ABSTRACT
This work aimed to determine whether seropositivity to Helicobacter pylori infection was an independent risk factor for hyperhomocysteinemia patients with cardiovascular disease. The H. pylori IgG, IgA and homocystein levels in 96 patients with cardiovascular disease and 64 participants free of cardiovascular disease as control subjects were determined by ELISA assay. The results showed that seropositivity to H. pylori IgG and IgA levels of coronary artery disease (CAD)patients was significantly higher than the controls and CAD patients with H. pylori IgG and IgA negative antibodies. A significant correlation was found between the seropositivity to H. pylori IgG and homocysteine levels of CAD patients in comparison with the controls and CAD patients with seronegativity to H. pylori IgG and IgA (r=0.233, P= 0.019 ). The involvement of H. pylori infection in atherosclerosis process was based on the chronic inflammation, which might facilitate the CAD-related pathologies. The effect of the presence of H. pylori infection on homocysteine levels elevation in the CAD patients (as a risk factor independent of other traditional factors) was remarkable.
Cardiovascular disease; ELISA assay; homocysteine; Helicobacter pylori
INTRODUCTION
Cardiovascular disease is the most common cause of mortality and morbidity in the United States and many other nations (Reddy-Vanga et al. 2010Reddy Vanga S, Good M, Howard PA, Vacek JL. Role of Vitamin D in Cardiovascular Health. Am J Cardiol. 2010; 106(6): 798-805.). Coronary atherosclerosis process is multi-factorial. Traditional and classic cardiovascular risk factors such as diabetes mellitus (DM), hypertension (HTN), smoking and obesity have introduced as major causes, but significant proportions of the patients with coronary artery disease (CAD) do not have these traditional risks. Other factors, which may affect this chronic process, have been evaluated (Folsom et al. 1998Folsom AR, Nieto FJ, Sorlie P, Chambless LE, Graham DY. Helicobacter pylori seropositivity and coronary heart disease incidence. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Circulation. 1998; 98(9): 845-850.; Reddy-Vanga et al. 2010; Rogha et al. 2012Rogha M, Nikvarz M, Pourmoghaddas Z, Shirneshan K, Dadkhah D, Pourmoghaddas M. Is helicobacter pylori infection a risk factor for coronary heart disease? ARYA Atheroscler. 2012; 8(1): 5-8.). For example, infection-related chronic inflammation from Helicobacter pylori (H. pylori) is one of the CAD risk factors, because the CAD risk factors plasma fibrinogen, C-reactive protein, and blood leukocyte count become elevated in the seropositive subjects (Folsom et al. 1998). H. pylori infection is the most common infection worldwide, especially in the developing countries (Rogha et al. 2012). According to many reports, 70-90% of apparently healthy people of developing countries are estimated to be infected with H. pylori (Rogha et al. 2012; Chmiela et al. 2015Chmiela M, Gajewski A, Rudnicka K. Helicobacter pylori vs coronary heart disease - searching for connections. World J Cardiol. 2015; 7(4): 187-203.; Javadi et al. 2015Javadi L, Pourghassem Gargari B, Salekzamani S, Yousefzadeh R. Folate and homocysteine levels and their association with dietary intakes in Iranian patients infected with Helicobacter pylori: a case-control study. Acta Med Iran. 2015; 53(3): 162-167.). H. pylori is a Gram-negative bacterium with perfect adaptation to the acidic environment of the stomach and high affinity to gastric epithelial cells. Recently, possible association between H. pylori infection and extragastric disorders has been also suggested (Franceschi et al. 2006Franceschi F, Roccarina D, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection. Minerva Med. 2006; 97(1): 39-45.; Pacifico et al. 2010Pacifico L, Anania C, Osborn JF, Ferraro F, Chiesa C. Consequences of Helicobacter pylori infection in children. World J Gastroenterol. 2010; 16(41): 5181-5194.; Pacifico et al. 2014). An indirect association between the prevalence of H. pylori and the occurrence of CAD is demonstrated by many research studies (Rogha et al. 2012; Chmiela et al. 2015; Javadi et al. 2015). A significant association of H. pylori infection with CAD (OR 3.18, 95% CI 1.08-9.40) was shown by a multivariate logistic regression analysis (Rogha et al. 2012). According to majority of findings, the involvement of H. pylori in this process was based on the chronic inflammation, which might facilitate the CAD-related pathologies (Rogha et al. 2012; Chmiela et al. 2015). Several mechanisms have been proposed for how H. pylori might accelerate macrovascular complications and increase CAD risk (Cenerelli et al. 2002Cenerelli S, Bonazzi P, Galeazzi R, Testa I, Bonfigli AR, Sirolla C, et al. Helicobacter pylori masks differences in homocysteine plasma levels between controls and type 2 diabetic patients. Eur J Clin Invest. 2002; 32(3): 158-62.; Rogha et al. 2012; Javadi et al. 2015). It has been demonstrated that H. pylori is an important and serious cause of elevated levels of homocysteine (HCY) and is prevalent in the Caucasian population, ranging from 30 to 40% incidence. On the other hand, HCY is recognized as an independent risk factor for cardiovascular diseases. HCY has been demonstrated to be toxic to the endothelial cells and lipoproteins due to generation of oxygen radicals. High level of HCY appears to be one of the factors responsible for the increased risk of vascular damage and clinical CAD events (Sacco et al. 2004Sacco RL, Anand K, Lee HS, Boden-Albala B, Stabler S, Allen R, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the Northern Manhattan Study. Stroke. 2004; 35(10): 2263-2269.). A study on 116 patients with CAD who were matched with 116 controls via age and sex although showed a minor association between H. pylori infection and CAD. However, a stronger correlation between higher levels of triglycerides (fats) and lower levels of high density high-density lipoprotein (HDL) -cholesterol was found in the H. pylori-infected patients (Laurila et al. 1999Laurila A, Bloigu A, Näyhä S, Hassi J, Leinonen M, Saikku P. Association of Helicobacter pylori infection with elevated serum lipids. Atherosclerosis. 1999; 142(1): 207-210.; Ekesbo et al. 2000Ekesbo R, Nilsson PM, Lindholm LH, Persson K, Wadström T. Combined seropositivity for H. pylori and C. pneumoniae is associated with age, obesity and social factors. J Cardiovasc Risk. 2000; 7(3): 191-195.; Hoffmeister et al. 2001Hoffmeister A, Rothenbacher D, Bode G, Persson K, März W, Nauck MA, et al. Current infection with Helicobacter pylori, but not seropositivity to Chlamydia pneumoniae or cytomegalovirus, is associated with an atherogenic, modified lipid profile. Arterioscler Thromb Vasc Biol. 2001; 21(3): 427-32.; Kowalski 2001Kowalski M. Helicobacter pylori (H. pylori) infection in coronary artery disease: influence of H. pylori eradication on coronary artery lumen after percutaneous transluminal coronary angioplasty. The detection of H. pylori specific DNA in human coronary atherosclerotic plaque. J Physiol Pharmacol. 2001; 52(1 Suppl 1): 3-31.). Based on the above findings, these results could be consistent with the hypothesis that H. pylori infection might modify the serum lipid concentrations in a way that could increase the risk of CAD (Sacco et al. 2004). Hence, knowing the inflammation as a cardiovascular risk factor in the one hand and H. pylori and hyper-homocysteinemia involvement in CAD incidence on the other hand could be interesting to evaluate the H. pylori infection effect on HCY levels and atherosclerosis processes.
Thus, this study examined whether H. pylori seropositivity was associated with hyperhomocysteinemia and cardiovascular disease occurrence.
MATERIAL AND METHODS
Sampling and Coronary Angiography
This study was approved by the Ethical Committee of Iran University of Medical Sciences. The cross-sectional study was performed in Rasool Akram Hospital of Tehran from June 2014Rasool S, Abid S, Iqbal MP, Mehboobali N, Haider G, Jafri W. Relationship between vitamin B12, folate and homocysteine levels and H. pylori infection in patients with functional dyspepsia: A cross-section study. BMC Res Notes. 2012; 5: 206. to October 2014. Ninety six consecutive CAD patients (68 men and 28 women; mean age 52. 95 ± 1.25 and 51.32 ± 1.61 years old, respectively) and 64 controls were enrolled into the study and candidates for coronary angiography and informed consent were selected. Before catheterization, all the subjects completed a semi-structured questionnaire regarding their past medical and drug history. The diagnosis was based on the decision of an experienced clinician. Coronary angiography was carried out by left-heart catheterization and arteriography using Judkins method, and then a cardiologist separately reviewed the angiography films. According to angiography reports, the clinical and laboratory evaluated patients with ≥50% coronary stenosis were considered as CAD positive group and participants with <50% coronary stenosis were considered as CAD negative group, or controls. Accordingly, patients with hepatic dysfunction, autoimmune disease, thyroid dysfunction and/or adrenal dysfunction as well as patients who consumed any kinds of glucocorticoids were excluded from the study.
Biochemical Measurements
Fasting blood sample of catheterization participants were taken to measure lipid profiles, immunoglobulins G and A (anti H. pylori IgG and IgA) and homocysteine levels. ELISA kit (Diagnostic kit, PISHTAZ TEB Company, Teheran, Iran) was used to measure the homocysteine levels. Anti-H. pylori antibody status was determined by measuring the IgG and IgA antibody by ELISA assay (Diagnostic kit, PISHTAZ TEB Company). Spectrophotometric assay was used for lipid profiles assay.
Statistical Data Analysis
Statistical analyses were carried out using SPSS software (version 16.0, Chicago, IL, USA). Unpaired student t-tests and ANOVA test were used for comparing the continuous variable. Chi-square test was used for discrete variables. To compare the association of H. pylori infection with homocysteine and thereby CAD, logistic regression tests were used by adjusting the sex and age plus history of diabetes, dyslipidemia, and/or hypertension.
RESULTS
Demographic characteristics of four study groups are shown in Tables 1 and 2. No significant differences were found in terms of demographic characteristics between the CAD patients and controls with anti-H. pylori IgG positive and negative and between the CAD patients and controls with anti-H. pylori IgA positive and negative. As shown in Table 1, the anti-H. pylori IgG (72.49 ± 3.64U/mL) and IgA (46.72 ± 3.24 U/mL) levels of CAD patient with positive anti -H. pylori IgG were significantly more than those were found in the CAD patients with negative anti-H. pylori IgG (9.34 ± 2.11 and 12.20 ± 1.15 U/mL). The values of 8.05 ± 0.40 and 15.48 ± 3.18 U/mL were achieved for anti-H. pylori IgG and anti-H. pylori IgA of controls with negative anti-H.P. IgG, respectively, which were lower significantly than those found for CAD patient with positive and negative anti-H. pylori IgG. The anti-H. pylori IgG (67.21 ± 4.00 U/mL) and anti-H. pylori IgA (38.90 ± 3.68 U/mL) levels of the control group with positive anti-H. pylori IgG were lower than CAD patient with positive anti-H. pylori IgG but significantly higher than negative anti-H. pylori IgG CAD patients.
According to Table 2, 64.96 ± 2.97 and 43.63 ± 3.07 U/mL of anti-H. pylori IgG and anti-H. pylori IgA, respectively of CAD patient with positive H. pylori IgA were significantly higher than those found for the CAD patients with negative anti-H. pylori IgA (21.16 ± 11.20 and 7.40 ± 0.48 U/mL). Controls with the negative anti-H. pylori IgA (15.62 ± 5.31 and 6.61± 0.63U/mL) and the control subjects with positive anti-H. pylori IgA (56.81 ± 4.72 and 38.06 ± 324 U/mL) respectively. As shown in Table 3 and Figure 1 (A), the serum homocysteine concentration of the CAD patients with positive anti-H. pylori IgG (27.70 ± 1.28 µmol/L) was significantly (P= 0.05) higher than CAD patients with negative anti-H. pylori IgG (22.16 ± 2.19 µmol/L). The difference between the HCY levels of CAD patients with positive anti-H. pylori IgG (27.70± 1.28µmol/L (and the control group with positive anti-H.P. IgG (22.38 ± 1.19 µmol /L) was significant (P=0.02). The homocysteine levels of the CAD patients with positive anti-H. pylori IgG (27.70 ± 1.28 µmol/L) was significantly (P=0.02) higher than the control subjects with negative anti-H.P IgG positive (20.62 ± 1.51 µmol /L). The serum homocysteine concentration of the control subjects with negative anti-H.P IgG positive (22.38 ± 1.19 µmol /L) and control group with negative anti-H.P IgG (20.62± 1.51 µmol /L) was not different significantly (P= 0.936). A significant correlation with r= 0.233 , P=0.0.19 was identified between anti-H. pylori IgG and homocysteine levels of the CAD patients with positive anti-H. pylori IgG (Fig.1 B), while the correlation between the anti-H. pylori IgG and homocysteine levels of CAD patients with negative anti-H. pylori IgG was not significant (r= 0.005, P=0.493). The correlation between the anti-H. pylori IgG and homocysteine levels of the control group with positive and negative anti-H.P IgG was not significant (r= -0.071, P=0.325 and r= -0.071, P=0.325, respectively). It is worth to note that correlation between the anti-H. pylori IgG and homocysteine levels of all the subjects was significant (r= 0.233, P=0.002).
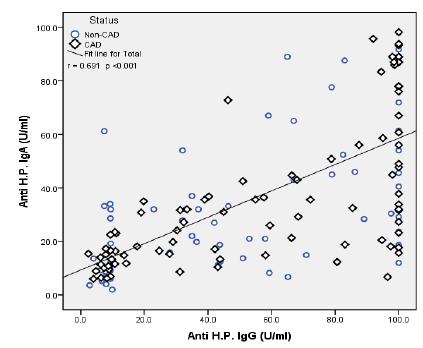
As shown in Table 4 and Figure 2 A, there was not a significant (P=1) difference between the homocysteine levels of the CAD patients with positive anti-H. pylori IgA (24.70 ± 0.80 µmol/L( as comparison with the CAD patients with negative anti-H. pylori IgA (26.50 ± 4.49 µmol/L). Serum homocysteine concentration of the CAD patients with positive anti-H. pylori IgA (24.70 ± 0.80 µmol/L µmol/L) was not significantly (P= 0.1) higher than the control subjects with positive anti-H. pylori IgA (22.79 ± 1.12 µmol/L) but was higher than the controls with negative anti-H.P. IgA positive (17.85 ± 1.07 µmol/L) significantly (P=0.01). The difference between the homocysteine levels of the control subjects with positive anti-H.P IgA (22.79 ± 1.12 µmol /L) and controls with negative anti H. pylori IgA (17.85 ± 1.07 µmol/L) was not different significantly (P=0.34). Serum homocysteine concentration of the CAD patients with negative anti-H. pylori IgA (26.50 ± 4.49 µmol/L) was not significantly (P= 0.75) higher than the control subjects with positive anti-H. pylori IgA (26.50 ± 4.49 µmol /L). A significant correlation (P<0.001, r=0.691) was found between the anti- H. pylori IgA and anti H. pylori IgG of CAD patients in comparison with non-CAD patients (Fig. 3).
(A): Homocysteine levels of CAD patients with positive and negative anti H. pylori IgG and controls with positive and negative anti H. pylori IgG (B): The correlation between homocysteine levels and anti H. pylori IgG levels of CAD patients with positive and negative anti H. pylori IgG and of controls with positive and negative anti H. pylori IgG groups were identified. 4 P=0.020 (in comparison with 1); 4 P=0.020 (in comparison with 2); 4, P=0.0 5 (in comparison with 3); 3, P=1.000 (in comparison with 2); 2, P=0.936 (in comparison with 1); 3, P=0. 935 (in comparison with 1); Correlation in all subjects, r= 0.233, P=0.002; ○) Correlation in controls with negative anti H. pylori IgG, r= 0.324, P= 0.076; □) Correlation in controls with positive anti H. pylori IgG, r= -0.071, P=0.325; ♦) Correlation in CAD patients with negative anti H. pylori IgG, r= 0.005, P=0.493; ♦♦) Correlation in CAD patients with positive anti H. Pylori IgG, r= 0.233, P=0.0.19.
- Homocysteine and anti H. pylori IgG and IgA levels of CAD patients with positive and negative anti-H.P IgG
- Homocysteine and anti H. pylori IgG and IgA levels of CAD patients with positive and negative anti H. pylori IgA and the control subjects with positive and negative anti-H. Pylori IgA
(A): Homocysteine levels of the CAD patients with positive and negative anti-H. pylori IgA and controls with positive and negative anti-H. pylori IgA. (B): The correlation between the homocysteine and anti-H. pylori IgA levels of CAD patients with positive and negative anti-H. pylori and of the controls with positive and negative anti H. pylori IgA groups. 4 P=0.011(in comparison with 1); 4 P=0.114(in comparison with 2); 4, P=1.000 (in comparison with 3); 3, P=0.197(in comparison with 1); 2, P=0.346 (in comparison with 1); 2, P=0.754(in comparison with 3); B) Correlation between all groups, r= 0.197, P=0.006; ○) Correlation for controls with negative anti H. pylori IgA, r= 0.324, P= 0.076; □) Correlation for controls with positive anti H. pylori IgA, r= -0.081, P=0.335; ♦) Correlation for CAD patients with negative anti H. pylori IgA, r= 0.007, P=0.489; ♦♦) Correlation for CAD patients with positive anti H. pylori IgA, r= 0.075, P=0.256.
Correlation between anti-H. pylori IgG and anti-H. pylori IgA of patients with the controls. r= 0.691, p< 0.001.
DISCUSSION
Several studies have demonstrated that hyperhomocysteinemia and H. pylori infection have contributed in the cardiovascular disease pathogenesis, independent of other conventional risk factors (Sung and Sanderson 1996Sung JJ, Sanderson JE. Hyperhomocysteinaemia, Helicobacter pylori, and coronary heart disease. Heart. 1996; 76(4): 305-307.; Leung et al. 2001Leung WK, Ma PK, Choi PC, Ching JY, Ng AC, Poon P, et al. Correlation between Helicobacter pylori infection, gastric inflammation and serum homocysteine concentration. Helicobacter. 2001; 6(2): 146-150.; Sharma and Aggarwal 2015Sharma V, Aggarwal A. Helicobacter pylori: Does it add to risk of coronary artery disease. World J Cardiol. 2015; 7(1): 19-25.). As shown in Tables 1 and 2, there was not a significant difference between the demographic characterization of the patients with CAD and controls. According to Figures 1 A and 2 A, a significant difference was found between anti-H.P. IgG and IgA levels of the patients with CAD (P= 0.020) and controls (P=0.011). Serum homocysteine concentration of the patients with CAD was more than the controls significantly. A positive correlation was found between the homocysteine levels and anti-H. pylori IgG in the patients with CAD as comparison to the control subjects. It has been proposed that H. pylori infection might modify the serum homocysteine concentration in a way that could increase the risk of CAD. The results of a case-control study showed that H. pylori infection increased a two-fold risk of CAD (Sung and Sanderson 1996). However, the possible mechanism of a chronic infection by H. pylori leading to atherosclerosis is yet to be identified. One of the proposed mechanisms is that H. pylori chronic infection increases the acute inflammation factors such as fibrinogen and sialic acid, which are predictors of CAD (Ringnér et al. 1994). In consistent with these results, a higher concentration of fibrinogen and total leukocyte count were reported for the patients with cardiovascular disease and infected by H. pylori as comparison to controls (Patel et al. 1995Patel P, Mendall MA, Carrington D, Strachan DP, Leatham E, Molineaux N, et al. Association of Helicobacter pylori and Chlamydia pneumoniae infections with coronary heart disease and cardiovascular risk factors. BMJ. 1995; 311(7007): 711-714.). The other hypothesis is that chronic H. pylori infection leads to malabsorption of vitamin B-6, vitamin B-12 and folate, methylation defeat and hyperhomocysteinaemia, thereby inducing arterial damage. It has been shown that nitric oxide secretion from the endothelial cells is inhibited by homocysteine, which comforts platelet aggregation and vasoconstriction. The balance between the procoagulants and anticoagulants might be changed by homocysteine via selective manners such as inhibition of the thrombomodulin processing and releasing, decreasing the protein C activation and inducing a protease activator of coagulation factor V (Sung and Sanderson 1996). Other mechanisms of H. pylori infection that could lead to atherosclerosis are destructive influence of H. pylori and its products like cytokines and cytotoxins on coronary endothelium, activation of immune mechanisms, which react with the nuclei of monocytes in atherosclerotic vessel wall and cytoplasm of fibroblast-like cell in atherosclerosis plaques (Rogha et al. 2012). In agreement with the present results, the results of a study on 93 patients under diagnostic coronary arteriography with infection H. pylori, showed a significant decrease of vitamin B12 and folate levels, thereby increasing homocysteine levels. They suggested that homocysteine could induce endothelial damage directly, affect platelet function and coagulation factors and increase the oxidation of LDL-C, which have critical role in cardiovascular disease occurrence (Ringnér et al. 1994). In a study patients with H. pylori infection exhibited a decreased secretion of ascorbic acid by gastric mucosa and elevated gastric pH, thereby the folate absorption from the diet was decreased due to low ascorbic acid in gastric juice, and subsequently a significant rise was found in homocysteine levels (Lucock et al. 1995Lucock MD, Priestnall M, Daskalakis I, Schorah CJ, Wild J, Levene MI. Nonenzymatic degradation and salvage of dietary folate: physicochemical factors likely to influence bioavailability. Biochem Mol Med. 1995; 55(1): 43-53.). However, it is important to consider that confounding variables such as vitamin deficiency, acute-phase response to vascular diseases, medication use, hypertension, advanced age and gender are well-known factors influencing homocysteinemia and should be considered. An inverse relationship was demonstrated among the homocysteine levels and H. pylori infection in the patients with functional dyspepsia in a cross-sectional study by Rasool et al. (2012). The authors showed that 46.2% of H. pylori- positive patients had hyperhomocysteinemia (>15 μmol/L) when compared to H. pylori- negative group (44%). They also reported that this was a higher proportion in comparison with that was observed in healthy population (Rasool et al. 2012). The results demonstrated that H. pylori did affect directly HCY metabolism in the liver (Cenerelli et al. 2002; Longo-Mbenza et al. 2012Longo-Mbenza B, Nsenga JN, Mokondjimobe E, Gombet T, Assori IN, Ibara JR, et al. Helicobacter pylori infection is identified as a cardiovascular risk factor in Central Africans. Vasc Health Risk Manag. 2012; 6: 455-461.). They showed that disrupted metabolism of HCY, which was induced by H. pylori led to an increase of HCY levels similar to those found in diabetic patients. Emphasizing the probable impairment of insulin function regarding the regulation of HCY level through the homocysteine/methionine metabolism, which caused higher levels of HCY in the CAD patients infected by H. pylori and the importance of H. pylori infection in determining the elevated HCY levels.
In summary, a small sample size was investigated and these observations should be confirmed in a larger sample of the patients with more analysis works. Here, only two independent variables were analysed, but it would be worthwhile to consider other probable variables involving in CAD disease in future studies.
CONCLUSION
The present study demonstrated an inverse relationship between the homocysteine levels and H. pylori seropositivity (IgG and IgA) and atherosclerosis occurrence in the patients with CAD. Since classic risk factors were not able to explain all cases of CAD, the results of present study suggested that chronic H. pylori infection affected the development or maintenance of CAD, since it induced chronic long term infection within gastric epithelium, which led to not only local but systemic inflammation. According to the present findings, the involvement of H. pylori in this process was based on the chronic inflammation, which might facilitate the CAD-related pathologies. Moreover, impact of the presence of H. pylori was found on homocysteine levels in such patients.
ACKNOWLEDGEMENTS
This study was supported by a grant from the University of Medical Sciences. The authors would like to thank Rasool Akram Hospital for providing the samples.
REFERENCES
- Cenerelli S, Bonazzi P, Galeazzi R, Testa I, Bonfigli AR, Sirolla C, et al. Helicobacter pylori masks differences in homocysteine plasma levels between controls and type 2 diabetic patients. Eur J Clin Invest. 2002; 32(3): 158-62.
- Chmiela M, Gajewski A, Rudnicka K. Helicobacter pylori vs coronary heart disease - searching for connections. World J Cardiol. 2015; 7(4): 187-203.
- Ekesbo R, Nilsson PM, Lindholm LH, Persson K, Wadström T. Combined seropositivity for H. pylori and C. pneumoniae is associated with age, obesity and social factors. J Cardiovasc Risk. 2000; 7(3): 191-195.
- Folsom AR, Nieto FJ, Sorlie P, Chambless LE, Graham DY. Helicobacter pylori seropositivity and coronary heart disease incidence. Atherosclerosis Risk in Communities (ARIC) Study Investigators. Circulation. 1998; 98(9): 845-850.
- Franceschi F, Roccarina D, Gasbarrini A. Extragastric manifestations of Helicobacter pylori infection. Minerva Med. 2006; 97(1): 39-45.
- Hoffmeister A, Rothenbacher D, Bode G, Persson K, März W, Nauck MA, et al. Current infection with Helicobacter pylori, but not seropositivity to Chlamydia pneumoniae or cytomegalovirus, is associated with an atherogenic, modified lipid profile. Arterioscler Thromb Vasc Biol. 2001; 21(3): 427-32.
- Javadi L, Pourghassem Gargari B, Salekzamani S, Yousefzadeh R. Folate and homocysteine levels and their association with dietary intakes in Iranian patients infected with Helicobacter pylori: a case-control study. Acta Med Iran. 2015; 53(3): 162-167.
- Kowalski M. Helicobacter pylori (H. pylori) infection in coronary artery disease: influence of H. pylori eradication on coronary artery lumen after percutaneous transluminal coronary angioplasty. The detection of H. pylori specific DNA in human coronary atherosclerotic plaque. J Physiol Pharmacol. 2001; 52(1 Suppl 1): 3-31.
- Laurila A, Bloigu A, Näyhä S, Hassi J, Leinonen M, Saikku P. Association of Helicobacter pylori infection with elevated serum lipids. Atherosclerosis. 1999; 142(1): 207-210.
- Leung WK, Ma PK, Choi PC, Ching JY, Ng AC, Poon P, et al. Correlation between Helicobacter pylori infection, gastric inflammation and serum homocysteine concentration. Helicobacter. 2001; 6(2): 146-150.
- Longo-Mbenza B, Nsenga JN, Mokondjimobe E, Gombet T, Assori IN, Ibara JR, et al. Helicobacter pylori infection is identified as a cardiovascular risk factor in Central Africans. Vasc Health Risk Manag. 2012; 6: 455-461.
- Lucock MD, Priestnall M, Daskalakis I, Schorah CJ, Wild J, Levene MI. Nonenzymatic degradation and salvage of dietary folate: physicochemical factors likely to influence bioavailability. Biochem Mol Med. 1995; 55(1): 43-53.
- Pacifico L, Anania C, Osborn JF, Ferraro F, Chiesa C. Consequences of Helicobacter pylori infection in children. World J Gastroenterol. 2010; 16(41): 5181-5194.
- Pacifico L, Osborn JF, Tromba V, Romaggioli S, Bascetta S, Chiesa C. Helicobacter pylori infection and extragastric disorders in children: a critical update. World J Gastroenterol. 2014; 20(6): 1379-1401.
- Patel P, Mendall MA, Carrington D, Strachan DP, Leatham E, Molineaux N, et al. Association of Helicobacter pylori and Chlamydia pneumoniae infections with coronary heart disease and cardiovascular risk factors. BMJ. 1995; 311(7007): 711-714.
- Rasool S, Abid S, Iqbal MP, Mehboobali N, Haider G, Jafri W. Relationship between vitamin B12, folate and homocysteine levels and H. pylori infection in patients with functional dyspepsia: A cross-section study. BMC Res Notes. 2012; 5: 206.
- Reddy Vanga S, Good M, Howard PA, Vacek JL. Role of Vitamin D in Cardiovascular Health. Am J Cardiol. 2010; 106(6): 798-805.
- Ringnér M, Valkonen KH, Wadström T. Binding of vitronectin and plasminogen to Helicobacter pylori. FEMS Immunol Med Microbiol. 1994; 9(1): 29-34.
- Rogha M, Nikvarz M, Pourmoghaddas Z, Shirneshan K, Dadkhah D, Pourmoghaddas M. Is helicobacter pylori infection a risk factor for coronary heart disease? ARYA Atheroscler. 2012; 8(1): 5-8.
- Sacco RL, Anand K, Lee HS, Boden-Albala B, Stabler S, Allen R, et al. Homocysteine and the risk of ischemic stroke in a triethnic cohort: the Northern Manhattan Study. Stroke. 2004; 35(10): 2263-2269.
- Sharma V, Aggarwal A. Helicobacter pylori: Does it add to risk of coronary artery disease. World J Cardiol. 2015; 7(1): 19-25.
- Sung JJ, Sanderson JE. Hyperhomocysteinaemia, Helicobacter pylori, and coronary heart disease. Heart. 1996; 76(4): 305-307.
Publication Dates
-
Publication in this collection
2016
History
-
Received
25 Aug 2015 -
Accepted
04 Oct 2015