Abstracts
Antimicrobial resistance is a threat to public health worldwide and is associated with higher mortality and morbidity. Despite the extensive knowledge about this problem, drug resistance has continued to emerge, especially in intensive care units (ICUs). The objective of this study was to evaluate the frequencies of epidemiologically relevant resistance phenotypes in pathogens isolated from ventilator-associated pneumonia (VAP), bloodstream infections (BSI) and urinary tract infections (UTI) in patients admitted in the adult intensive care unit (AICU) of the Clinical Hospital of Federal University of Uberlândia, during an one year period. Additionally, at the period of the study, the antibiotic consumption in AICU was verified. Coagulase-negative staphylococci and S. aureus were the main agents of BSI (43.9%), with 60.0% of oxacilin-resistance for both microorganisms, Klebsiella-Enterobacter group predominated in UTI (23.4%), with resistance to third generation cephalosporins in 58.0% of the isolates; and, Pseudomonas aeruginosa in VAP (42.0%), with 72.0% of resistance to imipenem. Cephalosporins (49.6%), vancomycin (37.4%) and carbapenems (26.6%) were the most prescribed antibiotics in the unit. The comparison of the results with a publication of the NNIS program evidenced a worse situation in the studied hospital, mainly between Gram-negative, that had surpassed the percentile 90% elaborated by that system. Based on these results a reconsideration on the empirical use of antibiotics and on prevention and control of nosocomial infections practices is recommended.
Nosocomial infection; epidemiology; multiresistant microorganisms
A resistência aos antimicrobianos é uma ameaça a saúde pública mundial e está associada a uma maior mortalidade e morbidade. Apesar dos vastos conhecimentos sobre este problema, a resistência aos antibióticos continua a emergir, especialmente em unidades de terapia intensiva (UTI). O objetivo deste estudo foi avaliar a freqüência de fenótipos de resistência epidemiologicamente importantes em patógenos isolados de pneumonia associada à ventilação mecânica (PAV), infecções de corrente sangüínea (ICS) e de infecções de trato urinário (UTI) nos pacientes atendidos na unidade de terapia intensiva de adultos (UTIA) do Hospital de Clínicas da Universidade Federal de Uberlândia, durante o período de um ano. Adicionalmente, no período do estudo, foi analisado o consumo de antibióticos na UTIA. Staphylococcus spp coagulase negativo e S. aureus foram os principais agentes de ICS (43,9%), com 60,0% de resistência à oxacilina em ambos os microrganismos. O grupo Klebsiella-Enterobacter predominou nas ITU (23,4%), com resistência às cefalosporinas de terceira geração em 58,0% dos isolados; e, Pseudomonas aeruginosa nas PAV (42,0%), com 72,0% de resistência ao imipenem. As cefalosporinas (49,6%), vancomicina (37,4%) e os carbapenêmicos (26,6%) foram os antibióticos mais prescritos na unidade. A comparação dos resultados com publicações do programa NNIS evidenciou uma pior situação no hospital estudado, especialmente entre os Gram-negativos, que ultrapassaram o percentil 90% elaborado por este programa. De acordo com os resultados apresentados neste estudo, uma revisão do uso empírico de antibióticos e da prevenção e controle de infecções hospitalares é recomendada.
Infecção hospitalar; epidemiologia; microrganismos multirresistentes
MEDICAL MICROBIOLOGY
Epidemiologically relevant antimicrobial resistance phenotypes in pathogens isolated from critically ill patients in a Brazilian Universitary Hospital
Fenótipos de resistência antimicrobiana epidemiologicamente importantes de patógenos isolados de pacientes críticos de um hospital universitário brasileiro
Rodolfo Henriques de Carvalho; Paulo P. Gontijo Filho
Instituto de Ciências Biomédicas, Hospital de Clínicas, Universidade Federal de Uberlândia, Uberlândia, MG, Brasil
ABSTRACT
Antimicrobial resistance is a threat to public health worldwide and is associated with higher mortality and morbidity. Despite the extensive knowledge about this problem, drug resistance has continued to emerge, especially in intensive care units (ICUs). The objective of this study was to evaluate the frequencies of epidemiologically relevant resistance phenotypes in pathogens isolated from ventilator-associated pneumonia (VAP), bloodstream infections (BSI) and urinary tract infections (UTI) in patients admitted in the adult intensive care unit (AICU) of the Clinical Hospital of Federal University of Uberlândia, during an one year period. Additionally, at the period of the study, the antibiotic consumption in AICU was verified. Coagulase-negative staphylococci and S. aureus were the main agents of BSI (43.9%), with 60.0% of oxacilin-resistance for both microorganisms, Klebsiella-Enterobacter group predominated in UTI (23.4%), with resistance to third generation cephalosporins in 58.0% of the isolates; and, Pseudomonas aeruginosa in VAP (42.0%), with 72.0% of resistance to imipenem. Cephalosporins (49.6%), vancomycin (37.4%) and carbapenems (26.6%) were the most prescribed antibiotics in the unit. The comparison of the results with a publication of the NNIS program evidenced a worse situation in the studied hospital, mainly between Gram-negative, that had surpassed the percentile 90% elaborated by that system. Based on these results a reconsideration on the empirical use of antibiotics and on prevention and control of nosocomial infections practices is recommended.
Key-words: Nosocomial infection, epidemiology, multiresistant microorganisms.
RESUMO
A resistência aos antimicrobianos é uma ameaça a saúde pública mundial e está associada a uma maior mortalidade e morbidade. Apesar dos vastos conhecimentos sobre este problema, a resistência aos antibióticos continua a emergir, especialmente em unidades de terapia intensiva (UTI). O objetivo deste estudo foi avaliar a freqüência de fenótipos de resistência epidemiologicamente importantes em patógenos isolados de pneumonia associada à ventilação mecânica (PAV), infecções de corrente sangüínea (ICS) e de infecções de trato urinário (UTI) nos pacientes atendidos na unidade de terapia intensiva de adultos (UTIA) do Hospital de Clínicas da Universidade Federal de Uberlândia, durante o período de um ano. Adicionalmente, no período do estudo, foi analisado o consumo de antibióticos na UTIA. Staphylococcus spp coagulase negativo e S. aureus foram os principais agentes de ICS (43,9%), com 60,0% de resistência à oxacilina em ambos os microrganismos. O grupo Klebsiella-Enterobacter predominou nas ITU (23,4%), com resistência às cefalosporinas de terceira geração em 58,0% dos isolados; e, Pseudomonas aeruginosa nas PAV (42,0%), com 72,0% de resistência ao imipenem. As cefalosporinas (49,6%), vancomicina (37,4%) e os carbapenêmicos (26,6%) foram os antibióticos mais prescritos na unidade. A comparação dos resultados com publicações do programa NNIS evidenciou uma pior situação no hospital estudado, especialmente entre os Gram-negativos, que ultrapassaram o percentil 90% elaborado por este programa. De acordo com os resultados apresentados neste estudo, uma revisão do uso empírico de antibióticos e da prevenção e controle de infecções hospitalares é recomendada.
Palavras-chave: Infecção hospitalar, epidemiologia, microrganismos multirresistentes.
INTRODUCTION
Antimicrobial resistance is a threat to public health in nations around the globe and is associated with higher mortality, morbidity and higher costs (9,19). Despite the extensive knowledge about the forces that drive antimicrobial-drug resistance (failures of hospital hygiene, selective pressures created by overuse of antibiotics, and mobile genetic elements that can encode bacterial resistance mechanisms), drug resistance has continued to emerge, especially in intensive care units (ICUs) (6,11,20), due to base illness (generally associated to a immunodefficiency) (1) and massive antibiotic use in these units, with a close correlation between the antimicrobials consumption and the emergence of bacterial resistance (7).
The mostly frequent microorganisms involved in nosocomial infections are oxacilin-resistant Staphylococcus aureus, oxacilin-resistant coagulase-negative staphylococci, vancomycin-resistant Enterococcus spp, third generation cephalosporins-resistant E. coli, Enterobacter spp and Klebsiella pneumoniae. Another important microorganism associated to nosocomial infection is Pseudomonas aeruginosa which have some phenotypes resistant to third generation cephalosporins, imipenem and fluoroquinolons (5).
In order to fight against these resistance cases, well-designed antimicrobial surveillance programs are essential to provide informations about microbial occurrence in different geographical regions and antimicrobial resistance patterns in nosocomial and community-acquired infections. The "Intensive Care Antimicrobial Resistance Epidemiology" (ICARE) (3) and the "European Prevalence of Infection in Intensive Care" (EPIC) (5) programs, designed to research the antibiotic resistance problem at ICU units in USA and Europe, respectively, should be considered. Other programs, as the "European Antimicrobial Resistance Surveillance System" (EARSS), extends the monitoring to critical and non-critical units (2).
In Brazil, despite the lack of information about this issue, the "Agência Nacional de Vigilância Sanitária" (ANVISA) launched the "Sistema Nacional de Informação para o Controle de Infecções em Serviços de Saúde" (SINAIS), aiming investigation and improvement of the actions in preventing and controlling nosocomial infections, and promotes the knowledge of infections rates, etiological agents and activity of the Controlling Committee of Nosocomial Infection of each participant hospital (17).
Additionally to these governmental programs, there are others, sponsored by pharmaceutical industries, as SENTRY (18) and the "Meropenem Yearly Susceptibility Test Information Collection" (MYSTIC) dedicated mainly to the analysis of the prescription and respective resistance to carbapenems, that also provide important data about bacterial resistance to antibiotics (14).
The objective of this study was to investigate the etiology and to determine the frequency of epidemiologically relevant resistance phenotypes of microorganisms recovered from patients with ventilator-associated pneumonia (VAP), bloodstream infections (BSI) and urinary tract infections (UTI) in the adult intensive care unit of Clinical Hospital of Federal University of Uberlândia, a clinical-surgical unit, comparing these data to those published by the "US Centers for Prevention and Disease Control" according to NNIS methodology. The antibiotic consumption in the unit during the study period was monitored.
MATERIAL AND METHODS
Institution
The Clinical Hospital of Federal University of Uberlândia (UFU) is a tertiary level hospital with 500 beds, 15 of them destined to adult Intensive Care Unit (AICU), a clinical-surgical unit.
Study Design
A prospective surveillance was performed in AICU from February/2006 to February/2007 looking for epidemiologically relevant resistant phenotypes among microorganisms isolated from ventilator-associated pneumonia (VAP), bloodstream infections (BSI) and urinary tract infections (UTI) in patients in use of vesical catheters. Additionally, antimicrobials consumption was monitored once a month at the study period. This study was approved by Ethics Committee of UFU (number 02406).
Specimen collection
Tracheal aspirate of patients that had presented clinical and radiological indications of pneumonia 48 hours after the use of mechanical ventilation for diagnosis of VAP was collected (8). Patients in use of vesical catheter with fever and absence of other infection focus 48 hours after the insertion of the catheter had their urine collected for diagnosis of UTI (symptomatic infection), and those who were in use of the urinary catheter for at least 7 days without any clinical symptoms of infection also had their urine collected for diagnosis of UTI (asymptomatic infection) (8). Hemocultures were performed in blood specimens obtained from peripheral puncture.
Microbiological techniques
The following phenotypes had been considered in this study: oxacilin-resistant Staphylococcus aureus (ORSA), oxacilin-resistant coagulase-negative staphylococci, β-lactamics-resistant and aminoglycosides-resistant Enterococcus spp, third generation cephalosporins-resistant and fluoroquinolons-resistant Escherichia coli, third generation cephalosporins-resistant Klebsiellae and other Enterobacteriaceae, ceftazidime, imipenem and fluoroquinolons-resistant Pseudomonas aeruginosa and carbapenem-resistant Acinetobacter spp.
Hemoculture
Hemocultures were performed inoculating 5-10 mL of blood into a flask of the automatic commercial system Bactec/Alert® (Vitek System). Positive cultures were further sub-cultured in human Müeller-Hinton Agar (Isofar LTDA, Brazil) supplemented with 5% of human blood and incubated for 24-48 hours at 35 ± 2ºC in the hospital's microbiology laboratory.
Tracheal aspirate
Quantitative technique was used by plating on MacConkey Agar (BD, USA), Manitol Salt Agar (Isofar LTDA, Brazil), Müeller-Hinton Agar (Isofar LTDA, Brazil) supplemented with 5% of human blood and Pseudomonas Agar (Merck RGaA, Germany), incubated for 24-48 hours at 35 ± 2ºC. The cultures were considered positive when the colonies counts were ³ 106 CFU/mL (8).
Urine
Quantitative technique was by plating on Müeller-Hinton Agar (Isofar LTDA, Brazil) supplemented with 5% of human blood, MacConkey Agar (BD, USA), Cled Agar (OXOID, England) and Sabouraud Agar (Merck, Germany), incubated for 24-48 hours at 35 ± 2ºC. The cultures were considered positive when the colonies counts were > 104 CFU/mL [8].
Microorganisms identification
The colonies were characterized as Staphylococcus through Gram staining and catalase test. Staphylococcus aureus identification was made by manitol salt agar fermentation and coagulase tests. Enterococcus spp were characterized by growth in trypticase soy broth (TSB) (Isofar, Brazil) supplemented with NaCl 6.5%, bile esculin (Laborclin, Brazil) and by PYR tests (BD, USA) (12).
Differentiation of Gram-negative microorganisms in Enterobacteriaceae family and non-fermenter bacilli was made through oxidation-fermentation (OF) and oxidase tests. The genus and species identification were made according to the following tests, carried out with kits produced by Newprov, Brazil:
- Enterobacteriaceae family: glucose and lactose fermentation, indol production, motility, citrate use, urea hydrolysis, sulfidric gas production, fenilalanine desaminase, lisine and ornitine descarboxilase, metil red reaction and Voges-Proskauer test.
- Non-fermenter Gram-negative bacilli: nitrate reduction, gluconate use, pigment production, lisine descarboxilase activity, urease activity, indol production, acetamide and esculin hydrolysis.
Antimicrobial susceptibility test
The test of diffusion in agar was applied according to recommendations of "Clinical and Laboratory Standards Institute (CLSI)" (4), using Müeller-Hinton Agar (Isofar LTDA, Brazil) and antibiotic disks (OXOID, England). The susceptibility of Staphylococcus aureus and coagulase-negative staphylococci to oxacilin was analyzed using disks of cefoxitine (30 µg). Enterococcus spp were tested for susceptibility to ampicillin (10 µg) and gentamicin (120 µg); Enterobacteriaceae family and Klebsiellae-Enterobacter group were tested for susceptibility to ceftriaxone (30 µg); E. coli group was tested for susceptibility to ciprofloxacin (5 µg) and ceftriaxone (30 µg); P. aeruginosa was tested for susceptibility to ciprofloxacin (5 µg), ceftazidime (30 µg) and imipenem (10 µg) and Acinetobacter spp were tested for susceptibility to imipenem (10 µg). Standard samples of Staphylococcus aureus (ATCC 25923), Escherichia coli (ATCC 25922), Klebsiella pneumoniae (ATCC 13883) and Pseudomonas aeruginosa (ATCC 27853) were used as controls.
Statistical analysis
Results were submitted to χ2 test, using the "Cálculos Estatísticos" (Version 1.8) statistical package.
RESULTS
The results corresponding to etiological agents and resistance phenotypes isolated from BSI, UTI and VAP of the AICU inpatients are listed in Tables 1 and 2. The main etiological agents of BSI at UTI were coagulase-negative staphylococci (24.6%), followed by S. aureus (19.3%), Klebsiellae and P. aeruginosa (23.4%). P. aeruginosa was also the main etiological agent of VAP (42.0%). The presence of candiduria (14.3%) and candidemia (8.8%) was considerable, contrasting with the few isolates of Enterococcus spp recovered in only three cases (5.7%) of BSI and in two cases (2.6%) of UTI.
The frequency of epidemiologically relevant resistance phenotypes like oxacilin-resistant S. aureus, oxacilin-resistant coagulase-negative staphylococci, third generation cephalosporins-resistant Klebsiellae and ceftazidime, fluoroquinolons and imipenem-resistant P. aeruginosa were superior to 50% (Table 2). The resistance to oxacilin was verified in approximately 64.0% and 47.0% of S. aureus samples isolated from blood and tracheal aspirate, respectively. Klebsielleae presented resistance to third generation cephalosporins in 55.5% and 83.0% of the isolates from urine and tracheal aspirate, respectively. The presence of fluoroquinolons-resistant P. aeruginosa (76.1%) and imipenem-resistant P. aeruginosa (72.0%) was also very high in the unit (Table 2).
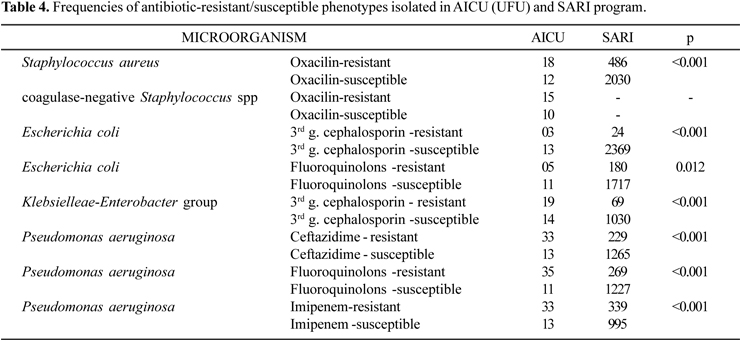
Table 3 shows the antibiotic consumption in the unit during the period of study, evidencing that cephalosporins (49.6%), glycopeptides (vancomycin) (37.4%) and carbapenems (26.6%) were the most prescribed antibiotics. It was observed that 80.3% of the patients were using some kind of antimicrobial, and 75.0% of them used two or more antimicrobials (Table 3). In Tables 4, 5 and 6 the results found in this study are compared to other results published in literature by national and international surveillance programs.
DISCUSSION
The extreme antibiotic use results in the emergence of resistant and multiresistant microorganisms, especially in hospital environment (13). This problem is even more serious in intensive care units, where oxacilin-resistant S. aureus, third generation cephalosporins-resistant, Klebsiella spp, Enterobacter spp and Escherichia coli, beyond carbapenems, ceftazidime and fluoroquinolons-resistant P. aeruginosa are isolated (5).
Due to the great importance of antibiotic-resistant microorganisms, the monitoring of their frequency, through surveillance programs such as ICARE in the United States (3), EPIC in Europe (5) and SARI (Germany) (15), is highly recommended. Additionally, programs developed by pharmaceutical industries such as SENTRY (18) and MYSTIC can provide relevant informations about antibiotic resistance (14).
In the present study, coagulase-negative staphylococci predominated as etiological agent of bloodstream infections (24.6% of the cases), followed by S. aureus (19.3%). P. aeruginosa was the main etiological agent of ventilator-associated pneumonia (42.0%), while the main etiological agent of urinary tract infection was the Klebsiella-Enterobacter group, responsible for 23.4% of the cases. In general, these results are similar to those report in other studies (3,5).
This research indicated a high resistance rate, especially among the Gram-negative bacilli. P. aeruginosa presented resistance above 70.0% to third generation cephalosporins, imipenem and fluoroquinolons, while ICARE published resistance rates to P. aeruginosa of 35.0% to fluoroquinolons, 19.0% to imipenem and 14.0% to third generation cephalosporins (3) and SARI reported resistance of 18.0% to fluoroquinolons, 25.4% to imipenem and 15.3% to third generation cephalosporins-resistance (15). SARI program also found 9.5% of fluoroquinolons-resistant E. coli and 6.3% of third generation cephalosporins-resistant Klebsiella-Enterobacter group (15), versus 31.2% and 57.6%, respectively, in Uberlândia. The differences between the results of this study and these international ones were statistically significant (p<0.05).
The frequencies of antibiotic resistant microorganisms detected in our study were higher than that observed in other Brazilian hospitals. The SENTRY program reported resistance to third generation cephalosporins in 43.7% of P. aeruginosa samples, contrasting with the results of this study where 71.7% of third generation cephalosporins-resistant P. aeruginosa were detected. The frequency of fluoroquinolons-resistant P. aeruginosa (76.1%) and imipenem-resistant P. aeruginosa (71.7%) found in this research was also higher than the presented by SENTRY program (50.1% and 37.8% respectively) (18). The comparison of the results showed a statistical significance. However, this observation was not the same for all microorganisms evaluated. For example, the higher rate of third generation cephalosporins-resistant E. coli (18.7%) when compared to that published by SENTRY (4.4%) (18), was not statistically significant.
In the Gram-positive group, only a low number of Enterococcus spp were isolated in this study. Their resistance to aminoglycosides was lower than in other studies (3,15,18). The frequency of oxacilin-resistant S. aureus was not statistically significant when compared to American hospitals data, (p=0.551) (3), and SENTRY program (p=0.129) (18), but it was statistically significant when compared to SARI program (p<0.01) (15). The same observation applies to oxacilin-resistant coagulase-negative staphylococci.
Compared to percentiles distribution elaborated by NNIS (25%, 50%, 75% and 90%), the frequency of oxacilin-resistant S. aureus in our study (60.0%) was higher than the average rate in North American critical units, where 75% of the evaluated units presented lower resistance rate than the observed in our unit. However, the occurrence of 60.0% oxacilin-resistant coagulase-negative staphylococci, figured in the percentile 25%, corresponding to the interval named "first quartile" (25%), means that such resistance rate was observed in only a quarter of the American critical units evaluated. In the group of Gram-negative bacilli, all microorganisms presented resistance frequencies above percentile 90%, what means that the resistance rate of this group in our unit was higher than the presented in 90% of North American critical units (3).
The evaluation of antibiotic consumption showed the cephalosporins (49.6%), glycopeptides (37.4%) and carbapenems (26.6%) as the most prescribed groups of antibiotics in the AICU, with the majority of patients (80.3%) in use of some kind of antimicrobial, during the period of study. Thus, the pressure force of antibiotics, added to other risk factors as invasive procedures and disease seriousness, makes intensive care units one of the most favorable places to emergency of resistant microorganisms (15). Additionally, the difficulties for implementation of measures to prevent and control nosocomial infections in developing countries (16), especially hands hygiene (10), must be considered. These measures are important for the reduction of horizontal dissemination of these microorganisms.
ACKNOWLEDGEMENTS
Our acknowledgements to Adult Intensive Care Unit's staff and UFU's microbiology laboratory for their valuable collaboration. This work was supported by "Conselho Nacional de Desenvolvimento Científico e Tecnológico" (CNPq).
Submitted: September 05, 2007; Returned to authors for corrections: October 24, 2007; Approved: October 22, 2008
* Corresponding Author. Mailing address:Universidade Federal de Uberlândia - Seção de Imunologia, Microbiologia e Parasitologia. Av. Pará, 1720 - Umuarama - CEP 38400-902 Uberlândia, MG, Brasil. Telfax: +55 34 3218-2332. E-mail: rodhc@hotmail.com
- 1. Abramczyk, M.L.; Carvalho, W.B.; Carvalho, E.S.; Medeiros, E.A.S. (2003). Nosocomial Infection in a Pediatric Intensive Care Unit in a Developing Country. Braz. J. Infect. Dis, 7 (3), 375-380.
- 2. Bronzwaer, S.L.A.M.; Cars, O.; Buchholz, U.; Mölstad, S.; Goettsch, W.; Veldhuijzen, I.K.; Kool, J.L.; Sprenger, M.J.W.; Degener, J.E. (2002). A European study on the relationship between antimicrobial use and antimicrobial resistance. Emerg. Infect. Dis, 8 (3), 278-282.
-
3CDC NNIS System. National Nosocomial Infections Surveillance (NNIS) system report, data summary from January 1992 through June 2004, issued October 2004 (2004). Am. J. Infect. Control, 32, 470-85.
-
4Clinical and Laboratory Standards Institute (CLSI). Performance standards for antimicrobial disk susceptibility tests, 9th ed. Approved M2-A9 (2006). Clin. Lab. Stand. Inst, 26 (1), 1-172.
- 5. Eggiman, P.; Pittet, D. (2001). Infection Control in the ICU. Chest, 120, 2059-2093.
- 6. Filius, P.M.G.; Gyssens, I.C.; Kershof, I.M.; Roovers, P.J.E.; Ott, A.; Vulto, A.G.; Verbrugh, H.A.; Endtz, H.P. Colonization and Resistance Dynamics of Gram-negative Bacteria in Patients during and after Hospitalization. Antimicrob. Agents Chemother, 49, 2879-2886.
- 7. Fridkin, S.K.; Gaynes, R.P. (1999). Antimicrobial resistance in intensive care units. Clin. Chest Med, 20 (2), 303-316.
- 8. Horan, T.C.; Gaynes, R.P. (2004). Surveillance of nosocomial infections. In: Mayhall, C.G. (ed). Hosp. Epidemiol. Infect. Control Lippincott Williams & Wilkins, Philadelphia, USA, p. 1659-1702.
- 9. Jones, M.E.; Draghi, D.C.; Thornsberry, C.; Karlowsky, J.A.; Sahm, D.F.; Wenzel, R.P. (2004). Emerging resistance among bacterial pathogens in the intensive care unit a European and North American Surveillance study (2000-2002). Ann. Clin. Microb., 3, 14-25.
- 10. Kampf, G.; Kramer, A. (2004). Epidemiology background of hand hygiene and evaluation on the most important agents for scrubs and rubs. Clin. Microbiol. Rev, 17 (4), 863-893.
- 11. Kollef, M.H.; Fraser, V.J. (2001). Antibiotic Resistance in the Intensive Care Unit. Ann. Intern. Med, 134, 298-314.
- 12. Konemam, E.W.; Allen, S.D.; Janda, W.M.; Schreckenberger, P.C.; Winn Jr., W.C. (1997). Guidelines for the collection, transport, processing, analysis, and reporting of cultures from specific specimen sources. In: __________. Color Atlas Textb. Diagn. Microbiol, New York, USA, p. 121-170.
- 13. Leibovici, L.; Soares-Weiser1, K.; Paul, M.; Goldberg1, E.; Herxheimer, A.; Garner, P. (2003). Considering resistance in systematic reviews of antibiotic treatment. J. Antimicrob. Chemother, 52, 564-571.
- 14. Mendes, C.; Oplustil, C.; Sakagami, E.; Turner, P.; Kiffer, C. (2005). Antimicrobial Susceptibility in Intensive Care Units: MYSTIC Program Brazil 2002. Braz. J. Infect. Dis., 9 (1), 44-51.
- 15. Meyer, E.; Jonas, D.; Schwab, F.; Rueden, H.; Gastmeider, P.; Daschner, F.D. (2003). Design of a surveillance system of antibiotic use and bacterial resistance in German intensive care unit (SARI). Infect., 31, 208-215.
- 16. Okeke, I.N.; Klugman, K.P.; Bhutta, Z.A.; Duse, A.G.; Jenkins, P.; O'brien, T.F.; Pablos-Mendes, A.; Laxminarayan, R. (2005). Antimicrobial resistance in developing countries. Part II: strategies for containment. Lancet, 5, 568-580.
- 17. Pó, M.V et. al (2006). O controle de infecção hospitalar no Brasil e os Consumidores. IDEC parceiro do consumidor, São Paulo, Jun. 2006. Disponível em <http://www.idec.org.br/arquivos/relatorio_IH.pdf>. Acesso em: 15 fev. 2007.
- 18. Sader, H.S.; Jones, R.N.; Gales, A.C.; Silva, J.B.; Pignatari, A.C. (2004) SENTRY Antimicrobial Surveillance Program Report: Latin American and Brazilian Results for 1997 through 2001. Braz. J. Infect. Dis. 8 (1), 25-79.
- 19. Shlaes, D.M.; Gerding, D.N.; John Jr., J.F.; Craig, W.A.; Bornstein, D.L.; Duncan, R.A.; Eckman, M.R.; Farrer, W.E.; Greene, W.H.; Lorian, V.; Levy, S.; McGowan Jr., J.E.; Paul, S.M.; Ruskin, J.; Tenover, F.C.; Watanakunakorn, C. (1997). Society for Healthcare Epidemiology of America and Infectious Diseases Society of America Joint Committee on the Prevention of Antimicrobial Resistance: Guidelines for the Prevention of Antimicrobial Resistance in Hospitals. Infect. Control Hosp. Epidemiol 18, 275-91.
- 20. Weber, D.J.; Raasch, R.; Rutala, W.A. (1999). Nosocomial infections in the ICU: The growing importance of antibiotic-resistant pathogens. Chest 115, 34-41.
Publication Dates
-
Publication in this collection
06 Apr 2009 -
Date of issue
Dec 2008
History
-
Accepted
24 Oct 2007 -
Received
05 Sept 2007