Abstract
OBJECTIVE: The aim of this study was to verify if ABO phenotypes are associated with allergic rhinitis. METHODS: 168 patients with allergic rhinitis and 168 control individuals from the same geographical region and paired by gender and age were enrolled in the study. ABO phenotypes were identified in red blood cells using the hemagglutination technique. The Fisher exact and chi-squared tests were employed to compare proportions. Statistical significance was set for an alpha error of 5% (p-value < 0.05). RESULTS: The overall differences in the frequencies of the ABO phenotypes of patients and controls were marginal (χ2: 7.569; degrees of freedom (DF): 3; p-value = 0.055) however the O blood group was associated with allergic rhinitis (χ2: 5.764; DF: 1; p-value = 0.016; OR: 1.735; CI 95%: 1.127-2.673). The differences in the frequencies of the O phenotype in patients and controls were statistically different for men (χ2: 8.520; DF: 1; p-value = 0.003) but not for women (χ2: 0.6375; DF: 1; p-value = 0.4246). The A phenotype was associated with protection (OR: 0.4385; CI 95%: 0.2043-0.9415; p-value = 0.049) and the O phenotype was associated with susceptibility (OR = 2.789; CI 95%: 1.385-5.616; p-value = 0.005) to allergic rhinitis only for men. CONCLUSION: The O blood group phenotype is associated with allergic rhinitis in male but not in female patients.
Rhinitis, allergic, seasonal; Blood group antigens; ABO blood-group system; Respiratory hypersensitivity; Asthma
ORIGINAL ARTICLE
Evidence of an association between the O blood group and allergic rhinitis
Nelson Falsarella; Ana Iara da Costa Ferreira; Fabiana Nakashima; Cinara de Cássia Brandão de Mattos; Luiz Carlos de Mattos
Immunogenetics Laboratory, Molecular Biology Department, Faculdade de Medicina de São José do Rio Preto - FAMERP, São José do Rio Preto, SP, Brazil
Corresponding author Corresponding author: Luiz Carlos de Mattos Departamento de Biologia Molecular. Faculdade de Medicina de São José do Rio Preto Avenida Brigadeiro Faria Lima, 5416 15090-000 - São José do Rio Preto SP, Brazil Phone: 55 17 3201-5857 luiz.carlos@famerp.br
ABSTRACT
OBJECTIVE: The aim of this study was to verify if ABO phenotypes are associated with allergic rhinitis.
METHODS: 168 patients with allergic rhinitis and 168 control individuals from the same geographical region and paired by gender and age were enrolled in the study. ABO phenotypes were identified in red blood cells using the hemagglutination technique. The Fisher exact and chi-squared tests were employed to compare proportions. Statistical significance was set for an alpha error of 5% (p-value < 0.05).
RESULTS: The overall differences in the frequencies of the ABO phenotypes of patients and controls were marginal (χ2: 7.569; degrees of freedom (DF): 3; p-value = 0.055) however the O blood group was associated with allergic rhinitis (χ2: 5.764; DF: 1; p-value = 0.016; OR: 1.735; CI 95%: 1.127-2.673). The differences in the frequencies of the O phenotype in patients and controls were statistically different for men (χ2: 8.520; DF: 1; p-value = 0.003) but not for women (χ2: 0.6375; DF: 1; p-value = 0.4246). The A phenotype was associated with protection (OR: 0.4385; CI 95%: 0.2043-0.9415; p-value = 0.049) and the O phenotype was associated with susceptibility (OR = 2.789; CI 95%: 1.385-5.616; p-value = 0.005) to allergic rhinitis only for men.
CONCLUSION: The O blood group phenotype is associated with allergic rhinitis in male but not in female patients.
Keywords: Rhinitis, allergic, seasonal; Blood group antigens; ABO blood-group system; Respiratory hypersensitivity; Asthma
Introduction
Allergic rhinitis is a disease that affects the upper airway tract causing inflammation of the nasal mucosa. It is mediated by immunoglobulin E (IgE) antibodies which are produced after exposure to and sensitization by environmental allergens. The most common symptoms, nasal congestion, watery rhinorrhea, sneezing and itching, can be reversed spontaneously or by treatment. Allergic rhinitis depends both on environmental and genetic factors.(1)
Epidemiologic data suggest that the prevalence of allergic rhinitis has been increased in developing countries during the last decades.(2) A recent survey conducted in Brazil reported that this disease is highly prevalent among male children and adolescents receiving medical attention in emergency care services.(3)
Allergic rhinitis and asthma are both respiratory diseases which have similar immunopathological mechanisms.(4) It has been suggested based on epidemiological and experimental data that allergic rhinitis and asthma represent the manifestations of one syndrome with a wide spectrum of severity.(5) Therefore it is possible that the genetic and environmental factors causing susceptibility to asthma are also involved in susceptibility for allergic rhinitis.
The ABO histo-blood group system is one of the genetic risk factors linked to the susceptibility to asthma in some populations. Independent studies have analyzed the importance of this system in both children and adults in respect to asthma. One such study found statistically significant differences in the frequencies of the ABO and related secretor phenotypes in Australian adults(6) and another reported a greater incidence of A and B red blood cell phenotypes in patients with different atopical conditions compared to controls.(7) Associations between the ABO and Secretor systems and asthma have also been observed in Italian(8) and Taiwanese children(9) but not in Indian adults.(10) Despite these contradictory results observed among patients suffering from asthma, studies associating these genetic markers with allergic rhinitis are scarce.
The composition of the glycoconjugate profile of the respiratory epithelium and of the exocrine secretions is controlled, at least in part, by epistatic interactions between the ABO (ABO; 9q34.1) and Secretor (FUT2; 19q13.3) genes and influenced by their polymorphisms.(11) As these profiles represent important risk factors for the adherence of microorganisms and allergens(12) it is possible that the action of the set of ABO and FUT2 genes influence the susceptibility to other respiratory diseases apart from asthma. The objective of this study was to test the hypothesis that ABO histo-blood group systems is associated with allergic rhinitis.
Methods
Ethical considerations
This study was approved by the Research Ethics Committee of the Medicine School in São José do Rio Preto (Case 085/2008) and all participants, after receiving information about the objectives of the study, gave their informed written consent.
Selection of patients and controls
One hundred and sixty-eight adult patients of both genders were enrolled. Under 18-year-old patients, smokers and those with a diagnosis of asthma were excluded. All patients were matched by age and gender with controls (n = 168) without allergic rhinitis or asthma. Taking in account the results of a previous study(9) the number of patients enrolled is sufficient to demonstrate the differences in the ABO histo-blood group system with power higher than 90%.
Diagnosis of allergic rhinitis
The diagnosis of allergic rhinitis followed the criteria proposed by the Second Brazilian Consensus for Rhinitis.(1) The clinical history of the patient, any family history of the disease, a physical examination and the patient's report (symptoms of rhinitis more than four days a week for five consecutive weeks) were recorded. The cardinal symptoms considered were nasal congestion, watery rhinorrhea, paroxysmal sneezing and pruritus of the nose and/or palate or eyes.
Blood sample collection
For each participant, a 5-mL sample of peripheral blood was drawn by venous puncture and placed in a vacuum tube containing ethylenediaminetetraacetic acid (EDTA). Red blood cells were utilized to determine the ABO phenotypes.
Identification of the red blood cell phenotype of the ABO histo-blood system
The identification of the red blood cell phenotype of the ABO histo-blood system was achieved employing the direct and reverse phenotyping method following the protocol of Mattos et al.(13) Direct phenotyping, which identifies red blood cell antigens, is achieved by adding a drop of 5% red blood cells diluted in an isotonic solution to three clearly identified test-tubes containing monoclonal antibodies (anti-A, anti-B and anti-A,B) (Fresenius-Kabi, São Paulo, Brazil). Reverse typing, which identifies the regular antibodies of the plasma, is achieved by adding drops of standard A1 and B red blood cells to two clearly-marked test tubes containing two drops of plasma (Fresenius-Kabi, São Paulo, Brazil). The red blood cell phenotype was identified for each participant by the presence or absence of agglutination in the different steps of direct and reverse phenotyping.
Statistical analysis
To demonstrate any association between results, the exact Fisher test and Pearson's chi-squared test with Yates correction were used with the limit of significance being set at 5%. The values of odds ratio (OR) and 95% confidence interval (CI) were calculated.
Results
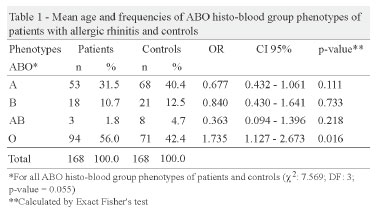
The results of the analysis of the data of patient and control groups, both with ages ranging from 18 to 85 years, are shown in Table 1. The mean ages were statistically similar (patients: 39.8 ± 17.5 years; control: 39.1 ± 16.7 years; p-value = 0.714).
The overall differences in the frequencies of the ABO histo-blood group systems between patients and controls were marginal (χ2: 7.569; degrees of freedom (DF): 3; p-value = 0.055) however the O blood group was associated with allergic rhinitis (χ2: 5.764; DF: 1; p-value = 0.016; OR: 1.735; CI 95%: 1.127-2.673).
Table 2 shows the results of the analysis of the patients and controls by gender. The differences in the frequencies of the ABO histo-blood group system phenotypes between patients and controls were statistically different for men (χ2: 8.520; DF: 1; p-value = 0.003) but not for women (χ2: 0.6375; DF: 1; p-value = 0.4246).
The A phenotype was associated with protection (OR: 0.4385; CI 95%: 0.2043-0.9415; p-value = 0.049) and the O phenotype was associated with susceptibility (OR = 2.789; CI 95%: 1.385-5.616; p-value = 0.005) to allergic rhinitis for men but not for women.
Discussion
The patients and controls enrolled in this study came from the northwestern region of the state of São Paulo, Brazil, which is a predominantly a farming and cattle-breeding region without large industrial centers.(14) This strategy was adopted in order to minimize the influence of industrial pollution, that is, atmospheric pollution which influences the prevalence of respiratory diseases.(15,16) Additionally, both patients and controls were non-smokers and were paired in respect to age and gender as there is evidence that these variables influence the prevalence of allergic rhinitis.(1)
The patient sample is representative of the population living in the region where this study was conducted in respect to ABO histo-blood group system. The overall frequencies of the four main phenotypes were similar to those reported in a previous study.(13) The number of male patients enrolled in this study is lower compared to women. Probably, this difference reflects the cultural behavior of men who are less inclined to seek medical attention compared to women.(17)
The overall frequencies of the ABO histo-blood group phenotypes of patients and controls showed a tendency that the O blood group phenotype is associated with allergic rhinitis. Additional comparisons of the participants by gender showed a smaller number of A blood group and a larger number O blood group male compared to female patients. Based on the p-values and Odds Ratio, the strength of the association seems to be much higher for the O blood group suggesting that this blood group confers almost a threefold higher risk of allergic rhinitis in men than in women compared to the A blood group.
The results reported here are in disagreement with those evaluating the ABO histo-blood group and atopic diseases, including allergic rhinitis and asthma.(6,7,10) Some aspects could contribute for these discordances. Our study evaluated only patients with diagnosis of allergic rhinitis. The majority of the patients enrolled in previous studies(6,7,10) were carriers of atopic diseases other than allergic rhinitis and the data were pooled. Therefore it is difficult to compare their results with those reported here.
Despite the differences mentioned above, the results of this study are in agreement, at least in part, with those reporting an association between the O blood group and asthma in Italian(8) and Taiwanese children(9) and European adults.(18) Since allergic rhinitis and asthma represent distinct manifestations of one syndrome,(5) it is possible that the mechanisms implicit in the association between the O blood group and asthma also favor the association of this genetic marker and allergic rhinitis in male individuals.
The biological basis of the association between the O blood group and allergic rhinitis in men remains unclear. The ABO gene, responsible for the genetic control of the ABO histo-blood group system is autosomal and there is no evidence that its phenotypic expression and pattern of inheritance are influenced by gender.(19) However the interaction between the O blood group and inflammatory immune response in the airway mucosa could increase the susceptibility for allergic rhinitis in men.
In fact, an inflammatory immune response characterized by increased lymphocyte infiltration in the gastric mucosa was observed in O blood group patients infected by Helicobacter pylori.(20) Additionally, it was demonstrated that the expression of inflammatory proteins in nasal secretions is higher in men that are diagnosed with seasonal allergic rhinitis, even after treatment using anti-inflammatory drugs, compared to women.(21) Therefore it is possible that the combined effect of the O blood group with the high expression of inflammatory proteins in the nasal secretions of male individuals contributes to the association observed in this study.
The importance of the ABO histo-blood group system as a risk factor for allergic rhinitis is still unknown. The ABO histo-blood group system is characterized by the expression of carbohydrate antigens in different tissues,(11) which are present in mucins, selectins, integrin receptors and in endothelial growth factor, as part of the glycosylation process.(22,23) The action of glycosyltransferases coded by the ABO genes modifies the glycoconjugate expression profile which reflects, at least in part, in the composition of the carbohydrates present in mucosae and exocrine secretions.(12) In fact the terminal structure of the glycoconjugates expressed in the O blood group differs from those expressed in the other ABO phenotypes.(11,19) Therefore the differences between distinct glycoconjugate profiles create different binding sites on the terminal structure the oligosaccharide chains.(12)
Since these glycoconjugates act as potential receptors for microorganisms, those expressed in the O blood group may bind allergens and influence the immune response.(12,24,25) It is possible that the profile of the glycoconjugates expressed by individuals with the O blood group, allied with the predisposition of men to express a higher level of anti-inflammatory proteins in nasal secretions favors the adherence of environmental allergens to the mucosa of the upper airway tract, thereby increasing their susceptibility for allergic rhinitis.
The association between the O blood group system and allergic rhinitis in men reported in this study contributes to a better understanding of the physiopathology and clinical variability of this disease and may help to improve strategies towards its prevention and diagnosis. Additionally, ABO histo-blood group phenotyping, an inexpensive and easily-to-perform assay, could be used to identify individuals at risk of developing allergic rhinitis.
Despite of the criteria adopted for the diagnosis of allergic rhinitis, the results of this study must be considered as preliminary as the measurement of specific IgE and the prick test were not performed for specific allergens. Even so, it sheds some light on the importance the genetic polymorphisms in the susceptibility for one specific respiratory disease the prevalence of which has been increasing over recent decades.(2) Similar investigations on patients from other Brazilian regions would be desirable to confirm the association reported here.
This study demonstrates the importance of the ABO histo-blood system and the gender in the manifestation of a respiratory disease influenced by environmental factors. Although only allergic rhinitis was evaluated, the results of this study agree, at least in part, with the observations on children(8,9) and adults(18) in relation to asthma.
Conclusion
The O blood group phenotype of the ABO histo-blood group system is associated with allergic rhinitis in male but not in female patients.
Acknowledgments
The study was carried out in the Immunogenetics Laboratory of the Molecular Biology Department, FAMERP and received financial support from the Brazilian Ministry of Education (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Demanda Social, Capes) Cinara de Cássia Brandão de Mattos and Ana Iara da Costa Ferreira received scholarships. Luis Carlos de Mattos received a research grant from the Faculdade de Medicina de São José do Rio Preto (FAMERP).
Submitted: 9/1/2011
Accepted: 10/17/2011
Conflict-of-interest disclosure: The authors declare no competing financial interest
- 1. Solé D, Mello Junior JF, Weckx LL, Rosário Filho NA, coordenadores. II Consenso Brasileiro sobre Rinites 2006. Rev Bras Alerg Immunopatol. [Internet] 2006 [cited 2011 Mar 30] 29(1):1-30. Available from: http://www.asbai.org.br/revistas/Vol291/consenso.pdf
- 2. Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002;347(12):911-20. Comment in: N Engl J Med. 2002;347(12):930-1.
- 3. Lasmar LM, Camargos PA, Ordones AB, Gaspar GR, Campos EG, Ribeiro GA. Prevalence of allergic rhinitis and its impact on the use of emergency care services in a group of children and adolescents with moderate to severe persistent asthma. J Pediatr (Rio J). 2007;83(6):555-61.
- 4. Baiardini I, Braido F, Tarantini F, Porcu A, Bonini S, Bousquet PJ, Zuberbier T, Demoly P, Canonica GW; GA2LEN. ARIA-suggested drugs for allergic rhinitis: what impact on quality of life? A GA2LEN review. Allergy. 2008;63(6):660-9.
- 5. Togias A. Rhinitis and asthma: evidence for respiratory system integration. J Allergy Clin Immunol. 2003;111(6):1171-83;quiz 1184.
- 6. Denborough MA, Downing HJ. Secretor status in asthma and hay fever. J Med Genet. 1968;5(4):302-5.
- 7. Brachtel R, Walter H, Beck W, Hilling M. Associations between a topic diseases and the polymorphic systems ABO, Kidd, Inv and red cell acid phosphatase. Hum Genet. 1979;49(3):337-48.
- 8. Ronchetti F, Villa MP, Ronchetti R, Bonci E, Latini L, Pascone R, et al. ABO/Secretor genetic complex and susceptibility to asthma in childhood. Eur Respir J. 2001;17(6):1236-8.
- 9. Chen YL, Chen JC, Lin TM, Huang TJ, Wangz ST, Lee MF, et al. ABO/secretor genetic complex is associated with the susceptibility of childhood asthma in Taiwan. Clin Exp Allergy. 2005;35(7):926-32.
- 10. Bijanzadeh M, Ramachandra NB, Mahesh PA, Savitha MR, Manjunath BS, Jayaraj BS. Lack of association between asthma and ABO blood group. Lung. 2009;187(6):389-92.
- 11. Oriol R. ABO, Hh, Lewis and secretion: serology, genetics and tissue distribution. In: Cartron JP, Rouger P, editors. Blood cell biochemistry: molecular basis of human blood group antigens. New York: Plenum; 1995. p.37-73.
- 12. Henry SM. Molecular diversity in the biosynthesis of GI tract glycoconjugates. A blood-group-related chart of microorganism receptors. Transfus Clin Biol. 2001;8(3):226-30.
- 13. Mattos LC, Sanches F, Cintra JR, Salles AB, Bonini-Domingos CR, Moreira HW. Genotipagem do locus ABO(9q34.1) em doadores de sangue da região noroeste do Estado de São Paulo. Rev Bras Hematol Hemoter. 2001;23(1):15-22.
-
14SEADE. Fundação Sistema Estadual de Análise de Dados. Secretaria de Planejamento e Desenvolvimento Regional. Perfil Regional. Região Administrativa de São José do Rio Preto. [Internet] 2009. [cited 2011 Mar 30] Available from: http://www.seade.gov.br/produtos/perfil/perfilMunEstado.php
- 15. Duchiade MP. Poluição do ar e doenças respiratórias: uma revisão. Cad Saúde Pública. 1992;8(3):311-30.
- 16. Bakonyi SM, Danni-Oliveira IM, Martins LC, Braga AL. Poluição atmosférica e doenças respiratórias em crianças na cidade de Curitiba, PR. Rev Saude Publica. 2004;38(5):695-700.
- 17. Gomes R, Nascimento EF, Araújo FC. Por que os homens buscam menos os serviços de saúde do que as mulheres? As explicações de homens com baixa escolaridade e homens com ensino superior. Cad Saude Publica. 2007;23(3):565-74.
- 18. Kauffmann F, Frette C, Pham QT, Nafissi S, Bertrand JP, Oriol R. Associations of blood group-related antigens to FEV1, wheezing, and asthma. Am J Respir Crit Care Med. 1996;153(1):76-82.
- 19. Schenkel-Brunner H. Human blood groups: chemical and biochemical basis of antigen specificity. Vien: Springer-Verlag; 2000.
- 20. Heneghan MA, Moran AP, Feeley KM, Egan EL, Goulding J, Connolly CE, et al. Effect of host Lewis and ABO blood group antigen expression on Helicobacter pylori colonisation density and the consequent inflammatory response. FEMS Immunol Med Microbiol. 1998;20(4):257-66.
- 21. Barrenäs F, Andersson B, Cardell LO, Langston M, Mobini R, Perkins A, et al. Gender differences in inflammatory proteins and pathways in seasonal allergic rhinitis. Cytokine. 2008;42(3):325-9.
- 22. Gooi HC, Schlessinger J, Lax I, Yarden Y, Libermann TA, Feizi T. Monoclonal antibodies reactive with the human epidermal-growth-factor receptor recognizes the blood-group-A antigen. Biosci Rep. 1983;3(11):1045-52.
- 23. Kuijper TW. Terminal glycosyltransferase activity - a selective role in cell-adhesion. Blood. 1993;81(4):873-82.
- 24. Karlsson KA, Angström J, Bergström J, Lanne B. Microbial interaction with animal cell surface carbohydrates. APMIS Suppl. 1992;27:71-83.
- 25. Lindén S, Mahdavi J, Semino-Mora C, Olsen C, Carlstedt I, Borén T , et al. Role of ABO secretor status in mucosal innate immunity and H. pylori infection. PLoS Pathog. 2008;4(1):e2.
Corresponding author:
Publication Dates
-
Publication in this collection
12 Mar 2012 -
Date of issue
Dec 2011
History
-
Received
01 Sept 2011 -
Accepted
17 Oct 2011