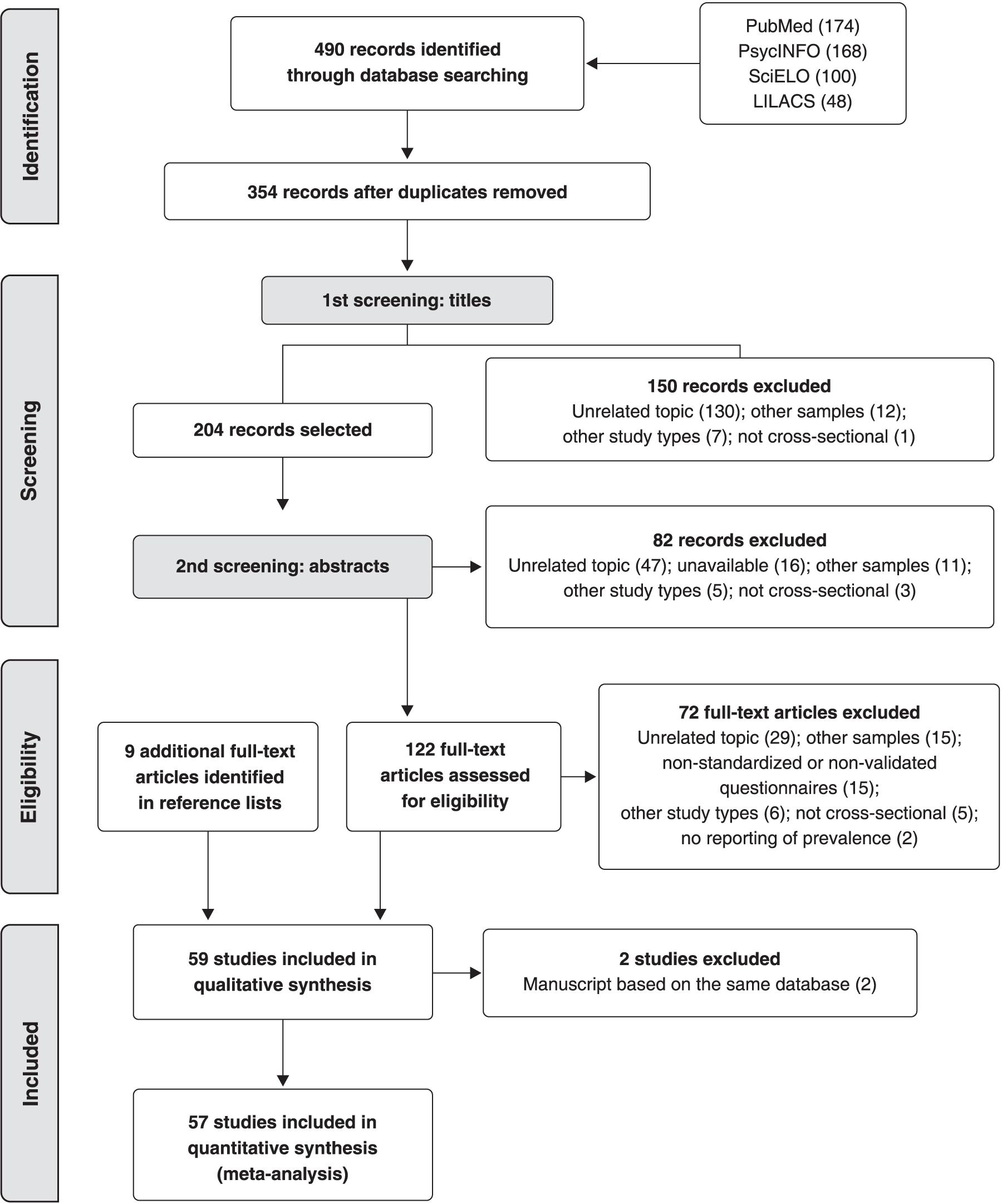
Two review team members (JPP and HTG) independently screened titles and abstracts, assessed studies for eligibility, and performed data extraction. Any discrepancies in study selection were resolved through discussion with a third reviewer (GCP). We used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses2020. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-9, W64. (PRISMA) flow chart to illustrate the study selection process (Figure 1).
The data extracted from each study included: study characteristics (e.g., location, sample size), participant characteristics (e.g., mean age, gender), and results for the prevalence of MHPs and factors associated with MHPs. Detailed information on data extraction is provided in the protocol.1919. Pacheco JPG, Ribeiro TB, Francischetto EC, Arab C, Lourenço CB, Bezerra IMP, et al. Prevalence of depression and other mental health problems amongst medical students in Brazil: systematic review and meta-analysis [Internet]. Heslington: University of York. 2016 [cited 2017 Apr 15]. http://crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016048236
http://crd.york.ac.uk/PROSPERO/display_r...
We requested missing data (such as exact number of participants, mean age, and gender) from study authors as necessary.
Risk of bias assessment
Two authors (JPP and HTG) assessed reporting of ethical approval and appraised the studies using the risk-of-bias tool developed by Hoy et al.2121. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934-9. We used this tool because it addresses external and internal validity and has high inter-rater agreement.2121. Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934-9. We omitted the last item of the tool (“Summary item on the overall risk of study bias”) because of its subjectivity. We resolved disagreements by discussion. We used ratings to generate a quality index for the quality-effects2222. Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45:123-9. (QE) meta-analysis.
Data synthesis and statistical analysis
We used the Meta-analysis of Observational Studies in Epidemiology (MOOSE) statement2323. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008-12. to guide the reporting of this review.
When studies provided appropriate data, we pooled the results using a random-effects (RE) model, thus reporting the aggregate prevalence, corresponding p-value, and 95% confidence interval (95%CI). We used double arcsine transformation and normalized prevalence data after pooling and back-transformation.2424. Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974-8. We presented the results in forest plots. We also performed a sensitivity analysis to examine whether use of a QE model2222. Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45:123-9. produced a substantial difference in the results. We investigated the QE model because it accounts for study quality and leads to a distinctly conservative confidence interval when heterogeneity exists.2222. Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45:123-9. When two or more studies reporting the same mental health problem were based on the same database, we selected only one for the quantitative synthesis, favoring the study that was first published. We selected this criterion because additional studies have focused on particular subgroups, which could augment their contribution to the meta-analysis results.
We assessed heterogeneity using the I2 statistic. We considered an I2 value of 75 to 100% to represent high heterogeneity.2525. Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. 2011 handbook.cochrane.org
handbook.cochrane.org...
,2626. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-60. When at least 10 studies2525. Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. 2011 handbook.cochrane.org
handbook.cochrane.org...
were available for a meta-analysis, we investigated heterogeneous results through subgroup analysis and meta-regression. For subgroup analyses, we considered the following characteristics: 1) gender; 2) study cycle (the Brazilian medical school years are divided into three cycles of 2 years each); 3) country region where the school is located; 4) cutoff scores (when we noted variation between studies); 5) symptom severity; and 6) risk-of-bias score. For the meta-regression, we considered: 1) proportion of male students; 2) age; and 3) risk-of-bias score. We divided studies into low ( ≥ 0.9) and high ( < 0.9) risk of bias. We assessed evidence of publication bias by Egger’s regression method,2727. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-34. when at least 10 studies were available.2525. Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. 2011 handbook.cochrane.org
handbook.cochrane.org...
We performed meta-analyses using MetaXL version 5.3 (EpiGear International, Sunrise Beach, Queensland, Australia), and carried out meta-regression and Egger’s regression method using the “metafor” function in R software version 3.2.0 (R Foundation for Statistical Computing, Vienna, Austria).
Results
We included 59 studies2828. Abrão CB, Coelho EP, Passos LBdS. Prevalência de sintomas depressivos entre estudantes de medicina da Universidade Federal de Uberlândia. Rev Bras Educ Med. 2008;32:315-23.
29. Aguiar SM, Vieira APGF, Fernandes Vieira KM, Aguiar SM, Nóbrega JO. Prevalência de sintomas de estresse nos estudantes de medicina. J Bras Psiquiatr. 2009;58:34-8.
30. Alberton VC, Dal-Bó MJ, Piovezan AP, Silva RMd. Abnormal eating behaviors among medical students at a university in southern Santa Catarina, Brazil. Rev Bras Educ Med. 2013;37:15-20.
31. Alexandrino-Silva C, Pereira ML, Bustamante C, Ferraz AC, Baldassin S, Andrade AG, et al. Suicidal ideation among students enrolled in healthcare training programs: a cross-sectional study. Rev Bras Psiquiatr. 2009;31:338-44.
32. Almeida AdM, Godinho TM, Bitencourt AGV, Teles MS, Silva AS, Fonseca DC, et al. Common mental disorders among medical students. J Bras Psiquiatr. 2007;56:245-51.
33. Almeida GdC, Souza HRd, Almeida PCd, Almeida BdC, Almeida GH. The prevalence of burnout syndrome in medical students. Arch Clin Psychiatry (São Paulo). 2016;43:6-10.
34. Amaral GFd, Gomide LMdP, Batista MdP, Píccolo PdP, Teles TBG, Oliveira PMd, et al. Sintomas depressivos em acadêmicos de medicina da Universidade Federal de Goiás: um estudo de prevalência. Rev Psiquiatr Rio Gd Sul. 2008;30:124-30.
35. Amorim TC, Amorim MES, Guedes LAC, Ramalho SL, Rivera GA. Evaluation of alcohol addiction among Brazilian Northeast medical students through the alcohol use disorders identification test and the relation with body mass index and smoking. Rev Soc Bras Clin Med. 2012;10:398-401.
36. Baldassin SP, Martins LC, Andrade AGd. Traços de ansiedade entre estudantes de medicina. Arq Med ABC. 2006;31:27-31.
37. Baldassin S, Alves TC, de Andrade AG, Nogueira Martins LA. The characteristics of depressive symptoms in medical students during medical education and training: a cross-sectional study. BMC Med Educ. 2008;8:60.
38. Baldassin S, Silva N, de Toledo Ferraz Alves TC, Castaldelli-Maia JM, Bhugra D, Nogueira-Martins MC, et al. Depression in medical students: cluster symptoms and management. J Affect Disord. 2013;150:110-4.
39. Baltieri DA, Aguiar AS, de Oliveira VH, de Souza Gatti AL, de Souza Aranha e Silva RA. Validation of the pornography consumption inventory in a sample of male Brazilian university students. J Sex Marital Ther. 2015;41:649-60.
40. Bassols AM, Okabayashi LS, Silva AB, Carneiro BB, Feijo F, Guimaraes GC, et al. First- and last-year medical students: is there a difference in the prevalence and intensity of anxiety and depressive symptoms? Rev Bras Psiquiatr. 2014;36:233-40.
41. Bassols AMS, Carneiro BB, Guimarães GC, Okabayashi LMS, Carvalho FG, da Silva AB, et al. Stress and coping in a sample of medical students in Brazil. Arch Clin Psychiatry (São Paulo). 2015;42:1-5.
42. Cardoso HC, Bueno FCdC, Mata JCd, Alves APR, Jochims I, Vaz Filho IHR, et al. Avaliação da qualidade do sono em estudantes de Medicina. Rev Bras Educ Med. 2009;33:349-55.
43. Castaldelli-Maia JM, Martins SS, Bhugra D, Machado MP, Andrade AG, Alexandrino-Silva C, et al. Does ragging play a role in medical student depression - cause or effect? J Affect Disord. 2012;139:291-7.
44. Costa EF, Andrade TM, Silvany Neto AM, Melo EV, Rosa AC, Alencar MA, et al. Common mental disorders among medical students at Universidade Federal de Sergipe: a cross-sectional study. Rev Bras Psiquiatr. 2010;32:11-9.
45. Costa EF, Santana YS, Santos AT, Martins LA, Melo EV, Andrade TM. [Depressive symptoms among medical intern students in a Brazilian public university]. Rev Assoc Med Bras (1992). 2012;58:53-9.
46. Costa EF, Santos SA, Santos AT, Melo EV, Andrade TM. Burnout Syndrome and associated factors among medical students: a cross-sectional study. Clinics (Sao Paulo). 2012;67:573-80.
47. Costa EF, Rocha MM, Santos AT, Melo EV, Martins LA, Andrade TM. Common mental disorders and associated factors among final-year healthcare students. Rev Assoc Med Bras (1992). 2014;60:525-30.
48. Cunha MAB, Neves AAdF, Moreira ME, Hehn FJ, Lopes TP, Ribeiro CCF, et al. Transtornos psiquiátricos menores e procura por cuidados em estudantes de Medicina. Rev Bras Educ Med. 2009;33:321-8.
49. Danda GJdN, Bastos O, de Souza KFR, Azenha M, Ferreira GR. Padrão do ciclo sono-vigília e sonolência excessiva diurna em estudantes de medicina. J Bras Psiquiatr. 2005;54:102-6.
50. Di Pietro M, Silveira DX. Internal validity, dimensionality and performance of the Body Shape Questionnaire in a group of Brazilian college students. Rev Bras Psiquiatr. 2009;31:21-4.
51. Facundes VL, Ludermir AB. Common mental disorders among health care students. Rev Bras Psiquiatr. 2005;27:194-200.
52. Fiorotti KP, Rossoni RR, Borges LH, Miranda AE. Transtornos mentais comuns entre os estudantes do curso de medicina: prevalência e fatores associados. J Bras Psiquiatr. 2010;59:17-23.
53. Gavioli MdA, Silva AG, Gonçalves RJ, Santos ME, Shi KL, Lima MCP. Formando grupos no internato: critérios de escolha, satisfação e sofrimento psíquico. Rev Bras Educ Med. 2009;33:4-9.
54. Hidalgo MP, Caumo W. Sleep disturbances associated with minor psychiatric disorders in medical students. Neurol Sci. 2002;23:35-9.
55. Hirata FC, Lima MC, de Bruin VM, Nobrega PR, Wenceslau GP, de Bruin PF. Depression in medical school: the influence of morningness-eveningness. Chronobiol Int. 2007;24:939-46.
56. Leao PB, Martins LA, Menezes PR, Bellodi PL. Well-being and help-seeking: an exploratory study among final-year medical students. Rev Assoc Med Bras (1992). 2011;57:379-86.
57. Lima MC, Domingues Mde S, Cerqueira AT. [Prevalence and risk factors of common mental disorders among medical students]. Rev Saude Publica. 2006;40:1035-41.
58. Loayza H MP, Ponte TS, Carvalho CG, Pedrotti MR, Nunes PV, Souza CM, et al. Association between mental health screening by self-report questionnaire and insomnia in medical students. Arq Neuropsiquiatr. 2001;59:180-5.
59. Macedo PNAG, Nardotto LL, Dieckmann LHJ, Ferreira YD, Macedo BAG, dos Santos MAP, et al. Factors associated with depressive symptoms in a sample of Brazilian medical students. Rev Bras Educ Med. 2009;33:595-604.
60. Moro A, Valle JBd, Lima LPd. Sintomas depressivos nos estudantes de medicina da Universidade da Região de Joinville (SC). Rev Bras Educ Med. 2005;29:97-102.
61. Nicoli MG, Junior RD. Binge eating disorder and body image perception among university students. Eat Behav. 2011;12:284-8.
62. Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38:438-44.
63. Pagnin D, de Queiroz V. Influence of burnout and sleep difficulties on the quality of life among medical students. Springerplus. 2015;4:676.
64. Paro HB, Morales NM, Silva CH, Rezende CH, Pinto RM, Morales RR, et al. Health-related quality of life of medical students. Med Educ. 2010;44:227-35.
65. de Paula JdA, Borges AMFS, Bezerra LRA, Parente HV, de Paula RCdA, Wajnsztejn R, et al. Prevalência e fatores associados à depressão em estudantes de medicina. Rev Bras Crescimento Desenvolv Hum. 2014;24:274-81.
66. Rique GL, Fernandes Filho GM, Ferreira AD, de Sousa-Munoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7:96-102.
67. Rocha ES, Sassi AP. Transtornos mentais menores entre estudantes de medicina. Rev Bras Educ Med. 2013;37:210-6.
68. de Abreu Santos AT, Grosseman S, de Oliva Costa EF, de Andrade TM. Burnout syndrome among internship medical students. Med Educ. 2011;45:1146.
69. Serra RD, Mattos e Dinato SL, Caseiro MM. Prevalence of depressive and anxiety symptoms in medical students in the city of Santos. J Bras Psiquiatr. 2015;64:213-20.
70. Silva AG, Cerqueira AT, Lima MC. Social support and common mental disorder among medical students. Rev Bras Epidemiol. 2014;17:229-42.
71. Silveira Rda R, Lejderman B, Ferreira PE, Rocha GM. Patterns of non-medical use of methylphenidate among 5th and 6th year students in a medical school in southern Brazil. Trends in Psychiatry Psychother. 2014;36:101-6.
72. Souza FGdMe, Menezes MdGC. Estresse nos estudantes de medicina da Universidade Federal do Ceará. Rev Bras Educ Med. 2005;29:91-6.
73. Tabalipa FdO, Souza MFd, Pfützenreuter G, Lima VC, Traebert E, Traebert J. Prevalence of anxiety and depression among medical students. Rev Bras Educ Med. 2015;39:388-94.
74. Tempski P, Santos IS, Mayer FB, Enns SC, Perotta B, Paro HB, et al. Relationship among medical student resilience, educational environment and quality of life. PLoS One. 2015;10:e0131535.
75. Torres AR, Cruz BL, Vicentini HC, Lima MC, Ramos-Cerqueira AT. Obsessive-compulsive symptoms in medical students: prevalence, severity, and correlates. Acad Psychiatry. 2016;40:46-54.
76. Vasconcelos TCd, Dias BRT, Andrade LR, Melo GF, Barbosa L, Souza E. Prevalência de sintomas de ansiedade e depressão em estudantes de medicina. Rev Bras Educ Med. 2015;39:135-42.
77. Volcan SM, Sousa PL, Mari Jde J, Horta BL. [Relationship between spiritual well-being and minor psychiatric disorders: a cross-sectional study]. Rev Saude Publica. 2003;37:440-5.
78. Amorim AVC, Kikko EO, Abrantes MM, Andrade VLâ. álcool e alcoolismo: estudo de prevalência entre discentes do curso de Medicina da UNIFENAS em Belo Horizonte - Minas Gerais. Rev Med Minas Gerais. 2008;18:16-23.
79. Baldisserotto CM, Filho ES, Nedel F, Sakae TM. Problemas psiquiátricos menores e indicadores do uso problemático de álcool entre os estudantes de medicina da Universidade do Sul de Santa Catarina - UNISUL. ACM Arq Catarin Med. 2005;34:73-9.
80. Bassols AM, Rodrigues GS, Seeger GM, Eizirik CL, Sordi AO, Reche M. A prevalência de estresse em uma amostra de estudantes do curso de medicina da Universidade Federal do Rio Grande do Sul. Rev HCPA. 2008;28:153-7.
81. Bruch TP, Jornada LK, Carneiro EA. Presença de sintomas psiquiátricos em estudantes de medicina de Universidade do sul do Brasil. ACM Arq Catarin Med. 2009;38:61-5.
82. Furtado ES, Falcone EMO, Clark C. Avaliação do estresse e das habilidades sociais na experiência acadêmica de estudantes de medicina de uma universidade do Rio de Janeiro. Interacao Psicol. 2003;7:43-51.
83. Guimarães KBS. Estresse e a formação médica: implicações na saúde mental dos estudantes [thesis]. São Paulo: UNESP de Assis; 2005.
84. Porcu M, Fritzen CV, Helber C. Sintomas depressivos nos estudantes de medicina da Universidade Estadual de Maringá [Internet]. [cited 2017 Apr 26]. www2.unifesp.br/dpsiq/polbr/ppm/original5_01.htm
www2.unifesp.br/dpsiq/polbr/ppm/original...
85. Souza L. Prevalência de sintomas depressivos, ansiosos e estresse em acadêmicos de medicina [dissertation]. São Paulo: Universidade de São Paulo; 2010.-8686. Vallilo NG, Danzi R Jr, Hübner CvK, Novo NF, Gobbo R. Prevalence of depressive symptoms in medical students. Rev Soc Bras Clin Med. 2011;9:36-41. in the qualitative analysis, and 572828. Abrão CB, Coelho EP, Passos LBdS. Prevalência de sintomas depressivos entre estudantes de medicina da Universidade Federal de Uberlândia. Rev Bras Educ Med. 2008;32:315-23.
29. Aguiar SM, Vieira APGF, Fernandes Vieira KM, Aguiar SM, Nóbrega JO. Prevalência de sintomas de estresse nos estudantes de medicina. J Bras Psiquiatr. 2009;58:34-8.
30. Alberton VC, Dal-Bó MJ, Piovezan AP, Silva RMd. Abnormal eating behaviors among medical students at a university in southern Santa Catarina, Brazil. Rev Bras Educ Med. 2013;37:15-20.
31. Alexandrino-Silva C, Pereira ML, Bustamante C, Ferraz AC, Baldassin S, Andrade AG, et al. Suicidal ideation among students enrolled in healthcare training programs: a cross-sectional study. Rev Bras Psiquiatr. 2009;31:338-44.
32. Almeida AdM, Godinho TM, Bitencourt AGV, Teles MS, Silva AS, Fonseca DC, et al. Common mental disorders among medical students. J Bras Psiquiatr. 2007;56:245-51.
33. Almeida GdC, Souza HRd, Almeida PCd, Almeida BdC, Almeida GH. The prevalence of burnout syndrome in medical students. Arch Clin Psychiatry (São Paulo). 2016;43:6-10.
34. Amaral GFd, Gomide LMdP, Batista MdP, Píccolo PdP, Teles TBG, Oliveira PMd, et al. Sintomas depressivos em acadêmicos de medicina da Universidade Federal de Goiás: um estudo de prevalência. Rev Psiquiatr Rio Gd Sul. 2008;30:124-30.
35. Amorim TC, Amorim MES, Guedes LAC, Ramalho SL, Rivera GA. Evaluation of alcohol addiction among Brazilian Northeast medical students through the alcohol use disorders identification test and the relation with body mass index and smoking. Rev Soc Bras Clin Med. 2012;10:398-401.
36. Baldassin SP, Martins LC, Andrade AGd. Traços de ansiedade entre estudantes de medicina. Arq Med ABC. 2006;31:27-31.-3737. Baldassin S, Alves TC, de Andrade AG, Nogueira Martins LA. The characteristics of depressive symptoms in medical students during medical education and training: a cross-sectional study. BMC Med Educ. 2008;8:60.,3939. Baltieri DA, Aguiar AS, de Oliveira VH, de Souza Gatti AL, de Souza Aranha e Silva RA. Validation of the pornography consumption inventory in a sample of male Brazilian university students. J Sex Marital Ther. 2015;41:649-60.
40. Bassols AM, Okabayashi LS, Silva AB, Carneiro BB, Feijo F, Guimaraes GC, et al. First- and last-year medical students: is there a difference in the prevalence and intensity of anxiety and depressive symptoms? Rev Bras Psiquiatr. 2014;36:233-40.
41. Bassols AMS, Carneiro BB, Guimarães GC, Okabayashi LMS, Carvalho FG, da Silva AB, et al. Stress and coping in a sample of medical students in Brazil. Arch Clin Psychiatry (São Paulo). 2015;42:1-5.
42. Cardoso HC, Bueno FCdC, Mata JCd, Alves APR, Jochims I, Vaz Filho IHR, et al. Avaliação da qualidade do sono em estudantes de Medicina. Rev Bras Educ Med. 2009;33:349-55.
43. Castaldelli-Maia JM, Martins SS, Bhugra D, Machado MP, Andrade AG, Alexandrino-Silva C, et al. Does ragging play a role in medical student depression - cause or effect? J Affect Disord. 2012;139:291-7.
44. Costa EF, Andrade TM, Silvany Neto AM, Melo EV, Rosa AC, Alencar MA, et al. Common mental disorders among medical students at Universidade Federal de Sergipe: a cross-sectional study. Rev Bras Psiquiatr. 2010;32:11-9.
45. Costa EF, Santana YS, Santos AT, Martins LA, Melo EV, Andrade TM. [Depressive symptoms among medical intern students in a Brazilian public university]. Rev Assoc Med Bras (1992). 2012;58:53-9.
46. Costa EF, Santos SA, Santos AT, Melo EV, Andrade TM. Burnout Syndrome and associated factors among medical students: a cross-sectional study. Clinics (Sao Paulo). 2012;67:573-80.
47. Costa EF, Rocha MM, Santos AT, Melo EV, Martins LA, Andrade TM. Common mental disorders and associated factors among final-year healthcare students. Rev Assoc Med Bras (1992). 2014;60:525-30.
48. Cunha MAB, Neves AAdF, Moreira ME, Hehn FJ, Lopes TP, Ribeiro CCF, et al. Transtornos psiquiátricos menores e procura por cuidados em estudantes de Medicina. Rev Bras Educ Med. 2009;33:321-8.
49. Danda GJdN, Bastos O, de Souza KFR, Azenha M, Ferreira GR. Padrão do ciclo sono-vigília e sonolência excessiva diurna em estudantes de medicina. J Bras Psiquiatr. 2005;54:102-6.
50. Di Pietro M, Silveira DX. Internal validity, dimensionality and performance of the Body Shape Questionnaire in a group of Brazilian college students. Rev Bras Psiquiatr. 2009;31:21-4.
51. Facundes VL, Ludermir AB. Common mental disorders among health care students. Rev Bras Psiquiatr. 2005;27:194-200.-5252. Fiorotti KP, Rossoni RR, Borges LH, Miranda AE. Transtornos mentais comuns entre os estudantes do curso de medicina: prevalência e fatores associados. J Bras Psiquiatr. 2010;59:17-23.,5454. Hidalgo MP, Caumo W. Sleep disturbances associated with minor psychiatric disorders in medical students. Neurol Sci. 2002;23:35-9.
55. Hirata FC, Lima MC, de Bruin VM, Nobrega PR, Wenceslau GP, de Bruin PF. Depression in medical school: the influence of morningness-eveningness. Chronobiol Int. 2007;24:939-46.
56. Leao PB, Martins LA, Menezes PR, Bellodi PL. Well-being and help-seeking: an exploratory study among final-year medical students. Rev Assoc Med Bras (1992). 2011;57:379-86.
57. Lima MC, Domingues Mde S, Cerqueira AT. [Prevalence and risk factors of common mental disorders among medical students]. Rev Saude Publica. 2006;40:1035-41.
58. Loayza H MP, Ponte TS, Carvalho CG, Pedrotti MR, Nunes PV, Souza CM, et al. Association between mental health screening by self-report questionnaire and insomnia in medical students. Arq Neuropsiquiatr. 2001;59:180-5.
59. Macedo PNAG, Nardotto LL, Dieckmann LHJ, Ferreira YD, Macedo BAG, dos Santos MAP, et al. Factors associated with depressive symptoms in a sample of Brazilian medical students. Rev Bras Educ Med. 2009;33:595-604.
60. Moro A, Valle JBd, Lima LPd. Sintomas depressivos nos estudantes de medicina da Universidade da Região de Joinville (SC). Rev Bras Educ Med. 2005;29:97-102.
61. Nicoli MG, Junior RD. Binge eating disorder and body image perception among university students. Eat Behav. 2011;12:284-8.
62. Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38:438-44.
63. Pagnin D, de Queiroz V. Influence of burnout and sleep difficulties on the quality of life among medical students. Springerplus. 2015;4:676.
64. Paro HB, Morales NM, Silva CH, Rezende CH, Pinto RM, Morales RR, et al. Health-related quality of life of medical students. Med Educ. 2010;44:227-35.
65. de Paula JdA, Borges AMFS, Bezerra LRA, Parente HV, de Paula RCdA, Wajnsztejn R, et al. Prevalência e fatores associados à depressão em estudantes de medicina. Rev Bras Crescimento Desenvolv Hum. 2014;24:274-81.
66. Rique GL, Fernandes Filho GM, Ferreira AD, de Sousa-Munoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7:96-102.
67. Rocha ES, Sassi AP. Transtornos mentais menores entre estudantes de medicina. Rev Bras Educ Med. 2013;37:210-6.
68. de Abreu Santos AT, Grosseman S, de Oliva Costa EF, de Andrade TM. Burnout syndrome among internship medical students. Med Educ. 2011;45:1146.
69. Serra RD, Mattos e Dinato SL, Caseiro MM. Prevalence of depressive and anxiety symptoms in medical students in the city of Santos. J Bras Psiquiatr. 2015;64:213-20.
70. Silva AG, Cerqueira AT, Lima MC. Social support and common mental disorder among medical students. Rev Bras Epidemiol. 2014;17:229-42.
71. Silveira Rda R, Lejderman B, Ferreira PE, Rocha GM. Patterns of non-medical use of methylphenidate among 5th and 6th year students in a medical school in southern Brazil. Trends in Psychiatry Psychother. 2014;36:101-6.
72. Souza FGdMe, Menezes MdGC. Estresse nos estudantes de medicina da Universidade Federal do Ceará. Rev Bras Educ Med. 2005;29:91-6.
73. Tabalipa FdO, Souza MFd, Pfützenreuter G, Lima VC, Traebert E, Traebert J. Prevalence of anxiety and depression among medical students. Rev Bras Educ Med. 2015;39:388-94.
74. Tempski P, Santos IS, Mayer FB, Enns SC, Perotta B, Paro HB, et al. Relationship among medical student resilience, educational environment and quality of life. PLoS One. 2015;10:e0131535.
75. Torres AR, Cruz BL, Vicentini HC, Lima MC, Ramos-Cerqueira AT. Obsessive-compulsive symptoms in medical students: prevalence, severity, and correlates. Acad Psychiatry. 2016;40:46-54.
76. Vasconcelos TCd, Dias BRT, Andrade LR, Melo GF, Barbosa L, Souza E. Prevalência de sintomas de ansiedade e depressão em estudantes de medicina. Rev Bras Educ Med. 2015;39:135-42.
77. Volcan SM, Sousa PL, Mari Jde J, Horta BL. [Relationship between spiritual well-being and minor psychiatric disorders: a cross-sectional study]. Rev Saude Publica. 2003;37:440-5.
78. Amorim AVC, Kikko EO, Abrantes MM, Andrade VLâ. álcool e alcoolismo: estudo de prevalência entre discentes do curso de Medicina da UNIFENAS em Belo Horizonte - Minas Gerais. Rev Med Minas Gerais. 2008;18:16-23.
79. Baldisserotto CM, Filho ES, Nedel F, Sakae TM. Problemas psiquiátricos menores e indicadores do uso problemático de álcool entre os estudantes de medicina da Universidade do Sul de Santa Catarina - UNISUL. ACM Arq Catarin Med. 2005;34:73-9.
80. Bassols AM, Rodrigues GS, Seeger GM, Eizirik CL, Sordi AO, Reche M. A prevalência de estresse em uma amostra de estudantes do curso de medicina da Universidade Federal do Rio Grande do Sul. Rev HCPA. 2008;28:153-7.
81. Bruch TP, Jornada LK, Carneiro EA. Presença de sintomas psiquiátricos em estudantes de medicina de Universidade do sul do Brasil. ACM Arq Catarin Med. 2009;38:61-5.
82. Furtado ES, Falcone EMO, Clark C. Avaliação do estresse e das habilidades sociais na experiência acadêmica de estudantes de medicina de uma universidade do Rio de Janeiro. Interacao Psicol. 2003;7:43-51.
83. Guimarães KBS. Estresse e a formação médica: implicações na saúde mental dos estudantes [thesis]. São Paulo: UNESP de Assis; 2005.
84. Porcu M, Fritzen CV, Helber C. Sintomas depressivos nos estudantes de medicina da Universidade Estadual de Maringá [Internet]. [cited 2017 Apr 26]. www2.unifesp.br/dpsiq/polbr/ppm/original5_01.htm
www2.unifesp.br/dpsiq/polbr/ppm/original...
85. Souza L. Prevalência de sintomas depressivos, ansiosos e estresse em acadêmicos de medicina [dissertation]. São Paulo: Universidade de São Paulo; 2010.-8686. Vallilo NG, Danzi R Jr, Hübner CvK, Novo NF, Gobbo R. Prevalence of depressive symptoms in medical students. Rev Soc Bras Clin Med. 2011;9:36-41. studies involving a total of 18,015 medical students in the quantitative analysis (Table 1). All forest plots are available on request from the authors. We conducted subgroup analyses for depression and CMD (Tables 2 and 3).
Prevalence of mental health problems
Depression
In an analysis of 25 studies, the summary prevalence of depression among medical students in Brazil was 30.6% (95%CI 24.0-37.7, p ≤ 0.01, I2 = 97.96%). Table 2 reports stratified prevalences of depression.
The prevalences of depression were significantly different when using medium (32.9%, 95%CI 28.9-37.2) vs. higher (9.9%, 95%CI 6.5-14.1) cutoff scores. When stratified by symptom severity, aggregate prevalence was 23.3% (95%CI 19.3-27.6) for students with mild symptoms, 8.4% (95%CI 5.4-12.0) for moderate symptoms, and 2.1% (95%CI 0.8-4.0) for severe symptoms. For meta-regression, only the risk-of-bias score was significant (beta = 0.7937, p = 0.0092).
Common mental disorders
CMDs can be translated as an indicator of a non-psychotic mental disorder,8787. Gonçalves DM, Stein AT, Kapczinski F. [Performance of the self-reporting questionnaire as a psychiatric screening questionnaire: a comparative study with structured clinical interview for DSM-IV-TR]. Cad Saude Publica. 2008;24:380-90. evaluated by the 20-item Self-Report Questionnaire (SRQ-20). The questionnaire assesses 20 somatic, mood and anxious symptoms. It is not a diagnostic instrument, but a community screening tool, and cutoff scores may vary according to the cultural context in which it is administered.
The prevalence of CMDs among medical students in Brazil was 31.5% (95%CI 26.1-37.1, p ≤ 0.01, I2 = 92.67%), based on 13 studies. Simple meta-regression showed that both risk-of-bias score (beta = 0.4986, p = 0.0029) and percentage of male students (beta = -0.0100, p < 0.01) were significant, but only the percentage of male students was significant when both variables were included in the regression.
We detected minimal variation in cutoff scores for CMD, and severity of symptoms is not reported for CMD. Thus, subgroup analyses were not conducted by these characteristics. When prevalences were stratified by region, students from the South region of the country showed a significantly lower prevalence (21.1%, 95%CI 18.9-23.6) compared to those from the Southeast (38.1%, 95%CI 29.5-47.15) and Northeast (31.5%, 95%CI 26.1-37.1) regions (Table 3).
Other mental health problems
Analysis of three studies yielded a summary prevalence of burnout of 13.1% (95%CI 10.2-16.4) among medical students in Brazil. One study reported the prevalence of current suicidal ideation and hopelessness through standardized and validated tools. The prevalences were, respectively, 13.4% and 95.5%.
Four studies reported prevalences of trait anxiety (89.6%, 95%CI 43.3-100.00), two of state anxiety (62.1%, 95%CI 0.00-100.00), six of anxiety in a general sense (32.9%, 95%CI 22.0-44.9), six of stress (49.9%, 95%CI 57.8-53.0), and one of obsessive-compulsive disorder (3.8%). Pooled data from three studies yielded an aggregate prevalence of problematic alcohol use of 32.9% (95%CI 29.3-36.6). The aggregate prevalence of low sleep quality was 51.5% (95%CI 21.2-81.2, pooled data from four studies), while that of excessive daytime sleepiness was 46.1% (95%CI 37.7-54.5, pooled data from four studies).
The prevalence of compulsive eating and disordered eating patterns was 10.9% and 10.0% respectively (data from one study). Disordered eating patterns were more prevalent among females (17.0%) than males (2.6%). One study investigated concern over body shape, but only reported prevalences for females (21.1%) and males (9.5%) independently.
Factors associated with mental health problems
To balance the effect of multiple comparisons (see paragraph on limitations, Discussion section) and for ease of interpretation, we assessed factors that showed significant correlations in more than one study or those significant after multivariate analyses (Table 4). Female gender was significantly associated with depression, anxiety, and stress, while male gender was more associated with burnout. Thoughts of dropping out, later stages of the course, little involvement in leisure activities, lack of emotional support, and academic overload were correlated with MHP.
Assessment of publication bias, quality of studies, and sensitivity analysis
We found no significant evidence of publication bias in the 25 studies that investigated depression (p = 0.0658) or in the 13 studies that investigated CMD (p = 0.6542). We did not conduct such analyses for the other conditions because too few studies were available.
Risk-of-bias tool scores ranged from 5 to 10 out of a possible 10 points (table available on request from the authors). As noted above, risk-of-bias score was the only significant factor in the meta-regression analysis for depression, while for CMD it was significant on simple meta-regression. Studies with low risk of bias tended to report higher prevalences of depression (37.4%, 95%CI 27.4-47.7) and CMD (37.7%, 95%CI 31.0-44.6), than those with high risk of bias (30.6% [95%CI 24.0-37.7] and 31.5% [95%CI 26.1-37.1] respectively). However, the difference was not significant. Sensitivity analysis showed no significant difference between results for the QE model, when compared to the RE model.
Discussion
Our findings support those from other parts of the world,99. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73.,1313. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-68.
14. Cuttilan AN, Sayampanathan AA, Ho RC. Mental health issues amongst medical students in Asia: a systematic review [2000-2015]. Ann Transl Med. 2016;4:72.
15. Lei XY, Xiao LM, Liu YN, Li YM. Prevalence of depression among chinese university students: a meta-analysis. PLoS One. 2016;11:e0153454.
16. Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ. 2014;48:963-79.-1717. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214-36. emphasizing how prevalent depression and other mental disorders are among medical students. Among the included studies, more had been published from 2010-2016 than during the entire preceding decade. This draws attention to the fact that, although these issues have long been reported, they continue to be common in the lives of medical students, possibly contributing to the high prevalence of MHPs among physicians.8888. Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314:2373-83.,8989. Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1:236-42.
We report that a high proportion of Brazilian medical students are suffering from various MHPs. These include psychological stress, anxiety, depression, sleep pattern disorders, burnout, eating disorders, and potentially hazardous alcohol use.
The most prevalent mental health problem that fitted the meta-analysis was trait anxiety (89.6%), indicating that most medical students have a considerably permanent tendency to experience anxiety, stress, and worries.9090. Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger state-trait anxiety inventory (STAI). Br J Clin Psychol. 1992;31:301-6. Yates et al.1111. Yates J, James D, Aston I. Pre-existing mental health problems in medical students: a retrospective survey. Med Teach. 2008;30:319-21. observed, in a retrospective survey, that medical students with a mental health problem were more inclined to have a pertinent pre-admission mental health history. Moreover, Puthran et al.1313. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-68. have found a tendency of depression prevalence to decline in later years of the medical course. These findings suggest that the high levels of mental disorders among medical students may not be predominantly due to a toxic learning environment, as some authors have argued,77. Tempski P, Bellodi PL, Paro HB, Enns SC, Martins MA, Schraiber LB. What do medical students think about their quality of life? A qualitative study. BMC Med Educ. 2012;12:106.,9191. Wolf TM. Stress, coping and health: enhancing well-being during medical school. Med Educ. 1994;28:8-17; discussion 55-7. but rather to the contribution of the characteristics of individuals selected through a highly competitive entrance exam. Other hypotheses are that final-year students might be receiving more treatment or feeling more fulfillment from their professional choice as they become more in charge of patient care. In the worst-case scenario, those more severely depressed students have already dropped out. This does not mean that students with MHPs should not receive appropriate support within their higher-education institutions. It is precisely because these high prevalences are observed that we believe an open, non-stigmatized communication should exist between students and the institution, especially during the early years of training.
Our analysis showed that depressive symptoms, when stratified by severity, are predominantly mild – an evaluation that was not done in previous reviews.1313. Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-68.,1717. Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214-36. Assessment of symptom severity in depression is based on the number of symptoms, functional impairment, and suffering imposed by symptoms.9292. Lux V, Aggen SH, Kendler KS. The DSM-IV definition of severity of major depression: inter-relationship and validity. Psychol Med. 2010;40:1691-701. Following this construct, which is also used by depression scales,9292. Lux V, Aggen SH, Kendler KS. The DSM-IV definition of severity of major depression: inter-relationship and validity. Psychol Med. 2010;40:1691-701.,9393. Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken). 2011;63:S454-66. mild depression imposes just the number of symptoms required for diagnosis or a few more, and produces only mild social/occupational impairment.9494. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Arlington: American Psychiatric Publishing; 1994. It is different from minor or minimal or subthreshold depression,9595. Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry. 2010;196:365-71. and benefits from evidence-based treatment (e.g., cognitive-behavioral therapy or interpersonal therapy, alone or in combination with antidepressants9696. Parikh SV, Segal ZV, Grigoriadis S, Ravindran AV, Kennedy SH, Lam RW, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication. J Affect Disord. 2009;117:S15-25.). The extent to which mild depression symptoms affect the lives of medical students should be investigated in future longitudinal studies. However, our finding is not completely unexpected. Because depression can be a debilitating disorder, only students that were performing academic activities at the times of data collection were appraised, making students that dropped out or were absent due to a mental disorder not visible to the study (see paragraph on limitations below).
Many MHPs and their correlations intersect, suggesting that they might be coexistent in high-risk groups of students. Female students tended to have higher prevalences of depression and CMD. Additionally, female gender was associated with mood and anxiety disorders, while male gender was associated with burnout. Similar gender differences are also observed in the general population and in medical students from other parts of the world.99. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73.,9797. Andrade LH, Wang YP, Andreoni S, Silveira CM, Alexandrino-Silva C, Siu ER, et al. Mental disorders in megacities: findings from the São Paulo megacity mental health survey, Brazil. PLoS One. 2012;7:e31879.,9898. Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095-105. Modifiable stressors also need to be addressed to improve well-being. As a recent systematic review9999. Wasson LT, Cusmano A, Meli L, Louh I, Falzon L, Hampsey M, et al. Association between learning environment interventions and medical student well-being: a systematic review. JAMA. 2016;316:2237-52. revealed, there is no satisfactory evidence that learning environment interventions could contribute to improved mental well-being in medical students; additional high-quality research is needed in this area. We observed that signs of lack of motivation (e.g., thoughts of dropping out, dissatisfaction with the course, decreased academic efficacy) and lack of emotional support were associated with MHP, as in medical students from other countries.99. Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73. The use of portfolios,100100. Buckley S, Coleman J, Davison I, Khan KS, Zamora J, Malick S, et al. The educational effects of portfolios on undergraduate student learning: a Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 11. Med Teach. 2009;31:282-98. self-assessments,101101. Sharma R, Jain A, Gupta N, Garg S, Batta M, Dhir SK. Impact of self-assessment by students on their learning. Int J Appl Basic Med Res. 2016;6:226-9. and continued mentorship102102. Kalén S, Ponzer S, Seeberger A, Kiessling A, Silén C. Longitudinal mentorship to support the development of medical students’ future professional role: a qualitative study. BMC Med Educ. 2015;15:97. in undergraduate medical education could improve students’ engagement and reflection about the course, alleviating sources of distress and helping students perceive their coursework as a gratifying activity. A drop in academic performance can be an indicative of a mental disorder. This is a key marker, because academic records are usually easily available to tutors. Future studies could consider the efficacy of using this kind of information to identify students that are potentially in decline.
This review has important limitations. We extracted data from cross-sectional studies to summarize associated factors; therefore, we must note that this type of study design is not suitable for making causal inferences. Also, many studies made simultaneous multiple comparisons between subgroups, possibly generating false-positive results. Obvious heterogeneity existed among studies. We consider that risk of bias is a relevant reason that can contribute to inter-study differences, as indicated by the meta-regression. Still, most of the heterogeneity remains unexplained. Neyman bias (where most severe cases would be inadvertently excluded from the study, e.g. due to hospitalization; also called survival bias) is an example of bias that is unlikely to be described, inadvertently leading to more optimistic findings. Prevalence values can also differ when researchers use different time frames, environments, or data collection methods. There is no consensus as to the ideal cutoff score for depression, and we observed significant differences in prevalence values for studies that used different cutoff scores. For most of the outcomes, few studies were available, possibly leading to skewed results. No study reported the prevalence of psychotic or personality disorders, suggesting that this is a gap in the literature. Finally, the tools used do not aim at diagnosis. This could result in larger prevalences, since sensitivity is commonly preferred when using screening tools.
On the basis of this review, the pooled prevalences of depression, anxiety, CMD, and problematic alcohol use among medical students in Brazil ranged from 30.6 to 32.9%. Approximately half of the students were experiencing low sleep quality, and 46.1% experienced excessive daytime sleepiness. Burnout affected approximately 13% of students. These findings suggest that future physicians are at great risk of depression, anxiety, alcohol-related, sleep, and eating disorders. Our findings are in line with studies reporting MHPs among medical students in other countries, which suggests the existence of a global problem. Signs of lack of motivation, insecurity, poor academic performance, financial problems, and lack of emotional support were all associated with MHPs, and constitute modifiable stressors that could be targets for novel interventions. As Brazilian medical students are at high risk of MHPs, it is imperative that psychosocial support be provided within higher-education institutions and that students be monitored for frequency and severity of these problems. Evidence-based interventions are needed to promote well-being and mental health.
Acknowledgements
The authors thank Dr. Christopher N. Connolly for his careful work in revising the manuscript and Dr. Christiane B. Lourenço and Ms. Elis C. Francischetto for their support in the development of the research protocol. The authors also thank Dr. George Stoica and Dr. Suhail A. Doi for their helpful advice.
References
-
1Lins L, Carvalho FM, Menezes MS, Porto-Silva L, Damasceno H. Health-related quality of life of students from a private medical school in Brazil. Int J Med Educ. 2015;6:149-54.
-
2Neumann M, Edelhäuser F, Tauschel D, Fischer MR, Wirtz M, Woopen C, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86:996-1009.
-
3Shanafelt TD, West C, Zhao X, Novotny P, Kolars J, Habermann T, et al. Relationship between increased personal well-being and enhanced empathy among internal medicine residents. J Gen Intern Med. 2005;20:559-64.
-
4Dyrbye LN, Harper W, Moutier C, Durning SJ, Power DV, Massie FS, et al. A multi-institutional study exploring the impact of positive mental health on medical students’ professionalism in an era of high burnout. Acad Med. 2012;87:1024-31.
-
5Pagnin D, de Queiroz V. Comparison of quality of life between medical students and young general populations. Educ Health (Abingdon). 2015;28:209-12.
-
6Dyrbye LN, West CP, Satele D, Boone S, Tan L, Sloan J, et al. Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med. 2014;89:443-51.
-
7Tempski P, Bellodi PL, Paro HB, Enns SC, Martins MA, Schraiber LB. What do medical students think about their quality of life? A qualitative study. BMC Med Educ. 2012;12:106.
-
8Figueiredo AMd, Ribeiro GM, Reggiani ALM, Pinheiro BdA, Leopoldo GO, Duarte JAH, et al. Percepções dos estudantes de medicina da ufop sobre sua qualidade de vida. Rev Bras Educ Med. 2014;38:435-43.
-
9Dyrbye LN, Thomas MR, Shanafelt TD. Systematic review of depression, anxiety, and other indicators of psychological distress among U.S. and Canadian medical students. Acad Med. 2006;81:354-73.
-
10Meyer C, Guimarães ACdA, Machado Z, Parcias SR. Qualidade de vida e estresse ocupacional em estudantes de medicina. Rev Bras Educ Med. 2012;36:489-98.
-
11Yates J, James D, Aston I. Pre-existing mental health problems in medical students: a retrospective survey. Med Teach. 2008;30:319-21.
-
12Zuardi AW, Prota Fdel G, Del-Ben CM. Reduction of the anxiety of medical students after curricular reform. Rev Bras Psiquiatr. 2008;30:136-8.
-
13Puthran R, Zhang MW, Tam WW, Ho RC. Prevalence of depression amongst medical students: a meta-analysis. Med Educ. 2016;50:456-68.
-
14Cuttilan AN, Sayampanathan AA, Ho RC. Mental health issues amongst medical students in Asia: a systematic review [2000-2015]. Ann Transl Med. 2016;4:72.
-
15Lei XY, Xiao LM, Liu YN, Li YM. Prevalence of depression among chinese university students: a meta-analysis. PLoS One. 2016;11:e0153454.
-
16Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ. 2014;48:963-79.
-
17Rotenstein LS, Ramos MA, Torre M, Segal JB, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students: a systematic review and meta-analysis. JAMA. 2016;316:2214-36.
-
18Baldassin S. Ansiedade e depressão no estudante de medicina: revisão de estudos brasileiros. Cadernos ABEM. 2010;6:19-26.
-
19Pacheco JPG, Ribeiro TB, Francischetto EC, Arab C, Lourenço CB, Bezerra IMP, et al. Prevalence of depression and other mental health problems amongst medical students in Brazil: systematic review and meta-analysis [Internet]. Heslington: University of York. 2016 [cited 2017 Apr 15]. http://crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016048236
» http://crd.york.ac.uk/PROSPERO/display_record.asp?ID=CRD42016048236 -
20Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264-9, W64.
-
21Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934-9.
-
22Doi SA, Barendregt JJ, Khan S, Thalib L, Williams GM. Advances in the meta-analysis of heterogeneous clinical trials II: the quality effects model. Contemp Clin Trials. 2015;45:123-9.
-
23Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000;283:2008-12.
-
24Barendregt JJ, Doi SA, Lee YY, Norman RE, Vos T. Meta-analysis of prevalence. J Epidemiol Community Health. 2013;67:974-8.
-
25Higgins J, Green S, editors. Cochrane handbook for systematic reviews of interventions. Version 5.1.0 [updated March 2011]. 2011 handbook.cochrane.org
» handbook.cochrane.org -
26Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-60.
-
27Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629-34.
-
28Abrão CB, Coelho EP, Passos LBdS. Prevalência de sintomas depressivos entre estudantes de medicina da Universidade Federal de Uberlândia. Rev Bras Educ Med. 2008;32:315-23.
-
29Aguiar SM, Vieira APGF, Fernandes Vieira KM, Aguiar SM, Nóbrega JO. Prevalência de sintomas de estresse nos estudantes de medicina. J Bras Psiquiatr. 2009;58:34-8.
-
30Alberton VC, Dal-Bó MJ, Piovezan AP, Silva RMd. Abnormal eating behaviors among medical students at a university in southern Santa Catarina, Brazil. Rev Bras Educ Med. 2013;37:15-20.
-
31Alexandrino-Silva C, Pereira ML, Bustamante C, Ferraz AC, Baldassin S, Andrade AG, et al. Suicidal ideation among students enrolled in healthcare training programs: a cross-sectional study. Rev Bras Psiquiatr. 2009;31:338-44.
-
32Almeida AdM, Godinho TM, Bitencourt AGV, Teles MS, Silva AS, Fonseca DC, et al. Common mental disorders among medical students. J Bras Psiquiatr. 2007;56:245-51.
-
33Almeida GdC, Souza HRd, Almeida PCd, Almeida BdC, Almeida GH. The prevalence of burnout syndrome in medical students. Arch Clin Psychiatry (São Paulo). 2016;43:6-10.
-
34Amaral GFd, Gomide LMdP, Batista MdP, Píccolo PdP, Teles TBG, Oliveira PMd, et al. Sintomas depressivos em acadêmicos de medicina da Universidade Federal de Goiás: um estudo de prevalência. Rev Psiquiatr Rio Gd Sul. 2008;30:124-30.
-
35Amorim TC, Amorim MES, Guedes LAC, Ramalho SL, Rivera GA. Evaluation of alcohol addiction among Brazilian Northeast medical students through the alcohol use disorders identification test and the relation with body mass index and smoking. Rev Soc Bras Clin Med. 2012;10:398-401.
-
36Baldassin SP, Martins LC, Andrade AGd. Traços de ansiedade entre estudantes de medicina. Arq Med ABC. 2006;31:27-31.
-
37Baldassin S, Alves TC, de Andrade AG, Nogueira Martins LA. The characteristics of depressive symptoms in medical students during medical education and training: a cross-sectional study. BMC Med Educ. 2008;8:60.
-
38Baldassin S, Silva N, de Toledo Ferraz Alves TC, Castaldelli-Maia JM, Bhugra D, Nogueira-Martins MC, et al. Depression in medical students: cluster symptoms and management. J Affect Disord. 2013;150:110-4.
-
39Baltieri DA, Aguiar AS, de Oliveira VH, de Souza Gatti AL, de Souza Aranha e Silva RA. Validation of the pornography consumption inventory in a sample of male Brazilian university students. J Sex Marital Ther. 2015;41:649-60.
-
40Bassols AM, Okabayashi LS, Silva AB, Carneiro BB, Feijo F, Guimaraes GC, et al. First- and last-year medical students: is there a difference in the prevalence and intensity of anxiety and depressive symptoms? Rev Bras Psiquiatr. 2014;36:233-40.
-
41Bassols AMS, Carneiro BB, Guimarães GC, Okabayashi LMS, Carvalho FG, da Silva AB, et al. Stress and coping in a sample of medical students in Brazil. Arch Clin Psychiatry (São Paulo). 2015;42:1-5.
-
42Cardoso HC, Bueno FCdC, Mata JCd, Alves APR, Jochims I, Vaz Filho IHR, et al. Avaliação da qualidade do sono em estudantes de Medicina. Rev Bras Educ Med. 2009;33:349-55.
-
43Castaldelli-Maia JM, Martins SS, Bhugra D, Machado MP, Andrade AG, Alexandrino-Silva C, et al. Does ragging play a role in medical student depression - cause or effect? J Affect Disord. 2012;139:291-7.
-
44Costa EF, Andrade TM, Silvany Neto AM, Melo EV, Rosa AC, Alencar MA, et al. Common mental disorders among medical students at Universidade Federal de Sergipe: a cross-sectional study. Rev Bras Psiquiatr. 2010;32:11-9.
-
45Costa EF, Santana YS, Santos AT, Martins LA, Melo EV, Andrade TM. [Depressive symptoms among medical intern students in a Brazilian public university]. Rev Assoc Med Bras (1992). 2012;58:53-9.
-
46Costa EF, Santos SA, Santos AT, Melo EV, Andrade TM. Burnout Syndrome and associated factors among medical students: a cross-sectional study. Clinics (Sao Paulo). 2012;67:573-80.
-
47Costa EF, Rocha MM, Santos AT, Melo EV, Martins LA, Andrade TM. Common mental disorders and associated factors among final-year healthcare students. Rev Assoc Med Bras (1992). 2014;60:525-30.
-
48Cunha MAB, Neves AAdF, Moreira ME, Hehn FJ, Lopes TP, Ribeiro CCF, et al. Transtornos psiquiátricos menores e procura por cuidados em estudantes de Medicina. Rev Bras Educ Med. 2009;33:321-8.
-
49Danda GJdN, Bastos O, de Souza KFR, Azenha M, Ferreira GR. Padrão do ciclo sono-vigília e sonolência excessiva diurna em estudantes de medicina. J Bras Psiquiatr. 2005;54:102-6.
-
50Di Pietro M, Silveira DX. Internal validity, dimensionality and performance of the Body Shape Questionnaire in a group of Brazilian college students. Rev Bras Psiquiatr. 2009;31:21-4.
-
51Facundes VL, Ludermir AB. Common mental disorders among health care students. Rev Bras Psiquiatr. 2005;27:194-200.
-
52Fiorotti KP, Rossoni RR, Borges LH, Miranda AE. Transtornos mentais comuns entre os estudantes do curso de medicina: prevalência e fatores associados. J Bras Psiquiatr. 2010;59:17-23.
-
53Gavioli MdA, Silva AG, Gonçalves RJ, Santos ME, Shi KL, Lima MCP. Formando grupos no internato: critérios de escolha, satisfação e sofrimento psíquico. Rev Bras Educ Med. 2009;33:4-9.
-
54Hidalgo MP, Caumo W. Sleep disturbances associated with minor psychiatric disorders in medical students. Neurol Sci. 2002;23:35-9.
-
55Hirata FC, Lima MC, de Bruin VM, Nobrega PR, Wenceslau GP, de Bruin PF. Depression in medical school: the influence of morningness-eveningness. Chronobiol Int. 2007;24:939-46.
-
56Leao PB, Martins LA, Menezes PR, Bellodi PL. Well-being and help-seeking: an exploratory study among final-year medical students. Rev Assoc Med Bras (1992). 2011;57:379-86.
-
57Lima MC, Domingues Mde S, Cerqueira AT. [Prevalence and risk factors of common mental disorders among medical students]. Rev Saude Publica. 2006;40:1035-41.
-
58Loayza H MP, Ponte TS, Carvalho CG, Pedrotti MR, Nunes PV, Souza CM, et al. Association between mental health screening by self-report questionnaire and insomnia in medical students. Arq Neuropsiquiatr. 2001;59:180-5.
-
59Macedo PNAG, Nardotto LL, Dieckmann LHJ, Ferreira YD, Macedo BAG, dos Santos MAP, et al. Factors associated with depressive symptoms in a sample of Brazilian medical students. Rev Bras Educ Med. 2009;33:595-604.
-
60Moro A, Valle JBd, Lima LPd. Sintomas depressivos nos estudantes de medicina da Universidade da Região de Joinville (SC). Rev Bras Educ Med. 2005;29:97-102.
-
61Nicoli MG, Junior RD. Binge eating disorder and body image perception among university students. Eat Behav. 2011;12:284-8.
-
62Pagnin D, de Queiroz V, Carvalho YT, Dutra AS, Amaral MB, Queiroz TT. The relation between burnout and sleep disorders in medical students. Acad Psychiatry. 2014;38:438-44.
-
63Pagnin D, de Queiroz V. Influence of burnout and sleep difficulties on the quality of life among medical students. Springerplus. 2015;4:676.
-
64Paro HB, Morales NM, Silva CH, Rezende CH, Pinto RM, Morales RR, et al. Health-related quality of life of medical students. Med Educ. 2010;44:227-35.
-
65de Paula JdA, Borges AMFS, Bezerra LRA, Parente HV, de Paula RCdA, Wajnsztejn R, et al. Prevalência e fatores associados à depressão em estudantes de medicina. Rev Bras Crescimento Desenvolv Hum. 2014;24:274-81.
-
66Rique GL, Fernandes Filho GM, Ferreira AD, de Sousa-Munoz RL. Relationship between chronotype and quality of sleep in medical students at the Federal University of Paraiba, Brazil. Sleep Sci. 2014;7:96-102.
-
67Rocha ES, Sassi AP. Transtornos mentais menores entre estudantes de medicina. Rev Bras Educ Med. 2013;37:210-6.
-
68de Abreu Santos AT, Grosseman S, de Oliva Costa EF, de Andrade TM. Burnout syndrome among internship medical students. Med Educ. 2011;45:1146.
-
69Serra RD, Mattos e Dinato SL, Caseiro MM. Prevalence of depressive and anxiety symptoms in medical students in the city of Santos. J Bras Psiquiatr. 2015;64:213-20.
-
70Silva AG, Cerqueira AT, Lima MC. Social support and common mental disorder among medical students. Rev Bras Epidemiol. 2014;17:229-42.
-
71Silveira Rda R, Lejderman B, Ferreira PE, Rocha GM. Patterns of non-medical use of methylphenidate among 5th and 6th year students in a medical school in southern Brazil. Trends in Psychiatry Psychother. 2014;36:101-6.
-
72Souza FGdMe, Menezes MdGC. Estresse nos estudantes de medicina da Universidade Federal do Ceará. Rev Bras Educ Med. 2005;29:91-6.
-
73Tabalipa FdO, Souza MFd, Pfützenreuter G, Lima VC, Traebert E, Traebert J. Prevalence of anxiety and depression among medical students. Rev Bras Educ Med. 2015;39:388-94.
-
74Tempski P, Santos IS, Mayer FB, Enns SC, Perotta B, Paro HB, et al. Relationship among medical student resilience, educational environment and quality of life. PLoS One. 2015;10:e0131535.
-
75Torres AR, Cruz BL, Vicentini HC, Lima MC, Ramos-Cerqueira AT. Obsessive-compulsive symptoms in medical students: prevalence, severity, and correlates. Acad Psychiatry. 2016;40:46-54.
-
76Vasconcelos TCd, Dias BRT, Andrade LR, Melo GF, Barbosa L, Souza E. Prevalência de sintomas de ansiedade e depressão em estudantes de medicina. Rev Bras Educ Med. 2015;39:135-42.
-
77Volcan SM, Sousa PL, Mari Jde J, Horta BL. [Relationship between spiritual well-being and minor psychiatric disorders: a cross-sectional study]. Rev Saude Publica. 2003;37:440-5.
-
78Amorim AVC, Kikko EO, Abrantes MM, Andrade VLâ. álcool e alcoolismo: estudo de prevalência entre discentes do curso de Medicina da UNIFENAS em Belo Horizonte - Minas Gerais. Rev Med Minas Gerais. 2008;18:16-23.
-
79Baldisserotto CM, Filho ES, Nedel F, Sakae TM. Problemas psiquiátricos menores e indicadores do uso problemático de álcool entre os estudantes de medicina da Universidade do Sul de Santa Catarina - UNISUL. ACM Arq Catarin Med. 2005;34:73-9.
-
80Bassols AM, Rodrigues GS, Seeger GM, Eizirik CL, Sordi AO, Reche M. A prevalência de estresse em uma amostra de estudantes do curso de medicina da Universidade Federal do Rio Grande do Sul. Rev HCPA. 2008;28:153-7.
-
81Bruch TP, Jornada LK, Carneiro EA. Presença de sintomas psiquiátricos em estudantes de medicina de Universidade do sul do Brasil. ACM Arq Catarin Med. 2009;38:61-5.
-
82Furtado ES, Falcone EMO, Clark C. Avaliação do estresse e das habilidades sociais na experiência acadêmica de estudantes de medicina de uma universidade do Rio de Janeiro. Interacao Psicol. 2003;7:43-51.
-
83Guimarães KBS. Estresse e a formação médica: implicações na saúde mental dos estudantes [thesis]. São Paulo: UNESP de Assis; 2005.
-
84Porcu M, Fritzen CV, Helber C. Sintomas depressivos nos estudantes de medicina da Universidade Estadual de Maringá [Internet]. [cited 2017 Apr 26]. www2.unifesp.br/dpsiq/polbr/ppm/original5_01.htm
» www2.unifesp.br/dpsiq/polbr/ppm/original5_01.htm -
85Souza L. Prevalência de sintomas depressivos, ansiosos e estresse em acadêmicos de medicina [dissertation]. São Paulo: Universidade de São Paulo; 2010.
-
86Vallilo NG, Danzi R Jr, Hübner CvK, Novo NF, Gobbo R. Prevalence of depressive symptoms in medical students. Rev Soc Bras Clin Med. 2011;9:36-41.
-
87Gonçalves DM, Stein AT, Kapczinski F. [Performance of the self-reporting questionnaire as a psychiatric screening questionnaire: a comparative study with structured clinical interview for DSM-IV-TR]. Cad Saude Publica. 2008;24:380-90.
-
88Mata DA, Ramos MA, Bansal N, Khan R, Guille C, Di Angelantonio E, et al. Prevalence of depression and depressive symptoms among resident physicians: a systematic review and meta-analysis. JAMA. 2015;314:2373-83.
-
89Ishak WW, Lederer S, Mandili C, Nikravesh R, Seligman L, Vasa M, et al. Burnout during residency training: a literature review. J Grad Med Educ. 2009;1:236-42.
-
90Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger state-trait anxiety inventory (STAI). Br J Clin Psychol. 1992;31:301-6.
-
91Wolf TM. Stress, coping and health: enhancing well-being during medical school. Med Educ. 1994;28:8-17; discussion 55-7.
-
92Lux V, Aggen SH, Kendler KS. The DSM-IV definition of severity of major depression: inter-relationship and validity. Psychol Med. 2010;40:1691-701.
-
93Smarr KL, Keefer AL. Measures of depression and depressive symptoms: Beck Depression Inventory-II (BDI-II), Center for Epidemiologic Studies Depression Scale (CES-D), Geriatric Depression Scale (GDS), Hospital Anxiety and Depression Scale (HADS), and Patient Health Questionnaire-9 (PHQ-9). Arthritis Care Res (Hoboken). 2011;63:S454-66.
-
94American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV). Arlington: American Psychiatric Publishing; 1994.
-
95Ayuso-Mateos JL, Nuevo R, Verdes E, Naidoo N, Chatterji S. From depressive symptoms to depressive disorders: the relevance of thresholds. Br J Psychiatry. 2010;196:365-71.
-
96Parikh SV, Segal ZV, Grigoriadis S, Ravindran AV, Kennedy SH, Lam RW, et al. Canadian Network for Mood and Anxiety Treatments (CANMAT) clinical guidelines for the management of major depressive disorder in adults. II. Psychotherapy alone or in combination with antidepressant medication. J Affect Disord. 2009;117:S15-25.
-
97Andrade LH, Wang YP, Andreoni S, Silveira CM, Alexandrino-Silva C, Siu ER, et al. Mental disorders in megacities: findings from the São Paulo megacity mental health survey, Brazil. PLoS One. 2012;7:e31879.
-
98Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R). JAMA. 2003;289:3095-105.
-
99Wasson LT, Cusmano A, Meli L, Louh I, Falzon L, Hampsey M, et al. Association between learning environment interventions and medical student well-being: a systematic review. JAMA. 2016;316:2237-52.
-
100Buckley S, Coleman J, Davison I, Khan KS, Zamora J, Malick S, et al. The educational effects of portfolios on undergraduate student learning: a Best Evidence Medical Education (BEME) systematic review. BEME Guide No. 11. Med Teach. 2009;31:282-98.
-
101Sharma R, Jain A, Gupta N, Garg S, Batta M, Dhir SK. Impact of self-assessment by students on their learning. Int J Appl Basic Med Res. 2016;6:226-9.
-
102Kalén S, Ponzer S, Seeberger A, Kiessling A, Silén C. Longitudinal mentorship to support the development of medical students’ future professional role: a qualitative study. BMC Med Educ. 2015;15:97.
Publication Dates
-
Publication in this collection
31 Aug 2017 -
Date of issue
Oct-Dec 2017
History
-
Received
10 Jan 2017 -
Accepted
25 Mar 2017