Abstracts
PURPOSE: To describe the results obtained in a newborn hearing screening program in the city of Cuiabá (MT), Brazil, in the period from 2009 to 2010. METHODS: We analyzed the otoacoustic emissions results of 1964 low-risk and 123 high-risk newborns, archived in the computer of the service, regarding the amount of those who passed or failed the screening. RESULTS: In the low-risk group, 94.5% passed, 1.2% failed and 4.3% did not return for re-test. In the high-risk group, 71.54% passed, 3.2% failed and 25.4% did not return for re-test. CONCLUSION: The results obtained by the program are in agreement with the expectations of international and national institutions.
Screening; Neonatal screening; Hearing loss; Hearing; Infant, newborn
OBJETIVO: Descrever os resultados obtidos em um programa de triagem auditiva neonatal, localizado na cidade de Cuiabá (MT) no período de 2009 a 2010. MÉTODOS: Foram analisados os exames de emissões otoacústicas de 1964 recém-nascidos de baixo risco e de 123 recém-nascidos de alto risco, arquivados no computador do serviço, em relação à quantidade dos que passaram ou falharam na triagem. RESULTADOS: No grupo de baixo risco 94,5% dos sujeitos passaram; 1,2% falharam e 4,3% não retornaram para o reteste. No grupo de alto risco, 71,54% passaram; 3,2% falharam e 25,4% não retornaram para o reteste. CONCLUSÃO: Os resultados obtidos pelo programa estão de acordo com as expectativas de órgãos internacionais e nacionais.
Triagem; Triagem neonatal; Perda auditiva; Audição; Recém-nascido
ORIGINAL ARTICLE
IGraduate Program (Doctorate degree) in Human Communication, Department of Physical Therapy, Speech-Language Pathology and Audiology, and Occupational Therapy, School of Medicine, Universidade de São Paulo - USP - São Paulo (SP), Brazil; Centro de Diagnóstico Auditivo de Cuiabá - CEDAC - Cuiabá (MT), Brazil
IIFundação Getúlio Vargas - FGV - Cuiabá (MT), Brazil
IIIDepartment of Pediatric Dentistry, Orthodontics, and Public Health, Bauru School of Dentistry, Universidade de São Paulo - USP - Bauru (SP), Brazil
IVDepartment of Physical Therapy, Speech-Language Pathology and Audiology, and Occupational Therapy, School of Medicine, Universidade de São Paulo - USP - São Paulo (SP), Brazil
Correspondence address
ABSTRACT
PURPOSE: To describe the results obtained in a newborn hearing screening program in the city of Cuiabá (MT), Brazil, in the period from 2009 to 2010.
METHODS: We analyzed the otoacoustic emissions results of 1964 low-risk and 123 high-risk newborns, archived in the computer of the service, regarding the amount of those who passed or failed the screening.
RESULTS: In the low-risk group, 94.5% passed, 1.2% failed and 4.3% did not return for re-test. In the high-risk group, 71.54% passed, 3.2% failed and 25.4% did not return for re-test.
CONCLUSION: The results obtained by the program are in agreement with the expectations of international and national institutions.
Keywords: Screening; Neonatal screening; Hearing loss; Hearing; Infant, newborn
INTRODUCTION
Newborn hearing screening programs are important because it aims early detection of hearing impairment and are viable due to the low cost and ease of execution under training and supervision(1).
There are several objective and subjective methods to assess the integrity of the auditory system in newborns (NB), both containing clinical advantages and disadvantages.
The otoacoustic emissions (OAE) test is an objective assessment of the peripheral auditory system pre-neural, which has the advantage of being a fast, noninvasive, easy to interpret and has high specificity and sensitivity, that observe the responses from the cochlea without depend on neurological conditions of the newborn(2).
The OAE are a type of acoustic energy generated by the contraction of the outer hair cells in the cochlear active mechanism that spread to the middle ear and external auditory canal, where they can be captured(3).
Since 1998, with the creation of support group for newborn hearing screening, several programs were implemented in the country, and currently there is a need to confirm the principles and the references to monitor the effectiveness of programs for universal newborn hearing screening(4).
At the moment, records were not notified of publications on the subject in the state of Mato Grosso, Brazil. Thus, this study aimed to examine whether the results obtained in a newborn hearing screening program in the city of Cuiabá (MT), Brasil, are consistent with the expectation of the international and national institutions.
METHODS
The research was initially approved by the Research Ethics Committee of the Julio Müller University Hospital of the Universidade Federal de Mato Grosso (UFMT) under number 735/CEP-HUJM/09, and used the database of the Centro de Diagnóstico Auditivo de Cuiabá (CEDAC), authorized by the participants and the institution. It was conducted a retrospective study, which analyzed the tests done from July 2009 to October 2010 in a newborn hearing screening service in the private sector of the city of Cuiabá (MT), Brazil.
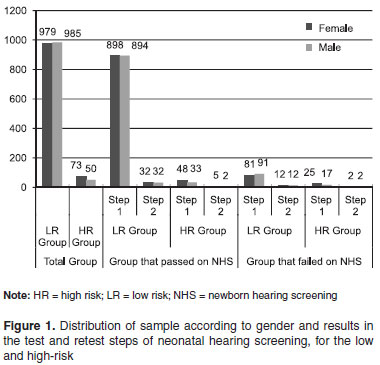
Data were collected from newborns (NB) who were submitted to hearing screening through the capture of transient otoacoustic emissions (TOAE), in order to analyze the functionality of the outer hair cells and rule out the possibility of hearing loss. The infants belonged to one of two groups: high or low risk for hearing loss. The low-risk group consisted of 1964 newborns and the high-risk group, of 123 newborns, totaling 2087 NB (1052 females and 1035 males). The risk criteria for hearing loss considered in this study were in accordance with that proposed by the Joint Comittee on Infant Hearing (JCIH)(5).
According to the Support Group for Universal Newborn Hearing Screening (GATANU), we considered as "passing" criterion in the screening the presence of responses greater than 6 dB in at least three frequency bands (frequencies tested were 1, 1.5, 2, 3 and 4 KHz) with reproducible response greater than 50%.
The protocol used in this study was suggested by GATANU(5), that is, infants of both groups were screened using TOAE (step 1) and, if they failed the test, they should return for a retest in 15-30 days (step 2). Those infants who failed after retest would be referred for diagnostic services for otorhinolaryngological evaluation, Brain Evoked Response Audiometry (BERA), tympanometry and behavioral assessment.
Were included in the sample tests of newborns under the age of three months. Data collection in the low-risk group was carried out outside the maternity hospital, when the family spontaneously sought the service to do the OAE, which was characterized as an optional newborn hearing screening (NHS); the high-risk NB were submitted to hearing screening at the intensive care unit (ICU) where they were admitted, and only the infants considered by the neonatologist as apt were evaluated. The high-risk group was assessed once a week, which explains the lower number of participants in this group.
Data collection was carried out through the analysis of the results stored in the computer of a private service in the city of Cuiabá (MT), Brazil. In addition to analyzing the results of TOAE, their correlations with age and gender were also analyzed.
The equipment used for data collection of the OAE was from Biologic®, Model 480 NAVPRO.
The results were descriptively analyzed by calculating the mean, median, minimum, maximum and standard deviation. To compare the high- and low-risk groups, as well as genders, it was used the Chi-square test, considering a significance level of 5%.
RESULTS
In the low-risk group 1792 NB (91.24%) passed the NHS, and 172 (8.76%) failed. After the retest these indexes changed to 1856 (94.50%) of "pass" and 24 (1.22%) of "fail", and 84 (4.28%) of the infants did not return to the service for completion of the hearing screening.
In the high-risk group, 81 NB (65.85%) passed the NHS and 42 (34.15%) failed. After retest, these ratios changed to 88 (71.54%) "pass" and four (3.25%) "fail", and 31 (25.21%) of the infants did not return to the service for completion of the hearing screening.
Figure 1 shows the sample distribution according to gender, and the result of the test and retest steps of the newborn hearing screening, for both low- and high-risk groups.
Descriptive statistical analysis of the age (in days) of the infants at the time of hearing screening can be found in Table 1.
The inferential analysis comparing the number of infants who passed and failed in steps 1 and 2 of the NHS between the low- and high-risk groups showed that there was a significant difference (p<0.001), with a greater number of NB that passed the screening in the low-risk group.
There was no difference between the responses observed according to the variable gender in the group of infants who passed or in the groups who failed, both in high- and low-risk groups, in steps 1 and 2 of the NHS (Table 2).
DISCUSSION
In this study we can observe a higher failure rate in the NHS for the high-risk group, when compared to the low-risk group, and this difference was significant. This finding may be explained by risk factors for hearing loss that permeate the lives of these infants, as well as several events during the test, such as environmental noise, noisy breathing or noise of oxygen equipment that in some cases cannot be removed during the test(6).
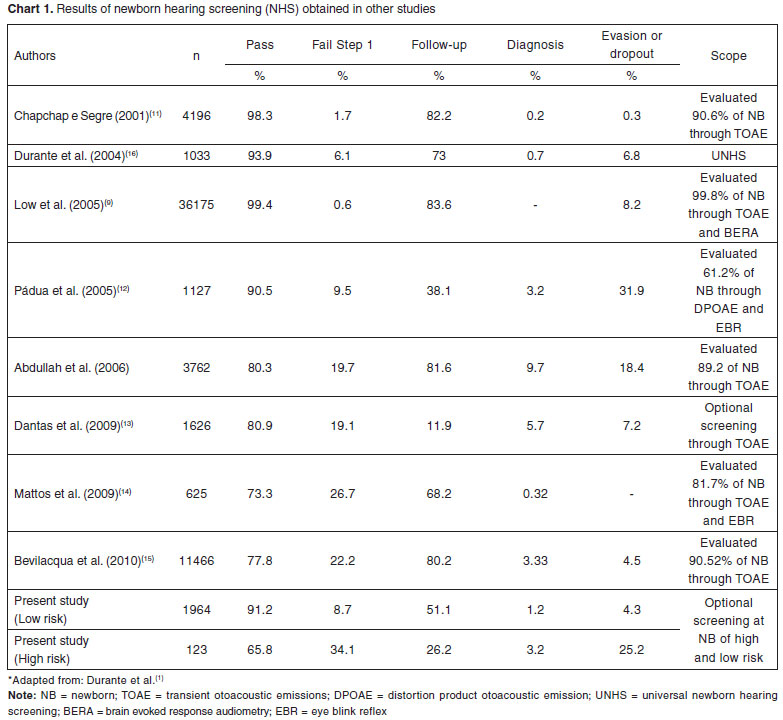
The indexes of "pass"/"failure" in the NHS for high- and low-risk groups are in accordance to the recommendations of international and national institutions(4,5), namely values lower than 4%. International and national studies(7-15) differ as to the results found in the various stages, from screening to diagnosis (Chart 1). These differences may be due to the different protocols used, which influences the specificity and sensitivity of screening or even socio-economic differences between countries that performed each study.
It also stands out the significant values found in relation to the dropout rates or abandonment in both groups. Similar data can be found in other national and international studies(16-18). The importance of the NHS should be more widely promoted both for patients and health professionals, especially pediatricians, who deal with these infants and should encourage the return to service for completing the NHS. This finding corroborates other studies(12,19-23).
It is important to note the need for information regarding the importance of early diagnosis of deafness, as well as the methods used to carry them out to the health professionals involved in the pre and post pregnancy, as well as to the patients(24-25). This fact can be explained by failures in the process of professional education, lack of interest or downgrade of them.
Other factors that may be related to the evasion of the existing services at the NHS are: low attendance at prenatal care, more than one child in the family, lack of partner and family support to assist in displacement and low maternal education(22). It is suggested, therefore, that future studies can clarify these factors.
On the world stage, the NHS has been performed and despite the barriers encountered, still being carried out and perfected in accordance with the possibilities of each place(26).
In Brazil, there was a great advance in public policies with the creation of National Policy of Hearing Care by Decree GM/MS No. 2073 of 09.28.2004 and the Law of the National Newborn Hearing Screening No. 12303 of 02/08/2010, in order to effect the early detection of deafness and support to individuals with hearing impairment, which should be widely publicized and enforced by society.
Developed countries and countries in development has common barriers to implant the NHS such as: lack of suitable environment for testing, few qualified professionals available to perform the NHS on the weekends, lack of sector monitoring and rehabilitating hearing impaired people, and lack of information about the benefits of early detection of deafness(27).
There was variability in the distribution of genres in both the total sample and among those who passed and failed in both low- and high-risk groups, and it was not observed a significant tendency of results related to gender, except in the high-risk group in step 2, in which there was a predominance of female infants among those who passed. We found no studies that prove the prevalence of hearing loss related to gender, it is known that individuals females have a higher number of outer hair cells and the presence of a higher prevalence of spontaneous otoacoustic emissions (SOAE)(28).
The mean age was higher in the low-risk group, because this was seen outside the maternity unlike the high risk newborns that were assessed in maternity, reinforcing the idea that the NHS should be performed, preferably before discharge hospital, aimed at early detection of hearing impairment. When comparing studies that were evaluated universal NHS and optional NHS, it can be seen the precocity evaluations of universal programs, but in the rate of avoidance of these studies, we find great variability of results, it is not possible to make a determination directly proportional between the dropout index of the programs and type of screening program(12,13,16,19,20,29-30). This study was conducted with the population assessed at a private service and therefore belong to a middle socioeconomic level. The possibility that economically disadvantaged groups would be greater failure rate in the NHS, thought in the beginning was not sustained; when comparing studies performed in private clinics(13,29) with others conducted in public places(11,15,19,28), we cannot establish a direct relationship between socioeconomic level and failure rate at the NHS, because the values were varied between groups.
Finally, we highlight the need to use an information system for data management services for the NHS to be possible to obtain the national prevalence of hearing loss and to establish, then, the epidemiological profile of the country(30).
To improve the NHS program in question, it is proposed greater integration of the health team that serves the NB through active search among professionals, in order to decrease the dropout rate of children and that they are accompanied by the diagnosis, fitting and rehabilitation, if necessary.
CONCLUSION
We conclude therefore that the results obtained by the program are consistent with the expectation of the international and national institutions and contributes to a multicenter study in Brazil. We emphasize the importance of active accompaniment of patients during the screening, to avoid large dropout rate at this stage.
REFERENCES
- 1. Durante AS, Carvallo, RM, Costa, MT, Cianciarullo MA, Voegels RL. Triagem auditiva neonatal: justificativa, possível e necessária. Rev Bras Otorrinolaringol. 2003;69(2):11-8.
- 2. Write KR, Vohr BR, Behrens R. Universal newborn hearing screening using transient evoked otoacoustic emissions: results by the Rhode Island Hearing Assessment Project. Semin Hear. 1993;14:18-29.
- 3. Kemp DT, Ryan S. Otoacoustic emission tests in neonatal screening programes. Acta Otolaryngol Suppl. 1991;482:73-84.
-
4Grupo de Apoio a Triagem Auditiva Neonatal Universal - GATANU [homepage na Internet]. 2009 [citado 2009 Dez 10]. Disponível em http://www.gatanu.org
» link - 5. Joint Committee on Infant Hearing. Year 2000 position statement: principles and guidelines for early hearing detection and intervention programs [Internet]. 2000 [cited 2010 Jan 18]. Available from: http://www.jcih.org/jcih2000.pdf
- 6. Bonfils P, Uziel A, Pujol R. Screening for auditory dysfunction in infants by evoked oto-acoustic emissions. Arch Otolaryngol Head Neck Surg. 1988;114(8):887-90.
- 7. Widen JE, Bull RW, Folsom RC. Newborn hearing screening: what it means for providers of early intervention services. Infants Young Child. 2003;16(3):249-57.
- 8. Lin CY, Huang CY, Lin CY, Lin YH, Wu JL. Community-based newborn hearing screening program in Taiwan. Int J Pediatr Otorhinolaryngol. 2004;68(2):185-9.
- 9. Low WK, Pang KY, Ho LY, Lim SB, Joseph R. Universal newborn hearing screening in Singapore: the need, implementation and challenges. Ann Acad Med Singapore. 2005;34(4):300-6.
- 10. Abdullah A, Hazim MY, Almyzan A, Jamilah AG, Roslin S, Ann MT, et al. Newborn hearing screening: experience in a Malasyan hospital. Singapore Med J. 2006;47(1):60-4.
- 11. Chapchap MJ, Segre CM. Universal newborn hearing screening and transient evoked otoacoustic emission: new concepts in Brazil. Scand Audiol Suppl. 2001;(53):33-6.
- 12. Pádua FG, Marone S, Bento RF, Carvallo RM, Durante AS, Soares JC, et al. Triagem auditiva neonatal: um desafio para sua implantação. Arq Int Otorrinolaringol. 2005;9(3):190-4.
- 13. Dantas MB, Anjos CA, Camboim ED, Pimentel MC. Resultados de um programa de triagem auditiva neonatal em Maceió. Rev Bras Otorrinolaringol. 2009;75(1):58-63.
- 14. Mattos WM, Cardoso LF, Bissani C, Pinheiro MM, Viveiros CM, Carreirão Filho W. Análise de implantação de programa de triagem auditiva neonatal em um hospital universitário. Rev Bras Otorrinolaringol. 2009;75(2):237-44.
- 15. Bevilacqua MC, Alvarenga KF, Costa OA, Moret AL. The universal newborn hearing screening in Brazil: from identification to intervention. Int J Pediatr Otorhinolaryngol. 2010;74(5):510-5.
- 16. Durante AS, Carvallo RM, Costa MT, Cianciarullo MA, Voegels RL, Takahashi GM, et al. Programa de triagem auditiva neonatal: modelo de implementação. Arq Int Otorrinolagingol. 2004;8(1):56-62.
- 17. Spivak L, Dalzell L, Berg A, Bradley M, Cacace A, Campbell D, et al. New York state universal newborn hearing screening demonstration project: inpatient outcome measures. Ear Hear. 2000;21(2):92-103.
- 18. Rouev P, Mumdzhiev H, Spiridonova J, Dimov P. Universal newborn hearing screening program in Bulgaria. Int J Pediatr Otorhinolaryngol. 2004;68(6):805-10.
- 19. Oliveira MC, Tavares TS. Programa de triagem auditiva neonatal do hospital naval Marcilio Dias. Arq Bras Med Naval. 2004;65(1):44-9.
- 20. Barreira-Nielsen C, Futuro Neto HA, Gattaz G. Processo de implantação de Programa de Saúde Auditiva em duas maternidades públicas. Rev Soc Bras Fonoaudiol. 2007;12(2):99-105.
- 21. Tiensoli LO, Goulart LM, Resende LM, Colosimo EA. Triagem auditiva em hospital público de Belo Horizonte, Minas Gerais, Brasil: deficiência auditiva e seus fatores de risco em neonatos e lactentes. Cad Saúde Pública. 2007;23(6):1431-41.
- 22. Fernandes JC, Nozawa MR. Estudo da efetividade de um programa de triagem auditiva neonatal universal. Ciênc Saúde Coletiva. 2010;15(2):353-61.
- 23. Soares CP, Marques LR, Flores NG. Triagem audidiva neonatal: aplicabilidade clínica na rotina dos médicos pediatras neonatologistas. Rev CEFAC. 2008;10(1):110-6.
- 24. Tochetto TM, Petry T, Pedroso FS, Gonçalves MS, Silva ML. Sentimentos manifestados por mães frente à triagem auditva neonatal. Rev CEFAC. 2008;10(4):566-71.
- 25. Hilú MR, Zeigelboim BS. O conhecimento, a valorização da triagem auditiva neonatal e a intervenção precoce da perda auditiva. Rev CEFAC. 2007;9(4):563-70.
- 26. Aurélio FS, Tochetto TM. Triagem auditiva neonatal: experiências de diferentes países. Arq Int Otorrinolaringol. 2010;14(3):355-63.
- 27. Kennedy C, McCann D. Universal neonatal hearing screening moving from evidence to practice. Arch Dis Child Fetal Neonatal Ed. 2004;89(5):F378-83.
- 28. Wright A, Davis A, Bredberg G, Ulehlová L, Spencer H, Bock G, et al. Hair cell distributions in the normal human cochlea. A report of a European working group. Acta Otolaryngol Suppl. 1987;436:15-24.
- 29. Hanna KF, Maia RA. Triagem auditiva neonatal: Incidência de deficiência auditiva neonatal sob a perspectiva da nova legislação paulista. Rev Bras Saúde Matern Infant. 2010;10(2):257-64.
- 30. Stumpf CC, Gambini C, Jacob-Corteletti LC, Roggia SM. Triagem auditiva neonatal: um estudo na cidade de Curitiba-PR. Rev CEFAC. 2009;11(3):478-85.
Results of a newborn hearing screening program in Cuiabá - Mato Grosso, Brazil
Publication Dates
-
Publication in this collection
24 Jan 2012 -
Date of issue
Dec 2011
History
-
Received
09 Dec 2010 -
Accepted
21 Dec 2010