Abstracts
INTRODUCTION: Hyperaggregation of platelets can cause the formation of thrombi and subsequent occlusion of blood vessels leading to ischemia. This phenomenon can be responsible for ischemic cardiovascular diseases such as angina pectoris and atherosclerosis as well as other forms of ischemia such as stroke. To decrease platelet function and reduce the formation of thrombi, acetylsalicylic acid has been used for antithrombotic treatment, with several studies showing its effectiveness. Therefore it is necessary to use a laboratory tool to monitor the effectiveness of treatment, which is achieved through laboratory testing of platelet aggregation. The aim of this study was to compare two different methods (impedance and turbidimetry) to test platelet aggregation in 30 adult patients of both genders taking acetylsalicylic acid. CONCLUSION: The results show that there is a good correlation between these two methods and so both these techniques can be used in the clinical routine.
Platelet aggregation; Aspirin; Nephelometry and turbidimetry; Electric impedance; Blood coagulation; Collagen; Heparin
INTRODUÇÃO: A hiperagregação (agregação excessiva) das plaquetas pode causar a formação de um trombo e a posterior oclusão dos vasos sanguíneos levando à isquemia. Esse fenômeno é responsável por doenças isquêmicas cardiovasculares, como angina pectoris e aterosclerose, bem como outras formas de isquemia, como o acidente vascular cerebral. Visando diminuir a função das plaquetas para reduzir a formação de trombos, o ácido acetilsalicílico vem sendo utilizado para tratamento antitrombótico, com diversos estudos mostrando sua eficácia. Dessa forma faz-se mister o uso de uma ferramenta laboratorial para o monitoramento da efetividade do tratamento, o que é feito por meio do teste de agregação plaquetária. O objetivo desse estudo foi comparar duas metodologias para esse exame (impedância elétrica e turbidimetria) em relação a trinta pacientes adultos de ambos os sexos em uso do fármaco. CONCLUSÃO: Os resultados mostraram uma boa correlação entre os métodos, possibilitando o uso concomitante de ambas as técnicas em laboratórios clínicos de rotina.
Agregação plaquetária; Aspirina; Nefelometria e turbidimetria; Impedância elétrica; Coagulação sanguinea; Colágeno; Heparina
ARTICLE
IMedical School, Universidade de São Paulo - USP, São Paulo (SP), Brazil
IIHematology Service, Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo - USP, São Paulo (SP), Brazil
Correspondence
ABSTRACT
INTRODUCTION: Hyperaggregation of platelets can cause the formation of thrombi and subsequent occlusion of blood vessels leading to ischemia. This phenomenon can be responsible for ischemic cardiovascular diseases such as angina pectoris, atherosclerosis, stroke and other forms of ischemia. To decrease platelet function and reduce the formation of thrombi, acetylsalicylic acid has been used for antithrombotic treatment, with several studies showing its effectiveness. Therefore it is necessary to use a laboratory tool to monitor the effectiveness of treatment, which is achieved through laboratory testing of platelet aggregation.
METHOD: Two different examinations (impedance and turbidimetry) were compared in 30 adult patients of both genders taking acetylsalicylic acid.
CONCLUSION: The results show that there is a good correlation between these two methods and so both these techniques can be used in the clinical routine.
Keywords: Platelet aggregation; Aspirin; Nephelometry and turbidimetry; Electric impedance; Blood coagulation; Collagen/pharmacology; Heparin/pharmacology
Introduction
The adhesion of platelets to the blood vessel wall and subsequent aggregation are crucial events in both hemorrhages and thrombosis. Hyperaggregation, that is, excessive aggregation, of platelets can cause the formation of thrombi and subsequent occlusion of blood vessels leading to ischemia. Arterial occlusion by platelet thrombi is often independent of platelet hyperaggregation as there is an injury to the vascular wall on which platelet adhesion and aggregation occurs; these are normal functions of platelets. However, this phenomenon can also be responsible for cardiovascular ischemic diseases such as angina pectoris, atherosclerosis, ischemic stroke, among other forms of ischemia.(1)
Antiplatelet therapy with acetylsalicylic acid (ASA) reduces the risk of nonfatal myocardial infarctions, strokes or deaths from vascular causes by 25% in high-risk patients regardless of gender, age or the presence of hypertension or diabetes mellitus. (2)
Several studies have shown that aspirin is an effective antithrombotic agent when used regularly in doses ranging from 50 to 100 mg per day. Higher doses (300-1200 mg daily) showed no difference in efficacy when compared to lower doses.(3,4) The use of low doses of aspirin (50-100 mg/day) is the most appropriate strategy to maximize AAS efficiency and reduce its adverse effects.(3)
A common laboratory exam utilized to monitor the effect of aspirin therapy is platelet aggregation by turbidimetry. This technique measures platelet function by optical changes in platelet-rich plasma upon stimulation by certain agonists such as adenosine diphosphate (ADP), epinephrine, collagen and arachidonic acid.(5) An alternative method to study the function of platelets is platelet aggregation by electrical impedance in whole blood (whole blood impedance aggregometry). Here an electrode is inserted into a citrated whole blood sample to measure variations in electrical resistance as platelets adhere to it and aggregate due to the action of stimulating agents.(6)
The opinions of authors differ on which is the better of these two techniques to measure the effect of aspirin therapy and also which is the best aggregating agent for more reliable monitoring of treatment. Arachidonic acid has been used to define monitoring as it promotes some in vitro aggregation of platelets even when ASA is administered at low doses to patients, but it remains unclear whether this is the best aggregating agent in this case and whether aggregation by impedance aggregometry is better than the traditional method that is widely used in all laboratories turbidimetry.(1,7-9)
Thus, the aim of this study was to compare the turbidimetric method of platelet aggregation with whole blood impedance aggregometry in patients under aspirin therapy.
Methods
Blood was collected from thirty normal healthy adult donors of both genders who had not used aspirin for at least ten days prior to donation (Control Group). Blood was also collected from thirty adult patients of both genders who regularly take aspirin. None of the participants had histories of anemia or other blood diseases. The samples of both groups were processed by the two methods as follows:
Aggregation by turbidimetry or platelet-rich plasma
The turbidimetry method is based on promoting the aggregation of platelets in platelet-rich plasma (PRP) using several agonists (arachidonic acid, ADP and collagen). The resulting aggregation is measured as the optical density of PRP decreases when platelets aggregate. The intensity and speed of this decrease is highly related to and dependent on platelet function. Optical density here is monitored using the Chronolog model 540 aggregometry apparatus with a photometer connected to a recorder.
The PRP was obtained after the collected blood samples were centrifuged for ten minutes at 1000 rpm, leaving the platelet count of this plasma, determined in a Neubauer chamber, at approximately 250,000 cells/mL. Aggregation in the PRP was achieved by adding the following aggregating agents at concentrations reported in the literature: 1 µM arachidonic acid, 2 µg/mL Collagen and 0.75 µM and 7.5 µM ADP.
Aggregation by whole blood impedance aggregometry
This method is based on platelet aggregation in citrated whole blood due to the action of the same aforementioned agonistic agents, but at different concentrations according to the literature (0.5µMArachidonic acid, 1.25 µg/mL Collagen, and 5 µM and 10 µM ADP).
The whole blood was diluted at 1:1 with saline solution giving a total of 1 mL of diluted blood, which acts to reduce resistance of electric current in the system. After placing the platinum electrode in the solution it is necessary to wait for the system to stabilize, before the addition of the aforementioned agonists. Platelet aggregation is measured by impedance (electrical resistance). As the platelets aggregate, the electrical resistance increases. Similar to turbidimetry, this increase, which is displayed as a curve by the Agrolink® software of the Chrono-log model 540 aggregometry apparatus, is proportional to platelet function.
Interpretation of the results
There is a difference in views concerning the interpretation of results of turbidimetric platelet aggregation. Some services and authors advocate the interpretation of results based on the final amplitude of aggregation curve expressed as a percentage of light transmittance, as well as grading the curve as low, normal or high aggregation or in relation to established ranges. Other services and authors prefer to interpret the results based on the structure or morphology of the aggregation curve taking into account the formation of the first and second waves, the presence or absence of platelet disaggregation (reduction in the transmittance rate after the initial aggregation) in view of the stages of the functional process of platelets (receptor activation/release of granules). Thus, the curve will be characterized as low, normal or high aggregation. In this work both forms of interpretation of turbidimetric platelet aggregation were employed numerical and descriptive for the evaluation of our results.(10)
Results
Table 1 shows the results of platelet aggregation by impedance aggregometry in the normal control population, where the lower limit corresponds to the mean -2 standard deviations (SD) and the upper limit corresponds to the mean +2 SD.(11,12)
Table 2 shows the results of platelet aggregation by the turbidimetric method in the normal population using different agonists.
The results described above define the normal values for the control population with the normal ranges being defined as between the lower to upper limits.
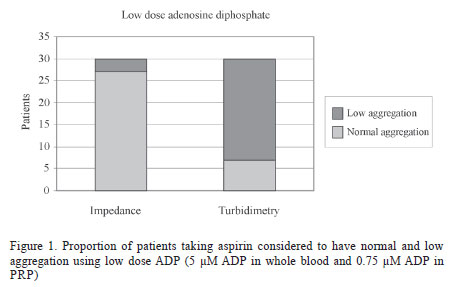
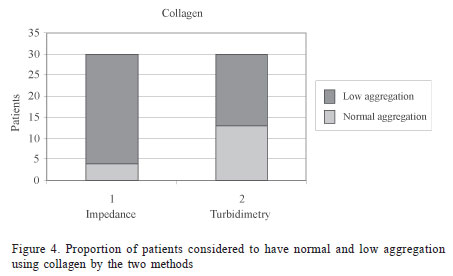
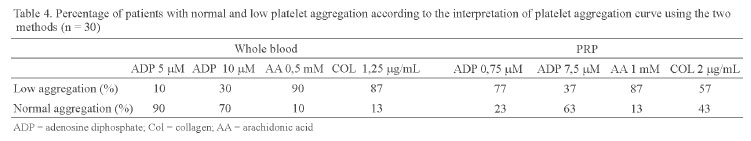
The total numbers of patients with low and normal aggregation were calculated from the maximum amplitude on the curve of the platelet aggregation graph (Tables 3 & 4).
Table 4 shows that in whole blood (impedance aggregometry), 10% of the total number of samples was characterized as low aggregation with 5 µM ADP, 30% with 10 µM ADP, 87% with 1.25 µg/dL collagen and 90% with 0.5µM arachidonic acid. Similarly in turbidimetry (PRP), 77% of samples was characterized as low aggregation with 0.75 µM ADP, 37% with 7.5 µM ADP, 57% with 2 µg/dL collagen and 87% with 1 µM arachidonic acid.
A statistically significant difference (p < 0.05) was demonstrated for the proportion of low aggregation samples between 5 µM ADP impedance aggregometry (3 samples) and 0.75 µM ADP turbidimetry (23 samples). However no statistically significant difference was demonstrated for the number of samples with low aggregation between 10 µM ADP impedance aggregometry (9 samples) and 7.5 µM ADP turbidimetry (11 samples).
Additionally, no statistically significant difference (p > 0.05) in the number of low aggregation samples was identified between the two methods using arachidonic acid (27 patients by impedance aggregometry and 26 patients by turbidimetry).
Classical concentrations of collagen are considered to be more sensitive in detecting cyclooxygenase (COX) inhibition by acetylsalicylic acid.(13) A significantly larger (p < 0.05) proportion of low aggregation samples were identified by impedance aggregometry (26 patients) than by turbidity (17 patients).
Discussion
With the increasing use of aspirin therapy to prevent thrombotic events, a laboratory test capable of monitoring the effectiveness of this therapy is necessary. This is important to define the degree of inhibition caused by aspirin and whether the effect of the aspirin is sufficient for the patient to be submitted to other clinical procedures.
For this, the most commonly employed test in the laboratory routine, with its aforementioned advantages and limitations, is platelet aggregation by turbidimetry. In this study we tested this method and compared it with impedance aggregometry.
Our results showed some similarities and differences between the two techniques in respect to the aggregating agents used.
The greatest divergence between the two methodologies was obtained with low-dose ADP with turbidimetry showing a significantly higher number of low aggregation samples (77%) compared to impedance aggregometry (10%). This result may be related to the low strength of the aggregating agent in whole blood, where we had normal results for the control group with maximum wave amplitudes starting at 1e (Figure 1).
With high-dose ADP the results of the two techniques were statistically similar. These results show that the high concentration of aggregating agent tends to distort or minimize the laboratorial effects of AAS, probably due to greater stimulation of purinergic receptors (Figure 2).
Additionally, no significant differences were seen between the results of the two methods using arachidonic acid showing that both were adequate to monitor the antiplatelet effect of aspirin. Both turbidimetry (87%) and impedance aggregometry
(90%) showed that many samples had low aggregation which is to be expected when patients are taking aspirin. These results suggest that the aggregating agent may be an important tool in the control of aspirin therapy, as with COX inhibition, arachidonic acid is not converted to thromboxane A2 (TXA2) (Figure 3).
With collagen, at doses used in conventional aspirin monitoring,(13) the impedance method identified a larger number of low aggregation samples (86.7%) than turbidimetry (57%). These results are in agreement with other authors, who demonstrated that impedance aggregometry was more sensitive (Figure 4).(10)
Similar to other authors this study demonstrated a high response to arachidonic acid in impedance aggregometry but it also showed a high response using the turbidimetry. This shows that this aggregating agent is really a strong indicator of the antiplatelet effect of aspirin in both methodologies. As the results of both techniques are similar both methodologies can be used in the laboratory practice.(7)
Impedance aggregometry can be used in laboratories to address some shortcomings of the traditional method; this technique requires smaller blood samples, which is extremely important in the elderly, obese, malnourished patients, children and newborns, for whom it is more difficult to collect blood.
It may also address other important aspects that interfere in platelet aggregation by turbidimetry such as hemolyzed, lipemic and icteric samples. These interferences are important causes of samples being rejected, a situation that can affect the clinical treatment of patients. By using impedance aggregometry, this interference is eliminated, thereby assisting the clinician.
Another advantage of platelet aggregation by impedance is related to the platelet count of the patient. Platelet aggregation by turbidimetry is not satisfactory using samples with counts below 90,000 platelets/mm3, while with impedance aggregometry this limit drops to 50,000 platelets/mm3.(14) This difference is of particular importance when it comes to testing patients with cancer, liver diseases or with other diseases that cause thrombocytopenia.
By using a medium more similar to in vivo conditions, platelet aggregation by impedance may have a greater influence to define results, as cellular elements important in the thrombus formation process are not lost. These cellular elements include the red blood cells, leukocytes with their chemotactic interactions, blood viscosity and highly reactive giant platelets, especially in inflammatory states, e.g. in cases of atherosclerotic plaque rupture.
As the time factor is of considerable importance in health for diagnosis and treatment, new monitoring methods are crucially important. This includes platelet aggregation by impedance; due to the shorter time required to perform the test, which is interesting both for the clinician with the results being released faster and for the laboratory, as employees need less time to complete the examination.
Conclusion
The results here show that the impedance aggregometry can be used in routine laboratory instead of or as a complement to the turbidimetric technique to monitor antiplatelet therapy based on acetylsalicylic acid.
References
- 1. Sudo T, Ito H, Ozeki Y, Kimura Y. Estimation of anti-platelet drugs on human platelet aggregation with a novel whole blood aggregometer by a screen filtration pressure method. Br J Pharmacol. 2001;133(8):1396-404.
- 2. Randomised trial of intravenous streptokinase, oral aspirin, both, or neither among 17,187 cases of suspected acute myocardial infarction: ISIS-2. ISIS-2 (Second International Study of Infarct Survival) Collaborative Group. Lancet. 1988;2(8607):349-60. Comment in: Lancet. 1997;349(9064):1551.
- 3. Patrono C, Baigent C, Hirsh J, Roth G; American College of Chest Physicians. Roth. Antiplatelet drugs: American College of Chest Physicians Evidence-Based Clinical Pract Practice Guidelines (8th edition). Chest. 2008;133(6 Suppl):199S-233S.
- 4. Farrell B, Godwin J, Richards S, Warlow C. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991;54(12):1044-54. Margaret LR, Roland L, Marian AP. Platelet function assays. Transfus Apheresis Sci. 2003;28:307-17.
- 5. Serebruany V, McKenzie M, Meister A, Fuzaylov S, Gurbel P, Atar D, et al. Whole blood impedance aggregometry for the assessment of platelet function in patients with congestive heart failure (EPCOT Trial). Eur J Heart Fail. 2002;4(4):461-7.
- 6. Szczeklik A, Musial J, Undas A, Sanak M, Nizankowski R. Aspirin resistance. Pharmacol Rep. 2005;57 Suppl:33-41.
- 7. Hillarp A, Lethagen S, Mattiasson I. Aspirin resistance is not a common biochemical phenotype explained by unblocked cyclooxygenase-1 activity. J Thromb Haemost. 2003;1(1):196-7.
- 8. Hart RG, Leonard AD, Talbert RL, Pearce LA, Cornell E, Bovill E, et al. Aspirin dosage and thromboxane synthesis in patients with vascular disease. Pharmacotherapy. 2003;23(5):579-84.
- 9. Riess H, Braun G, Brehm G, Hiller E. Critical evaluation of platelet aggregation in whole human blood. Am J Clin Pathol. 1986; 85 (1):50-6.
- 11. Botter DA, Paula GA, Leite JG, Cordani LK. Noções de estatística. São Paulo: Instituto de Matemática e Estatística/Universidade de São Paulo; 1996
- 12. Clinical and Laboratory Standard Institute. Defining, establishing and verifying reference intervals in the clinical laboratory; Approved guideline [Internet]. 3th ed. Pennsylvania; CLSI; 2008.[cited 2009 Dec 12]. Available from: http://www.clsi.org/source/orders/free/c28-a3.pdf
- 13. Mackie IJ, Jones R, Machin SJ. Platelet impedance aggregation in whole blood and its inhibition by antiplatelet drugs. J Clin Pathol. 1984;37(8):874-8.
- 14. Eikelboom J, Feldman M, Mehta SR, Michelson AD, Oates JA, Topol E. Aspirin resistance and its implications in clinical practice. Med Gen Med. 2005;7(3):76.
Comparative study of platelet aggregation by turbidimetric and impedance methods in patients under acetylsalicylic acid antiplatelet therapy
Publication Dates
-
Publication in this collection
01 Feb 2012 -
Date of issue
2010
History
-
Received
11 June 2010 -
Accepted
27 Aug 2010